Abstract
BACKGROUND/OBJECTIVES
Nursing home (NH) residents are a vulnerable population, susceptible to respiratory disease outbreaks such as coronavirus disease 2019 (COVID‐19). Poor outcome in COVID‐19 is at least partly attributed to hypercoagulability, resulting in a high incidence of thromboembolic complications. It is unknown whether commonly used antithrombotic therapies may protect the vulnerable NH population with COVID‐19 against mortality. This study aimed to investigate whether the use of oral antithrombotic therapy (OAT) was associated with a lower mortality in NH residents with COVID‐19.
DESIGN
A retrospective case series.
SETTING
Fourteen NH facilities from the NH organization Envida, Maastricht, the Netherlands
PARTICIPANTS
A total of 101 NH residents with COVID‐19 were enrolled.
MEASUREMENTS
The primary outcome was all‐cause mortality. The association between age, sex, comorbidity, OAT, and mortality was assessed using logistic regression analysis.
RESULTS
Overall mortality was 47.5% in NH residents from 14 NH facilities. Age, comorbidity, and medication use were comparable among NH residents who survived and who died. OAT was associated with a lower mortality in NH residents with COVID‐19 in the univariable analysis (odds ratio (OR) = 0.89; 95% confidence interval (CI) = 0.41–1.95). However, additional adjustments for sex, age, and comorbidity attenuated this difference. Mortality in males was higher compared with female residents (OR = 3.96; 95% CI = 1.62–9.65). Male residents who died were younger compared with female residents (82.2 (standard deviation (SD) = 6.3) vs 89.1 (SD = 6.8) years; P < .001).
CONCLUSION
NH residents in the 14 facilities we studied were severely affected by the COVID‐19 pandemic, with a mortality of 47.5%. Male NH residents with COVID‐19 had worse outcomes than females. We did not find evidence for any protection against mortality by OAT, necessitating further research into strategies to mitigate poor outcome of COVID‐19 in vulnerable NH populations. J Am Geriatr Soc 68:1647‐1652, 2020.
Keywords: COVID‐19, nursing home, older people, thromboembolic complications, mortality
1. INTRODUCTION
Severe acute respiratory syndrome coronavirus‐2 (SARS‐CoV‐2) and the disease it causes, coronavirus disease 2019 (COVID‐19), currently places a tremendous burden on public life and health care worldwide. It is associated with poor outcome in certain high‐risk populations and has decimated nursing home (NH) populations in several parts of the world. NHs are known to be especially vulnerable to respiratory disease outbreaks, such as COVID‐19, resulting in substantial morbidity and mortality. 1 , 2 Furthermore, it is likely that distinct risk factors determine the poor outcome in NH populations relative to the general population. Most notably are an increased susceptibility to infection due to immune dysfunction and preexisting hyperinflammation attributed to the aging process, leading to a higher risk of adult respiratory distress syndrome 3 , 4 and a higher proportion of comorbidities and reduced pulmonary reserves. 5 Although NH residents are among the most severely affected populations by the current pandemic, they are severely underrepresented in the literature on COVID‐19. To date, only one study has reported on outcome in older patients (defined as ≥60 years) with COVID‐19. 6
An emerging body of studies suggests that COVID‐19 is associated with hypercoagulability and a strikingly high incidence of thromboembolic complications 7 and disseminated intravascular coagulation, especially in subgroups with a high mortality rate. 8 The origin of this profound thrombotic tendency appears to comprise a complex interplay of several hemostatic and inflammatory mechanisms. 9 , 10 In the Dutch NH population, a relatively large part of the population is using some form of oral antithrombotic therapy (OAT) for (secondary) prevention of cardiovascular or venous thromboembolic events (VTEs), such as anticoagulant therapy (AT) or antiplatelet therapy (APT). 11 In combination with their high event rate, the Dutch NH population constitutes an important entity to test the hypothesis of whether preexisting use of AT or APT is associated with a lower mortality in NH residents with COVID‐19.
In view of these considerations, the objective of the current study was to investigate whether the use of OAT was associated with lower mortality in NH residents with COVID‐19.
2. METHODS
2.1. Study Design, Setting, and Participants
A retrospective case series of 101 NH residents with COVID‐19 was collected at 14 NH facilities from the NH organization Envida between March 20, 2020, and May 1, 2020, in Maastricht, the Netherlands. The NH facilities are both small‐ and large‐scale homes, ranging from 14 (smallest) to 150 (largest) beds, adding up to a total capacity of 727 beds, which were all occupied. On most locations, medical as well as psychogeriatric wards are present.
NH residents with COVID‐19, as confirmed by real‐time reverse‐transcriptase polymerase chain reaction (rRT‐PCR) assay of SARS‐CoV‐2 mRNA in nasal or pharyngeal swabs, or those with symptoms, such as fever, respiratory complaints (cough, sneezing, and sore throat), but also malaise, muscle aches, headache, and gastrointestinal symptoms and a disease course consistent with COVID‐19 (rapid respiratory deterioration over several hours, or opposite, lingering, persistent illness with later deterioration) in absence of an alternative diagnosis were enrolled. In all facilities, according to directives from the area health organization, after two residents per location had been diagnosed with COVID‐19 based on a positive rRT‐PCR, subsequent residents with symptoms consistent with COVID‐19 were no longer tested, due to limited testing capacity. These residents were considered as COVID‐19 highly suspected and included in the current analysis. Overall, COVID‐19 was rRT‐PCR confirmed in 66% of the residents, and 34% were considered COVID‐19 highly suspected.
2.2. Covariates and Outcome
Age, sex, NH facility, medical history, medication use, and the result of the SARS‐CoV‐2 mRNA rRT‐PCR were retrospectively gathered from the patient records. In addition, we retrieved additional data on type and indication for OAT, vital status, and date of death.
Based on the medical history, the Charlson Comorbidity Index (CCI) was calculated to assess the comorbidity levels of the residents. AT was divided into vitamin K antagonists (VKAs), direct oral anticoagulants (DOACs), and APT. The primary outcome of this study is all‐cause mortality.
2.3. Data Analysis
Statistical analyses were performed using SPSS version 25.0. The characteristics of the residents were compared with a chi‐square test for categorical variables and unpaired t‐test or Mann‐Whitney U test for numerical variables, whichever was appropriate. To estimate the effect of OAT (VKA, DOAC, and APT were also tested separately) on mortality, univariable and multivariable logistic regression analyses were performed, and presented as odds ratios (ORs) with 95% confidence intervals (CIs). Potential confounders assessed included age, sex, CCI, other medication, and rRT‐PCR COVID‐19 result. Multivariable analysis included all variables considered clinically relevant. P < .05 was considered statistically significant.
To determine whether associations with mortality were underestimated by including individuals without rRT‐PCR proven COVID, a sensitivity analysis was performed, excluding these residents from the analyses on mortality and OAT.
3. RESULTS
3.1. Demographic Characteristics
In total, 101 NH residents, from 14 NH facilities with a total capacity of 727 beds, were included in this case series. Prevalence of COVID‐19 varied from 3.3% to 28.8% in the different facilities. Overall, the NH residents had a mean age of 85 years (standard deviation (SD) = 8.1 years), and 32.7% were male. The mean CCI was 2.0 (SD = 1.4), and mean medications used were 8.2 (SD = 3.8) (Table 1). Overall, 51.5% received OAT, of which 18% received either VKA or DOAC and 34% received APT. Table 2 shows the characteristics of the NH residents with COVID‐19 confirmed by rRT‐PCR.
Table 1.
Characteristics of the Total Nursing Home Population with Positive Viral Cultures and Those Highly Suspected of Having COVID‐19, but with No Documented Cultures
| Characteristics | Total (n = 101) | Survivor (n = 53) | Nonsurvivor (n = 48) | P value |
|---|---|---|---|---|
| Age, mean (SD), y | 85.0 (8.1) | 84.3 (8.7) | 85.8 (7.4) | .358 |
| Male, No. (%) | 33 (32.7) | 10 (18.9) | 23 (47.9) | .003 |
| COVID‐19 rRT‐PCR confirmed, No. (%) a | 67 (66.3) | 32 (60.4) | 35 (72.9) | .210 |
| Coexisting conditions, No. (%) | ||||
| Hypertension | 52 (51.5) | 32 (60.4) | 20 (41.7) | .074 |
| Dementia | 79 (78.2) | 41 (77.4) | 38 (79.2) | 1.00 |
| Myocardial infarction | 7 (6.9) | 2 (3.8) | 5 (10.4) | .252 |
| CHF | 18 (17.8) | 13 (24.5) | 5 (10.4) | .074 |
| Diabetes mellitus, type II | 14 (13.9) | 8 (15.1) | 6 (12.5) | .779 |
| CVA/TIA | 34 (33.7) | 20 (37.7) | 14 (29.2) | .404 |
| CCI, mean (SD) | 2.04 (1.4) | 2.2 (1.5) | 1.9 (1.3) | .409 |
| No. of medications, mean (SD) | 8.2 (3.8) | 8.5 (4.0) | 7.8 (3.5) | .328 |
| OAT, No. (%) | ||||
| No OAT | 49 (48.5) | 25 (47.2) | 24 (50) | .590 |
| VKA/DOAC | 18 (17.8) | 8 (15.1) | 10 (20.8) | |
| APT | 34 (33.7) | 20 (37.7) | 14 (29.2) | |
Abbreviations: APT, antiplatelet therapy; CCI, Charlson Comorbidity Index; CHF, congestive heart failure; COVID‐19, coronavirus disease 2019; CVA, cerebrovascular accident; DOAC, direct oral anticoagulant; OAT, oral antithrombotic therapy; rRT‐PCR, real‐time reverse‐transcriptase polymerase chain reaction; SD, standard deviation; TIA, transient ischemic attack; VKA, vitamin K antagonist.
Specific breakdown of rRT‐PCR–positive residents is shown in Table 2.
Table 2.
Characteristics of Nursing Home Residents with COVID‐19 rRT‐PCR Confirmed
| Characteristics | Total (n = 67) | Survivor (n = 32) | Nonsurvivor (n = 35) | P value |
|---|---|---|---|---|
| Age, mean (SD), y | 84.4 (8.5) | 82.5 (9.6) | 86.2 (7.0) | .076 |
| Male, No. (%) | 25 (37.3) | 7 (21.9) | 18 (51.4) | .022 |
| Coexisting conditions, No. (%) | ||||
| Hypertension | 33 (49.3) | 19 (59.4) | 14 (40) | .145 |
| Dementia | 45 (67.2) | 20 (62.5) | 25 (71.4) | .603 |
| Myocardial infarction | 7 (10.4) | 2 (6.3) | 5 (14.3) | .431 |
| CHF | 13 (19.4) | 9 (28.1) | 4 (11.4) | .123 |
| Diabetes mellitus, type II | 9 (13.4) | 4 (12.5) | 5 (14.3) | 1.00 |
| CVA/TIA | 20 (29.9) | 10 (31.3) | 10 (28.6) | 1.00 |
| CCI, mean (SD) | 2.0 (1.3) | 2.0 (1.2) | 2.1 (1.3) | .760 |
| No. of medications, mean (SD) | 9.0 (3.8) | 9.5 (4.2) | 8.6 (3.4) | .356 |
| OAT, No. (%) | ||||
| No OAT | 29 (43.3) | 13 (40.6) | 16 (45.7) | .737 |
| VKA/DOAC | 16 (23.9) | 7 (21.9) | 9 (25.7) | |
| APT | 22 (32.8) | 12 (37.5) | 10 (28.6) | |
Abbreviations: APT, antiplatelet therapy; CCI, Charlson Comorbidity Index; CHF, congestive heart failure; COVID‐19, coronavirus disease 2019; CVA, cerebrovascular accident; DOAC, direct oral anticoagulant; OAT, oral antithrombotic therapy; rRT‐PCR, real‐time reverse‐transcriptase polymerase chain reaction; SD, standard deviation; TIA, transient ischemic attack; VKA, vitamin K antagonist.
COVID‐19 highly suspected NH residents used on average fewer medications (mean = 6.5 vs 9.0; P = .001) and were more often diagnosed with dementia (100% vs 49.3%; P < .001) compared with NH residents with rRT‐PCR confirmed COVID‐19 (Supplementary Table S1).
3.2. Mortality
Overall, 47.5% of the NH residents with COVID‐19 died. Demographic characteristics were similar between survivors and nonsurvivors in the total population (Table 1), whereas in the population with rRT‐PCR confirmed COVID‐19, nonsurvivors were more often male (Table 2).
We found no obvious associations between age, COVID‐19 rRT‐PCR, CCI, hypertension, other medication, and mortality. Additionally, OAT was associated with lower mortality in NH residents with COVID‐19 in the univariable analysis (OR = 0.89; 95% CI = 0.41–1.95). However, this effect attenuated in the multivariable analysis after adjustment for age, sex, CCI, and hypertension (Table 3).
Table 3.
Univariable and Multivariable Logistic Regression Analyses to Explore the Association Between Clinical Characteristics and Mortality in NH Residents with COVID‐19
| Characteristics | Univariable analysis | Multivariable analysis, | |
|---|---|---|---|
| OR (95% CI) | P value | adjusted OR (95% CI) a | |
| Age (years) | 1.02 (0.97–1.08) | .356 | 1.04 (0.39–2.77) |
| Sex (male) | 3.96 (1.62–9.65) | .002 | 4.79 (1.74–13.18) |
| COVID‐19 rRT‐PCR confirmed | 0.57 (0.24–1.31) | .185 | 1.68 (0.61–4.57) |
| CCI (unit) | 0.88 (0.66–1.18) | .404 | 0.79 (0.55–1.16) |
| Hypertension (no is reference) | 2.13 (0.96–4.73) | .062 | 0.54 (0.22–1.37) |
| No. of medications | 0.95 (0.85–1.05) | .325 | 0.98 (0.83–1.14) |
| OAT (no is reference) | 0.89 (0.41–1.95) | .776 | 1.04 (0.39–2.77) |
Abbreviations: CCI, Charlson Comorbidity Index; CI, confidence interval; COVID‐19, coronavirus disease 2019; NH, nursing home; OAT, oral antithrombotic therapy; OR, odds ratio; rRT‐PCR, real‐time reverse‐transcriptase polymerase chain reaction.
Adjusted for age, sex, COVID‐19 rRT‐PCR result, CCI, hypertension, medication use, and OAT.
Male sex was associated with considerably higher mortality compared with female residents (OR = 3.96; 95% CI = 1.62–9.65). This association did not attenuate after adjustment for age, OAT, CCI, and hypertension (OR = 4.79; 95% CI = 1.74–13.18). Moreover, male residents with COVID‐19 who died were relatively younger compared with those who recovered (82.2 (SD = 6.3) vs 85.2 (SD = 4.9) years) and compared with female residents who died (89.1 (SD = 6.3) years; P < .001) (Figure 1).
Figure 1.
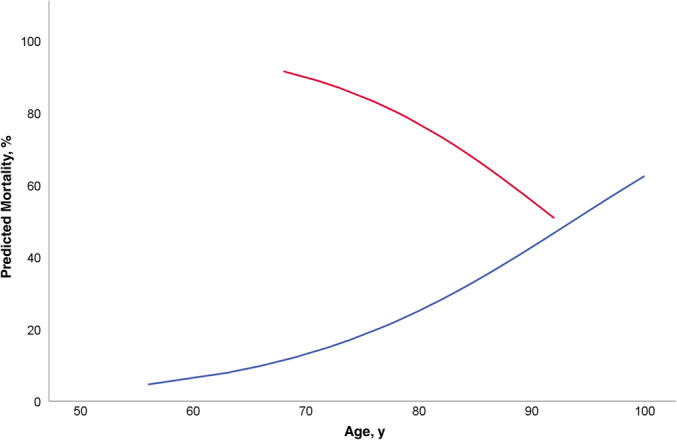
Predicted probability of death from the logistic regression model illustrating the interaction effect of sex and age on mortality. Male nursing home residents (red line) at younger ages have higher mortality than older men, and their mortality rates steadily decrease with age. Female nursing home residents (blue line) show the opposite.
We found similar results when we excluded the COVID‐19 highly suspected residents (Supplementary Table S2).
4. DISCUSSION
This study did not demonstrate any obvious benefit from the use of OAT in vulnerable NH residents on mortality from COVID‐19 infection. Strikingly, almost half of the population had died within 2 weeks after the diagnosis of COVID‐19 was made. This was particularly the case for male residents, and this risk was not attenuated after adjustment for OAT as well as other potential confounders.
A protective effect of OAT was postulated based on current literature showing a high rate of VTE, as well as ischemic stroke. 7 , 12 APT provides some protection against VTE, although it is not a cornerstone treatment in the prevention of VTE. Therefore, because most OAT was composed of APT, the protective effect of OAT may have been insufficient in these patients with such high mortality. The slight but nonsignificant benefit of OAT in the univariable analysis might theoretically be related to the use of oral anticoagulants, but the fraction of AT users may have been too small and the disease burden too high to reveal any effect on mortality.
Although COVID‐19 is associated with hypercoagulability and a strikingly high incidence of thromboembolic complications in other, predominantly intensive care unit, populations, 7 mortality may not be greatly reduced by expanding the prescription of OAT in the NH population to protect this vulnerable population against excess mortality when a COVID‐19 outbreak in an NH becomes apparent. However, retrospective analyses in hospital settings suggest a possible benefit of the use of low‐molecular‐weight heparin (LMWH)/heparin on COVID‐19–related mortality. 13 , 14 Given the fact that most patients in this study on OAT used an antiplatelet agent, the addition of LMWH thromboprophylaxis may therefore be of benefit, and should be investigated in the NH setting. An important consideration is that we also did not find evidence for a negative impact of OAT on mortality, suggesting the relative safety of OAT in the context of COVID‐19.
COVID‐19 is a heterogenic disease, and may therefore run a different course in NH residents compared with other populations. This is substantiated by the alarming proportion of residents who died after COVID‐19 diagnosis. These residents might die because of respiratory failure due to the viral pneumonia itself, whereas patients with a larger pulmonary reserve have less competing risk to die as a direct result of the pulmonary disease, allowing for a higher event rate of fatal VTE.
To the best of our knowledge, this is the first study to report a mortality of 47.5% in NH residents with COVID‐19, who resided in 14 NH facilities. Male residents had a particularly high mortality, which is consistent with previous studies. 15 , 16 In our current study, we found no confounding effect by hypertension or CCI. Higher previous smoking rates, higher body mass index, and more subclinical atherosclerosis are possible candidates that may explain this association, but these factors could not be recorded in the current study. As our study population consisted solely of older NH residents, a higher mortality rate was to be expected, although the excessively high mortality emphasizes the vulnerability of this population. Moreover, disease presentation is often atypical, which may result in underestimation of disease severity and delayed diagnosis of COVID‐19, 17 while subsequent implementation of infection prevention is compromised. 2
Our study offers important insights into the tremendous impact of COVID‐19 on NH residents, a vulnerable population in whom information on outcomes is currently limited. Nevertheless, our study has several limitations that warrant careful consideration, such as its retrospective design and observational nature. Furthermore, we investigated mortality in 14 NH facilities in the southern region of the Netherlands. Although we were not able to estimate conclusive prevalence figures due to limited testing capacity, this region appeared to be one of the country's most severely affected. Therefore, our findings may not be generalizable to all NHs.
Next, as mentioned before, older patients and in particular NH residents who are frail and have multiple chronic conditions often have an atypical disease presentation and therefore NH residents with COVID‐19 could have been missed. However, the opposite is also true; despite having typical symptoms, we might have included residents without COVID‐19 but with, for example, influenza, albeit flu season was largely over.
Further, residual confounding is likely as we had no access to clinical variables, such as pack‐years smoked, body weight index, and systolic blood pressure. Additionally, not all residents had an rRT‐PCR confirmed diagnosis of COVID‐19; and although the sensitivity analysis revealed no differences, this may have resulted in underestimation of the effect that OAT may have on mortality due to possible misclassification. Also, none of the residents had been assessed for occurrence of VTE. We therefore cannot exclude that OAT prevented VTE, and we may have missed effects on mortality due to limited statistical power.
In conclusion, our case series demonstrates that NH residents are severely affected by the COVID‐19 pandemic, with a mortality of 47.5%. In particular, male NH residents with COVID‐19 appear to have a poor outcome. We did not find evidence for any protection against mortality by OAT. Therefore, additional studies evaluating compressive stockings and LMWH are urgently needed in NH residents, as an approach to reduce mortality by COVID‐19 in this vulnerable population.
5.
Editor's Note.
This is a very well done retrospective analysis completed very quickly by colleagues in the Netherlands in 14 nursing homes (NHs) involving 101 NH residents – 67 with proven and 34 with highly suspected COVID‐19 disease. Despite the limitations of incomplete testing, retrospective design, and lack of robust propensity matching, this paper illustrates a critical paradigm in Geriatrics and nursing home (NH) care.
Primum non‐nocere – first do no harm ‐ should be in the minds of all clinicians who care for NH reidents. We have learned over the last three months that we cannot get ahead of the evidence. The use of hydroxychloroquine, alone or in combination with azithromycin, for documented or presumed COVID‐19 disease was associated with increased, not decreased mortality. Clinicians prescribing these medications, understandably to help NH residents under their care, may have unintentionally done more harm than good due at least in part to the susceptibility of older NH residents with underlying cardiovascular disease to develop prolonged QT intervals and sudden death due to related arrhythmias.
Because of the predisposition of NH residents to thrombotic events, reported associations between COVID‐19 and thrombotic events, the non‐specific or atypical presentation of COVID‐19 in this population, and the lack of rapid, accurate testing, some clinicians started prescribing oral anticoagulation therapy (OAT) routinely for NH residents suspected of having COVID‐19. This approach certainly seems reasonable based on the desire to prevent the potentially devastating consequences of a stroke or pulmonary embolism. However, the risks of bleeding with OAT may outweigh the benefits in the NH population, especially among those with life‐limiting illness.
This study adds another cautionary note to getting ahead of the evidence when treating the vulnerable NH population. Only larger, prospective studies with robust propensity matching will help us understand the best approach to using OAT in NH residents with proven or highly suspected COVID‐19.
Joseph G. Ouslander, MD
Supporting information
Supplementary Table S1: Characteristics of NH Residents with Confirmed Versus Highly Suspected COVID‐19
Supplementary Table S2: Sensitivity Analysis for Multivariable Analysis, Excluding COVID‐19 Highly Suspected
ACKNOWLEDGMENTS
Conflict of Interest
The authors have declared no conflicts of interest.
Author Contributions
Study conception and design: Magdelijns, Joosten, Schols, ten Cate‐Hoek, and Spaetgens. Acquisition of data: Brouns, Brüggemann, Linkens, Heijnen, Schols, and Spaetgens. Analysis and interpretation of data: Brouns, Linkens, ten Cate‐Hoek, ten Cate, and Spaetgens.
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be submitted for publication.
Sponsor's Role
No funding was received for this work.
REFERENCES
- 1. McMichael TM, Currie DW, Clark S, et al. Epidemiology of Covid‐19 in a long‐term care facility in King County, Washington. N Engl J Med. 2020;382:2005‐2011. 10.1056/NEJMoa2005412. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Arons MM, Hatfield KM, Reddy SC, et al. Presymptomatic SARS‐CoV‐2 infections and transmission in a skilled nursing facility. N Engl J Med. 2020;382:2081‐2090. 10.1056/NEJMoa2008457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Franceschi C, Garagnani P, Parini P, Giuliani C, Santoro A. Inflammaging: a new immune–metabolic viewpoint for age‐related diseases. Nat Rev Endocrinol. 2018;14:576‐590. [DOI] [PubMed] [Google Scholar]
- 4. Hecker L. Mechanisms and consequences of oxidative stress in lung disease: therapeutic implications for an aging populace. Am J Physiol Lung Cell Mol Physiol. 2018;314:L642‐L653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lowery EM, Brubaker AL, Kuhlmann E, Kovacs EJ. The aging lung. Clin Interv Aging. 2013;8:1489‐1496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sun H, Ning R, Tao Y, et al. Risk factors for mortality in 244 older adults with COVID‐19 in Wuhan, China: a retrospective study. J Am Geriatr Soc. 2020;68(6). 10.1111/jgs.16533. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Klok FA, Kruip M, van der Meer NJM, et al. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID‐19: an updated analysis. Thromb Res. 2020;191:148‐150. 10.1016/j.thromres.2020.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18:844‐847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Oudkerk M, Büller HR, Kuijpers D, et al. Diagnosis, prevention, and treatment of thromboembolic complications in COVID‐19: report of the national institute for public health of the Netherlands. Radiology. 2020;201629. 10.1148/radiol.2020201629. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Levi M, Thachil J, Iba T, Levy JH. Coagulation abnormalities and thrombosis in patients with COVID‐19. Lancet Haematol. 2020;7:e438‐e440. 10.1016/S2352-3026(20)30145-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Malek Makan A, van Hout H, Onder G, Finne‐Soveri H, van der Roest H, van Marum R. Prevalence of preventive cardiovascular medication use in nursing home residents: room for deprescribing? the SHELTER study. J Am Med Dir Assoc. 2017;18:1037‐1042. [DOI] [PubMed] [Google Scholar]
- 12. Lodigiani C, Iapichino G, Carenzo L, et al. Venous and arterial thromboembolic complications in COVID‐19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18:1094‐1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Paranjpe FV, Lala A, et al. Association of treatment dose anticoagulation with in‐hospital survival among hospitalized patients with COVID‐19. J Am Coll Cardiol. 2020;S0735‐1098:35218‐9. 10.1016/j.jacc.2020.05.001. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497‐506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708‐1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Norman RE, Stall NM, Sinha SK. Typically atypical: COVID‐19 presenting as a fall in an older adult. J Am Geriatr Soc. 2020. 10.1111/jgs.16526. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1: Characteristics of NH Residents with Confirmed Versus Highly Suspected COVID‐19
Supplementary Table S2: Sensitivity Analysis for Multivariable Analysis, Excluding COVID‐19 Highly Suspected


