Editor
An optimized workflow is mandatory to restore surgical care to the population in the ‘new-normal’ of COVID-19 pandemic1–3. Our hospital was the largest tertiary centre in Beijing that continued to provide full-ranged surgical care from January 26 through April 29. We have received 99 809 surgical outpatients and 4376 emergencies, and 5378 surgeries have been performed. We herein introduce our modified workflow based on gateway screening, fever clinic and observational ward (Fig. 1).
Fig. 1.
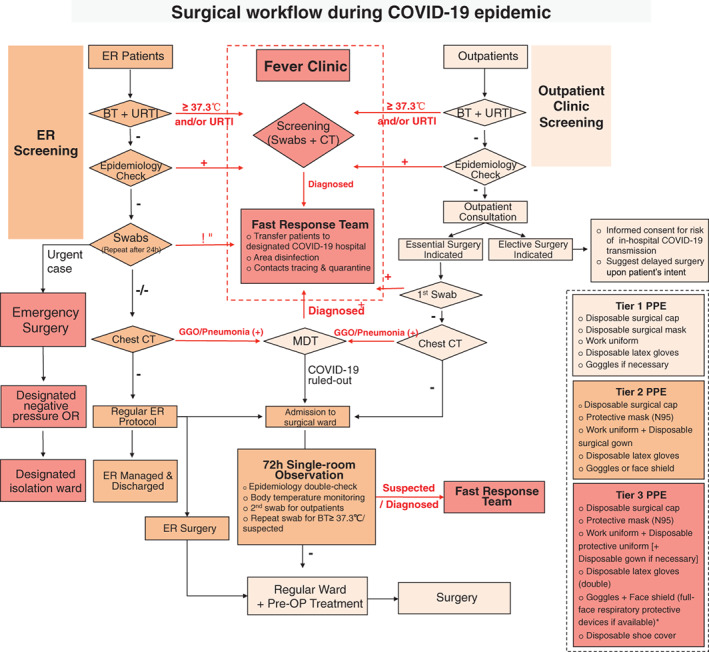
Surgical workflow during COVID-19 epidemic. ER- emergency room; BT- body temperature; URTI- upper respiratory tract infection; CT- computed tomography; MDT- multiple disciplinary team involving initial consulting surgeon, fever clinic expert and physician of respiratory diseases; PPE- personal protective equipment; OP- operation; *- There could be some disagreement about the choice of respiratory protection—N95 respirator or powered air purifying respirator (PAPR) in Tier 3 PPE. (The patients screening criteria primarily included high body temperature, upper respiratory tract infection (URTI) symptoms, clustering occurrences, contact with suspected/confirmed COVID-19 patients and/or travel history to a severe epidemic area)
Patients were interviewed by a triage nurse in PPE at a designated zone outside the emergency and outpatient entrance. This screening helped keep potential COVID-19 patients out of the main areas of the hospital.
Patients with risk factor or possible pneumonia on chest CT were transferred to the fever clinic that was established for febrile outpatients since the SARS outbreak in 2003. It is isolated from the heavy-traffic zone of the hospital. In this pandemic, the fever clinic was transformed into a makeshift fully fledged centre with a screening clinic, an isolation ward and two negative-pressure operating rooms for emergency surgery of suspect patients. Patients with risk factors for COVID-19 were screened and swabbed in the fever clinic and waited in single isolation rooms for the results. They were transferred to a designated hospital for COVID-19 if positive.
Patients with essential elective surgical indications who pass the screening are admitted to hospital. They stay first in an observational single room for 72 hours with no contact, body temperature monitoring, and symptoms and epidemiology checks. This waiting period helps identify any potential incubational patients that may slip through screening. A fast-response team will be on-call for re-swabbing and to take over the patient-transfer as well as ward disinfection and quarantine upon viral confirmation. After an uneventful observation, patients move to a regular room for perioperative care.
Acknowledgement
The authors thank all professionals from the Departments of Hepatobiliary Surgery, General Surgery, Emergency, Fever Clinic, Respiratory Medicine, Infection Management & Disease Control and Operating & Anesthesia Center who were involved in the diagnosis and surgical management of patients at the frontline. The authors thank Mr. Douglas Corley for his language editing to this paper.
REFERENCE
- 1. Brindle M, Gawande A. Managing COVID-19 in Surgical Systems. Ann Surg 2020; doi: 10.1097/SLA.0000000000003923 [Epub before print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. China National Health Commission . Diagnosis and treatment of novel coronavirus pneumonia (7th trial version). http://www.kankyokansen.org/uploads/uploads/files/jsipc/protocol_V7.pdf.
- 3. World Health Organisation . Coronavirus disease (COVID-2019) situation reports-100 (4/29/2020). www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.


