Abstract
Historically, the prone position was used almost exclusively in the ICU for patients suffering from refractory hypoxemia due to acute respiratory distress syndrome (ARDS). Amidst the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) pandemic, however, this technique has been increasingly utilized in settings outside of the ICU, particularly in the emergency department. With emerging evidence that patients diagnosed with COVID‐19 who are not intubated and mechanically ventilated may benefit from the prone position, this strategy should not be isolated to only those with critical illness. This is a review of the pertinent physiology and evidence supporting prone positioning along with a step‐by‐step guide meant to familiarize those who are not already comfortable with the maneuver. Placing a patient in the prone position helps to improve ventilation‐perfusion matching, dorsal lung recruitment, and ultimately gas exchange. Evidence also suggests there is improved oxygenation in both mechanically ventilated patients and those who are awake and spontaneously breathing, further reinforcing the utility of the prone position in non‐ICU settings. Given present concerns about resource limitations because of the pandemic, prone positioning has especially demonstrable value as a technique to delay or even prevent intubation. Patients who are able to self‐prone should be directed into the ''swimmer's position'' and then placed in reverse Trendelenburg position if further oxygenation is needed. If a mechanically ventilated patient is to be placed in the prone position, specific precautions should be taken to ensure the patient's safety and to prevent any unwanted sequelae of prone positioning.
Keywords: ARDS, COVID‐19, emergency department, hypoxia, prone position, SARS‐CoV‐2, self proning
1. INTRODUCTION
Prone positioning has been successfully employed for refractory hypoxemia in patients with acute respiratory distress syndrome (ARDS) since the 1970s, but this maneuver has traditionally been used only inICUs. 1 As the global medical community combats the unprecedented impact of the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) virus, this paradigm is rapidly changing. 2 In strained emergency departments (EDs) and medical wards, clinicians are treating this virus with a variety of respiratory strategies not commonly deployed in the ED, including the prone position. This is especially true as prone positioning has been increasingly utilized in awake, spontaneously breathing patients. 3 , 4 Although there are growing data to support the early use of prone positioning in patients with coronavirus disease 2019 (COVID‐19), many emergency physicians may be unfamiliar with the maneuver or how to successfully utilize it. This article is intended as a primer on both the literature behind prone positioning and its safe application in EDs unaccustomed to its use.
2. PRONING PHYSIOLOGY
The mechanism underlying the beneficial effects of prone positioning has become clearer as the understanding of normal and abnormal lung physiology has evolved. While in the supine position under normal conditions, the lung parenchyma is subject to the forces of gravity and constrained by the anatomical shape of the thorax. During inspiration, recruited alveoli are inflated and gas exchange occurs. 5 The magnitude of lung ventilation is affected by the degree of inflation at both the level of the individual alveolus as well as the sum expansion of the entire lung. In the supine position, alveoli in the most dependent dorsal regions are often collapsed due to compression by overlying lung tissue. 6 Further compression of these regions occurs from weight placed on lung tissue by the heart and abdomen.
ARDS is an acute, inflammatory lung injury defined by the Berlin criteria as shown in Table 1. 7 This syndrome is known to lead to hypoxemia, diminished lung aeration, and edema. The compressive effects of supine positioning are magnified in lung tissue affected by ARDS because of this edema and the corresponding increased weight of lung parenchyma. 6 This results in less alveolar expansion in dorsal regions as compared to those in the ventral areas and subsequently less gas exchange occurs in these regions. This has been corroborated by imaging studies of patients with ARDS, which have documented dense consolidation in the dorsal lung regions when patients are supine. 6 , 8
TABLE 1.
The Berlin criteria of ARDS
| Timing | Acute onset: within 1 week of known clinical insult or new/worsening respiratory symptoms. | ||
| Chest imaging | Bilateral opacities not fully explained by effusions, lobar/lung collapse or nodules seen on chest radiograph or CT. | ||
| Etiology of edema | Not fully explained by other causes such as cardiac failure or fluid overload. | ||
|
PaO2/FiO2 (on PEEP ≥ 5 cm H2O) |
Mild ARDS 200–300 mm Hg |
Moderate ARDS 100–200 mm Hg |
Severe ARDS 100 mm Hg or less |
PEEP, positive end‐expiratory pressure; PaO2; partial pressure of arterial oxygen; FiO2, fraction of inspired oxygen; ARDS, acute respiratory distress syndrome; CT, computed tomography
Because the dorsal regions of the lung contain more lung tissue as compared to the ventral regions, prone positioning improves ventilation by allowing for a more homogenous distribution of compressional forces on alveoli thereby improving ventilation and oxygenation. 5 , 6 , 8 Perfusion in the lungs is also greater in dorsal regions compared with ventral regions even while prone, and the combination of increased recruitment in these dorsal regions with greater perfusion leads to improved ventilation‐perfusion matching and improvement in hypoxemia (Figure 1). 5 , 6 , 8
FIGURE 1.
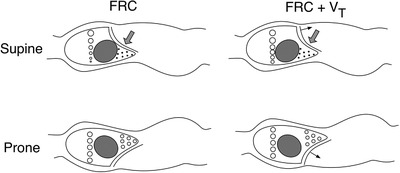
The effect of the prone position on alveolar size at functional residual capacity (FRC) and FRC plus tidal volume (VT). In the supine posture, at FRC, the most dependent alveoli are small because of higher pleural pressures, compression from the heart, and extrinsic compression from abdominal contents as compared with the prone posture. During tidal breathing, the distribution of local ventilation is more uniform in the prone posture because the alveolar volumes are more uniform at the initiation of each breath. This allows tidal volumes to be more evenly distributed throughout the lung, leading to less alveolar stress and lung injury. Figure reprinted with permission from Johnson NJ, Luks AM, Glenny RW. Gas Exchange in the prone posture. respir care. 2017 Aug;62(8):1097‐1110. PMID: 28559471
Additionally, the prone position allows for more uniform alveolar expansion, which results in more evenly distributed ventilation and perfusion and an improved distribution of tidal volumes to the lung parenchyma. 6 , 8 This more uniform expansion combined with a decrease in the areas of hyperinflation also reduces the amount of mechanical lung injury seen in supine patients. 11
3. EVIDENCE FOR PRONE POSITION
Though a number of studies have shown the benefit of the prone position as determined by physiologic parameters (mostly improvement in oxygenation), the evidence for a significant survival benefit in prone patients with ARDS remains mixed. 6 , 9 , 10 , 11 Multiple studies examining prone positioning failed to identify improved patient‐centered outcomes, though several were conducted prior to the widespread adoption of lung‐protective mechanical ventilation strategies. 6 , 9 Although some earlier trials had shown a trend toward survival benefit or statistical significance in subgroup analyses, the strongest published evidence for prone positioning in ARDS came from the landmark PROSEVA trial. 9 , 10 That study explored prone positioning in patients with moderate‐to‐severe ARDS (partial pressure of arterial oxygen/fraction of inspired oxygen [PaO2/FiO2] <150) and demonstrated a 16.8% reduction for 28‐day mortality and a 17.4% reduction for 90‐day mortality. 10 As the survival advantage of prone positioning has been most consistently identified in those with moderate to severe ARDS, the Intensive Care Society and British Thoracic Society strongly recommends its use in this patient population. 12
The use of prone positioning in awake patients has been the subject of less dedicated scholarship but recent studies have shown benefit from the maneuver. 3 , 4 , 13 In one study of awake, non‐intubated ICU patients with acute hypoxemic respiratory failure, prone positioning was performed on patients receiving varying levels of respiratory support, including high‐flow nasal cannula and non‐invasive ventilation. 13 Significant improvements in PaO2 and FaO2/FiO2 ratio were observed during prone positioning as compared to supine positioning without significant complications. In a separate study, intensivists in Jiangsu, China, noted an infrequent need for mechanical ventilation when pairing prone positioning with restrictive fluid resuscitation and non‐invasive ventilation or high‐flow nasal cannula while managing patients with COVID‐19. 4 Although the rate of critically ill patients exceeded 10%, <1% of patients required mechanical ventilation using this treatment approach. This contributes to a growing body of evidence that indicates prone positioning may help prevent the need for intubation in patients with ARDS. 3 , 4
Another recent study of 15 patients receiving non‐invasive ventilation on a general hospital ward demonstrated improvement in respiratory rate, SpO2, and PaO2/FiO2 after prone positioning was initiated. 14 The majority (73%) of patients reported improvement in comfort, and only 1 required intubation during the 14‐day follow‐up period.
Expanding the use of prone positioning in awake or intubated patients while they remain in the ED has shown promise as an early intervention for ARDS patients or those with refractory hypoxia. A recent case series in New York examined 50 adult ED patients with hypoxemia and confirmed COVID‐19. 15 Patients who remained hypoxemic despite supplemental oxygen via face mask or nasal cannula were instructed to self‐prone. Within 5 minutes of self‐proning, the median oxygen saturation of the prone patients increased from 84% to 94%. Among the self‐proned patients, a total of 18 (36%) eventually required intubation with 13 patients requiring intubation within the first 24 hours. 15
In a small pilot study, mechanically ventilated ED patients with ARDS who had a PaO2/FiO2 ratio <150 mmHg, FiO2 ≥0.6 and positive end‐expiratory pressure (PEEP) ≥5 were placed in the prone position within 24 hours of stabilization. All patients were noted to have an improvement in PaO2/FiO2 ratios and improved respiratory compliance. The maneuver was performed by a team of 5 department staff members and took less than 5 minutes to position patients. 16
Though these studies demonstrate both the feasibility and efficacy of prone positioning in the ED, it should be noted that prone patients necessitate close monitoring by staff and resources, which may not be reliably available. Although proning an intubated patient remains viable in the ED setting, this maneuver in particular should not be considered the standard of care. The decision to employ prone positioning in mechanically ventilated patients should always be guided by resource considerations, staff experience, and physician comfort with the procedure.
4. WHEN TO PRONE
As prone positioning has been primarily studied and applied in patients with ARDS, it was traditionally reserved for intubated and mechanically ventilated patients with moderate to severe disease. 6 , 8 , 9 , 10 , 17 , 18 With emerging evidence that patients diagnosed with COVID‐19 who are not intubated may benefit, this maneuver should not be isolated to only those with critical illness. 3 , 4 , 15 Although there are other disease states for which prone positioning has been used successfully, including non‐ARDS associated acute hypoxemic respiratory failure and pediatric bronchiolitis, this is significantly less studied and should not be routinely used in the ED without specialty consultation. 19 , 20
There is no general consensus on absolute contraindications to proning, but several relative contraindications and clinical scenarios should give clinicians serious pause before considering prone positioning. 21 , 22 , 23 , 24 , 25 These include:
Increased intracranial pressure
Spinal instability
Significant hemodynamic instability
Patients imminently requiring intubation
Life‐threatening dysrhythmias
Recurrent vomiting in non‐intubated patients
Recurrent seizures
In the absence of specialized beds intended to facilitate proning, morbid obesity, and second or third trimester pregnancy are relative contraindications to prone positioning. 25
5. ''HOW‐TO GUIDE'': PRONE PATIENTS AND SELF‐PRONING
For patients who can self‐prone, direct them into the swimmer's position or similar position of comfort (Figure 2). 23 , 24 , 25 The arm ipsilateral to the patient's face is raised with the shoulder in abduction between 60 and 80 degrees and the elbow flexed to approximately 90 degrees. The contralateral arm rests at the patient's side in a position of comfort, usually with a small degree of elbow flexion and palm facing upwards. Padding can be placed under the chest for comfort and to reduce pressure on the abdomen. To foster prolonged compliance with this positioning, patients may rotate to right and/or left lateral decubitus positioning as temporary respite from prone positioning rather than returning to supine. A protocol rotating between prone positioning, left lateral decubitus, right lateral decubitus, and upright sitting position has been described, with each position maintained between 30 and 120 minutes. 15
FIGURE 2.

A prone patient in the swimmer's position
For patients who cannot self‐prone, 5 or more staff members will usually be required to safely turn the patient with 2 on each side and 1 at the head of the bed. This maneuver should be practiced before implementation in your department to ensure the safety of the patient and staff members. With the necessary staff in place, the following steps should be followed 21 , 22 , 23 , 24 , 25 , 26 :
Disconnect or cap all non‐essential lines and medical devices. Remove blood pressure cuff and all anterior chest EKG leads. Secure all remaining lines, drains, and tubes as necessary. Ensure there is adequate tubing length to allow for patient repositioning. Affix any urinary catheter to the medial leg.
Place pillows or alternative padding (eg, stacked sheets or towels) on top of the patient's chest and pelvis. When the patient is prone, pressure on the abdomen should be minimized. If the patient is deeply sedated, paralyzed, or otherwise immobilized, place additional cushioning over the knees.
Drape a sheet over the top of the patient and pillows/padding, leaving the head, and neck exposed. Staff on both sides should grab the edges of this sheet and the one underneath the patient, tightly rolling the 2 together until firm against the patient's sides. Little or no slack should remain in the sheets so that the cushioning remains correctly positioned after turning.
Slide the patient to the edge of the bed away from the ventilator or source of non‐invasive ventilation while ensuring securement of an endotracheal tube if in place. Turn the patient 90 degrees so that he or she is on their side (now facing toward the ventilator/oxygen source).
While maintaining constant support of the head and neck, rotate additional 90 degrees until the patient is in a prone position with his or her face rotated toward the ventilator/oxygen source and then return the patient to the center of the bed. When available or easily fashioned, a “horseshoe” or proning pillow may be used to avoid pressure on the nose and to support endotracheal tubing (Figure 3). Such a pillow can rest atop a proning board placed under the head of the bed to allow space for lines and tubes (Figure 4).
Loosen sheets to “unwrap” the patient. Place arms in the swimmer's position as above. Alternate between left and right arm in forward position every 2 hours to minimize risk of brachial plexus injuries.
Ensure no lines or tubes were dislodged or occluded. Reconnect or uncap all lines and devices as needed. Posterior EKG leads may be placed in lieu of anterior leads that were removed (Figure 2). Place padding under forearms as needed and take care to avoid hyperextension of the ankles by placing additional support under their dorsal surface (Figure 5).
Place the bed in 5 to 10 degrees of reverse Trendelenburg angulation (head up and feet down).
FIGURE 3.

A mechanically ventilated patient on a foam proning pillow
FIGURE 4.

A proning board can be placed under the head of the bed for mechanically ventilated patients in order to better position and secure tubes and lines
FIGURE 5.

Additional padding can be placed under the anterior lower legs to prevent hyperextension of the ankles
6. PEARLS AND PITFALLS
If there is an insufficient response in oxygenation after proning, consider adding a larger degree (20 to 30 degrees or more) of vertical tilt/reverse Trendelenburg. 27 , 28 , 29 In limited studies, oxygenation has been shown to improve with the combination of both prone and upright positioning. Although proning in reverse Trendelenburg has been the subject of less‐dedicated scholarship, it is also an easily executed and low‐risk adjustment to trial. Existing research shows little or no effect on patient hemodynamics when adding this vertical tilt to the prone position.
If a patient has unilateral or asymmetric lung disease, lateral positioning (starting with the less‐diseased side down) is a reasonable alternative.
For beds likely to be used for patient proning (ie, a high acuity/resuscitation portion of the ED, ward for patients with COVID‐19, etc) consider placing a second top sheet prior to the patient using the bed. When a patient cannot self‐prone, the lower of the 2 sheets can then serve as a''slide sheet'' reducing the number of steps necessary to safely position him or her.
EDs are likely to have neither the mattresses nor headrests specific to prone positioning that might be found in ICUs or operating rooms. As such, ED staff must remain mindful of anatomic regions at greatest risk for pressure damage or nerve injury. 22 , 23 , 24 , 25 , 26 This is especially true in sedated or paralyzed patients. Specific attention should be paid to the nose and eyes, breasts, elbows/cubital tunnel, pelvis, and the dorsum of the foot. Patients with silicone breast implants may be at increased risk for breast tissue damage or necrosis in the prone position. 30
For patients who require central venous access or arterial monitoring, consider insertion sites that are less likely to occlude and will remain more accessible for medication administration or blood draws once prone. 22 , 23 , 24 , 25 A well‐secured radial arterial line may present fewer logistical challenges than one placed in the femoral artery.
Every effort should be made to place necessary central lines while the patient is supine. As patients should not be proned with significant hemodynamic instability, central access while in prone positioning should be avoided. If a prone patient requires emergent central vein cannulation, however, accessing the internal jugular vein under ultrasound guidance has been previously described. 31 , 32 From this position, the internal jugular vein will be visualized superficial to the carotid artery and the needle tip should be directed toward the vein's lateral wall.
Any patient with significant hemodynamic instability or one for whom immediate risk of cardiopulmonary arrest is high should not be placed in the prone position. If a prone patient does experience cardiac arrest, cardiopulmonary resuscitation can reasonably be initiated with compressions immediately inferior to the tip of the scapula. 33 , 34 Defibrillator pads can be placed on the left in the mid‐axillary line at approximately the level of the fifth intercostal space and on the right between the thoracic spine and the tip of the scapula. 35 , 36
Intubated and mechanically ventilated patients with moderate‐to‐severe ARDS who are being proned should also be treated with the other cornerstones of ARDS management: low tidal volume ventilation, deliberate PEEP and FIO2 titration, conservative fluid management, and deep sedation and neuromuscular blockade for refractory hypoxemia or ventilator dyssynchrony.
The transportation of a critically ill patient requiring prone positioning can help prevent delays in necessary treatment. Albeit rare, with proper equipment, preparation, and personnel it can be done safely either via ground or aeromedical transport over long distances with few or no complications. 37 , 38 , 39 , 40
Prone positioning, in the appropriate clinical context, has been shown to be a safe and efficacious maneuver. Once relegated exclusively to the ICU for those with critical illness, prone positioning can be performed in the ED for both awake, spontaneously breathing patients and those requiring mechanical ventilation. As the medical community navigates the unique challenges posed by the COVID‐19 pandemic, prone positioning represents a readily implemented and potentially beneficial treatment option for hypoxic patients in the ED.
McGurk K, Riveros T, Johnson N, Dyer S. A primer on proning in the emergency department. JACEP Open. 2020;1:1703–1708. 10.1002/emp2.12175
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
Supervising Editor: Nicholas Caputo, MD, MSc.
REFERENCES
- 1. Douglas W, Rehder K, Beynen F, et al. Improved oxygenation in patients with acute respiratory failure: the prone position. Am Rev Respir Dis. 1977;115(4):559‐566. [DOI] [PubMed] [Google Scholar]
- 2. Zhu N, Zhang D, Wang W, et al. A Novel coronavirus from patients with pneumonia in China. N Engl J Med. 2019;382(8):727‐733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ding L, Wang L, Ma W, et al. Efficacy and safety of early prone positioning combined with HFNC or NIV in moderate to severe ARDS: a multi‐center prospective cohort study. Crit Care. 2020;24(1):28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sun Q, Qin H, Huang M, et al. Lower mortality of COVID‐19 by early recognition and intervention: experience from Jiangsu Province. Ann Intensive Care. 2020;10(1):33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Johnson NJ, Luks AM, Glenny RW. Gas exchange in the prone posture. Respiratory Care. 2017;62(8):1097‐1110. [DOI] [PubMed] [Google Scholar]
- 6. Koulouras V, Papathanakos G, Papathanasiou A, et al. Efficacy of prone position in acute respiratory distress syndrome patients: a pathophysiology‐based review. World J Crit Care Med. 2016;5(2):121‐136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Force ADT, Ranieri VM, Rubenfeld GD, et al. Acute respiratory distress syndrome. JAMA. 2012;307(23):2526‐2533. [DOI] [PubMed] [Google Scholar]
- 8. Gattinoni L, Busana M, Giosa L, et al. Prone positioning in acute respiratory distress syndrome. Semin Respir Critl Care Med. 2019;40(1):94‐100. [DOI] [PubMed] [Google Scholar]
- 9. Sud S, Sud M, Friedrich JO, et al, Effect of mechanical ventilation in the prone position on clinical outcomes in patients with acute hypoxemic respiratory failure: a systematic review and meta‐analysis. CMAJ. 2008;178(9):1153‐1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. 10 Guérin C, Reignier J, Richard JC, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368:2159‐2168. [DOI] [PubMed] [Google Scholar]
- 11. Scholten EL, Beitler JR, Prisk GK, et al Treatment of ARDS with prone positioning. Chest. 2017;151(1):215‐224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Griffiths MJD, McAuley DF, Perkins GD, et al. Guidelines on the management of acute respiratory distress syndrome. BMJ Open Respir Res. 2019;6(1):e000420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Scaravilli V, Grasselli G, Castagna L, et al. Prone positioning improves oxygenation in spontaneously breathing nonintubated patients with hypoxemic acute respiratory failure: a retrospective study. J Crit Care. 2015;30:1390‐1394. [DOI] [PubMed] [Google Scholar]
- 14. Sartini C, Tresoldi M, Scarpellini P, et al. Respiratory parameters in patients with COVID‐19 after using noninvasive ventilation in the prone position outside the intensive care unit JAMA. 2020;323: e207861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Caputo ND, Strayer RJ, Levitan R. Early self‐proning in awake, non‐intubated patients in the emergency department: a single ED's experience during the COVID‐19 pandemic. Acad Emerge Med. 2020;27(5):375‐378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Vieira L, Figueiredo L, Castro J, et al. Early prone position at the emergency room in acute respiratory distress syndrome: a pilot study. [Abstract B54]. Am J Respir Criti Care Med. 2017;195:A3758. [Google Scholar]
- 17. Galiatsou E, Kostanti E, Svarna E, et al. Prone position augments recruitment and prevents alveolar overinflation in acute lung injury. Am J Respir Crit Care Med. 2006;174:187‐197. [DOI] [PubMed] [Google Scholar]
- 18. Sud S, Friedrich JO, Taccone P, et al. Prone ventilation reduces mortality in patients with acute respiratory failure and severe hypoxemia: systematic review and meta‐analysis. Intensive Care Med. 2010;36(4):585‐599. [DOI] [PubMed] [Google Scholar]
- 19. Baudin F, Emeriaud G, Essouri S, et al. Physiological effect of prone position in children with severe bronchiolitis: a randomized cross‐over study (BRONCHIO‐DV). J Pediatr. 2019;205:112‐119. [DOI] [PubMed] [Google Scholar]
- 20. Bloomfield R, Noble DW, Sudlow A. Prone position for acute respiratory failure in adults. Cochrane Database Syst Rev. 2015;2015(11):CD008095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Papazian L, Aubron C, Brochard L, et al. Formal guidelines: management of acute respiratory distress syndrome. Ann Intensive Care. 2019;9(1):69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Messerole E, Peine P, Wittkopp S, et al. The pragmatics of prone positioning. Am J Respir Crit Care Med. 2002;165:1359. [DOI] [PubMed] [Google Scholar]
- 23. Oliveira VM, Piekala DM, Deponti GN, et al. Safe prone checklist: construction and implementation of a tool for performing the prone maneuver. Rev Bras Ter Intensiva. 2017;29(2):131‐141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Knight DJW, Mahajan RP. Patient positioning in anaesthesia. BJA Educ. 2004;4:160‐163. [Google Scholar]
- 25. Guidance for Prone Positioning in Adult Critical Care . London: Intensive Care Society. 2019. https://www.ficm.ac.uk/sites/default/files/prone_position_in_adult_critical_care_2019.pdf Accessed March 28, 2020.
- 26. Kwee MM, Ho YH, Rozen WM. The prone position during surgery and its complications: a systematic review and evidence‐based guidelines. Int Surg. 2015;100(2):292‐303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Robak O, Schellongowski P, Bojic A, et al. Short‐term effects of combining upright and prone positions in patients with ARDS: a prospective randomized study. Crit Care. 2011;15(5):R230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hoste EA, Roosens CD, Bracke S, et al. Acute effects of upright position on gas exchange in patients with acute respiratory distress syndrome. J Intensive Care Med. 2005;20(1):43‐49. [DOI] [PubMed] [Google Scholar]
- 29. Richard JC, Lefebvre JC. Positioning of patients with acute respiratory distress syndrome: combining prone and upright makes sense. Crit Care. 2011;15(6):1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Burdet L, Liaudet L, Schaller M, et al. Bilateral breast necrosis after prone position ventilation. Intensive Care Med. 2001;27:1435. [DOI] [PubMed] [Google Scholar]
- 31. Sofi K, Arab S. Ultrasound‐guided central venous catheterization in prone position. Saudi J Anaesth. 2010;4(1):28‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Chen GY, Cheng KI, Hsu HT, et al, Ultrasound‐guided central venous catheterization in the prone position. Br JAnaesth. 2017;119(2):337‐338. [DOI] [PubMed] [Google Scholar]
- 33. Mazer SP, Weisfeldt M, Bai D, et al. Reverse CPR: a pilot study of CPR in the prone position. Resuscitation. 2003;57:279‐285. [DOI] [PubMed] [Google Scholar]
- 34. Kwon MJ, Kim EH, Song IK, et al. Optimizing prone cardiopulmonary resuscitation: identifying the vertebral level correlating with the largest left ventricle cross‐sectional area via computed tomography scan. Anesth Analg. 2017;124:520‐523. [DOI] [PubMed] [Google Scholar]
- 35. Link MS, Atkins DL, Passman RS, et al. Part 6: electrical therapies: automated external defibrillators, defibrillation, cardioversion, and pacing: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122‐18(Suppl 3):S706‐19. [DOI] [PubMed] [Google Scholar]
- 36. Nanjangud P, Nileshwar A. Cardiopulmonary resuscitation in adult patients in prone position. Indian J Respir Care. 2017;6:791‐792. [Google Scholar]
- 37. Hersey D, Witter T, Kovacs G, Transport of a prone position acute respiratory distress syndrome patient. Air Med J. 2018;37(3):206‐210. [DOI] [PubMed] [Google Scholar]
- 38. DellaVolpe JD, Lovett J, Martin‐Gill C, et al. Transport of mechanically ventilated patients in the prone position. Prehosp Emerge Care. 2016;20(5):643‐647. [DOI] [PubMed] [Google Scholar]
- 39. Uusaro A, Parviainen I, Takala J, et al. Safe long‐distance interhospital ground transfer of critically ill patients with acute severe unstable respiratory and circulatory failure. Intensive Care Med. 2002;28:1122‐1125. [DOI] [PubMed] [Google Scholar]
- 40. Flabrouis A, Schoettker P, Garner A. ARDS with severe hypoxia—aeromedical transportation during prone ventilation. Anaesth Intensive Care. 2003;31(6):675‐678. [DOI] [PubMed] [Google Scholar]


