Summary
There are scarce data on the impact of COVID‐19 pandemic on liver transplantation (LT) in Europe. The aim of this study was to obtain a preliminary data on incidence, management, and outcome of COVID‐19 in liver transplant recipients and candidates in Europe. An Internet‐based survey was sent to the centers affiliated with European Liver Transplant Registry (ELTR). One hundred nine out of 149 (73%) of ELTR centers located in 28 European countries (93%) responded. Ninety‐four (86%) of the centers tested all donors, and 75 (69%) centers tested all LT recipients for SARS‐CoV‐2. Seventy‐three (67%) centers selected recipients for LT in the COVID‐19 pandemic, whereas 33% did not. Eighty‐eight centers reported COVID‐19 infection in 57 LT candidates and in 272 LT recipients. Overall crude incidence of COVID‐19 among LT candidates and recipients was estimated 1.05% (range 0.5–20%) and 0.34% (range 0.1–4.8%), respectively, and it was significantly higher among candidates (P < 0.001). Crude rate of death was 18% (10/57) among candidates and 15% (36/244) among recipients. This first large‐scale European snapshot study clearly shows that both LT candidates and recipients are at a high risk for COVID‐19. These results plead for an early and pro‐active screening of COVID‐19 symptoms in these populations.
Keywords: COVID‐19, liver recipient, liver transplantation, mortality, SARS‐CoV‐2, survey
Introduction
Since the declaration on March 11, 2020, by the World Health Organization of the SARS‐CoV‐2/COVID‐19 pandemic, a considerable amount of publications and data regarding clinical presentation, natural history of the disease, and risk factors driving prognosis in general population have been accumulated [1, 2, 3]. However, there are still scarce data regarding specific populations with unique risks, such an organ transplant recipients [4, 5, 6]. Whether immunosuppression is associated with more aggressive patterns of infection versus general population or, on the contrary, may protect against the dramatic innate, inflammatory immune response that arises with relative frequency in the course of the disease is unknown [7, 8].
A recent short communication reported on three severe cases of COVID‐19 leading to death among a cohort of 111 COVID‐19 liver transplant recipients in Lombardy, providing initial indication of a potentially aggressive disease pattern in this population [9]. Aside from disease in recipients, LT teams have also faced and continue to face other important issues of uncertainty surrounding donor and recipient selection and testing as well as disease affecting LT candidates. To address the practice patterns surrounding incidence, management, and outcome of COVID‐19 in liver transplant recipients and candidates, the European Liver and Intestine Transplantation Association (ELITA) launched a survey on March 24, 2020, among the 149 active LT centers located in 30 European countries that are affiliated with the European Liver Transplant Registry (ELTR). Herein, we report preliminary data on incidence and impact of COVID‐19 in both LT candidates and recipients as well as on strategies adopted by LT centers to cope with LT in this unprecedented period.
Patients and methods
Study design
An Internet‐based survey was sent to the main investigator, and all the co‐investigators registered in the ELTR platform, in accordance with ELTR regulations. The survey consists of two parts (Fig. 1). The first questionnaire (SurveyMonkey 1: SM1) contained 17 items (Appendix S1). Apart from center identifying information and case volume, all the other items were multiple‐choice questions related to how SARS‐CoV‐2 affected LT donor, candidate, and recipient management at each center. In the second questionnaire (SurveyMonkey 2: SM2), in order to obtain more concrete data regarding symptomatic COVID‐19 infection among LT candidates and recipients, 14 questions were sent in parallel and scheduled to be updated on a regular basis over the period of the epidemic (Appendix S2). Symptomatic COVID 19 cases in LT candidates/recipients were defined as patients presenting with relevant clinical symptoms and positive swab PCR and/or highly suggestive lung injury on thoracic CT scan. Data from the second questionnaire have been updated through April 24, 2020.
Figure 1.
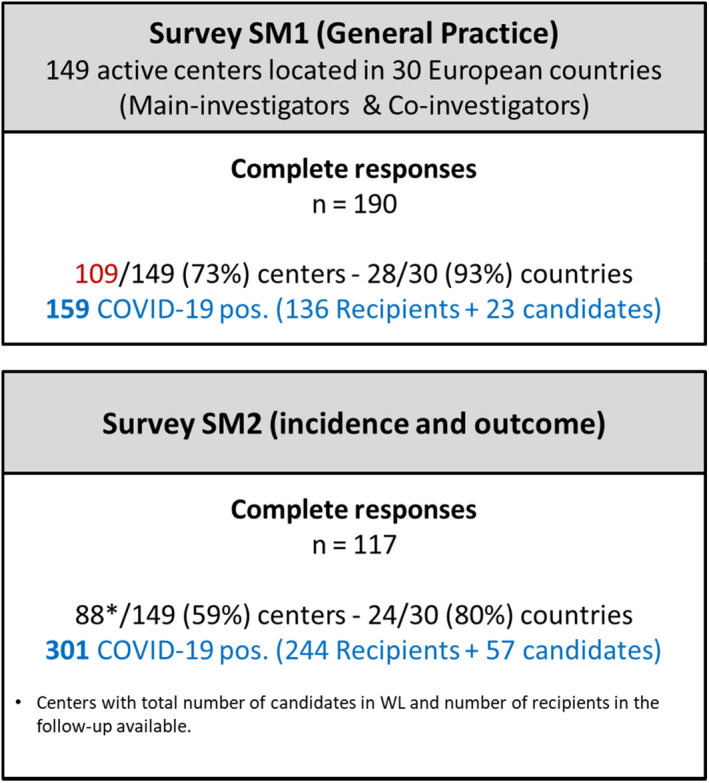
Outline of the study.
Survey administration
The first questionnaire (SM1) was distributed by SurveyMonkey® (Palo Alto, CA, USA) between March 24, 2020, and April 8, 2020. The subsequent reminders were sent to nonresponders every three days. The second questionnaire (SM2) was distributed first on March 24 with updates between April 4 and 10 and again between April 20 and 24. Participation in the survey was entirely voluntary. Data were collected in accordance with General Data Protection Regulation (GDPR), in accordance with European Union Legislation, the ELTR privacy declaration, and the SurveyMonkey® privacy policy.
Statistical analysis
Descriptive statistics are presented as percentage for SM1 and crude incidences for SM2. For SM2, the fixed denominators were the number of patients on the waiting lists and the number of living adult LT recipients in each center; incidences were calculated overall or by country when appropriate. As benchmarks, incidence of symptomatic COVID‐19 and COVID‐19‐related deaths among the adult general population in each country were estimated based on the number of COVID 19 recorded by GISAID (https://www.gisaid.org) through April 24, 2020, and on adult population estimates by country as reported by the world population review website (https://worldpopulationreview.com) [10, 11].
Categorical variables were summarized as frequencies and percentages, and groups were compared by chi‐squared test. P‐value of <0.05 was considered significant.
Results
Results of survey on the practices in the liver transplant centers (SM)
One hundred nine out of 149 (73%) of ELTR centers located in 28 European countries (93%) responded the survey SM1 (Fig. 1).
Donor management
Eighty‐six percent of the centers tested all donors for SARS‐CoV‐2, while 8% did not (Fig. 2a). Remaining centers (6%) temporarily halted all transplant activity due to the lack of donors and/or other collateral effects the pandemic. The majority centers (91%) responded that they did not transplant livers from SARS‐CoV‐2 positive donors. Only 3% centers responded that they did or would consider transplanting organs from SARS‐CoV‐2 positive donors (Fig. 2b): 51% to high urgent candidates only, 2% to high MELD candidates only, and remaining 47% to any potential LT candidates (Fig. 2c). In centers performing living donor liver transplantation, 54% responded that they tested their donors for SARS‐CoV‐2, whereas 32% did not (Fig. 2d). If the living donor turned out to be SARS‐CoV‐2 positive, 53% of the centers responded that they would delay donation after donor recovery >2 weeks (Fig. 2e), and additional 39% would extend that delay to >4 weeks (data not shown).
Figure 2.
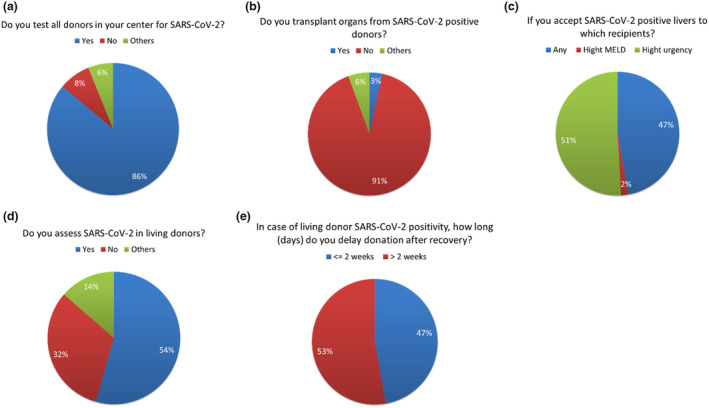
Management of liver donors in European center during COVID‐19 pandemic. (a) Donor testing with nasopharyngeal swab PCR for SARS‐CoV‐2. (b) Liver transplantation from SARS‐CoV‐2 positive donors. (c) Recipient selection for liver grafts from SARS‐CoV‐2 positive donors. (d) Living liver donors testing for SARS‐CoV‐2. E. Delay time in live liver donation in SARS‐CoV‐2 positive donors.
Recipient management
Among responders, 69% tested all liver transplant recipients for SARS‐CoV‐2 at the moment a liver became available for transplantation, while 30% performed no test (Fig. 3a). If the test resulted positive, 55% of responders canceled LT, 34% re‐allocated the liver to another potential recipient, and only 5% responded that they would proceed with LT as originally planned (Fig. 3b). In case of unknown status of SARS‐CoV‐2 in the potential liver recipient, 42% centers went forward with LT, 22% canceled LT, and 18% re‐allocated the liver to another recipient (Fig. 3c).
Figure 3.
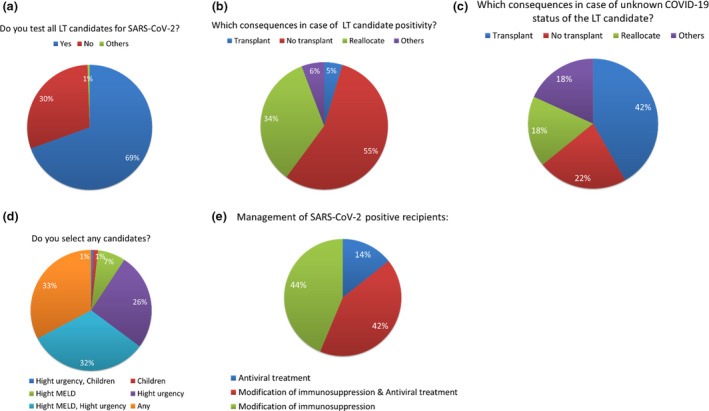
Management of liver recipients in European center during COVID‐19 pandemic. (a) Potential recipient testing with nasopharyngeal swab PCR for SARS‐CoV‐2. (b) Consequences of SARS‐CoV‐2 positivity in the potential liver recipient. (c) Consequences of unknown SARS‐CoV‐19 status in the potential liver recipient. (d) Selection of liver recipient for transplantation in COVID‐19 pandemic. (e) Management of SARS‐CoV‐2 positive liver recipients.
During the height of COVID‐19 pandemic, 33% centers did not select potential recipients for LT, 32% selected only high MELD or high urgency patients, 26% selected only high urgency patients, 7% selected only high MELD patients, 1% selected only children, and 1% selected only high urgency children (Fig. 3d).
If COVID‐19 were to be diagnosed post‐transplant, 44% of responders modified immunosuppression therapy, 42% modified immunosuppression and started antiviral treatment, and 14% started only antiviral treatment without modification of immunosuppression regimen (Fig. 3e).
COVID‐19 in LT candidates and recipients (analysis of survey SM2)
Among the 149 active ELTR centers, 117 completed the SM2 (79%) providing data from 80% of ELTR countries. Fifty‐seven cases of symptomatic COVID‐19 among LT candidates and 272 cases of COVID‐19 among LT recipients were identified. No cases symptomatic cases were detected among candidates and recipients at 49% centers (57/117) and 74% centers (86/117), respectively.
Dynamics and incidence of COVID 19 in LT candidates and recipients
Evolution of the overall number of COVID‐19 cases reported to the survey is shown in Fig. 4. In one month, the number of infected candidates increased sixfold and grew twice as fast as the number of recipients, which tripled at the same time period. The distribution of cases across countries is shown in Fig. 5 (this figure is regularly updated at the ESOT website) [12]. COVID‐19 among LT patients was disproportionately higher in three countries—Italy, France, and Spain—which accounted for 74% of the total number of cases.
Figure 4.
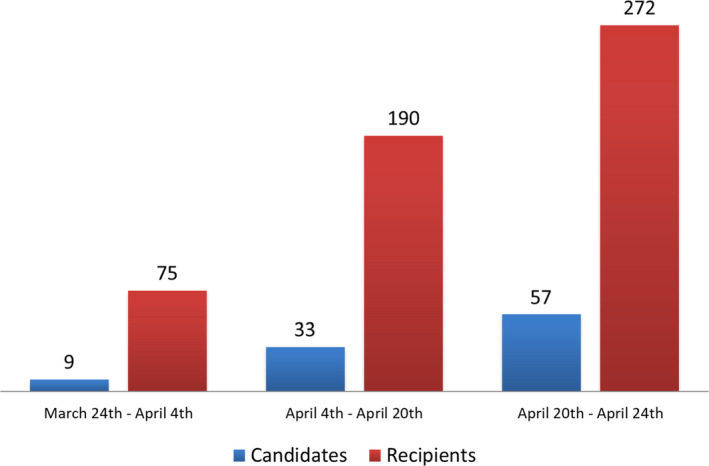
Number of SARS‐CoV‐2 positive liver transplant recipient and candidates.
Figure 5.
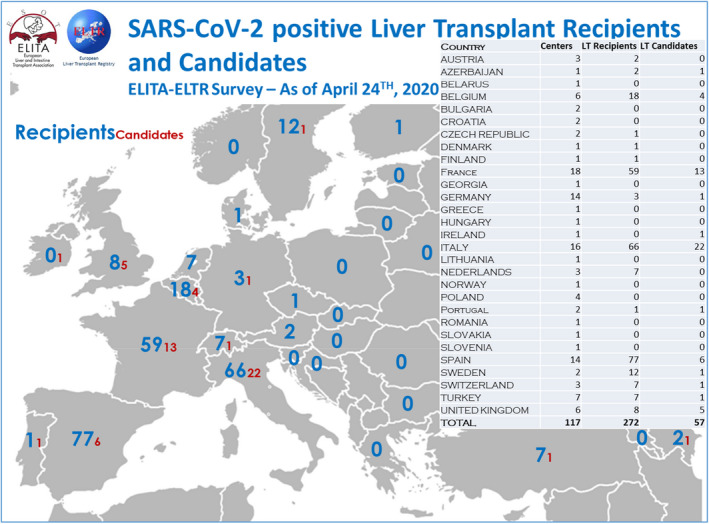
Distribution of SARS‐CoV‐2 positive liver transplant candidates and recipient and in Europe.
Among the 117 centers which responded to SM2, 88 provided the total number of candidates in waiting lists and adult LT recipients they had in follow‐up; among these, cases were included the aforementioned 57 LT candidates and 244 of the aforementioned 272 LT recipients that developed symptomatic COVID‐19. The corresponding cumulative numbers of LT candidates and living adult LT recipients were 5440 and 71 516, respectively.
Based on these figures, the overall crude incidence of symptomatic COVID‐19 in the LT candidates was estimated to be 1.05% (57/5440) ranging from 0.5% to 20% across centers. Among LT recipients, the incidence was estimated to be 0.3% (244/71 516), ranging from 0.1% to 5%. The incidence of symptomatic COVID‐19 infection was significantly higher in LT candidates compared with LT recipients (P < 0.001). It was also significantly higher among LT candidates compared with the general population (P < 0.001) as shown in Fig. 6. The incidence of symptomatic COVID‐19 infection among LT recipients was not different compared to the general population.
Figure 6.
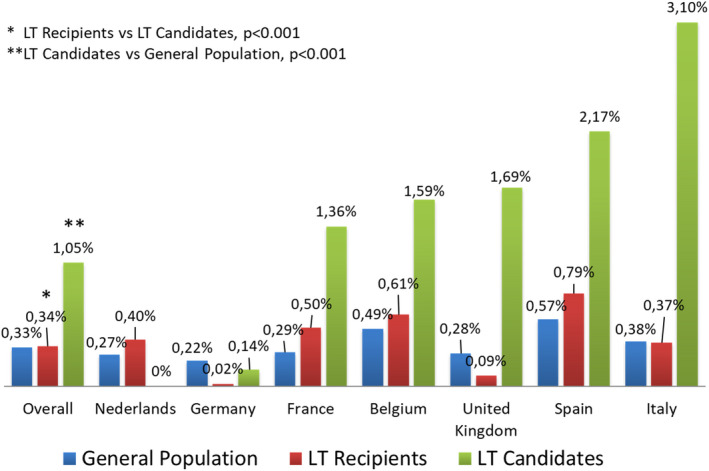
Incidence of SARS‐CoV‐2 in liver transplant patients compared to the general population.
Morbidity and mortality associated with COVID‐19 in LT candidates and recipients
Eight LT candidates and 33 LT recipients were admitted to intensive care over the observation period, corresponding to a crude incidence for intensive care admission of 14% for both groups Fig. 7.
Figure 7.
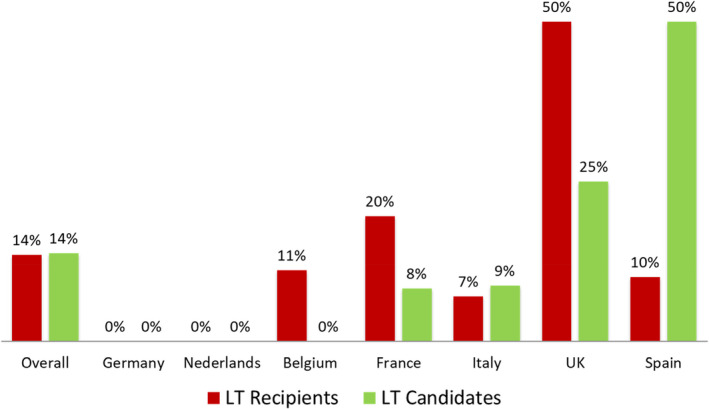
Intensive care admission among SARS‐CoV‐2 positive liver transplant patients.
Mortality rates among LT candidates, LT recipients, and in the general population, overall and by country, are shown in Fig. 8. Among the 57 and 244 COVID‐19 cases reported pre‐LT and post‐LT, 10 and 36 patients, respectively, died due to COVID‐19 or its complications corresponding to a crude rate of death of 18% (10/57) among LT candidates and 15% (36/244) among LT recipients.
Figure 8.
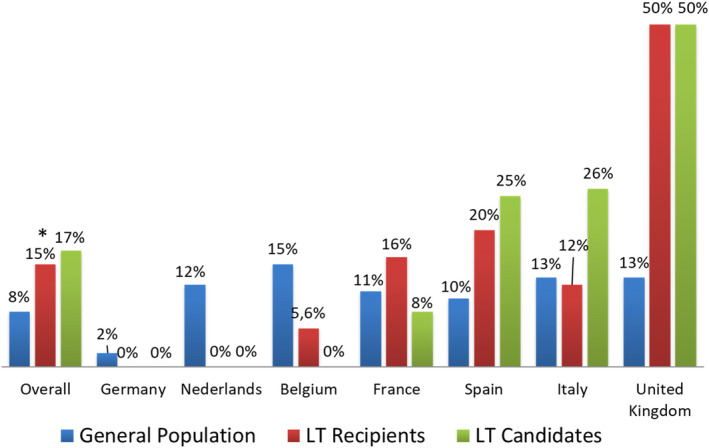
Incidence of mortality among SARS‐CoV‐2 positive liver transplant patients compared to the general population.
While death rates did not vary significantly between candidates and recipients, mortality due to COVID‐19 was significantly higher among LT patients than among the general population (79 039 deaths among 939 741 infections—8%; P < 0.05 vs. LT candidates and <0.001 vs. LT recipients).
Discussion
Although a considerable amount of data about the incidence and severity of COVID‐19 in the general population have accumulated over the past 2 months, data regarding COVID‐19 in transplant populations are still scarce [4, 5, 9]. A preliminary report provided an initial indication that severe forms of COVID‐19 may lead to death among LT patients, but the magnitude of the problem up until this point has remained relatively unclear [9].
The present survey is the first attempt to estimate frequency and severity of COVID‐19 in LT candidates and recipients across Europe. The European Liver Transplantation Association (ELITA) and the European Liver Transplant Registry (ELTR) launched a simple survey across the ELTR network of LT centers between March and April 2020. Fifty‐seven and 272 cases of COVID‐19 infection were identified among LT candidates and recipients, respectively, with a rapid increase in reported cases observed over the survey period. These figures correspond to crude COVID‐19 incidence rates of 1% among LT candidates and 0.3% among LT recipients, with a disproportionate number of cases detected in Western and Southern European countries, namely France, Spain, and Italy, compared to Eastern and Northern European countries [13, 14]. Such a distribution was not unexpected and follows the distribution of COVID‐19 observed in the general European population. Notably, very few cases were reported from Austria, Germany, Poland, Czech Republic, and Norway though this might be due to a certain degree of underreporting .
Interestingly, symptomatic COVID‐19 cases were identified with significantly greater frequency among LT candidates than recipients. One of the possible explanations for this could be that LT recipients, based on their baseline experience with immunosuppression, are more aware of their risk of infection and have better adherence to social distancing and other preventative measures (handwashing, mask wearing, etc.). Though not without limitations, our preliminary data also suggest that symptomatic COVID‐19 may be observed significantly more frequently in both LT candidates and recipients than in the general population.
The rate of admission to intensive care and deaths related to COVID‐19 were high in both LT candidates and LT recipients and did not differ significantly between these two groups. Mortality related to COVID‐19 was 18% among LT candidates and 15% among LT recipients, and was significantly higher than mortality estimated among the general adult population (8%). Of note, data on the incidence of symptomatic COVID‐19 infection and associated mortality rates were unadjusted yet and should be interpreted with caution. More studies are needed to define risk factors for a poor outcome following COVID‐19 infection in the LT setting, in order to effectively use limited medical resources and avoid futile treatment.
It is well known that among the general population symptomatic cases of COVID‐19 and cases resulting in death bear direct relation with male sex increasing age, and obesity. It is also known that male sex is more frequent among the LT population in general, among which approximately 70% of LT candidates and recipients are men [15]. Although gender and age were not available for the whole survey population (data collection in progress), preliminary analysis of a subset of LT candidates and recipients (data not shown) has revealed, a higher percentage of men among LT candidates (93%) and LT recipients (67%) and mean ages of 59 ± 15 and 62 ± 14 years for each group, respectively. One cannot, therefore, exclude the possibility that the apparently higher incidence of symptomatic and severe forms of COVID‐19 compared to general population as observed in this survey is driven by higher percentage of men among LT candidates and LT recipients and higher mean ages for each group.
To overcome this issue, collection of more detailed data in our study population, including age, sex, co‐morbidities, clinical presentation, and management of COVID‐19 infection, is in progress and will be the basis of another future report.
Another part of our study focused on the current practices among LT centers in Europe regarding donor and recipient management in the period surrounding the peak of COVID‐19 infection. Not surprisingly, the majority of the centers are performing PCR tests on nasopharyngeal swab among both deceased donors (86%) and recipients (69%) in order to detect presence of SARS‐CoV‐2, which is in a line with the recommendations of transplant societies [16]. However, as recently reported the transplant centers also face a lack of empiric evidence on COVID‐19 and standardized protocols to ruled out SARS‐CoV‐2 infection [17]. Another striking information from the survey is that 6% of liver transplant centers in Europe temporarily halted LT activity due to lack of the donors and other collateral effects of the pandemic (e.g., lack of non‐COVID intensive care, general ward, and even operating room space to safely care for LT patients in the perioperative period). Significant decreases in organ donation have been reported by many organ sharing organizations in Europe since the start of the pandemic, though there are also other reports that suggest that even in countries with a high prevalence of COVID‐19, such as Italy, LT programs can continue their activities [18, 19]. As well, 3% of responding centers claimed that they would use the liver from SARS‐CoV‐2 positive donor for high urgent or high MELD recipients. While there is no evidence about the risk of SARS‐CoV‐2 transmission via solid organ transplant, this practice cannot currently be advised, as it also potentially places the organ recovery team at risk for infection. As LT is lifesaving procedure, two‐third of responding centers do selectively recipients in the COVID‐19 pandemic (32% with high MELD or high urgency indication, 26% only high urgency indication, seven only high MELD, 2% only children), whereas remaining third does not. In consideration of the aforementioned decrease in the donation rate, it seems reasonable that transplant centers in areas with high rates of COVID‐19 infection may find themselves obliged to select only recipients at risk of death or dropout from the waiting list.
In conclusion, this first large‐scale European snapshot study shows that COVID‐19 pandemic has had a significantly impact on LT activity in a majority of centers, which have restricted LT to most urgent candidates. Moreover, this study clearly shows that LT candidates and recipients are both at high risk for COVID‐19 infection to an extent that could potentially be higher than the general population. Mortality could be particularly high in this population, as well, because of disproportionate numbers of men and individuals of more advanced age (≥50–60 years) These preliminary results should serve as a prompt for early screening of COVID‐19 symptoms among LT candidates and recipients and pro‐active management according to current best practice guidelines, in order to potentially counteract the dramatic consequences of SARS‐CoV‐2 infection in this seemingly high‐risk population.
Authorship
WGP and CD: designed and performed the study, analyzed data and wrote the manuscript. CF and RA: designed and performed the study, and wrote the manuscript. VK: collected and analyzed data, and wrote the manuscript. UB, GG, SN, PT, CT, RIT, KZ and LB: designed and performed the study, and critically revised the manuscript.
Funding
The authors have declared no funding.
Conflict of interest
The authors have declared no conflicts of interest.
Supporting information
Appendix S1. XXX.
Appendix S2. XXX.
Appendix S3. XXX.
Acknowledgements
The authors would like to acknowledge Dr. Amelia Hessheimer for a critical review of this manuscript. ELITA would like to express gratitude to all ELTR centers contributing for this survey (Appendix S3). The Organ Sharing Organizations the French ABM (Sami Djabbour), the Dutch NTS (Maaike de Wolf), the Eurotransplant Foundation (Marieke Van Meel), the Spanish ONT (Gloria de la Rosa), the UK–Ireland NHSBT (Michael Daynes), and the Scandiatransplant (Ilse Duus Weinreich) are acknowledged for their support in the conducting of the survey. The ELTR is supported by a grant from Astellas, Novartis, Institut Georges Lopez, Sandoz, and logistic support from the Paul Brousse Hospital (Assistance Publique—Hôpitaux de Paris).
References
- 1. Lescure FX, Bouadma L, Nguyen D, et al. Clinical and virological data of the first cases of COVID‐19 in Europe: a case series. Lancet Infect Dis 2020; 20: 697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID‐19 in Wuhan, China: a retrospective cohort study. Lancet 2020; 395: 1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. http://www.euro.who.int/en/health‐topics/health‐emergencies/coronavirus‐covid‐19/news/news/2020/3/who‐announces‐covid‐19‐outbreak‐a‐pandemic.
- 4. Akalin E, Azzi Y, Bartash R, et al. Covid‐19 and kidney transplantation. N Engl J Med 2020; 382: 2475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fernández‐Ruiz M, Andrés A, Loinaz C, et al. COVID‐19 in solid organ transplant recipients: a single‐center case series from Spain. Am J Transplant 2020; 20: 1849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Aigner C, Dittmer U, Kamler M, Collaud S, Taube C. COVID‐19 in a lung transplant recipient. J Heart Lung Transplant 2020; 39: 610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mehta P, McAuley DF, Brown M, et al. COVID‐19: consider cytokine storm syndromes and immunosuppression. Lancet 2020; 395: 1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Guillen E, Pineiro GJ, Revuelta I, et al. Case report of COVID‐19 in a kidney transplant recipient: does immunosuppression alter the clinical presentation? Am J Transplant 2020; 20: 1875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bhoori S, Rossi RE, Citterio D, Mazzaferro V. long‐term liver transplant patients: preliminary experience from an Italian transplant centre in Lombardy. Lancet Gastroenterol Hepatol 2020; 5: 532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. www.gisaid.org.
- 11. worldpopulationreview.com.
- 12. https://edu.esottransplantlive.org.
- 13. Domínguez‐Gil B, Coll E, Fernández‐Ruiz M, et al. COVID‐19 in Spain: transplantation in the midst of the pandemic. Am J Transplant 2020. 10.1111/ajt.15983. Online ahead of print [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Angelico R, Trapani S, Manzia TM, Lombardini L, Tisone G, Cardillo M. The COVID‐19 outbreak in Italy: initial implications for organ transplantation programs. Am J Transplant 2020; 20: 1780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Adam R, Karam V, Cailliez V, et al. Annual report of the European Liver Transplant Registry (ELTR) – 50‐year evolution of liver transplantation. Transpl Int 2018; 31: 1293. [DOI] [PubMed] [Google Scholar]
- 16. Fix OK, Hameed B, Fontana RJ, et al. Clinical best practice advice for hepatology and liver transplant providers during the COVID‐19 pandemic: AASLD expert panel consensus statement. Hepatology 2020; 72: 287. 10.1002/hep.31281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ritschl PV, Nevermann N, Wiering L, et al. Solid organ transplantation programs facing lack of empiric evidence in the COVID‐19 pandemic: a by‐proxy society recommendation consensus approach. Am J Transplant 2020; 20: 1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Maggi U, De Carlis L, Yiu D, et al. The impact of the COVID‐19 outbreak on liver transplantation programmes in Northern Italy. Am J Transplant 2020). 20, 1840. 10.1111/ajt.15948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lauterio A, De Carlis R, Belli L, Fumagalli R, De Carlis L. How to guarantee liver transplantation in the north of Italy during the COVID‐19 pandemic. A sound transplant protection strategy. Transpl Int 2020). 33, 969. 10.1111/tri.13633. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. XXX.
Appendix S2. XXX.
Appendix S3. XXX.


