Abstract
Over the last 4 months, the novel coronavirus, SARS‐CoV‐2, has caused a significant economic, political, and public health impact on a global scale. The natural history of the disease and surge in the need for invasive ventilation has required the provision of intensive care beds in London to be reallocated. NHS England have proposed the formation of a Pan‐London Emergency Cardiac surgery (PLECS) service to provide urgent and emergency cardiac surgery for the whole of London. In this initial report, we outline our experience of setting up and delivering a pan‐regional service for the delivery of urgent and emergency cardiac surgery with a focus on maintaining a COVID‐free in‐hospital environment. In doing so, we hope that other regions can use this as a starting point in developing their own region‐specific pathways if the spread of coronavirus necessitates similar measures be put in place across the United Kingdom.
Keywords: cardiac surgery, COVID‐19
1. INTRODUCTION
Over the last 4 months, the novel coronavirus, SARS‐CoV‐2, has caused a significant economic, political, and public health impact on a global scale. COVID‐19 (the clinical syndrome from the virus) has been declared as a pandemic by the World Health Organisation (WHO) and is placing an unprecedented burden on the National Health Service (NHS) of the UK and London in particular. 1 The natural history of the disease and significant requirement for invasive ventilation necessitates the reallocation of the provision of intensive care beds in London. To accommodate this, the provision of services such as cardiac surgery with its high need for intensive care beds have had to be restructured. 2 In common with all other surgical specialties, all elective cardiac surgery has been put on hold for the duration of the pandemic to focus resources on acute services. NHS England have proposed the formation of a Pan‐London Emergency Cardiac Surgery (PLECS) service to provide urgent and emergency surgery for the whole of London. After consultation with the local clinical leads at individual cardiac centers across London, a two‐unit delivery model was proposed. The two cardiac centers chosen are high volume cardiac surgery centers without on‐site Accident & Emergency (A&E) services, namely Barts Heart Center (part of the Barts Health NHS Trust) and Harefield Hospital (Royal Brompton and Harefield NHS Foundation Trust). It is proposed that these hospitals be kept at least partially COVID‐19 free to support the safe provision of emergency cardiac surgery. This protocol aims to provide clear arrangements and guidance on how the PLECS service is constructed and its operation pathways. We hope that this protocol in conjunction with key stakeholders can help other surgical departments in developing their own responses.
2. CARDIAC SURGICAL ACTIVITY IN LONDON
There are seven NHS centers that provide cardiac surgical services in London, with an additional five independent hospitals covering a population of 8.5 million. Before the COVID‐19 pandemic, approximately 7000 cardiac surgical procedures were performed on average in London every year, with the majority (90%) performed in NHS hospitals. The two centers chosen to deliver the PLECS service, Barts Heart Centre (BHC) and Harefield Hospital (HH), performed approximately 1800? and 900 procedures per year respectively. 3
Due to the impact of COVID‐19, an initial pan‐London conference call was set up on the 18 March 2020. At this point, almost all units had stopped elective cardiac surgery and were only operating on interhospital transfers for urgent cardiac surgery or emergencies. Some units had triaged “urgent from home” patients from the waiting list with life‐threatening anatomy to be offered surgery if capacity allowed. From the details discussed in the conference call, it was apparent that a pan‐London approach was not only sensible but necessary to maintain emergency cardiac surgery whilst maximizing resources for reallocation to the COVID‐19 response. Two centers (BHC and HH) were chosen based on their capacity, geographical location, and the absence of an on‐site A&E service, as it was felt that having to accommodate acute admissions via A&E would make maintaining a COVID‐free environment challenging. There was a complete agreement from all units that the PLECS pathway was necessary, logical, and should be actioned as soon as possible. A steering committee was put in place to develop a protocol for the set up and delivery of the PLECS referral pathway, led by surgeons from Barts Heart Centre. It is important to note that due to the novel challenge of providing a cardiac surgical service in the midst of a global pandemic the PLECS pathway detailed in the subsequent sections was not implemented in its entirety from the outset. Some aspects were developed over time and modifications were made to the pathway, particularly in relation to how best to maintain a COVID‐free environment. Outlined below is the final version of the pathway that incorporates these modifications.
3. CASE DEFINITION
The first duty in developing the PLECS pathway was to define the cohort of patients that would be eligible for referral and treatment. Cardiac surgical patients can be considered in a few categories depending on clinical urgency. The initial referral pathway depends on the level of urgency at the time of referral/presentation and is schematically represented in Figure 1.
Level 1 ‐ Elective—patients who have indications for routine cardiac surgery who would normally be added to an elective waiting list. Such patients under the PLECS protocol would be treated by local centers as normal and be placed on waiting lists at the local center, with the knowledge that these waiting lists could be longer than usual. Level 1 patients will not receive surgery within the PLECS pathway.
Level 2 ‐ Urgent from home—such patients are on the existing waiting lists or in the process of referral—but have critical/life‐threatening anatomy with worsening symptoms or the need for urgent prognostic intervention. Such patients will be triaged by the local centers and if appropriate passed through to the hub command center for consideration of surgical intervention should capacity allow.
Level 3 ‐ Urgent interhospital transfers—such patients are in hospital with prognostic/critical anatomy or physiology or with unstable symptoms. They require cardiac surgery within this hospital admission (but not on the same day). The PLECS pathway dictates that such patients must all be discussed in a local multi‐disciplinary team (MDT) meeting to determine whether any other options for treatment are possible such as medical or percutaneous management. If a percutaneous treatment option such as transcatheter aortic valve implantation (TAVI) or percutaneous coronary intervention (PCI) is a reasonable treatment for the patient's condition then it should be performed where possible, even if it would not be the usual recommended treatment as dictated by best evidence practice. This decision was taken with the aim of limiting the use of cardiac surgery to those patients who have no other options and minimizing the burden on intensive care capacity. If there is no nonsurgical treatment option, patients will be triaged by their local cardiac surgical center and passed through to the command center at BHC.
Level 4 ‐ Emergency (most commonly, but not exclusively, acute aortic dissections)—these patients have life‐threatening emergency cardiac conditions and require surgery within hours. Such patients can be referred either directly into one of the two delivery centers via the on‐call surgeons or via their local center. Direct referral to the delivery center would be preferred, but there must be an understanding that other hospitals (ie, noncardiac) may not be aware of the PLECS pathway, so non delivery cardiac centers may be required to help the flow of information if an emergency referral is made to a non‐delivery center initially.
Figure 1.
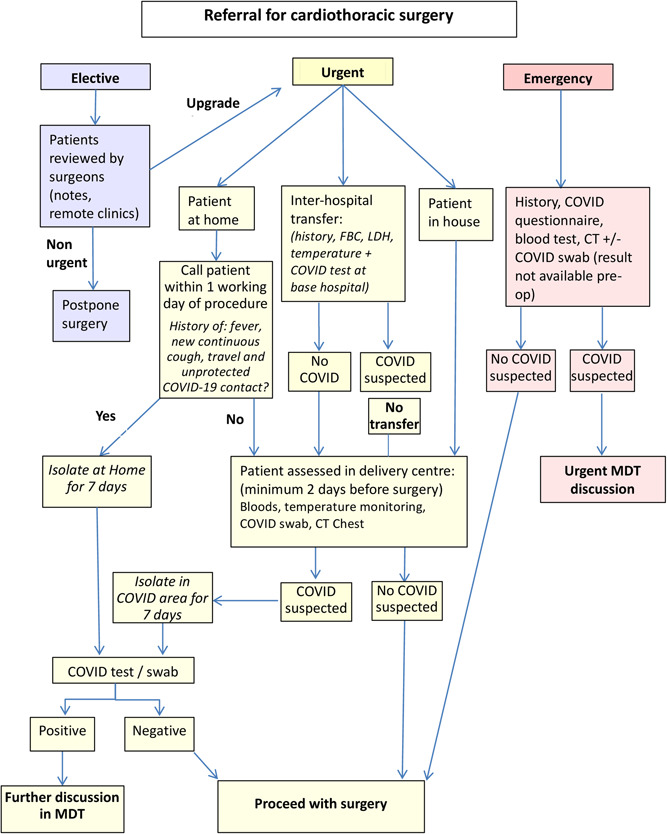
Schematic representation of PLECS referral pathways. PLECS, Pan‐London Emergency Cardiac surgery
4. PREOPERATIVE WORK UP AT LOCAL CARDIAC CENTERS
It is assumed that all nondelivery cardiac centers will have performed the basic preoperative investigations such as echocardiography and coronary imaging. Patients will not be transferred to a delivery center unless imaging has been transferred or is in the process of being transferred via the appropriate method. As such it is expected that referring centers and the delivery center will have adequate staff trained and able to facilitate the transfer of urgent image transfers.
It is accepted that some of the additional investigations routinely used to assess cardiac patients preoperatively (such as carotid doppler ultrasonography, lung function tests) will be unlikely to take place. Detailed histories and clinical examination will be essential in documenting physiological reserve and suitability for cardiac surgery.
As the local cardiac surgical center is triaging referrals for level 3 and 4 patients, it is important to have a named clinician responsible for the referral at the local center. This will allow the surgeon at the delivery center to communicate easily with the local center regarding the status of the patient.
5. MAINTAINING A COVID‐FREE ENVIRONMENT AT THE DELIVERY CENTERS
5.1. COVID‐19 swabs
All level 3 patients are required to have a COVID‐19 swab test before a referral being accepted by the delivery center. This is a critical step in the delivery centers maintaining a COVID‐free environment. If these patients return a COVID positive swab they are to remain at their local referral center until they have become COVID negative. Upon transfer to the delivery center, all patients should be swabbed on arrival and isolated inside rooms until the results are known. However, reverse transcription‐polymerase chain reaction (RT‐PCR) is not without limitations, including the availability of testing kits nationally, delays in acquiring results, and importantly the current reported high false‐negative rates. 4 As part of the PLECS pathway, all patients transferred receive another COVID‐19 swab test on arrival. Patients who test positive on arrival at the delivery center who were negative before transfer are immediately transferred to a designated COVID ‐19 area. If such patients are clinically stable, their surgery can be deferred until they have cleared the virus and returned two subsequent negative swabs. Patients who require inpatient surgery but who remain persistently COVID positive on testing but present with little or no symptoms of the disease present a management challenge. The decision to operate should be made on a case‐by‐case basis with a balance of risk between delaying surgery or operating with active COVID‐19 infection. In such cases, we recommend joint decision making utilizing a mini‐MDT comprised of a cardiac surgeon, a cardiologist, and an infectious disease consultant.
The need for emergency surgery in level 4 patients may allow insufficient time for a COVID‐19 swab to be processed. As such the PLECS pathway makes provision for level 4 patients of unknown COVID status to be admitted into an area of isolation within the delivery centers. Such patients will be treated as if they are COVID positive with full personal protective equipment (PPE) measures until such time as they are proven to be COVID negative. This includes the process of taking the patient to the theater, performing surgery, and returning them to the intensive treatment unit (ITU). If such patients subsequently diagnosed to have a positive swab, they should continue their postoperative recovery in a designated COVID ITU/ward until they have been proven to clear the virus.
Due to the high false‐negative rate of the current COVID swab in use, and the processing time of 24 hours, other investigations can provide an indication of possible COVID‐19 status. These tests are outlined below and can result in patients being considered COVID positive even in the presence of a negative swab result.
5.2. Computed topography scans
Recent studies published from Wuhan, China have suggested a pivotal role for computed tomography (CT) thorax scans in diagnosing COVID‐19 pneumonitis with a high sensitivity. 5 Due to the time constraints in level 4 patients and the current prolonged turnaround for COVID‐19 swabs results, a CT scan could prove an invaluable tool in determining the likelihood of COVID‐19. In addition, a CT scan will provide valuable information on the condition of the lung parenchyma acting as a surrogate marker of lung function in patients unable to undergo lung function tests. It should be noted however, that CT findings in patients with COVID‐19 are also seen with numerous other pathogens and as well as noninfectious pathologies. If COVID‐19 is suspected on CT (but negative on a swab), patients should be isolated with further interval COVID‐19 PCR swabs or until the isolation period has lapsed. The results of the CT scan should be used in conjunction with the overall clinical picture to determine the probability of COVID‐19 infection.
5.3. Lactate dehydrogenase/lymphocyte counts
We propose that all patients being referred via the PLECS pathway should have a lactate dehydrogenase (LDH) level and a lymphocyte count. Limited data from China and Iran suggest that high LDH levels and low lymphocyte counts predict severity and prognosis in patients with COVID‐19. 6 , 7 Whilst these blood results may not be useful in decision making in isolation when combined with other factors such as swab results, imaging of the chest and the patient's clinical condition they help to build a picture of the likelihood of COVID‐19 infection and the risk of proceeding with cardiac surgery. until further studies are performed or until other biomarkers become available. However, they should be used in conjunction with other investigations. For example, a COVID‐19 negative swab patient with positive/indeterminate CT findings and a raised LDH/low lymphocyte count may warrant further observation/isolation if not a clinical emergency.
6. OPERATIVE CONSIDERATIONS
An operative protocol was developed for patients with proven/suspected COVID‐19 with input from anesthesiology, perfusionists and scrub nurses. All stages of a patient pathway and theatre set‐up has been considered and modified to reduce the risk of transmission. Personal protective equipment (PPE) guidelines are as per Public Health England (PHE) guidelines. The principals of this pathway are to limit the number of theatre staff in contact with the patient before endotracheal intubation. Intubation is performed in theatre with a consultant anesthetist, anesthetic trainee, and operative department practitioner (ODP) wearing full PPE. Once the patient is anesthetised a 20‐minute period must pass before other theatre staff can enter the theatre and start to prepare the case. This period is to allow the air in theatre to be recycled to reduce the viral load. All theatre staff in theatre wear full PPE and remain inside the operating theatre throughout the case. This set up requires additional staff to remain outside of the theatre and bring any additional equipment that may be required. This pathway is followed by irrespective of the COVID status of the patient due to the risk of false‐negative swab results in the presence of aerosol‐generating procedures that occur during the course of cardiac surgical operation. Key details of the theatre operating pathway can be found in the Appendix. Full details of the theatre operating pathway at BHC (incorporating thoracic surgery, anesthesiology and cardiology catheter laboratories) can be found at the Society for Cardiac and Thoracic Surgery website. 8
7. OPERATIONAL MEETINGS
Close coordination between the command center and the nondelivering center will be essential. We expect continued dialog through the working day. However, two operational calls should be scheduled:
-
1.
8 am—check theatre and bed availability and plans for the current day/review any emergency referrals overnight.
-
2.
4 pm—coordination of triaged referrals and operative scheduling for the next working day.
It is anticipated there will be a weekly telephone conference with representation (clinical and managerial) from all participating sites. Daily feedback from the command center to the consultants on call at the delivery site will be expected to document a number of referrals and bed availability.
8. STAFFING CONSIDERATIONS
8.1. Staff deployment
The government has actively encouraged limiting unnecessary interactions in the workplace which includes certain staff in the healthcare system. The majority of staff without direct patient contact have been sent home with the ability to work remotely. Inevitably, frontline staff treating cardiac surgical patients may at some point expect to have to self‐isolate either as a result of themselves becoming symptomatic or inhabiting with someone who is symptomatic. As such staffing plans must inherently assume a high rate of attrition. It is envisaged that the PLECS protocol will be able to draw on a pan London pool of cardiac surgical staff including surgeons, anesthetists, nurses, and technical staff. Each unit should consider which staff would be suitable for redeployment to a delivery center if needed. For example, perfusionists, if not working in an extracorporeal membrane oxygenation delivery center, could be used to cross cover services at the two delivery centers. Consideration should also be given to any senior staff members over the age of 70 to work in roles outside the hospital to minimize their risk of contracting the virus.
The cessation of cardiac surgery in cardiac surgical centers outside the two delivery sites should enable the redeployment of staff from cardiac surgery services to help other essential services dealing with the outbreak.
8.2. The PLECS command center
The PLECS command center will be based at Barts Heart Centre staffed 24 hours, seven days a week. The command centre at BHC will coordinate the transfer of referrals to both treatment centres (BHC and HH). During main working hours (8 am‐8 pm) staffing will consist of two members of the cardiac surgery scheduling team, a senior surgical registrar/resident, and a dedicated PLECS consultant surgeon. The consultant surgeon does not necessarily have to be from the delivery center and it is possible that surgeons from other local cardiac units may be asked to cover if there is a staff shortage. Outside of normal working hours, the hub will be primarily staffed by the registrar and the on‐call consultant surgeon.
8.3. Local cardiac center
In general, the role of cardiac surgical staff at local cardiac surgical hospitals will be determined by local policies. If surgeons are required from local cardiac units at the delivery center, then fast‐tracking of honorary contracts and induction arrangements will be necessary.
9. DISCHARGE PLANNING AND REPATRIATION
Flow‐through the delivery centers will be paramount to allow the pathway to function. Wherever possible, a preplan to discharge patients home from the delivery center will be followed. However, in the event of the need for prolonged hospitalization following surgery, repatriation to the local cardiac surgery unit may be required. This would be decided on a case by case basis. All options for ongoing care for patients not able to be discharged will be explored, including step down to the private sector.
10. CLINICS AND TELEMEDICINE
Before the COVID‐19 pandemic a small portion of all outpatient clinic appointments for postoperative patients at BHC was performed in “virtual clinics” using online video conferencing apps. Given the current pandemic, all face‐to‐face clinic visits have been canceled and replaced with virtual or telephone clinics at the local cardiac center. Concerns regarding medical access with telemedicine have limited its expansion, but there have been several instances (for example during the H1N1 pandemic) where unnecessary clinic visits were reduced via a telephone triage system without reducing medical access. 9
All follow‐up clinic patients should be contacted a week in advance of their appointment and triaged to determine whether they need to be seen physically or are in need of clinical tests (ECG, bloods, echocardiogram, CT). This triage tool can also be used to screen for COVID‐19 symptoms and patients can be directed to their nearest facility. At BHC, we have rapidly deployed remote IT access for surgeons scheduled for follow‐up clinics. This has allowed virtual follow‐up clinics to be performed at home (with full access to imaging, operation notes, etc) and avoid unnecessary clinician visits to the hospital.
New patient clinics are being performed physically and virtually depending on clinical urgency. All patients are triaged by telephone consultation before the visit and COVID‐19 screening questionnaires performed. These new referrals should ideally be limited to level 2 patients as assessed by the local cardiac unit. If urgent surgery is deemed necessary, such patients are seen physically and referred to the delivery center for consideration of surgical intervention. Routine review of the new level 1 patient should be deferred until the peak of the pandemic has passed.
11. INDEPENDENT SECTOR SUPPORT
The Independent Sector cardiac surgery providers are in discussion with NHS England about how they can support urgent cardiac surgery provision in the capital incorporating an appropriate governance structure. It is likely that the independent sector will be asked to support patient flow and ongoing hospital treatment for patients after cardiac surgery who cannot be discharged from a delivery center. It is also possible that independent hospitals could deliver some level 3 and level 2 operations where capacity allows. These patients would be triaged and processed through the command center, to ensure the most urgent in‐hospital patients are treated quickly and that capacity is optimized. The Independent Sector support will have representatives on the weekly interhospital meeting. At the time of writing, the independent sector is not taking an active role in the delivery of the PLECS pathway.
12. GOING FORWARD
The COVID‐19 pandemic is causing a paradigm shift in the way we practice cardiac surgery. The nature of our specialty mandates the use of the very precious resources that are required to combat this unprecedented pandemic. This protocol is an initial pathway aimed at delivering safe care for patients with an urgent need for cardiac surgery without compromising on healthcare resources. Due to the lack of precedent in the current pandemic, the majority of the measures proposed are based on limited, sometimes anecdotal evidence. As such, the protocol will be continually reviewed and updated as our understanding of the disease process improves, and our experience of operating in these challenging circumstances increases.
Many questions remain unanswered as to how to optimize outcomes for patients presenting with heart disease in the midst of the pandemic. It is not yet clear who should be offered surgery and who would be better served with watchful waiting. Work is ongoing regarding how to optimize cardiac surgical patients to prevent the development of COVID‐19 in the postoperative period and outcome data is being collected on all operated and nonoperated patients referred via the PLECS pathway. It is hoped that analysis of this data over time will allow a picture to emerge of who should be offered surgical treatment, at what time points, and how best to minimize the risk of concomitant COVID infection. It is imperative that we are meticulous in this process during this pandemic, as it is likely that COVID‐19 as a disease process will persist for many years to come.
13. SUMMARY
In the spread of coronavirus, London has so far borne the brunt of cases and mortality. However, as the pandemic spreads through the population we can expect that centers around the UK will be similarly affected. In this initial report, we outline our experience of setting up and delivering a pan‐regional service for the delivery of urgent and emergency cardiac surgery with a focus on maintaining a COVID‐free in‐hospital environment. In doing so, we hope that other regions can use this a starting point in developing their own region‐specific pathways if the spread of coronavirus necessitates similar measures be put in place across the United Kingdom.
BSC GROUP
The following are members of BSC (Bart's Surgical Consortium): Stephen Edmondson (Clinical Director for Surgery), Kulvinder Lall (Clinical Lead), Aung Oo, Neil Roberts, David Lawrence, Rakesh Uppal, John Yap, Kit Wong, Alex Shipolini, Shirish Ambekar, Carmelo Di Salvo, Amir Sheikh, Wael Awad, Shyamsunder Kolvekar and Benjamin Adams.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
Contributors and sources: All authors conceived the study together; SE is the clinical director of surgery at St Bartholomew's Hospital. KL is the clinical lead for cardiac surgery at St Bartholomew's Hospital. CR is the anesthetic lead and JL is the microbiologly lead. AH, DB, MY, ALM are the senior cardiothoracic registrars and prepared the initial draft and collated the information. All members of the BSC contributed to the subsequent revision and final approval of the present manuscript. AH is the guarantor of the paper. All sources are referenced.
PATIENT INVOLVEMENT
No patients were involved in this analysis.
Supporting information
Supporting information
ACKNOWLEDGMENTS
We would like to thank our surgical colleagues from the London Cardiac centers (King's College Hospital, Hammersmith Hospital, St Thomas's Hospital, St Georges Hospital, Royal Brompton and Harefield Hospital) for their cooperation and help in ensuring this protocol could be implemented in a timely manner.
Hussain A, Balmforth D, Yates M, et al. The Pan London Emergency Cardiac Surgery service: Coordinating a response to the COVID‐19 pandemic. J Card Surg. 2020;35:1563–1569. 10.1111/jocs.14747
REFERENCES
- 1. World Health Organization . WHO announces COVID‐19 outbreak a pandemic. World Health Organ. 2020;3 http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic [Google Scholar]
- 2. NHS England . Next Step on NHS Response to COVID‐19 . 2020. https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/urgent-next-steps-on-nhs-response-to-covid-19-letter-simon-stevens.pdf. Accessed 23 April 2020.
- 3. Society for Cardiothoracic surgery . UK Cardiothoracic Units & Outcomes . 2020. http://scts.org/hospitals/cardiac/. Accessed 24 April 2020.
- 4. Li Y, Yao L, Li J, et al. Stability issues of RT‐PCR testing of SARS‐CoV‐2 for hospitalized patients clinically diagnosed with COVID‐19. J Med Virol. 2020;1–6. 10.1002/jmv.25786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hope MD, Raptis CA, Shah A, Hammer MM, Henry TS. A role for CT in COVID‐19? What data really tell us so far. Lancet. 2020;395(10231):1189–1190. 10.1016/s0140-6736(20)30728-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mardani R, Ahmadi Vasmehjani A, Zali F, et al. Laboratory parameters in detection of COVID‐19 patients with positive RT‐PCR: a diagnostic accuracy study. Arch Acad Emerg Med. 2020;8(1):e43 10.1101/2020.03.24.20040162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tan L, Wang Q, Zhang D, et al. Lymphopenia predicts disease severity of COVID‐19: a descriptive and predictive study. Signal Transduct Target Ther. 2020;5:61 10.1038/s41392-020-0148-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. SCTS . St Bartholomew's Hospital Theatre Standard Operating Protocol for COVID‐19 . 2020. https://scts.org/wp-content/uploads/2020/04/St-Bartholomews-Theatre-SOP-for-COVID-19-8th-April-2020.pdf. Accessed 23 April 2020.
- 9. North F, Varkey P, Bartel GA, Cox DL, Jensen PL, Stroebel RJ. Can an office practice telephonic response meet the needs of a pandemic? Telemed e‐Health. 2010;16:1012 10.1089/tmj.2010.0102 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information


