Prior studies on proning awake, nonintubated patients with hypoxemic acute respiratory failure, 1 , 2 as well as evolving study of similar COVID‐19 patients, 3 , 4 , 5 , 6 coupled with experience and dramatic anecdotal evidence from the COVID‐19 pandemic, suggest the importance of proning all such patients with COVID‐19 to improve oxygenation and reduce respiratory effort. Literature and experience from health care teams in the midst of the pandemic suggest that any COVID‐19 patients with respiratory compromise severe enough to warrant admission should be considered for proning. We additionally suggest that these patients should be considered for proning as well as ongoing patient repositioning (e.g., right lateral decubitus, seated, and left lateral decubitus positions). Figure 1 represents the proning and positioning instructions developed at New York City Health + Hospitals/Elmhurst, a large, inner‐city, tertiary public hospital in the epicenter of the COVID‐19 pandemic in New York City and later adapted and utilized at facilities across the United States.
Figure 1.
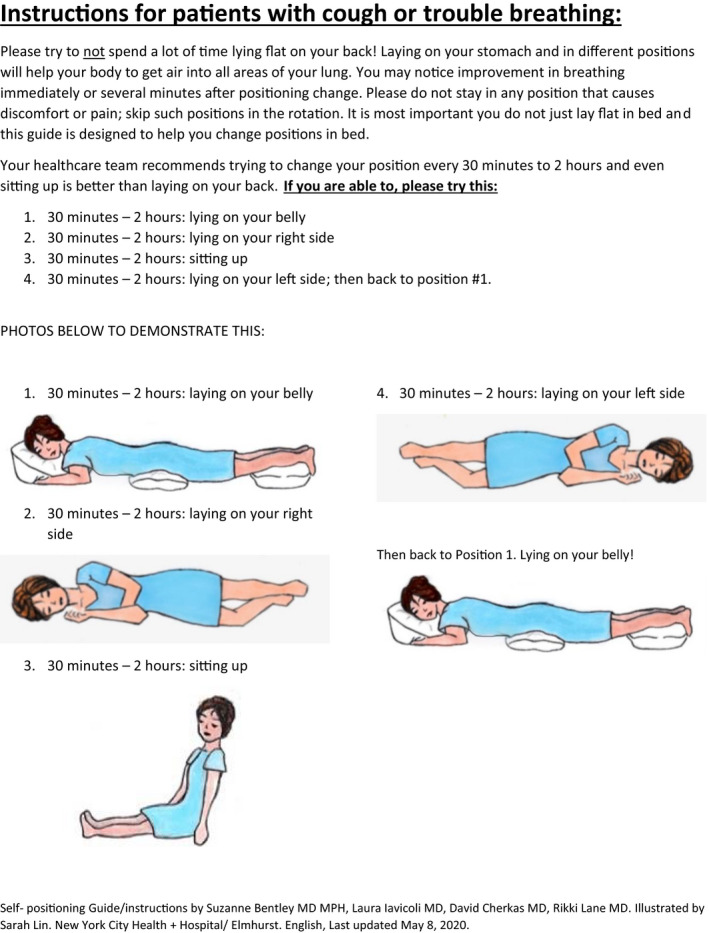
Patient handout.
Additionally, we suggest the use of these proning and repositioning instructions for mild and discharged COVID‐19 patients to be completed independently. Mild COVID‐19 patients often still have respiratory involvement that may benefit from these exercises. Studies are needed to evaluate if it may also stave off disease progression. Like all medical interventions, it remains a risk/benefit analysis and such positioning most commonly presents very little risk in appropriately selected patients. The Intensive Care Society Guidance for Prone Positioning of the Conscious COVID‐19 Patient 7 includes the following absolute contraindications: acute respiratory distress (requiring higher level intervention, e.g., immediate need for intubation), hemodynamic instability, agitation or altered mental status, unstable spine, thoracic injury, or recent abdominal surgery. Relative contraindications to consider include facial injuries, neurologic conditions (e.g., seizure disorder), morbid obesity, pregnancy due to gravid abdomen, and pressure sores/ulcers or high risk for pressure sores/ulcers due to positioning.
New York City Health + Hospitals/Elmhurst successfully developed and implemented the proning and positioning guide with awake, nonintubated patients as well as provided it to patients suspicious for or with confirmed COVID‐19 who were discharged from the emergency department (ED). The guide was developed via expert consensus of an interdisciplinary team of emergency medicine physicians and physical therapists and iteratively revised based on usability testing and understandability feedback from providers and patients, with whom it was piloted through several rounds of revisions. Distribution of the guide was implemented by the emergency medicine team and physical therapist collaborating in the department and provided to ED patients awaiting admitted bed availability and was utilized by the majority of appropriate patients in the ED independently (occasionally with verbal reminders). Majority of awake, nonintubated moderately ill COVID‐19 patients in the ED are on continuous pulse oximetry monitoring and patients have oxygen saturation, oxygen requirement (e.g., number of liters oxygen via nasal cannula), and position recorded hourly on a sheet attached at patient bedside (Figure 2). A vital signs documentation sheet was in use in the department and a column was added to denote patient positioning upon development of this proning guidance.
Figure 2.
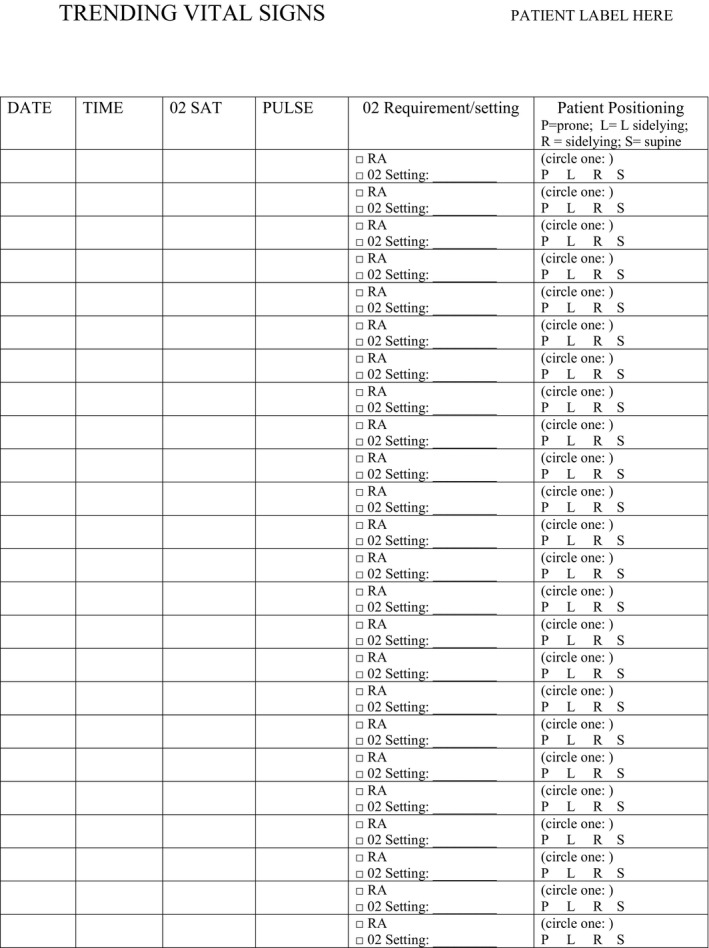
Vital signs and positioning flowsheet.
For patients in the ED, inclusion criteria for recommending self‐conducted repositioning and proning began if oxygen saturation was < 92% (including if < 92% on room air prior to improved saturation with oxygen delivery while in ED) and patient deemed to be independent in bed mobility (Figure 3). Patients requiring noninvasive ventilation (BiPAP or CPAP) in the department were generally encouraged to side lie and sit up; however, proning and repositioning was accomplished with many of these patients in conjunction with direct assistance by the physical therapy team or other health care team members due to concern about mask or equipment dislodging with proning independently.
Figure 3.
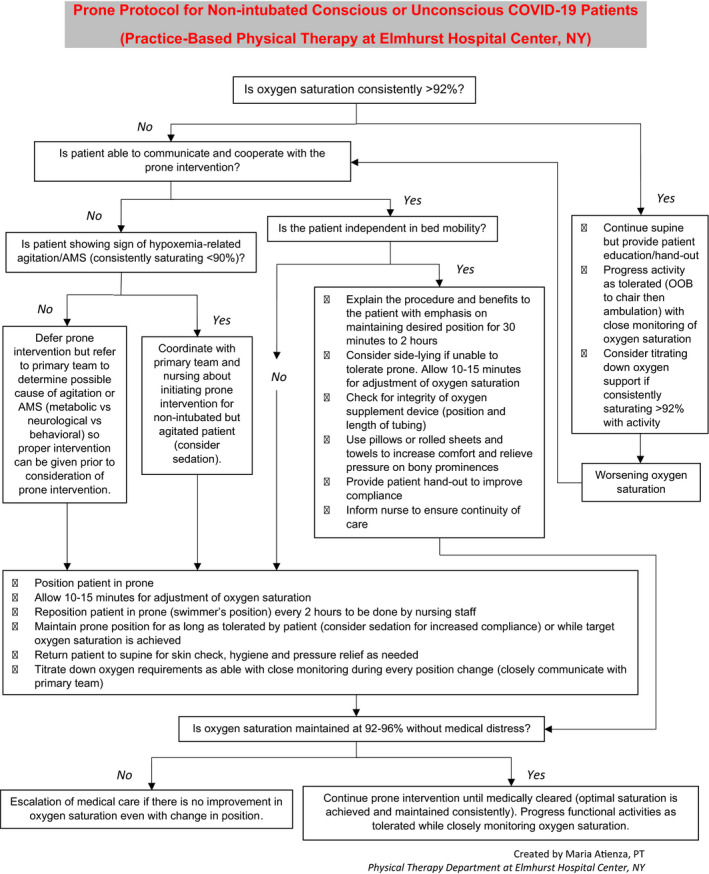
Prone algorithm.
The procedure and highlighted benefits should be explained to the patient, emphasizing goal to maintain each position for 30 minutes to 2 hours. Specific illustrated instructions were provided via patient handout (Figure 1). If a patient does not tolerate lying prone or a specific position, then alternative positions are encouraged and patients are reminded not to stay in any positions of discomfort. Ten to 15 minutes are allotted for adjustment in oxygen saturation and saturations and positions were recorded as noted above (Figure 2). If no improvement in oxygen saturation with a change in position, escalation of medical care is necessary. Generally, patients that desaturate, look uncomfortable, or request assistance to change position should all be urgently repositioned with repeat saturation monitoring until patient is in a position of comfort with improvement in saturation. It is prudent for staff to check for integrity of oxygen delivery device (e.g., position and length of tubing) after position changes or immediately if oxygen desaturation. Additionally, using pillows or rolled sheets and towels can increase comfort and relieve pressure on bony prominences. All members of patient care team must be made aware patients have been encouraged to self‐position and prone.
In conclusion, awake, nonintubated patients appear to greatly benefit from self‐proning and alternating positioning, with many being able to independently change positions without disrupting flow of oxygen. Special consideration for position changes in patients requiring noninvasive ventilation (BiPAP or CPAP) is required but patient positioning is similarly achievable in such patients with direct assistance from physical therapists or other health care team members.
The authors have no relevant financial information or potential conflicts of interest to disclose.
References
- 1. Scaravilli V, Grasselli G, Castagna L, et al. Prone positioning improves oxygenation in spontaneously breathing nonintubated patients with hypoxemic acute respiratory failure: a retrospective study. J Crit Care 2015;30:1390–4. [DOI] [PubMed] [Google Scholar]
- 2. Guérin C, Reignier J, Richard JC, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med 2013;368:2159–68. [DOI] [PubMed] [Google Scholar]
- 3. Caputo ND, Strayer RJ, Levitan R. Early self‐proning in awake, non‐intubated patients in the emergency department: a single ED's experience during the COVID‐19 pandemic. Acad Emerg Med 2020;27:375–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sun Q, Qiu H, Huang M, Yang Y. Lower mortality of COVID‐19 by early recognition and intervention: experience from Jiangsu Province. Ann Intensive Care 2020;10:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Slessarev M, Cheng J, Ondrejicka M, Arntfield R. Patient self‐proning with high‐flow nasal cannula improves oxygenation in COVID‐19 pneumonia. Can J Anesth 2020. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ding L, Wang L, Ma W, He H. Efficacy and safety of early prone positioning combined with HFNC or NIV in moderate to severe ARDS: a multi‐center prospective cohort study. Crit Care 2020;24:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bamford P, Bentley A, Dean J, Whitmore D, Wilson‐Baig N. ICS Guidance for Prone Positioning of the Conscious COVID Patient 2020. Available from: https://icmanaesthesiacovid-19.org/news/ics-guidance-for-prone-positioning-of-the-conscious-covid-patient-2020. Accessed May 27, 2020.


