Over 300 health and social care staff died in the UK during the first COVID‐19 wave. There are concerns regarding infection risks but very little discussion of personal protective equipment (PPE) design [1, 2]. To understand how PPE changes clinical tasks, we conducted an online survey between (via Twitter, LinkedIn, etc.) 4 April and 8 May 2020, when there was a peak of 33,173 deaths. We focused on human factors/ergonomic issues [3] to avoid preconception bias about availability to ask with regard to fit and comfort, reading and operating equipment, hearing and communicating, reaching and moving, and dexterity to use touch screens, press buttons, open vials/taps and use syringes. We included a wide range of PPE to reflect changing guidelines for face cover (safety glasses with/without prescription spectacles, safety goggles, surgical masks, surgical hood with ties, FFP3 facemask and visor), body cover (plastic apron, surgical gown with sleeves, one‐piece coverall), and gloves (disposable, viral protection). Each section (face, body and gloves), had closed questions with a free text comment box. The questionnaire is available as online supporting information, Appendix S1.
Ethical approval was granted by Loughborough University. Data were analysed with SPSS software and NVivo12 for thematic analysis. The survey received 405 responses from 292 (72%) women and 111 (28%) men, representative of NHS staff [4]. The free text responses for face cover (n = 129), body cover (n = 54) and hand cover (n = 55) were used to frame the results as four themes: wearing PPE; working in PPE; surviving PPE; and supplying (the right) PPE (Fig. 1).
Figure 1.
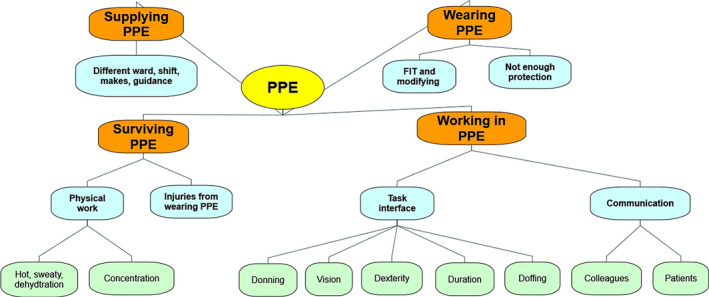
Qualitative themes.
Wearing PPE posed problems with fit; “Apparently masks for smaller faces don't exist!”, “I'm quite short and overweight and find that the all in one suits do not fit me very well due to the proportions”. Safety glasses were a poor fit for 34% (n = 83/247), rising to 62% (n = 118/190) when placed over prescription spectacles (significant association between fit and sex (p = 0.022), women reporting poorer fit). Surgical masks were a poor fit for 21% (n = 69/335) with more discomfort reported by women.
Several human factor/ergonomic issues were reported when working in PPE. Visual difficulties were reported for safety glasses (23%, n = 52/243) and visors (27%, n = 76/296) where the “glare of the FFP3 mask … makes my vision worse especially doing fine motor tasks (suturing a central line)”. Problems with communication and hearing alarms, etc., were reported for surgical masks (49%, n = 166/341), and visors (49%, n = 141/287) with women reporting significantly more difficulty (p = 0.038). Hand (fine motor) function was impaired “We now wear more than one pair of gloves to do complex fiddly tasks‐cannula/arterial line, local anaesthetic blocks, sutures, central line insertion, spinal or epidural block. My dexterity and ‘feel’ (haptic feedback) is definitely affected negatively”, with additional problems for non‐clinical activities including typing and using electronic interfaces. Reaching (gross motor) activities were restricted by both surgical gowns with sleeves (44%, n = 116/265) and one‐piece coveralls (66%, n = 39/59).
The surviving PPE theme included injuries and overheating “2 x plastic aprons and surgical gown as per PHE [5]guidance can get very sweaty and hot doing manual work, which can make it harder to focus or continue to give the same effort to the physical work”, “It contributes to stress, exhaustion”. Skin breakdown was reported “goggles pin my ears and apply pressure to frame, very uncomfortable and sore”, and musculoskeletal injuries associated with the “way your head seems to be held with full visor”. Supplying PPE included varying provision between shifts with up to 6 different designs of surgical masks.
Personal protective equipment acts as a safety barrier by changing the task interface, and we suggest that more human factors/ergonomic research is needed to improve the functional design of PPE so that healthcare workers are better supported to carry out critical care and other medical treatment.
Supporting information
Appendix S1. Usability of PPE for COVID‐19 questionnaire.
Acknowledgements
We thank D. Roland and E. Crumpton for comments on the survey design/content and D. Gyi and A. Lloyd for reviewing the results/analysis. No external funding or competing interests declared.
References
- 1. Sayburn A. Are UK doctors getting sufficient protective equipment against covid‐19? British Medical Journal 2020; 369: m1297. [DOI] [PubMed] [Google Scholar]
- 2. Heij R, Steel AG, Young PJ. Testing for coverage from personal protective equipment. Anaesthesia 2020; 75: 962–3. [DOI] [PubMed] [Google Scholar]
- 3. Hignett S, Lang A, Pickup L, et al. More holes than cheese. What prevents the delivery of effective, high quality, and safe healthcare in England? Ergonomics 2016; 61: 5–14. [DOI] [PubMed] [Google Scholar]
- 4. NHS Digital . Narrowing of NHS gender divide but men still the majority in senior roles. 2018. https://digital.nhs.uk/news-and-events/latest-news/narrowing-of-nhs-gender-divide-but-men-still-the-majority-in-senior-roles (accessed 08/06/2020).
- 5. Public Health England . COVID‐19 personal protective equipment (PPE). 2020. https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control/covid-19-personal-protective-equipment-ppe (accessed 27/05/2020).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Usability of PPE for COVID‐19 questionnaire.


