Abstract
Background
The coronavirus disease 2019 (COVID‐19) epidemic affected blood collection in Guangzhou, China.
Study Design and Methods
This paper includes three studies. The observational study reported the trends of blood collection during the epidemic in Guangzhou, China. The cross‐sectional survey investigated factors influencing blood donation during the COVID‐19 epidemic, and a self‐administered questionnaire was given to 1584 street whole blood donors (SWBDs) who donated during the epidemic. The randomized controlled trial involved 19 491 SWBDs who donated in 2019 but did not donate during the epidemic. Trial participants were randomly assigned to two intervention groups: Group 1 completed Questionnaire 1, which contained precautionary measures in response to COVID‐19 and other messages about blood donation during the epidemic; Group 2 completed Questionnaire 2, which did not include this information. A control group did not receive any questionnaire.
Results
As measures were implemented, the number of blood donors increased accordingly. Both first‐time and repeat SWBDs perceived the same level of blood need and donated blood because it would save lives. SWBDs who completed Questionnaire 1 expressed a greater intention to donate during the epidemic. Enabling blood donors to perceive a higher level of blood need and a lower level of COVID‐19 infection risk related to blood donation mobilized experienced SWBDs to donate within 3 weeks. Intention‐to‐treat analyses and average‐treatment‐effect‐on‐the‐treated estimations confirmed that Questionnaire 1 could motivate SWBDs to actually donate blood.
Conclusion
Various measures could ease blood shortage during the COVID‐19 epidemic. Administration of Questionnaire 1 could increase blood donations during the epidemic.
Abbreviations
- ANCOVA
analysis of covariance
- ANOVA
analysis of variance
- ATT
average treatment effect on the treated
- CFA
confirmatory factor analysis
- CI
confidence interval
- COVID‐19
coronavirus disease 2019
- EFA
exploratory factor analysis
- GWBDs
group whole blood donors
- ITT
intention‐to‐treat
- SWBDs
street whole blood donors
1. INTRODUCTION
In December 2019, an unknown pneumonia rapidly spread in Wuhan, China, and subsequently, a new coronavirus, coronavirus disease 2019 (COVID‐19), aroused the attention of the entire world. Given the unprecedented nature of this event, the epidemic is threating the collection and supply of blood in China. To contain the spread of the disease, local governments closed many public places, including social and entertainment venues. Many organizations delayed the return to work until 1 March 2020. Schools and universities were shut down. Every street was virtually deserted for weeks. The number of voluntary nonremunerated blood donors decreased dramatically. Because of the blood shortage, patient blood management and cessation of elective surgery has contributed to decreasing demand, but sepsis may increase requirements, and salient reductions will not be possible in areas such as trauma, cancer, hereditary hemolytic anemias, and childbirth. Therefore, recruiting a sufficient number of blood donors during this epidemic is vital for public health in China and globally.
Guangdong Province is located in southernmost mainland China and has 21 prefecture‐level cities and 30 blood collection and supply institutions. Guangdong Province also had the largest population (115.21 million) and the largest gross domestic product (US$1.59 trillion) among Chinese regions. 1 Its provincial capital, Guangzhou, is one of Chinaʼs well‐developed cities and is one of the first‐tier cities along with Beijing, Shanghai, and Shenzhen. Guangzhou has 11 districts and a resident population of 15.30 million. There is one blood center (Guangzhou Blood Center) and four blood stations (Guangzhou Panyu District Central Blood Station, Guangzhou Blood Center Conghua District Blood Station, Guangzhou Blood Center Zengcheng District Blood Station, and Guangzhou Blood Center Huadu District Blood Station) in Guangzhou. The four blood stations are operationally affiliated with the blood center but are administratively independent. The Guangzhou Blood Center has the authority to collect blood in all 21 prefecture‐level cities in Guangdong, whereas other blood collection and supply institutions, including the four blood stations in Guangzhou, cannot collect blood outside their administrative regions. The blood collection and supply amount of the Guangzhou Blood Center was the second highest in China, ranked behind Beijing and ahead of Shanghai. In 2019, the total number of blood donations (one blood donor might donate more than once) collected by the Guangzhou Blood Center was 326 400, in which 277 574 were from whole blood donation and 48 826 were from apheresis platelet donation. In 2019, 5093 medical and health organizations were located in Guangzhou, of which 269 were hospitals. The Guangzhou Blood Center supplied 451 010 units of red blood cells and 87 303 units of apheresis platelets to >160 medical institutions in 2019.
Since the first patient with confirmed COVID‐19 was reported on 20 January 2020, in Guangzhou, the numbers of both whole blood and platelet donors began to drop. This decrease was primarily caused by an unavailability of blood donors as a result of the avoidance of public places and the closing of workplaces and universities, which typically are locations for blood drives during normal times. Some potential donors also feared that giving blood might weaken their immune defense, thereby rendering them more susceptible to the COVID‐19 infection. Other reasons, such as quarantine, caring for relatives, and fear of exposure to COVID‐19, also must be considered. 2 To solve the blood shortage crisis, the Guangzhou Blood Center activated emergency blood donor recruitment measures, including the use of media and communication tools to spread the message of blood shortage to citizens, sending cell phone messages and making telephone calls to those who previously had donated blood but had not yet donated again (ie, experienced donors), and training the staff with special guidelines to follow during the epidemic. 3 Moreover, national, provincial, and municipal governments released official blood donation proposals, appealing to citizens to donate blood and organizations to host blood donation activities. After a series of such measures, the number of blood donors had increased.
Blood donors in China typically can be categorized as one of two forms: those who spontaneously donate at blood collection sites (so‐called street blood donors) and those who donate through a group donation (so‐called group blood donors). Street blood donors are different from community volunteer blood donors because street blood donors are not just from the community. Fixed blood donation sites, including blood drives and blood donation stations, are open every day and are located in popular and busy pedestrian zones or shopping malls to ensure that donors from across China, including tourists, can donate whole blood and platelets whenever they encounter the sites. In addition, blood drives occasionally will be sent to some communities to serve whole blood donors in those communities. Street blood donors donate blood solely because of their willingness. State‐owned and state‐run enterprises, such as hospitals, government agencies, high schools, universities, and liberation armies, organize blood donation activities to mobilize their staff, students, or militaries to donate whole blood or platelets, which follows government instructions. Some private enterprises and nongovernmental organizations also organize blood donation activities mainly because of social responsibility. Enterprises, institutions, and organizations that organize blood donation activities are called “groups” in China. Donors from the same group donate whole blood or platelets at the same location (either a workplace or blood donation site) simultaneously. These groups organize blood donation activities at regularly scheduled times. Blood drives organized by the Guangzhou Blood Center are seldom or never sent to collect blood from street blood donors outside Guangzhou, whereas blood drives may be sent out to collect blood from group blood donors outside Guangzhou if those groups organize blood donation activities. In 2019, the numbers of donations of street blood donors and group blood donors collected by the Guangzhou Blood Center were 224 658 (68.8%) and 101 742 (31.2%), respectively. The National Health Commission of the Peopleʼs Republic of China dispatched a document on 22 September 2017, which stipulated that mutual (family/replacement) blood donation must cease before the end of March 2018. Therefore, there are now only volunteer nonremunerated blood donors in China no matter how they are categorized. Individuals who are affiliated with the groups mentioned earlier, however, have been encouraged to voluntarily donate blood and often are awarded subsidies (small amounts of money for nutritional supplement) or are given a few days off (with or without paid vacations). In light of these subsidies, the objectives for blood donation of group donors, other than pure altruism, might include a combination of motives, such as modestly self‐serving incentives, persuasion by colleagues or schoolmates, and group pressure. Therefore, compared with group blood donors, street blood donors in China might be more likely to donate spontaneously and altruistically, while also combining some self‐serving motives, which is typical of most blood donors around the world. 4 , 5 , 6 , 7 , 8
This paper reports an observational study, a cross‐sectional survey, and a randomized controlled trial. The observational study explored the trend of blood donation in Guangzhou, China, during the COVID‐19 epidemic. The cross‐sectional survey of street whole blood donors (SWBDs) who donated whole blood at donation sites during the epidemic was conducted to understand the factors influencing their donation. Characteristics of both first‐time and repeat whole blood donors were compared simultaneously. The single‐center, single‐blind, parallel randomized controlled trial involved two intervention groups and a control group. In this trial, two different questionnaires were provided to experienced SWBDs who donated in 2019 but had not donated during the epidemic. At the same time, an equal number of SWBDs were coded as the control group. The objectives of this trial were to examine (a) factors of their deferral and (b) how the questionnaireʼs information about blood donation precautionary measures in response to COVID‐19 and other messages about blood donation during the epidemic affected participantsʼ willingness to donate blood. Actual behavior (ie, blood donation within 3 weeks) of these three groups in this trial were compared. Finally, common factors in the survey and the trial were compared. All procedures of the study, the survey, and the trial were reviewed and approved by the Institutional Review Board of the Guangzhou Blood Center. The registration IDs for the trial on ClinicalTrial.gov is NCT04306055. This trial was reported according to the Consolidated Standards of Reporting Trials statements.
2. MATERIALS AND METHODS
2.1. The observational study
Trends of blood collection in Guangzhou, China, from 1 January to 31 March, 2020, compared with the same time period in year 2019 were reported. Trends in blood collection along with the number of confirmed cases of COVID‐19 from January 20 (the first confirmed case was reported in Guangzhou) to 31 March 2020, in Guangzhou were also presented. Donors cannot donate whole blood again for 180 days and cannot donate platelets for 90 days if they have donated whole blood. Donors cannot donate platelets again for 15 days and cannot donate whole blood for 90 days if they have donated platelets. Therefore, the comparison of trends of blood collection included the number of whole blood and platelet donations that donors could have made from January to March (≥90 days), and they could have donated platelets more than once. Total whole blood donation and platelet donation referred to the total number of whole blood and platelet donations made by donors from street and group donors. Street whole blood donation referred to the number of whole blood donations made by donors who donated whole blood solely because of their willingness rather than group organization. Group whole blood donation referred to the number of whole blood donations made by donors who donated whole blood during the donation activities held by their groups (group whole blood donors, GWBDs); “nonhospital groups” referred to all groups except for hospitals. Trends of blood donors in 2019 and 2020 were compared by sex, age, donation frequency, donation type (whole blood or platelet donation), and donation form (street or group donation). The attributes of a blood donor were based on his or her last donation; for instance, if a donor donated platelets on 1 January 2020, which was his or her fourth donation, and he or she donated whole blood on February 1, then he or she was defined as a whole blood donor with a donation frequency of five. Numbers of serologic markers for transfusion‐transmitted infections during the same period were also compared. All of the data were provided by the Guangzhou Blood Center through the Blood Donation and Supply System. 9
The Guangzhou Blood Center kept sending reminders to experienced blood donors every day by an automated message system after they reached the appropriate donation interval. In response to the blood shortage, on 30 January 2020, the Guangzhou Blood Center sent recruitment cell phone text messages to experienced blood donors whose last donations were between 20 July 2016 and 20 July 2019 (n = 432 396). The content of the message was as following:
The first batch of blood products has been sent to Wuhan before the Spring Festival. Due to the COVID‐19 epidemic, the number of blood donors decreased sharply during the Spring Festival, and blood for clinical use in Guangzhou is urgently need. Please participate in blood donation while ensuring your personal protection.
During the epidemic, recruiters from the Guangzhou Blood Center were prevented from going back to work, but they still made telephone calls from home to recruit experienced donors, as they did at the blood center in 2019. On 2 February and 20 February, various media channels broadcasted blood shortage messages and appeals from the Guangzhou Blood Center to the public, stating that there were not enough blood products for clinical use and that people donating blood were urgently needed. The national, Guangdong, and Guangzhou governments released official blood donation announcements to advocate for state‐owned and state‐run enterprises to organize group blood donation activities. On March 13, the academician Zhong Nan‐Shan, who is a specialist in respiratory diseases and a leading figure in Chinaʼs fight against COVID‐19, appealed to citizens to donate blood through a television news interview. No blood shortage message was broadcasted by media, no blood donation announcement was released by any government, and no celebrity made an appeal for blood donation in Guangzhou in 2019.
2.2. The cross‐sectional survey
2.2.1. Study design and participants
This survey focused only on SWBDs because recruitment of platelet donors in Guangzhou is different from recruitment of whole blood donors. For instance, there was a blood credit system for apheresis platelet donation in Guangzhou, and donors would receive extra incentives if they donated platelets a specific number of times. Blood donors could get different values of prepaid shopping cards according to their credits earned in 1 year. Because this credit system was canceled on 1 April 2020, the objectives of blood donation among the platelet donors in this study who had donated before 1 April would be difficult to determine. 10 At 10:00 on 10 March 2020, cell phone text messages containing the questionnaire link were sent to SWBDs who had donated blood in Guangzhou between 23 January 2020 and 8 March 2020. During this period, 9244 SWBDs donated blood, and messages were sent to 9117 SWBDs with a valid cell phone number. The link was set to be closed at 23:59 on 10 March 2020. First‐time SWBDs were those who had never donated blood in Guangzhou before the epidemic and who made their first blood donation at the blood donation site in Guangzhou; repeat SWBDs were those who had donated blood before the epidemic and who made another donation at the whole blood donation site.
2.2.2. Questionnaire
Little research has examined blood donor recruitment during an epidemic. Therefore, the principal investigators designed the questionnaire and four experts in the blood donor recruitment field improved it (Appendix 1). The survey required SWBDs to answer the question on a 5‐point Likert scale, other than the questions about purposes of the latest donation, which were rated on the following 3‐point scale: 1 = not at all, 2 = not entirely, and 3 = entirely.
2.2.3. Analysis
Computer software (SPSS Statistics version 22 for Windows, SPSS Inc.) was used for all of the quantitative analysis in the survey and the trial. Exploratory factor analysis (EFA) was applied to examine the construct validity of the questionnaire, and the questionnaire was modified for further use in the trial. Factors influencing blood donation during the epidemic by first‐time and repeat SWBDs were compared using independent‐sample t tests.
2.3. The randomized controlled trial
2.3.1. Study design and participants
This was a single‐center (only data from the Guangzhou Blood Center were collected), single‐blind, parallel randomized trial. Two different questionnaires were entered into the Web site: Questionnaire 1 contained precautionary measures in response to COVID‐19 and other messages about blood donation during the epidemic, and Questionnaire 2 did not. As mentioned, it was difficult to identify which recruitment methods were able to successfully urge the platelet donors to return. Therefore, to avoid contaminations, only SWBDs were recruited. SWBDs were excluded if they had a cause for temporary or permanent deferral status, had an obviously invalid cell phone number, and were ≥60 years old (the upper age limit for blood donation in China is 55 years old; for repeat blood donors who meet the requirements of a health examination and have not had an adverse reaction to previous blood donation, the age limit of blood donation can be raised to 60 years old). In total, 19 491 eligible SWBDs whose last donations were between 1 February 2019 and 31 March 2019, were identified. These donors were randomly assigned to the following questionnaire groups based on a computer‐generated list of random numbers: Group 1, questionnaire contained the information (Questionnaire 1); Group 2, the questionnaire did not contain the information (Questionnaire 2); and Group 3, a no‐questionnaire control group. Figure 1 shows the flowchart of this trial.
FIGURE 1.
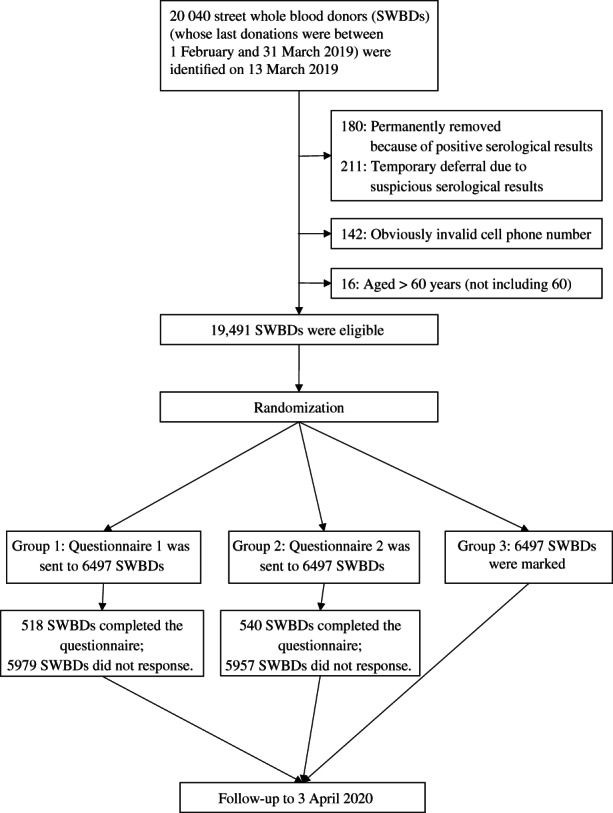
Flowchart of the randomized controlled trial
At 9:00 am on 13 March 2020, cell phone text messages containing the corresponding link for the questionnaire were sent to SWBDs in Groups 1 and 2. They were told in the messages that they were being asked to complete the questionnaire to promote blood donation during the epidemic. After the SWBDs had completed the questionnaire, they were redirected to a page requiring them to provide their name and cell phone number for follow‐up, and they were given the chance to win a small souvenir (a cutlery set) by a lucky draw. The personal information and the results of the questionnaire were separated to protect their privacy.
2.3.2. Interventions and endpoint
The questionnaire in this trial was designed based on the EFA results in the observational study. Questions in Questionnaires 1 and 2 were the same, but Questionnaire 1 also included the information about the epidemic of COVID‐19, such as the reasons why blood was needed during the epidemic and measures the blood center adopted to protect blood donors; corresponding vignettes were also presented in this questionnaire. Appendix 2 provides the details of the questionnaires. In consideration of time, personnel, and other resources, the Web sites of the questionnaire were set to be closed at 11:59 pm on 13 March 2020.
The factors related to blood donation during the epidemic, including the willingness to donate within 3 weeks, were analyzed and compared. The donation behavior of each participant in the three groups was followed for 3 weeks. The blood redonation rate of each group, which was defined as the occurrence of the next blood donation attempt among all of the participants within the 3‐week follow‐up, were compared.
2.3.3. Analysis
A confirmatory factor analysis (CFA) applying SPSS Amos version 22 was conducted. A linear regression model was applied to predict donation intention within 3 weeks, included interventions, demographic variables, and variables of interest. Analysis of variance (ANOVA) and analysis of covariance (ANCOVA) were used. The R Project for Statistical Computing (R version 3.6.1) was also used. For intention‐to‐treat (ITT) analysis, the actual donation rate was calculated by dividing the number of all participants who donated again during the follow‐up period by the corresponding number of initially randomized SWBDs. Estimation of the effects of the interventions on SWBDs while accounting for compliance with assigned intervention was also conducted.
Previous studies defined four compliance types on the basis of individualsʼ treatment assignment status and potential treatment receipt status. 11 , 12 , 13 In this study, strict adherence to the intervention assignment meant that those in the control group did not receive any message containing questionnaire link; meanwhile, participants in Group 1 did not receive a message containing the Questionnaire 2 link and vice versa. Thus, this was a one‐sided noncompliance situation, with only compliers (who completed the questionnaire successfully in the intervention groups, and who were in the control group) and never‐takers (who did not complete the questionnaire in the intervention groups). 11 Therefore, the average treatment effect on the treated (ATT) was also estimated. 11 R Package “ATE” was used to estimate the ATT among compliers (those who completed the questionnaires and those who were in the control group) under the intervention and control conditions (random assignment was used as an instrumental variable where Group 1 or Group 2 was coded as 1, the control group was coded as 0, the complier in Group 1 or Group 2 was coded as 1, and the never‐taker and those in the control group were coded as 0).
2.3.4. Ethical considerations
All of the procedures were reviewed and approved by the ethics committee (Institutional Review Board of the Guangzhou Blood Center; approval number: 20200306). Digital informed consent was obtained from all of the participants before they completed the questionnaires. These were low‐risk studies comparing operational recruitment techniques that would have been applied to the donors in any case other than randomization; in addition, all of the data were processed anonymously. All of the participants were not informed of the study goals and were not given explanations about the nature of the interventions; otherwise, they might have altered their return behavior and compromised the results of the trial. The ethics committee approved the digital consent procedure for participants and this single‐blind method. Before donation, staff from the blood center would ask all blood donors to provide their cell phone number in the registration form and explain to donors that blood test results and recruitment message would be delivered to them, but they had the authority to refuse to provide their cell phone number. If they received the text message from the blood center and no longer wanted to receive these messages, they could opt out by replying to the text message with the letter T.
3. RESULTS
3.1. The observational study
As of 31 March 2020, 1501 cases of COVID‐19 were confirmed positive by nucleic acid testing in Guangdong Province, with 440 confirmed in Guangzhou. There were 56 and 57 blood donors who had donated whole blood 1 month after they donated platelets during 1 January to 31 March, in 2019 and 2020, respectively. No blood donors donated platelets after they had donated whole blood when they reached the donation interval, whereas platelet donors repeated platelet donation during the same time period in both 2019 and 2020. Therefore, the number of whole blood donations equaled the number of whole blood donors. Figure 2 shows that compared with 2019, the total number of whole blood donors in 2020 decreased dramatically from Week 3, and the number of SWBDs in 2020 was smaller than that in 2019 except for the first week. The Spring Festival vacation was held from 4 February 2019 to 10 February 2019, and from 24 January 2020 to 2 February 2020 (the Spring Festival vacation was usually 7 days, but the national government lengthened the vacation this year in consideration of the epidemic). During that time, the number of blood donors decreased 3 weeks before the vacation, and no group donation occurred during the vacation. In response to calls for blood, however, hospitals were the first agencies to organize group donations at Week 6. The number of GWBDs from hospitals in 2020 was higher than in 2019. Starting in Week 9, the number of GWBDs (nonhospital groups) in 2020 was also higher than in 2019. There was no group platelet donation during this period in 2020. The number of platelet donations in 2020 decreased and, beginning in Week 4, never caught up with the number of donations in 2019. Appendices [Link], [Link] present the comparisons of detailed information for blood donations made during the same period in 2019 and 2020. Note that both proportions of female whole blood donors from hospitals in 2019 and 2020 were larger than that from street and nonhospital groups.
FIGURE 2.
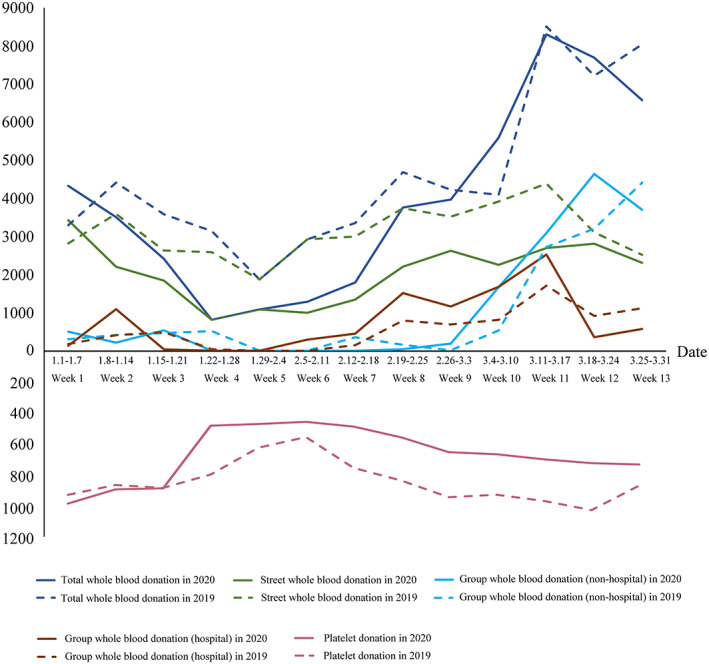
Blood collection trends in Guangzhou, China, from 1 January 2020 to 31 March 2020, compared with the same time period in 2019 [Color figure can be viewed at wileyonlinelibrary.com]
Figure 3 shows changes in blood collection in relation to some important events. After sending recruitment cell phone text messages on 30 January to experienced blood donors, the number of SWBDs increased. When the blood shortage message was broadcasted to the public, hospitals organized blood donation activities and mobilized medical staff to donate blood. On 20 February, Guangzhou Blood Center broadcasted an appeal encouraging people to donate blood through various media channels, and the number of both whole blood and platelet donors increased. Beginning on 5 March, the Guangdong government released an official announcement advocating governmental institutions to organize blood donation, and the number of GWBDs has increased ever since.
FIGURE 3.
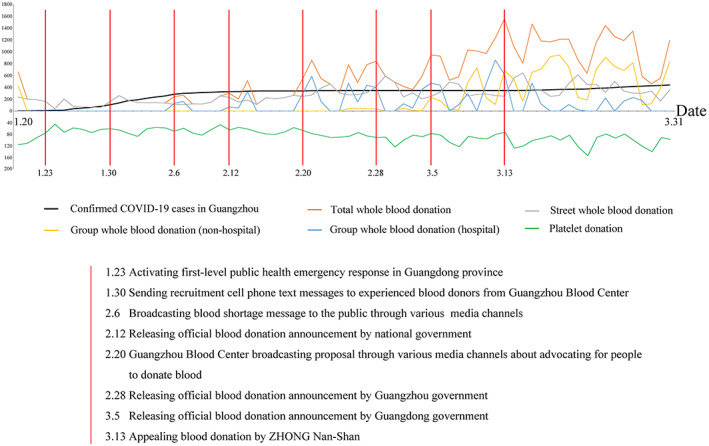
Blood collection trends in relation to the number of confirmed cases of COVID‐19 from 20 January 2020 to 31 March 2020 in Guangzhou, China [Color figure can be viewed at wileyonlinelibrary.com]
3.2. The cross‐sectional survey
Appendix S3 presents the comparisons of the 9117 first‐time and repeat SWBDs who received the questionnaire by sex and age in the cross‐sectional survey. There were 1685 (18.5%) SWBDs who completed the questionnaire, and 1584 (94.0%) of the questionnaires were valid. Validity was determined by those who provided the right answer to the test question: This is a test question—please select the number that corresponds to the current month. Questionnaire respondents included 291 (18.4%) first‐time SWBDs and 1293 (81.6%) repeat SWBDs. No data were missing because of the nature of the digital questionnaire. In Appendix S4, demographic information and relational closeness 14 , 15 (“Have any of your family members or close friends ever received a blood transfusion or been waiting for blood during this epidemic?”) among participants is provided. The mean and the standard error of donation frequency among all participants was 6.5 ± 6.7 (mean ± SD).
3.2.1. Exploratory factor analysis
The reliability of the questionnaire was acceptable (Cronbachʼs alpha was 0.73 for all 5‐point scale items). An EFA with a Varimax (orthogonal) rotation (Kaiser‐Meyer‐Olkin = 0.83, Bartlettʼs test P < .001) of these items resulted in four factors with a total variance of 55.1% (Appendix S5). Five items were removed from the questionnaire because their common factor variances were <0.3 (Appendix S6). The results of the EFA for the final 13 items of the questionnaire (Appendices S7 and S8) produced four factors (Appendix 3): concern about COVID‐19 epidemic (concern, Cronbachʼs alpha of 0.73), perceived knowledge about blood donation (perceived knowledge, 0.92), perception of blood need during the COVID‐19 epidemic (perception of blood need, 0.86), and COVID‐19 infection risk related to making a blood donation (donation risk, 0.83). The four factors explained 67.8% of the variance. The corresponding items were averaged for analyses.
3.2.2. Comparison of factors between first‐time and repeat SWBDs
Table 1 shows the independent‐sample t test results of the four factors between first‐time and repeat SWBDs. First‐time SWBDs were more concerned about the epidemic and perceived a higher risk of infection related to blood donation during the epidemic compared with repeat SWBDs, and repeat SWBDs thought they knew more about blood donation than first‐time SWBDs. Both of them shared the same opinions about the level of blood need in Guangzhou during the epidemic.
TABLE 1.
Independent‐sample t test results of the four factors between first‐time and repeat SWBDs in the survey
| Factors | First‐time SWBDs | Repeat SWBDs | t 1582 | P |
|---|---|---|---|---|
| Concern | 3.02 ± 0.94 | 2.80 ± 0.94 | 3.61 | <.001 |
| Perceived knowledge | 3.51 ± 1.01 | 4.19 ± 0.74 | −13.08 | <.001 |
| Perception of blood need | 4.01 ± 0.69 | 4.02 ± 0.53 | −0.32 | .746 |
| Donation risk | 2.24 ± 0.81 | 2.12 ± 0.75 | 2.32 | .020 |
SWBDs, street whole blood donors.
Appendix S9 shows the relationships between factors and SWBDʼs characteristics. Concern was positively associated with being male and negatively associated with education level and donation frequency. Perceived knowledge was positively associated with age, donation frequency, and relational closeness. Perception of blood need was positively associated with education level and relational closeness. Donation risk was negatively associated with age.
3.2.3. Comparison of the latest blood donation purposes between first‐time and repeat SWBDs
Appendix S10 compared the purpose of the latest blood donation between first‐time and repeat SWBDs. Both of them gave the highest score to the purpose of saving lives.
3.3. The randomized controlled trial
A total of 1060 (1060/12994, 8.2%, group 1 = 518, group 2 = 540) questionnaires were collected on 13 March 2020. Those who gave the wrong answer to the test question were excluded (Group 1 = 24, Group 2 = 49), and 986 were analyzed (Group 1 = 495, Group 2 = 491). A χ2 test showed that there were significantly more valid questionnaires in Group 1 than in Group 2 (95.6% vs 90.9%; P = 0 .004). Appendix S11 shows the details of the demographic information, donation frequency, and relational closeness among participants. Participants in Group 1 expressed a greater willingness to donate within 3 weeks (M = 3.46, SD = 1.20) than those in group 2 (M = 3.14, SD = 1.12; t 984 = 4.35, P < .001).
3.3.1. Confirmatory factor analysis
A CFA model (χ2 (48) = 180.55, P < .001, normed fit index = 0.97, comparative fit index = 0.98, root mean square error of approximation = 0.05) showed that factor loadings were all >0.50, which were considered to be meaningful given that no item was excluded (Appendix S12). 16 The minimum square root of average value explained (0.76) was larger than the maximum interconstruct correlation coefficient (0.31), which indicated there was discriminant validity (Appendix S13). The overall reliability of the questionnaire was 0.72. Four factors also formed acceptable reliable scales (concern, α = 0.84; perceived knowledge, α = 0.86; perception of blood need, α = 0.87; donation risk, α = 0.84), and the items were averaged for analyses.
3.3.2. Comparison of factors between SWBDs in Groups 1 and 2
Independent‐sample t test results of the four factors between SWBDs in Groups 1 and Group2 are shown in Table 2. SWBDs in Group 1 perceived a higher level of blood need and a lower risk of COVID‐19 infection related to making a blood donation during this epidemic. The difference in levels of concern about the epidemic and perception of blood donation knowledge were not significant between Group 1 and Group 2.
TABLE 2.
Independent‐sample t test results of the four factors between experienced SWBDs in Groups 1 and 2
| Factors | Group 1 | Group 2 | t 984 | P |
|---|---|---|---|---|
| Concern | 3.05 ± 0.93 | 3.03 ± 0.90 | 0.41 | .681 |
| Perceived knowledge | 3.91 ± 0.88 | 3.89 ± 0.39 | 0.41 | .682 |
| Perception of blood need | 3.95 ± 0.61 | 3.77 ± 0.64 | 4.71 | <.001 |
| Donation risk | 2.50 ± 0.79 | 2.71 ± 0.85 | −4.09 | <.001 |
SWBDs, street whole blood donors.
3.3.3. Considering blood donation within 3 weeks
Table 3 presents the linear regression model (forced‐entry method) predicting SWBDsʼ intention to donate within 3 weeks, and Appendix S14 shows that there is no obvious multicollinearity. Donation intention was positively associated with completing Questionnaire 1, being female, perception of having more knowledge about blood donation, perceiving a higher level of blood need, and perceiving a lower risk of COVID‐19 infection related to making a blood donation. Appendix S15 reports the correlations for the variables.
TABLE 3.
Linear regression model for predicting experienced SWBDsʼ donation intention within 3 weeks
| Predictor | β | SE | t | P | Tolerance | VIF |
|---|---|---|---|---|---|---|
| Constant | 1.99 | 0.37 | 5.44 | <.001 | ||
| Group | ||||||
| 1 | 0.22 | 0.07 | 3.04 | .002 | 0.96 | 1.05 |
| 2 | Reference | |||||
| Sex | ||||||
| Male | −0.18 | 0.07 | −2.38 | .018 | 0.94 | 1.07 |
| Female | Reference | |||||
| Age | 0.01 | 0.00 | 1.92 | .055 | 0.72 | 1.40 |
| Education level | −0.02 | 0.05 | −0.33 | .741 | 0.92 | 1.08 |
| Donation frequency | 0.00 | 0.01 | 0.45 | .653 | 0.77 | 1.29 |
| Relational closeness | ||||||
| Yes | 0.04 | 0.07 | 0.50 | .615 | 0.99 | 1.01 |
| No | Reference | |||||
| Concern | 0.02 | 0.04 | 0.52 | .605 | 0.85 | 1.17 |
| Perceived knowledge | 0.22 | 0.04 | 4.99 | <.001 | 0.88 | 1.13 |
| Perception of blood need | 0.21 | 0.05 | 4.16 | <.001 | 0.86 | 1.16 |
| Donation risk | −0.23 | 0.05 | −4.72 | <.001 | 0.76 | 1.31 |
| Total R 2 = 0.13 | ||||||
SWBDs, street whole blood donors.
Groups and relational closeness
An independent‐sample t test showed that relational closeness was not significantly associated with donation intention (P = .343). A 2 × 2 (group × relational closeness) ANOVA was performed. There was a main effect of groups (F(1985) = 18.08, P < .001, η2 = 0.02), but not of relational closeness (P < .364), but there was a significant interaction between group and relational closeness (F(1985) = 4.82, P = .028, η2 = 0.01). The pairwise comparison demonstrated that SWBDs in Group 1 who had any family members or close friends who had ever received a blood transfusion or had been waiting for blood during this epidemic (3.6 ± 0.07) were more likely to donate within 3 weeks than those who did not (3.3 ± 0.08, P < .001), but there was no significant difference among the SWBDs in Group 2.
Groups and concern
A linear regression model showed that concern about the COVID‐19 epidemic was not significantly associated with donation intention (P = .576). An ANCOVA was conducted, with donation intention as the dependent factor, groups serving as the between‐subjects factor, and concern as the covariate (continuous, mean‐centered). The main effect for groups was significant (F(1985) = 19.01, P < .001, η2 = 0.01) but not for concern about the epidemic (P = .541), and there was no significant interaction (P = .798).
Groups and perceived knowledge
The linear regression model showed that perceived knowledge of blood donation was positively correlated with donation intention that donors perceiving they had more knowledge would be more likely to donate (F(1985) = 59.65, β = .33, P < .001, R2 = 0.06). An ANCOVA was conducted, with donation intention as the dependent factor, groups serving as the between‐subjects factor, and perceived knowledge as the covariate (continuous, mean‐centered). The main effects of both groups (F(1985) = 18.97, P < .001, η2 = 0.02) and perceived knowledge (F(1985) = 60.01, P < .001, η2 = 0.06) were significant, and there was no significant interaction (P = .666).
Groups and perception of blood need
Following the procedures identified by Baron and Kenny, 17 the regression of perception of blood need on groups was significant. Regressing donation intention onto groups also reached significance. Finally, regressing donation intention onto both groups and perception of blood need still reached significance that message framing was reduced in size (Appendix S16). In addition, a 95% confidence interval (CI) computed around the indirect pathway (bootstrap) did not include zero (95% CI, 0.02‐0.03), which indicated a significant mediating role for the perception of blood need. In total, perception of blood need in Guangzhou during the epidemic partially mediated the relationship between group and donation intention. Thus, completion of Questionnaire 1 created a higher level of blood need that contributed to greater intention to donate.
Groups and donation risk
The same method was applied to detect mediational effect of donation risk (Appendix S17). In addition, a 95% CI computed around the indirect pathway (bootstrap) did not include zero (95% CI, 0.02‐0.05). Therefore, donation risk was also a partial mediator in the relationship between group and donation intention. Completion of Questionnaire 1 made SWBDs perceive a lower risk of COVID‐19 infection related to making a blood donation and these SWBDs were more likely to donate within 3 weeks.
3.3.4. Actual donation behavior among three groups
Among those who completed the questionnaires in Groups 1 and Group2, 38 (38/518, 7.34%) and 31 (31/540, 5.74%) SWBDs donated blood within 3 weeks, respectively. In the ITT analyses, significant differences were observed only between Group 1 and Group 3 (Table 4). The ATT estimation results, however, showed that among those who completed the questionnaires, completing Questionnaire 1, which contained the information, was estimated to significantly increase redonation by 4.7 percentage points compared with completing Questionnaire 2 within 3 weeks, and to increase redonation by 5.5 compared with no intervention; completing Questionnaire 2 was estimated to significantly increase redonation by 4.0 percentage points compared with no intervention (Table 5). Logistic regression analyses indicated that redonation during the epidemic was positively associated with age, donation history, and successfully completing the questionnaires (Appendix S18).
TABLE 4.
Comparisons of actual donation behavior among all participants during 3‐week follow‐up by ITT analyses in the trial
| Group | Actual donation rate (%, n) | Comparison | χ2 Raw P | Bonferroni corrected P | |
|---|---|---|---|---|---|
| Within 1 week | 1 | 1.14 (74/6497) | 1 vs 2 | .191 | .222 |
| 2 | 0.91 (59/6497) | 2 vs 3 | .111 | .136 | |
| 3 | 0.66 (43/6497) | 1 vs 3 | .004 | .005 | |
| Within 2 weeks | 1 | 1.69 (110/6497) | 1 vs 2 | .731 | .783 |
| 2 | 1.62 (105/6497) | 2 vs 3 | .053 | .063 | |
| 3 | 1.22 (79/6497) | 1 vs 3 | .023 | .028 | |
| Within 3 weeks | 1 | 2.25 (146/6497) | 1 vs 2 | .547 | .587 |
| 2 | 2.09 (136/6497) | 2 vs 3 | .082 | .094 | |
| 3 | 1.68 (109/6497) | 1 vs 3 | .019 | .028 |
ITT, intention‐to‐treat.
TABLE 5.
Comparisons of actual donation behavior among three groups by ATT estimations in the trial
| Point estimate | Standard error | 95% CI | Z | P | |
|---|---|---|---|---|---|
| Group 1 vs Group 2 | 0.047 | 0.008 | 0.032‐0.062 | 6.16 | <.001 |
| Group 1 vs Group 3 | 0.055 | 0.012 | 0.033‐0.078 | 4.77 | <.001 |
| Group 2 vs Group 3 | 0.040 | 0.010 | 0.020‐0.060 | 3.92 | <.001 |
ATT, average treatment effect on the treated; CI, confidence interval.
3.3.5. Comparison of common factors between SWBDs in the survey and the trial
Appendix S19 shows that SWBDs who did not donate during the epidemic expressed more concern about the epidemic and felt a higher risk of COVID‐19 infection related to making a blood donation. SWBDs who donated during the epidemic perceived more blood need in Guangzhou and believed they knew more about blood donation.
4. DISCUSSION
A blood shortage crisis triggered by infectious disease occurred in Beijing, China, during the SARS epdemic. 18 After measures were implemented in Beijing, significant numbers of blood products from other Chinese regions were imported to ensure blood availability for clinical use between April and early July during that epidemic. 18 During the COVID‐19 outbreak, this same situation occurred across China. Although the situation was more severe than in 2003, blood shortage was mitigated in a short period. The observational study showed that along with measures implemented, the number of both whole blood donors and platelet donors increased accordingly. The cross‐sectional survey indicated that both first‐time and repeat SWBDs perceived the same level of blood need and donated blood to save lives. The randomized controlled trial revealed that making blood donors perceive a higher level of blood need and a lower level of COVID‐19 infection risk related to making a blood donation could mobilize experienced SWBDs to donate within 3 weeks. SWBDs who completed Questionnaire 1 expressed a greater intention to donate during the epidemic. ITT analyses and ATT estimations confirmed that Questionnaire 1 could activate SWBDs to make an actual donation.
Group and street blood donations ensure sufficient blood supply in Guangzhou. Although group blood donation accounted for 31% of the total donations, group blood donation is more reliable than street blood donation. In ordinary times, universities guarantee the blood supply from March to June and September to December (two semesters). Universities would hold blood donation activities during semesters to organize their students to donate. Nonhospital groups and hospitals would organize blood donation activities from January to March and June to September. Guangzhou is one of cities that has the biggest immigrant population (9.53 million; 62.3%), with people from all over China. The Spring Festival is a traditional festival and the most important festival in China; people from outside Guangzhou return to their hometowns 1 to 3 weeks before the festival vacation. Coupled with the cold weather, therefore, the number of both street and group blood donations would begin to decrease 3 weeks before the Spring Festival. At this time, because mutual (family/replacement) blood donation was canceled, blood supply was strictly controlled to ensure emergency use; patients needing elective surgery or suffering from nonlethal anemia must wait for blood. Both public and private hospitals would organize blood donation activities when blood products were insufficient. Medical staff might be more likely to be aware of the important and precious nature of blood. 19 Also, medical staff affiliated with hospitals must remain at their posts at all times, even during the Spring Festival vacation. Therefore, medical staff members are the primary blood resource when facing an emergency situation. During this epidemic, groups followed government instructions to organize blood donation activities, and hospitals were the first responders, which effectively replenished the stockpile of blood. To some extent, medical staff taking the lead to donate blood served as a good example for street and group blood donors who were lacked a medical background. Hospitals will continue to play a vital role in blood donation even after the epidemic.
First‐time and repeat SWBDs sensed an urgent need for blood and decided to donate to save lives during the epidemic. The result of the cross‐sectional survey was in line with previous studies that found when blood donors feel a sense of urgency to donate blood, they probably take the action. 20 , 21 , 22 SWBDs who donated during the epidemic felt less concern about the epidemic and perceived a lower risk of COVID‐19 infection related to making a blood donation. They also perceived more blood need in Guangzhou and felt they had more knowledge about blood donation than those SWBDs who did not donate. These results further confirmed the findings noted previously.
Using the questionnaire to recruit lapsed blood donors proved to be effective. 23 Additionally, the randomized trial confirmed that completing a questionnaire regardless of whether it contained or did not contain information about blood donation precautionary measures in response to COVID‐19 and other messages about blood donation during the epidemic could motivate experienced SWBDs to make a subsequent donation. Questionnaire 1 was actually promotional material aimed at eliminating SWBDsʼ concerns about transmission of COVID‐19 infection during a blood donation. Completion of the questionnaire significantly increased both donation intention and actual donation behavior. This questionnaire could be applied to recruit blood donors during the COVID‐19 epidemic and could be used to recruit blood donors as a reference during a future epidemic.
The strength of this study was that it was the first research to apply a questionnaire to understand factors affecting blood donors who donated during an epidemic and to recruit experienced blood donors to redonate during such a period. Another strength of the study was that the actual behavior of donors was assessed to determine the effectiveness of the intervention rather than a self‐reported behavior.
Some limitations need to be addressed. First, the COVID‐19 epidemic in Guangzhou was severe but not as severe as it was in Wuhan, Hubei Province. Thus, the results might not suitably be extended to the worst‐hit areas during an epidemic. Second, the questionnaire in the cross‐sectional survey was not based on previous validated questionnaires, and because of the time limitation, it was not pretested to assess the clarity of the questionnaire or the suitability and consistency for participants. Third, in the randomized controlled trial, all of the questionnaires were anonymous for the sake of privacy protection, and the actual donation behavior could not be matched precisely to blood donation intention. Fourth, the survey and the trial focused only on whole blood donors and platelet donors might have different opinions on blood donation during the epidemic. Finally, the questionnaire links were closed in a short period and additional participants might have intended to complete the questionnaire. Therefore, future research that increases the questionnaire collection time is needed to explore the effectiveness of using a questionnaire to recruit blood donors during an epidemic. Moreover, the sex ratio was 100:99.58 for female citizens vs male citizens in 2018 in Guangzhou, 24 but the ratio of female blood donors vs male blood donors was 54.21:100. There were more female blood donors from the hospitals both in 2019 and 2020; it may be worth studying whether this difference was simply because more female medical staff (nurses are mostly women) worked in hospitals or whether the blood donation intentions between female medical staff and ordinary citizens were different. Also, research focused on street blood donors and group blood donors responding to public health events simultaneously could be addressed.
In conclusion, the blood shortage during COVID‐19 epidemic in Guangzhou was solved by recruiting experienced blood donors through the blood center, mass media campaigns, and advocating groups to organize blood donation activities by government at all levels. Both first‐time and repeat SWBDs perceived the same level of blood need and donated blood to save lives during the epidemic. The questionnaire with information about blood donation precautionary measures in response to COVID‐19 and other messages about blood donation during the epidemic successfully increased the blood donation intention of experienced SWBDs, and even increased actual blood donation during the COVID‐19 epidemic. The results are specific to data that come from Guangzhou, but we believe many of the insights are true for China in general and are informative with regard to the international public health response.
CONFLICT OF INTEREST
The authors declare no potential conflict of interest.
Supporting information
Appendix S1. Supporting information.
Appendix S2. Supporting information.
Appendix S3. Supporting information.
Appendix S4. Supporting information.
Ou‐Yang J, Li S‐J, Bei C, et al. Blood donor recruitment in Guangzhou, China, during the 2019 novel coronavirus (COVID‐19) epidemic. Transfusion. 2020;60:2597–2610. 10.1111/trf.15971
Jian Ou‐Yang and Shi‐Jie Li contributed equally to this work.
Funding information Medical Science and Technology Research Foundation of Guangdong Province 2020, Grant/Award Number: B2020141; Natural Science Foundation of Guangdong Province 2019, Grant/Award Number: 2019A1515011505; The Key Medical Disciplines and Specialties Program of Guangzhou
REFERENCES
- 1. National Bureau of Statistics of China . Annual by Province 2019. [accessed 2020 Jun 2] Available from: http://data.stats.gov.cn/english/easyquery.htm?cn=E0103.
- 2. Simonetti A, Ezzeldin H, Walderhaug M, et al. An inter‐regional US blood supply simulation model to evaluate blood availability to support planning for emergency preparedness and medical countermeasures. Disaster Med Public Health Prep 2018;12:201‐10. [DOI] [PubMed] [Google Scholar]
- 3. Veronica H, Philip K, Yan Q, et al. APBN Rapid Brief White Paper: 2019 Novel Coronavirus (SARS‐CoV‐2); Expected Challenges and Risks to Blood Safety, Manila, Philippines: Asia Pacific Blood Network; 2020. [Google Scholar]
- 4. Karacan E, Cengiz Seval G, Aktan Z, et al. Blood donors and factors impacting the blood donation decision: motives for donating blood in Turkish sample. Transfus Apher Sci 2013;49:468‐73. [DOI] [PubMed] [Google Scholar]
- 5. Sugden N, King N. A descriptive phenomenological analysis of the experience of blood donation as a regular donor. J Health Psychol 2019:1359105319890014. 10.1177/1359105319890014. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 6. Tey YS, Arsil P, Brindal M, et al. Motivation structures of blood donation: a means‐end chain approach. Int J Health Econ Manag 2020;20:41‐54. [DOI] [PubMed] [Google Scholar]
- 7. Ferguson E. Mechanism of altruism approach to blood donor recruitment and retention: a review and future directions. Transfus Med 2015;25:211‐26. [DOI] [PubMed] [Google Scholar]
- 8. Huis in ʻt Veld EM, de Kort WL, Merz EM. Determinants of blood donation willingness in the European Union: a cross‐country perspective on perceived transfusion safety, concerns, and incentives. Transfusion 2019;59:1273‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Guangzhou Blood Center . PAss Aladdin System of Blood Collection and Supply. Passsoft CO. LTD.; 2020.
- 10. Ou‐Yang J, Bei CH, He B, et al. Factors influencing blood donation: a cross‐sectional survey in Guangzhou, China. Transfus Med 2017;27:256‐67. [DOI] [PubMed] [Google Scholar]
- 11. Frölich M, Melly B. Identification of treatment effects on the treated with one‐sided non‐compliance. Econom Rev 2013;32:384‐414. [Google Scholar]
- 12. Holland Paul W. Statistics and causal inference. J Am Stat Assoc 2012;81:945‐70. [Google Scholar]
- 13. Frangakis CE, Rubin DB. Principal stratification in causal inference. Biometrics 2015;58:21‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cialdini RB, Brown SL, Lewis BP, et al. Reinterpreting the empathy‐altruism relationship: when one into one equals oneness. J Pers Soc Psychol 1997;73:481‐94. [PubMed] [Google Scholar]
- 15. Chou EY, Murnighan JK. Life or death decisions: framing the call for help. PLoS One 2013;8:e57351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Floyd FJ, Widaman KF. Factor analysis in the development and refinement of clinical assessment instruments. Psychol Assess 1995;7:286‐99. [Google Scholar]
- 17. Baron RM, Kenny DA. The moderator‐mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 1986;51:1173‐82. [DOI] [PubMed] [Google Scholar]
- 18. Shan H, Zhang P. Viral attacks on the blood supply: the impact of severe acute respiratory syndrome in Beijing. Transfusion 2004;44:467‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Malako D, Yoseph F, Bekele ML. Assessment of knowledge, attitude and practice and associated factors of blood donation among health care workers in Ethiopia: a cross‐sectional study. BMC Hematol 2019;19:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wevers A, Wigboldus DH, Van Den Hurk K, et al. Increasing first‐time blood donation of newly registered donors using implementation intentions and explicit commitment techniques. Vox Sang 2015;108:18‐26. [DOI] [PubMed] [Google Scholar]
- 21. Duboz P, Cuneo B. How barriers to blood donation differ between lapsed donors and non‐donors in France. Transfus Med 2010;20:227‐36. [DOI] [PubMed] [Google Scholar]
- 22. Hughes JD, Hernandez MC, Jenkins DH, et al. Survey of medical center employeesʼ willingness and availability to donate blood in support of a civilian warm fresh whole blood program. Am J Disaster Med 2019;14:101‐11. [DOI] [PubMed] [Google Scholar]
- 23. Godin G, Germain M, Conner M, et al. Promoting the return of lapsed blood donors: a seven‐arm randomized controlled trial of the question‐behavior effect. Health Psychol 2014;33:646‐55. [DOI] [PubMed] [Google Scholar]
- 24. Guangzhou Statistics Bureau . Statistical Yearbook 2019. Population. Guangzhou, China: Guangzhou Statistics Bureau; 2019.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Supporting information.
Appendix S2. Supporting information.
Appendix S3. Supporting information.
Appendix S4. Supporting information.


