Abstract
Face masks wearing during the coronavirus disease 2019 (COVID‐19) pandemic became ubiquitous. The aim of our study was to assess the use of face masks among young adults during the current viral pandemic. The survey was based on specially created Google Forms and posted on numerous Facebook groups for young people in Poland. Seven days were considered as a recall period. A total of 2315 answers were obtained, 2307 were finally analysis, as eight questionnaires were removed because of data incompleteness. 60.4% of responders declared using the face masks. Those who reported an atopic predisposition wore face masks significantly (P = .007) more commonly (65.5% and 57.7%, respectively). Cloth masks (46.2%) appeared to be most popular ones, followed by surgical masks (39.2%), respirators (N95 and FFP) (13.3%), half‐face elastomeric respirators (0.8%) and full‐face respirators (0.4%). Females significantly more frequently (P = .0001) used cloth masks; respirators, half‐face elastomeric respirators and full‐face respirators were used more commonly by males (P < .0001, P = .001 and P = .001, respectively). 23.9% of responders who used single‐use mask wore it again. Moreover, 73.6% participants declared mask decontamination; however, the procedures were not always appropriate. We suggest that our results may be of help in construction of general public education campaigns on the proper use of face masks.
Keywords: COVID‐19, face masks
1. INTRODUCTION
The use of face masks by general population became ubiquitous during the coronavirus disease 2019 (COVID‐19) pandemic, 1 , 2 , 3 although the scientific evidence on their prevention against viral infection spreading is scarce. 4 , 5 Due to the crisis of availability of professional face masks, including N95 masks, in some countries, non‐medical masks, such as cloth masks, were recommended for general public. 1 , 3 The aim of this study was to assess the use of facial masks among young adults during the current viral pandemic.
2. MATERIALS AND METHODS
The study was based on the specially designed online survey. The questionnaire was developed based on the interviews of 10 students. All the relevant issues raised during the interviews were put up together and considered for the questionnaire. Then, the proposed questionnaire was assessed by two independent experts in such studies, who gave their comments on the proper wording and understanding of each question. A 7‐day period was taken as a recall period. The final survey was created with Google Forms and posted on numerous Facebook groups for young people in Poland. This population was our target as young adults are the most mobile and active part of population, and therefore particularly exposed to increased risk of viral infection. On 9 April 2020, Polish Ministry of Health announced that starting from 16 April 2020 covering the nose and mouth when being in public space is obligatory. Thus, we intentionally collected data in 48 hours (between 12 April 2020, 10:00 pm and 14 April 2020, 10:00 pm) when face masks use was not obligatory, but clearly recommended. A total of 2315 answers were obtained. Due to the incompleteness of the data, eight questionnaires were removed. Therefore, 2307 surveys (99.7%) were considered for final analysis. Such sample size reached 95% confidence level with only 2% margin of error (385 people were calculated as a representative sample size). The mean age of the group was 20.2 ± 1.7 years (range: 18‐27 years). The selected responses were downloaded for statistical analysis (Statistica 13; Statsoft, Tulsa, Oklahoma). The chi‐square test was applied to determine statistical differences between the studied groups. The resulting P values were considered significant if P < .05.
3. RESULTS
In total, 1393 responders (60.4%) declared the use of face masks. There was no difference (P = .12) in the frequency of face protection use between females and males (Table 1). Interestingly, significantly more responders (P = .007) who reported an atopic predisposition wore face masks (65.5% and 57.7%, respectively). Having self‐reported sensitive skin did not influence the frequency of face masks wearing (P = .06). 34.0% participants (significantly more males, P = .0012) used several types of face masks (Table 1). Out of all usages, cloth masks (46.2%) appeared to be the most popular ones, followed by surgical masks (39.2%), respirators (N95 and FFP (filtering facepiece)) (13.3%), half‐face elastomeric respirators (0.8%) and full‐face respirators (0.4%). Females significantly more frequently (P = .0001) used cloth masks; respirators, half‐face elastomeric respirators and full‐face respirators were used more commonly by males (P < .0001, P = .001 and P = .001, respectively) (Table 1). Among those using several types of masks, 52.7% declared cloth mask as the most frequently used, 36.8% responders declared surgical mask as a dominant type and the remaining 10.5% preferred respirators. Most frequently, face masks were worn, independent of the sex of responders, for less than 1 hour per day; however, almost 4% of users wore them for more than 5 hours per day (Table 1, Figure 1). Concerning all the masks used, single‐use masks constituted 52.5%. It appeared that 23.9% of responders who used single‐use staff wore it again. There was no difference in this attitude between males and females (Table 1). 73.6% of participants declared mask decontamination (Table 1). This procedure was significantly more common among females (P = .004). Washing combined with ironing was the most common modality applied (63%), followed by the use of disinfectants (19.4%), ironing alone (4.8%) and putting into the oven (3.5%). Other procedures, such as washing alone, microwaving, boiling and scalding with boiling water, were practiced by a single responder.
TABLE 1.
Face mask use among young adults during the COVID‐19: comparison of females and males
| Total | Females | Males | P value* | |
|---|---|---|---|---|
| Participants using face masks | .12 | |||
| Yes | 1393 (60.4%) | 138 (61.1%) | 255 (57.2%) | |
| No | 914 (39.6%) | 723 (38.9%) | 191 (42.8%) | |
| Types of face masks used | ||||
| Surgical masks | 755 (39.2%) | 606 (39.1%) | 149 (39.4%) | .13 |
| Cloth masks | 891 (46.2%) | 753 (48.6%) | 138 (36.5%) | .0003 |
| Respirators (N95 + FFP) | 257 (13.3%) | 179 (11.6%) | 78 (20.6%) | <.0001 |
| Half‐face elastometric respirator | 16 (0.8%) | 8 (0.5%) | 8 (2.2%) | .001 |
| Full‐face respirator | 8 (0.4%) | 3 (0.2%) | 5 (1.3%) | .001 |
| Several types of masks used | 473 (34.0%) | 364 (32.0%) | 109 (42.7%) | .0012 |
| Duration of masks used per day | ||||
| More than 1 hr | 680 (48.8%) | 552 (48.5%) | 128 (50.2%) | .57 |
| More than 2 hr | 217 (15.6%) | 172 (15.1%) | 45 (17.6%) | .29 |
| Multiple use of single‐use masks | 333 (23.9)% | 263 (23.1%) | 70 (27.5%) | .21 |
| Decontamination of masks | 1026 (73.6%) | 857 (75.3%) | 169 (66.3%) | .004 |
Abbreviations: COVID‐19, coronavirus disease 2019; FFP, filtering facepiece.
*P values were considered significant if P < .05 (bold).
FIGURE 1.
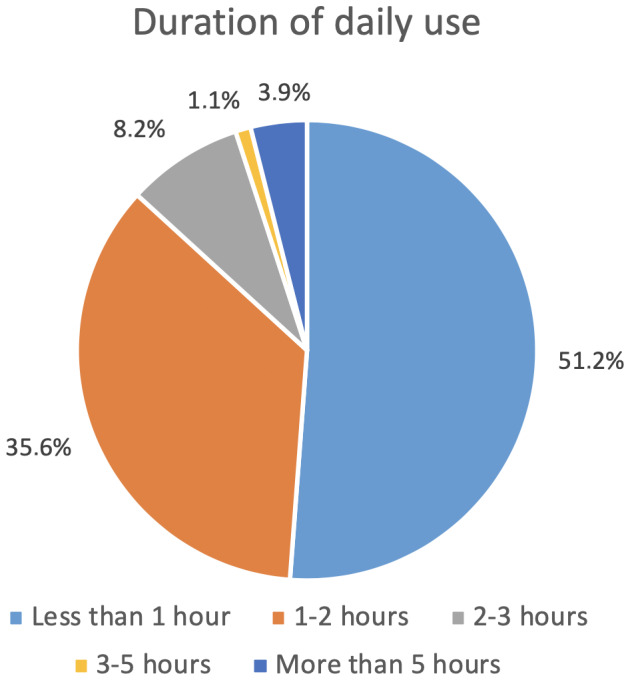
Duration of daily use of face masks (hours per day)
4. DISCUSSION
To the best of our knowledge, such real‐life data on the use of face masks have not been reported so far. Although the scientific evidence on the protective efficacy of face masks wearing against human‐to‐human viral transmission is not strong enough, 4 , 5 many governments and institutions (eg, Robert Koch Institute and Centers for Disease Control) at least recommend to cover mouth and nose with the cloth face cover when around others during the COVID‐19 pandemic.
In this survey, we documented that people with self‐reported atopic predisposition wore face masks more frequently. It seems to be obvious as atopic disorders are clearly linked to the involvement of respiratory tract and increased risk of infections. 6 , 7 Such relationship could be bidirectional with atopy predisposing to viral infections and viral infection may trigger the atopic asthma. 8 In the previous viral pandemics, there was a clear crisis in the availability of professional face protection. 3 Therefore, cloth masks were used commonly. This is in agreement with our findings showing the popularity of cloth mask protection used by the general public. One can consider that despite of protection provided by face masks they may be the cause of some side effects, including breathing difficulties, slurred speech, warming/sweating and itching. 9 , 10 , 11 This may influence the use of face masks when they are only recommended and not obligatory. Limited availability of professional face masks most probably was the reason that almost one‐quarter of our responders used single‐use masks several times. Moreover, three‐quarters of the evaluated individuals wearing face masks declared mask decontamination. Nonetheless, our results showed that some practices among young people could be regarded as inappropriate. This can lead to decreased efficacy of face protection and eventual spread of viral infection. Therefore, we believe that our results might be of value in construction of general public education campaigns on the proper use of face masks, especially if the role of face mask wearing in controlling the spread of infection is clearly documented.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
AUTHOR CONTRIBUTIONS
Łukasz Matusiak: Research concept and design; Collection and/or assembly of data; Data analysis and interpretation; Writing the article; Critical revision of the article; Final approval of article. Marta Szepietowska: Research concept and design; Collection and/or assembly of data; Writing the article; Critical revision of the article. Piotr K. Krajewski: Collection and/or assembly of data; Data analysis and interpretation; Writing the article; Critical revision of the article. Rafał Białynicki: Research concept and design; Collection and/or assembly of data; Writing the article; Critical revision of the article. Jacek C. Szepietowski: Research concept and design; Collection and/or assembly of data; Data analysis and interpretation; Writing the article; Critical revision of the article; Final approval of article.
Matusiak Ł, Szepietowska M, Krajewski PK, Białynicki‐Birula R, Szepietowski JC. The use of face masks during the COVID‐19 pandemic in Poland: A survey study of 2315 young adults. Dermatologic Therapy. 2020;33:e13909. 10.1111/dth.13909
Łukasz Matusiak and Marta Szepietowska share co‐first authorship for this study.
REFERENCES
- 1. Feng S, Shen C, Xia N, Song W, Fan M, Cowling BJ. Rational use of face masks in the COVID‐19 pandemic. Lancet Respir Med. 2020;8:434‐436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kirby T. Australian government releases face masks to protect against coronavirus. Lancet Respir Med. 2020;8:239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wang MW, Zhou MY, Ji GH, et al. Mask crisis during the COVID‐19 outbreak. Eur Rev Med Pharmacol Sci. 2020;24:3397‐3399. [DOI] [PubMed] [Google Scholar]
- 4. Javid B, Weekes MP, Matheson NJ. Covid‐19: should the public wear face masks? BMJ. 2020;369:m1442. [DOI] [PubMed] [Google Scholar]
- 5. Xiao J, Shiu EYC, Gao H, et al. Nonpharmaceutical measures for pandemic influenza in nonhealthcare settings‐personal protective and environmental measures. Emerg Infect Dis. 2020;26:967‐975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Narla S, Silverberg JI. Association between atopic dermatitis and serious cutaneous, multiorgan and systemic infections in US adults. Ann Allergy Asthma Immunol. 2018;120(1):66‐72.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Juhn YJ. Risks for infection in patients with asthma (or other atopic conditions): is asthma more than a chronic airway disease? J Allergy Clin Immunol. 2014;134(2):247‐259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jartti T, Bønnelykke K, Elenius V, Feleszko W. Role of viruses in asthma. Semin Immunopathol. 2020;42:61‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Matusiak Ł, Szepietowska M, Krajewski P, Białynicki‐Birula R, Szepietowski JC. Inconveniences due to the use of face masks during the COVID‐19 pandemic: a survey study of 876 young people. Dermatol Ther. 2020;e13567. 10.1111/dth.13567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Szepietowski JC, Matusiak Ł, Szepietowska M, Krajewski PK, Białynicki‐Birula R. Face mask‐induced itch: a self‐questionnaire study of 2,315 responders during the COVID‐19 pandemic. Acta Derm Venereol. 2020;100(10):adv00152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zuo Y, Hua W, Luo Y, Li L. Skin reactions of N95 masks and medial masks among health‐care personnel: a self‐report questionnaire survey in China. Contact Dermatitis. 2020. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]


