Abstract
Objective
To retrospectively review the impact of the outbreak of coronavirus disease 2019 (COVID-19) on services in the oral emergency room.
Materials and methods
A statistical analysis of epidemiological characteristics and the patients’ diagnoses and treatments in the Emergency Department of Peking University Hospital of Stomatology during the outbreak of COVID-19 in 2020 compared with those in 2019 in Beijing, China.
Results
There were fewer total visits in 2020 than in 2019 (P = 0.001), and the proportions of patients who were children, adolescents and elderly people were lower in 2020 than in 2019 (P < 0.001). The proportions of patients with acute toothache and infections were higher in 2020 than in 2019, and the proportions of patients with maxillofacial trauma and non-emergencies were lower in 2020 than in 2019 (P < 0.001). Drug treatment for acute pulpitis was used more often in 2020 than in 2019, and endodontic treatment and examination consultations were less common in 2020 than in 2019 (P = 0.022).
Conclusions
The outbreak of COVID-19 affected the patient population and structure of disease types and oral services in the emergency room. The number of visits to the oral emergency room and the proportions of the patients who were children, adolescents and elderly people were reduced, meanwhile the percentage of emergency cases, except trauma, and conservative treatments increased during the outbreak of COVID-19.
Key words: COVID-19, Oral, Emergency
Introduction
Since the outbreak of coronavirus disease 2019 (COVID-19) in December 2019, the epidemic has rapidly spread across China and many other countries. The numbers of diagnosed cases, suspected cases and deaths have continued to rise, and the general population is susceptible.1,2 The common transmission routes of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) include direct transmission (coughing, sneezing and inhalation of respiratory secretion droplets) and contact transmission (contact with oral, nasal and eye mucous membranes).3 The pathogenic microorganisms could be transmitted in dental settings through the inhalation of airborne microorganisms that can remain suspended in the air for long periods2,4; contact with nasal or oral mucosa and the droplets and aerosols containing the microorganisms5,6 generated by an infected individual, and propelled a short distance by talking or while performing an oral examination without a mask5,7; and indirect contact with contaminated instruments and/or surfaces in the examination room environment.8 Infections could be transmitted via any of these routes by an infected individual, even by asymptomatic patients in dental clinics and hospitals,9 especially during the COVID-19 outbreak.10 There is also a possibility for aerosol transmission in a relatively closed environment in which there is exposure to high concentrations of aerosols.2 A large amount of water mist, droplets and aerosols are generated during oral treatment,5 and close proximity to patients is unavoidable for dental professionals during the diagnosis and treatment process. Cross-infection is highly likely if there is an infected patient who is in the latent period or the asymptomatic period, and if that patient undergoes any treatment that involves spraying water.2,6
The Spring Festival is a traditional Chinese holiday, and it is a public holiday that is celebrated throughout the country. Usually, most urgent dental patients have to receive services from the oral emergency room during the Spring Festival because dental departments in hospitals and private dental clinics are closed. The Emergency Department of Peking University Hospital of Stomatology, one of the two public oral emergency rooms in Beijing city, has been operating 24 hours a day ever since its establishment in 1998, mainly for patients with oral emergencies; the hospital maintains this mode of operation even during the Spring Festival. In 2020, the Spring Festival holidays started on 24 January and ended on 2 February; the Chinese government began to take proactive national public health measures to combat COVID-19 on 20 January 2020.2
We retrospectively reviewed the files of the patients seen in the oral emergency room during the Spring Festival, eliminating the confounding impact of the availability of other dental clinic services, to determine the exact impact of COVID-19 on oral emergency services.
Materials and methods
Medical records were collected for the patients who visited the Emergency Department of Peking University Hospital of Stomatology during the statutory holiday period of the Spring Festival in China between 24 January 2020 and 2 February 2020 (Chinese Lunar New Year Eve to the ninth day of the first month in the Chinese lunar calendar), and the period between 4 February 2019 and 10 February 2019 (Chinese Lunar New Year Eve to the sixth day of the first month in the Chinese lunar calendar); the data collected included age, sex, diagnosis of the oral emergency, and emergency treatment methods. The study was approved by the Ethics Committee, and was conducted under the guidance of international ethical standards.
SPSS 20.0 was used for the statistical analysis.
Results
General information
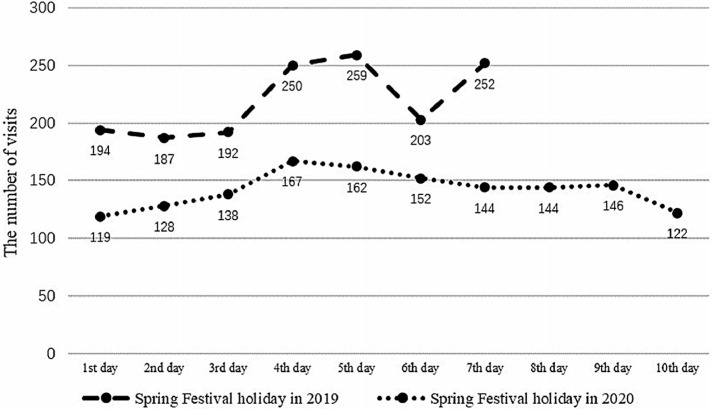
The Spring Festival lasted 10 days in 2020 (the government extended the holiday due to the COVID-19 epidemic), whereas it lasted 7 days in 2019. A total of 1,422 patients visited the Emergency Department of Peking University Hospital of Stomatology during the Spring Festival holiday in 2020, with a median of 144 patients per day (Figure 1). Of all the patients who visited the department, 775 were males and 647 were females, with a male to female ratio of 1.2:1. The youngest patient was 13 months old, and the oldest was 93 years old, with a median age of 42 years (Table 1). There were 1,537 patients who visited the department during the Spring Festival holiday in 2019, with a median of 203 patients per day (Figure 1). Of these, 742 were males and 795 were females, with a male to female ratio of 0.93:1. The youngest patient was 4 months old, and the oldest was 95 years old, with a median age of 40 years (Table 1). There were significantly fewer visits in 2020 than in 2019 (Mann–Whitney non-parametric test, Z = –3.419, P = 0.001). The proportions of the patients who were children and adolescents under 18 years of age and elderly patients over 65 years of age were significantly lower during the Spring Festival in 2020 than in 2019 (Pearson chi-square test, χ2 = 25.562, P < 0.001).
Fig. 1.
Comparison of the number of visits to the emergency department during the Spring Festival holidays in 2019 and 2020.
Table 1.
Comparison of the age of visits to the emergency department during the Spring Festival holidays in 2019 and 2020
| Age groups | 2019 Person-time (ratio, %) | 2020 Person-time (ratio, %) |
|---|---|---|
| <18 years old | 285 (18.5) | 185 (13.0) |
| 18–65 years old | 1,017 (66.2) | 1,059 (74.5) |
| >65 years old | 235 (15.3) | 178 (12.5) |
| Total | 1,537 (100.0) | 1,422 (100.0) |
Disease profile
The most common emergency problems among patients during the Spring Festival holidays in 2020 and 2019 were acute toothache, infections, and oral and maxillofacial trauma (including dental trauma, soft tissue injury and jaw fracture; Table 2). The proportions of patients with acute toothaches and infections were significantly higher in 2020 than in 2019, and the proportions of patients with oral and maxillofacial trauma and non-urgent issues were significantly lower in 2020 than in 2019 (Pearson chi-square test, χ2 = 48.888, P < 0.001). The most common diseases were acute pulpitis, abscess and acute periapical periodontitis. The incidences of those conditions were 24.5% (348/1,422), 12.9% (184/1,422) and 11.1% (158/1,422) in 2020, and 18.1% (278/1,537), 9.6% (147/1,537) and 9.3% (143/1,537) in 2019, respectively. The percentages of patients with acute pulpitis, abscess and acute periapical periodontitis were significantly higher in 2020 than in 2019 (Pearson chi-square test, χ2 = 41.325, P < 0.001).
Table 2.
Distribution of disease type and diagnosis in the emergency department during the Spring Festival holidays in 2020
| Disease type | Diagnosis | Person-time (2019) | Total person-time | Person-time (2020) | Total person-time |
|---|---|---|---|---|---|
| Acute toothache | Acute pulpitis | 278 (18.09%) | 628 (40.86%) | 348 (24.50%) | 646 (45.40%) |
| Acute periapical periodontitis | 143 (9.30%) | 158 (11.10%) | |||
| Combined periodontic-endodontic lesion | 36 (2.34%) | 46 (3.20%) | |||
| Periodontitis | 75 (4.88%) | 62 (4.40%) | |||
| Others* | 96 (6.25%) | 32 (2.30%) | |||
| Maxillofacial and dental trauma | Dental trauma | 117 (7.61%) | 201 (13.08%) | 105 (7.40%) | 176 (12.40%) |
| Soft tissue injury | 82 (5.34%) | 67 (4.70%) | |||
| Jaw fracture | 2 (0.13%) | 4 (0.30%) | |||
| Infections | Abscess | 147 (9.56%) | 313 (20.36%) | 184 (12.90%) | 335 (23.60%) |
| Pericoronitis | 96 (6.25%) | 96 (6.80%) | |||
| Maxillofacial space infection | 56 (3.64%) | 41 (2.90%) | |||
| Others† | 14 (0.91%) | 14 (1.00%) | |||
| Postoperative response and return visit | Postoperative response‡ | 61 (3.97%) | 141 (9.17%) | 54 (3.80%) | 137 (9.60%) |
| Return visit§ | 80 (5.20%) | 83 (5.80%) | |||
| Other emergency disease | Temporomandibular joint emergency¶ | 14 (0.91%) | 117 (7.61%) | 20 (1.40%) | 81 (5.70%) |
| Active bleeding | 18 (1.17%) | 8 (0.60%) | |||
| Oral mucosa emergency⁎⁎ | 31 (2.02%) | 29 (2.00%) | |||
| Maxillofacial emergency†† | 1 (0.07%) | 1 (0.10%) | |||
| Endodontic emergency‡‡ | 47 (3.06%) | 21 (1.50%) | |||
| Implant emergency§§ | – | 1 (0.10%) | |||
| Orthodontic emergency¶¶ | 5 (0.33%) | 1 (0.10%) | |||
| Prosthodontic emergency⁎⁎⁎ | 1 (0.07%) | - | |||
| Non-urgent††† | Caries, retention of primary teeth, residual crown, residual root, etc. | 137 (8.91%) | 137 (8.91%) | 47 (3.30%) | 47 (3.30%) |
| Total | 1537 (100.00%) | 1537 (100.00%) | 1422 (100.00%) | 1422 (100.00%) |
Non-odontogenic toothache, toothache waiting for investigation, etc.
Parotitis, infection of jaw cyst, lithiasis of submaxillary gland duct, etc.
Postoperative pain of root canal treatment, tooth extraction and implantation, etc.
Remove sutures and dental splint, etc.
Dislocation of temporomandibular joint.
Traumatic ulcer, herpetic stomatitis, etc.
Trigeminal neuralgia, etc.
Temporary restoration needed, root fracture, etc.
Healing abutment loosening.
Detachment of orthodontic arch wire, etc.
Crown loose.
Caries, retention of primary teeth, residual crown, residual root, etc.
Treatments for common emergency conditions
Table 3 shows the emergency treatments for acute pulpitis, acute periapical periodontitis and abscess during the Spring Festival holidays in 2020 and 2019. The percentage of patients receiving drug treatment for acute pulpitis in 2020 was significantly higher than that in 2019, while the proportions of patients receiving endodontic treatment and consultations in 2020 were significantly lower than those in 2019. There were no significant differences in the treatment of acute periapical periodontitis and abscesses in 2020 versus 2019 (Table 3).
Table 3.
Comparison of the treatment of common oral emergencies during the Spring Festival holidays in 2019 and 2020
| Diagnosis | Treatment | 2019 (person-time, %) | 2020 (person-time, %) | χ2-value | P-value |
|---|---|---|---|---|---|
| Acute pulpitis | Endodontic treatment | 119 (42.8) | 125 (35.9) | 9.636 | 0.022 |
| Endodontic treatment + drug* | 13 (4.7) | 17 (4.9) | |||
| Drug* | 75 (27.0) | 134 (38.5) | |||
| Examination and consultation | 71 (25.5) | 72 (20.7) | |||
| Total | 278 (100.0) | 348 (100.0) | |||
| Acute periapical periodontitis | Endodontic treatment | 41 (28.7) | 35 (22.2) | 4.990 | 0.173 |
| Endodontic treatment + drug† | 10 (7.0) | 20 (12.7) | |||
| Drug† | 47 (32.9) | 61 (38.6) | |||
| Examination and consultation | 45 (31.5) | 42 (26.6) | |||
| Total | 143 (100.0) | 158 (100.0) | |||
| Abscess | Incision and drainage | 98 (66.7) | 112 (60.9) | 5.286 | 0.152 |
| Incision and drainage + drug† | 31 (21.1) | 55 (29.9) | |||
| Drug† | 10 (6.8) | 13 (7.1) | |||
| Examination and consultation | 8 (5.4) | 4 (2.2) | |||
| Total | 147 (100.0) | 184 (100.0) |
Pain-control drugs.
Anti-inflammatories/antibiotics.
Discussion
The number of visits to the oral emergency room during the Spring Festival holiday was lower in 2020 than in 2019, although the statutory holiday for the Spring Festival in 2020 was extended to 10 days. COVID-19 was categorised as a Class B infectious disease in China, and the management measures for Class A infectious diseases were implemented by the Chinese government on 20 January 20202. This initiated a series of prevention and control measures, such as limitations on outdoor activities, and the suspension of businesses and classes. These measures, which were taken to reduce population migration during the Spring Festival and thereby control the COVID-19 epidemic, might be the main reasons for the decrease in the number of patients being seen for oral emergencies. In addition, similar to SARS, as the number of diagnosed cases with pneumonia increased during the initial outbreak, the number of dental patients decreased.11 In this study, the proportions of patients who were children and adolescents and elderly people over 65 years of age were lower in 2020 than in 2019. This finding may be because children, adolescents and elderly people are susceptible to various contagious respiratory diseases, which is a cause of concern for those visiting the stomatology hospital due to the possibility of being infected on the way or in the hospital. Based on the current cases of COVID-19, the prognosis of elderly patients and patients with chronic underlying disease is poor.2 Such patients engage in fewer visits during an outbreak. Most people have limited their outdoor activities during the outbreak due to concerns about being infected, and some of those who would normally visit the oral emergency room, such as those seeking pain relief, instead obtain drugs from drug stores, primary medical care institutions or other outpatient clinics in the general hospital.
The percentage of emergency cases in 2020 was significantly higher than that in 2019, and the percentage of non-urgent cases was significantly lower than that in 2019. Some patients with non-urgent oral conditions might decide to temporarily avoid visiting the dentist due to the COVID-19 epidemic. In the past, some non-urgent patients visited the emergency room because the cost of emergency treatment was the same as that of treatment in outpatient departments in public hospitals, but registration was easier,12 while others came to the emergency room due to an urgent need for treatment, such as the need to extract primary teeth.13
The most common types of oral emergency conditions in this study were acute toothache, infections and maxillofacial trauma, and the most common diagnoses were acute pulpitis, abscesses and acute periapical periodontitis, which were similar to the results of previous studies.14, 15, 16 The percentages of patients with acute toothaches and infections were higher in 2020 than in 2019, while the percentage of patients with maxillofacial trauma was lower in 2020 than in 2019. This might be due to the government's implementation of prevention and control measures, such as a limitation on traffic during the epidemic, which decreased engagement in outdoor activities, various sports and group activities during the Spring Festival, including visits to hospitals for non-urgent reasons. In addition, the decrease in the use of various forms of transportation might have reduced traffic accidents, including those resulting in oral and maxillofacial damage.
In this study, drug treatment for acute pulpitis was used more often in 2020 than in 2019, and there were fewer endodontic treatment and examination consultations in 2020 than in 2019. Pulpectomy is the most commonly used treatment in emergency dental care,16 and it can effectively alleviate the symptoms of acute pulpitis. SARS-CoV-2 is extremely infectious, and patients with asymptomatic infections can also become sources of infection. There is a strong potential for the transmission of the virus in a relatively closed environment, and the virus can be transmitted through high concentrations in aerosols2; these transmission conditions are met during pulpectomy. The percentage of patients undergoing pulpectomy decreased significantly from 2019 to 2020, which might be due to fear on the parts of both the patients and the dentists regarding the spread of COVID-19.17 Therefore, pain-control drugs were selected as an alternative treatment.
Only examinations and consultations were performed for a considerable number of patients with acute pulpitis and acute periapical periodontitis in this study. There have been two causes for this suggested by previous research18: first, the patient's main complaint was inconsistent with the symptoms, and no emergency treatment was needed; and second, no other regimen was available to the dentist or the dentist was unable to address the emergency condition. However, it is believed in this study that antibiotics and drugs for pain control might be routinely administered to some patients. These drugs might be used to relieve the symptoms and, therefore, only examinations and consultations were performed for those patients. Some patients chose the other options due to the cost to reimbursement ratio based on medical insurance for treatment in a specialised hospital or the lack of confidence in emergency treatment, leading to the preference for treatment in other hospitals or other professional departments in dental hospitals. As shown in this study, the decrease in the percentage of patients with acute pulpitis undergoing examinations and consultations from 2019 to 2020 may be related to the decrease in the number of outpatient registrations in public hospitals during the epidemic, the suspension of the operation of private clinics, and the narrowing of patient treatment options.
Conclusions
The spread of the COVID-19 epidemic affected the patient population and structure of disease types and oral services. The number of visits to the oral emergency room and the proportions of patients who were children, adolescents and elderly people reduced, meanwhile the percentage of emergency cases, except trauma, and the conservative treatments increased during the outbreak of COVID-19.
Funding
This study was supported by National Natural Science Foundation of China, (Grant Number 81502652).
Authors' contributions
Jie Bai and Tao Xu conceived and designed the study. Jie Bai, Tao Xu and Wei Sun collected and analysed the data. Jie Bai and Tao Xu wrote the paper. Jie Bai, Tao Xu, Ming-Wei Huang and Ai-Ping Ji reviewed and edited the manuscript. Jie Bai and Tao Xu contributed equally to the study, and are co-first authors. All authors read and approved the manuscript.
Conflict of interest
The authors have no conflict of interest in relation to this work.
Footnotes
Jie Bai and Tao Xu are joint first authors, and they contributed equally to this work.
REFERENCES
- 1.National Health Commission of the People's Republic of China. Epidemic Bulletin. Available from: http://www.nhc.gov.cn/xcs/yqtb/list_gzbd.shtml. Accessed 30 March 2020.
- 2.General Office of National Health Commission of the People's Republic of China and General Office of National Administration of Traditional Chinese Medicine. Notice on Issuance of Diagnosis and Treatment Regimen for Novel Coronavirus Pneumonia (Pilot, Version 7). Available from: http://www.gov.cn/zhengce/zhengceku/2020-03/04/content_5486705.htm. Accessed 30 March 2020.
- 3.Lu C-W, Liu X-F, Jia Z-F. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. 2020;395 doi: 10.1016/S0140-6736(20)30313-5. e39-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kampf G, Todt D, Pfaender S, et al. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infec. 2020;104:246–251. doi: 10.1016/j.jhin.2020.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harrel SK, Molinari J. Aerosols and splatter in dentistry: a brief review of the literature and infection control implications. J Am Dent Assoc. 2004;135:429–437. doi: 10.14219/jada.archive.2004.0207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Day CJ, Sandy JR, Ireland AJ. Vol. 33. 2006. p. 601. (Aerosols and splatter in dentistry – a neglected menace? Dental Update). [DOI] [PubMed] [Google Scholar]
- 7.Cleveland JL, Gray SK, Harte JA, et al. Transmission of blood-borne pathogens in US dental health care settings: 2016 update. J Am Dent Assoc. 2016;147:729–738. doi: 10.1016/j.adaj.2016.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu L, Wei Q, Alvarez X, et al. Epithelial cells lining salivary gland ducts are early target cells of severe acute respiratory syndrome coronavirus infection in the upper respiratory tracts of rhesus macaques. J Virol. 2011;85:4025–4030. doi: 10.1128/JVI.02292-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hoelscher M, Guggemos W, Vollmar P, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382:970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peng X, Xu X, Li Y, et al. Transmission routes of 2019-nCoV and controls in dental practice Int. J Oral Sci. 2020;12:1–6. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Samaranyake LP, Smales FC. Maintaining dental education and specialist dental care during an outbreak of a new coronavirus infection. Part 1: a deadly viral epidemic begins. Br Dent J. 2003;195:557–561. doi: 10.1038/sj.bdj.4810723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shqair AQ, Gomes GB, Oliveira A, et al. Dental emergencies in a university pediatric dentistry clinic: a retrospective study. Braz Oral Res. 2012;26:50–56. doi: 10.1590/s1806-83242012000100009. [DOI] [PubMed] [Google Scholar]
- 13.Xia B, Ge LH, Wang ZG, et al. Conditions analysis for 256 children patients in emergency Department of Peking University Hospital of Stomatology. J Modern Stomatol. 2006;20:214–215. [Google Scholar]
- 14.Tramini P, Al Qadi Nassar B, Valcarcel J, et al. Factors associated with the use of emergency dental care facilities in a French public hospital. Spec Care Dentist. 2010;30:66–71. doi: 10.1111/j.1754-4505.2009.00125.x. [DOI] [PubMed] [Google Scholar]
- 15.Huang J-Y, Yu H-C, Chen Y-T, et al. Analysis of emergency dental revisits in Taiwan (1999–2012) from Taiwanese National Health Insurance Research Database (NHIRD) J Dent Sci. 2019;14:395–400. doi: 10.1016/j.jds.2019.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Farmakis ETR, Palamidakis FD, Skondra FG, et al. Emergency care provided in a Greek dental school and analysis of the patients’ demographic characteristics: a prospective study. Int Dent J. 2016;66:280–286. doi: 10.1111/idj.12245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xiang Y-T, Yang Y, Li W, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marshman Z, Broomhead T, Rodd HD, et al. Who attends a Children's Hospital Emergency Department for dental reasons? A two-step cluster analysis approach. Community Dent Oral Epidemiol. 2017;45:49–58. doi: 10.1111/cdoe.12258. [DOI] [PubMed] [Google Scholar]