The “coronavirus disease 2019 (COVID‐19)” outbreak was first reported in December 2019 (China). Since then, this disease has rapidly spread across the globe and in March 2020 the World Health Organization (WHO) declared the COVID‐19 pandemic. 1 Since the outbreak was first announced, our journal has extensively focused on the clinical features, outcomes, diagnosis, immunology, and pathogenesis of COVID‐19 and its infectious agent severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2). We published our first COVID‐19 article on 19 February, focusing for the first time on the clinical characteristics of 140 cases of human‐to‐human coronavirus transmission without any links to the Huanan Wet Market. 2 Hypertension and diabetes were mentioned as risk factors and there was no increased prevalence in allergic patients. This early study reported that the main symptoms at hospital admission were fever (91.7%), cough (75.0%), fatigue (75.0%), gastrointestinal symptoms (39.6%), and dyspnea (36.7%). Lymphopenia and eosinopenia were also reported as important signs and biomarkers for monitoring and severity of the patients. 2 The prevalent eosinopenia in COVID‐19 patients and the possible anti‐viral role of eosinophils were further discussed in several following publications in Allergy. 3 , 4 Our second COVID‐19 paper brought attention to the wide range of clinical manifestations of this disease, from asymptomatic cases to patients with mild and severe symptoms, with or without pneumonia as well as with only diarrhea. 5 Patients with common allergic diseases did not develop distinct symptoms and severe courses. Cases with pre‐existing chronic obstructive pulmonary disease or complicated with a secondary bacterial pneumonia were severe. Another article, timely appearing in our journal, alerted the scientific community that even in experienced hands there was a 14.1% false‐negative polymerase chain reaction (PCR) diagnosis in COVID‐19 cases and were later diagnosed positive after repeated tests. 6 A pediatric article was also published extensively analyzing 182 cases, and it was reported that children with COVID‐19 showed a mild clinical course. 7 Patients with pneumonia had a higher proportion of fever and cough and increased inflammatory biomarkers compared to those without pneumonia. There were 43 allergic patients in this series, and there was no significant difference between allergic and nonallergic COVID‐19 children in disease incidence, clinical features, laboratory, and immunological findings. Allergy was not a risk factor for disease and severity of SARS‐CoV‐2 infection and did not significantly influence the disease course of COVID‐19 in children. 7
The immunology of COVID‐19 was extensively reviewed in two articles from leading experts with a comprehensive discussion of the tip of the iceberg in COVID‐19 epidemiology, anti‐viral response, antibody response to SARS‐CoV‐2, acute phase reactants, cytokine storm, and pathogenesis of tissue injury and severity. 8 , 9
Two studies timely reported the role of possible trained immunity in countries with a Bacillus Calmette‐Guérin (BCG) vaccination program and a relatively low COVID‐19 prevalence and mortality rate. 10 , 11 In an extensive RNA sequencing analyses of SARS‐CoV‐2 receptor and their molecular partners revealed that ACE2 and TMPRSS2 were coexpressed at the epithelial sites of the lung and skin, whereas CD147 (BSG), cyclophilins (PPIA and PPIB), CD26 (DPP4) and related molecules were expressed in both, epithelium and in immune cells. 12
Allergists, respiratory physicians, pediatricians, and other healthcare providers treating patients with allergic diseases are frequently in contact with patients potentially infected with SARS‐CoV‐2. Practical considerations and recommendations given by experts in the field of allergic diseases can provide useful recommendations for clinical daily work. Since the beginning of this current pandemic, our journal has disseminated clinical reports, 2 , 3 , 5 , 6 , 13 statements on the urgent need for accuracy in designing and reporting clinical trials in COVID‐19, 14 preventive measures, 10 , 11 , 15 and Position Statements elaborated by experts in the field in close collaboration with the European Academy of Allergy and Clinical Immunology (EAACI) and the organization “Allergy and Its Impact on Asthma (ARIA)”. 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 27 (keynote information in Table 1). A compendium answering 150 frequently encountered questions regarding COVID‐19 and allergic diseases has been recently published by experts in their respective area (Figure 1). 28 In addition, readers can put further questions regarding this “living” compendium electronically to the authors and their answers will be available through a new category in the journal's web page. 29 Besides, EAACI in collaboration with ARIA, has provided recommendations on operational plans and practical procedures for ensuring optimal standards in the daily clinical care of patients with allergic diseases, while ensuring the safety of patients and healthcare workers. 23
Table 1.
Examples of recently published recommendations, statements, and Position Papers of the EAACI
| Clinical Topic | Keynote message(s) | Title and Reference |
|---|---|---|
| Asthma | Prescribed inhaled (or oral) corticosteroids as controller medication should be further applied to patients with asthma as cessation may lead to asthma exacerbations | ARIA‐EAACI statement on Asthma and COVID‐19 16 |
| Allergic rhinitis |
Intranasal corticosteroids (including nasal sprays) can be further applied in COVID‐19 patients at the recommended dosages, and a cessation or interruption is not recommended Furthermore, a cessation or interruption of allergen immunotherapy (AIT) for both the subcutaneous route (SCIT) or sublingual route (SLIT) is not recommended in asymptomatic patients without suspicion for SARS‐CoV‐2 infection and/or contact to SARS‐CoV‐2 positive individuals or in other conditions as outlined |
Intranasal corticosteroids in allergic rhinitis in COVID‐19‐infected patients: An ARIA‐EAACI statement 21 Handling of allergen immunotherapy in the COVID‐19 pandemic: An ARIA‐EAACI statement 22 |
| Biological‐Treatment |
Biologicals should be applied in type 2 inflammations (asthma, atopic dermatitis, chronic rhinosinusitis with nasal polyps, chronic spontaneous urticaria) via self‐application in noninfected patients In patient with an active SARS‐CoV‐2 infection treatment with biologicals should be paused and re‐initiated after recovery and SARS‐CoV‐2 negativity of patients |
Considerations on biologicals for patients with allergic disease in times of the COVID‐19 pandemic: an EAACI Statement 27 |
| Children |
Less severe courses of COVID‐19 in the pediatric population have been reported Similar to the adult age group, severe forms of asthma and immunodeficiencies are reported to be risk factors A sufficient control of symptoms in children with allergies, asthma and immunodeficiency in accordance with current guidelines is key in the current pandemic |
Managing childhood allergies and immunodeficiencies during respiratory virus epidemics—The 2020 COVID‐19 pandemic: A statement from the EAACI‐section on pediatrics 24 |
| Drug allergy |
Drugs being used in different phases of COVID‐19 disease seem to cause rare but potentially severe drug hypersensitivity reactions (DHRs) Most of these DHRs affect the skin and are nonimmediate The most important differential diagnosis of these DHRs is COVID‐19‐related exanthems |
Diagnosis and management of the drug hypersensitivity reactions in Coronavirus disease 19: An EAACI Position Paper 26 |
| Ocular allergy |
An international survey revealed that experts in the field recommend that during the ongoing pandemic therapy strategies in line with current guidelines should be followed However, particular caution for the use of corticosteroids and immunomodulators in COVID‐19‐infected patients is expressed |
Managing ocular allergy in the time of COVID‐19 19 |
| Organization of an allergy clinic |
Recommendations on operational plans and procedures to maintain high standards in the daily clinical care of allergic patients while ensuring necessary safety in the current COVID‐19 pandemic should be followed Nine different scenarios and topics are discussed |
COVID‐19 pandemic: Practical considerations on the organization of an allergy clinic—an EAACI/ARIA Position Paper 23 |
FIGURE 1.
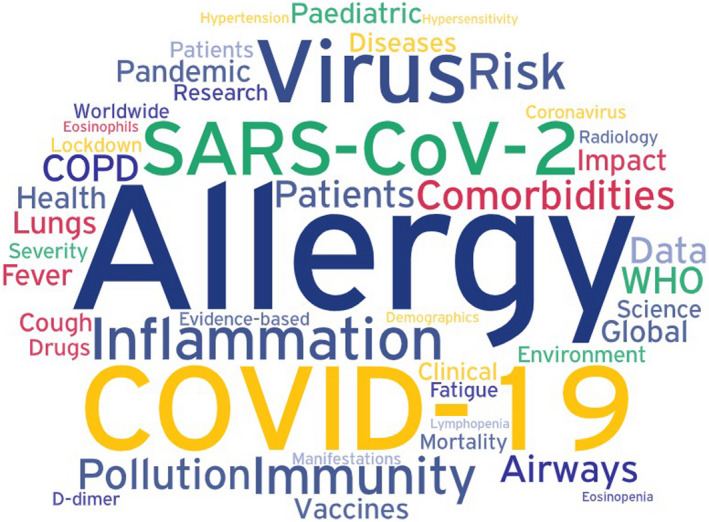
The wide range of aspects involved in the clinical picture of COVID‐19
Even though there has been a decrease in both infection rates and prevalence of COVID‐19 in some parts of the world, in some countries the spread of COVID‐19 has not been adequately controlled and the numbers are still rising. Epidemiologists have warned of possible subsequent waves until an effective vaccination becomes available. Until then, recommendations for different aspects of patient care are strictly needed, which underlines the importance of the COVID‐19 series of publications in this journal. The recommendations provided in these articles will inform allergists and healthcare providers on the management and treatment of patients during this pandemic. It should be noted that these statements are based on current evidence and medical knowledge and there is a paucity of prospective clinical trials regarding some of the information provided in these documents. These clinical statements need to be regularly updated with incoming new clinical data.
CONFLICTS OF INTEREST
Dr Pfaar reports grants and/or personal fees from ALK‐Abelló, Allergopharma, Stallergenes Greer, HAL Allergy Holding BV/HAL Allergie GmbH, Bencard Allergie GmbH/Allergy Therapeutics, Lofarma, Biomay, Circassia, ASIT Biotech Tools SA, Laboratorios LETI/LETI Pharma, MEDA Pharma/MYLAN, Anergis SA, Mobile Chamber Experts (a GA2LEN Partner), Indoor Biotechnologies, GSK, Astellas Pharma Global, EUFOREA, ROXALL, NOVARTIS, SANOFI AVENTIS, Med Update Europe GmbH, and streamedup! GmbH. Dr Torres has no conflict of interest in relation to this work. Dr Akdis reports grants from Allergopharma, Idorsia, Swiss National Science Foundation, Christine Kühne‐Center for Allergy Research and Education, European Commission's Horizon's 2020 Framework Programme, Cure, Novartis Research Institutes, AstraZeneca, SciBase, GSK, and other from Sanofi and Regeneron.
REFERENCES
- 1. Coronavirus disease (COVID‐2019) situation reports. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports, Accessed on 16 Apr 2020.
- 2. Zhang JJ, Dong X, Cao YY, et al. Clinical characteristics of 140 patients infected with SARS‐CoV‐2 in Wuhan, China. Allergy. 2020;75(7):1730–1741. [DOI] [PubMed] [Google Scholar]
- 3. Jesenak M, Banovcin P, Diamant Z. COVID‐19, chronic inflammatory respiratory diseases and eosinophils ‐ Observations from reported clinical case series. Allergy. 2020;75(7):1819–1822. [DOI] [PubMed] [Google Scholar]
- 4. Xie G, Ding F, Han L, et al. The role of peripheral blood eosinophil counts in COVID‐19 patients. Allergy. 2021;76:471–482. 10.1111/all.14465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dong X, Cao YY, Lu XX, et al. Eleven faces of coronavirus disease 2019. Allergy. 2020;75(7):1699–1709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zhang JJ, Cao YY, Dong X, et al. Distinct characteristics of COVID‐19 patients with initial rRT‐PCR‐positive and rRT‐PCR‐negative results for SARS‐CoV‐2. Allergy. 2020;75(7):1809–1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Du H, Dong X, Zhang JJ, et al. Clinical characteristics of 182 pediatric COVID‐19 patients with different severities and allergic status. Allergy. 2021;76:510–532. 10.1111/all.14452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sokolowska M, Lukasik ZM, Agache I, et al. Immunology of COVID‐19: Mechanisms, clinical outcome, diagnostics, and perspectives‐A report of the European Academy of Allergy and Clinical Immunology (EAACI). Allergy. 2020;75(10):2445–2476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Azkur AK, Akdis M, Azkur D, et al. Immune response to SARS‐CoV‐2 and mechanisms of immunopathological changes in COVID‐19. Allergy. 2020;75(7):1564–1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gursel M, Gursel I. Is global BCG vaccination‐induced trained immunity relevant to the progression of SARS‐CoV‐2 pandemic? Allergy. 2020;75(7):1815–1819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ozdemir C, Kucuksezer UC, Tamay ZU. Is BCG vaccination affecting the spread and severity of COVID‐19? Allergy. 2020;75(7):1824–1827. [DOI] [PubMed] [Google Scholar]
- 12. Radzikowska U, Ding M, Tan G, et al. Distribution of ACE2, CD147, CD26 and other SARS‐CoV‐2 associated molecules in tissues and immune cells in health and in asthma, COPD, obesity, hypertension, and COVID‐19 risk factors. Allergy. 2020;75(11):2829–2845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cai Q, Huang D, Ou P, et al. COVID‐19 in a designated infectious diseases hospital outside Hubei Province, China. Allergy. 2020;75(7):1742–1752. [DOI] [PubMed] [Google Scholar]
- 14. Bonini S, Maltese G. COVID‐19 Clinical trials: quality matters more than quantity. Allergy. 2020;75(10):2542–2547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sotgiu G, Gerli AG, Centanni S, et al. Advanced forecasting of SARS‐CoV‐2‐related deaths in Italy, Germany, Spain, and New York State. Allergy. 2020;75(7):1813–1815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bousquet J, Jutel M, Akdis CA, et al. ARIA‐EAACI statement on Asthma and COVID‐19 (June 2, 2020). Allergy. 2021;76:689–697. 10.1111/all.14471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Carli G, Cecchi L, Stebbing J, Parronchi P, Farsi A. Is asthma protective against COVID‐19? Allergy. 2021;76:866–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Johnston SL. Asthma and COVID‐19: is asthma a risk factor for severe outcomes? Allergy. 2020;75(7):1543–1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Leonardi A, Fauquert JL, Doan S, et al. Managing ocular allergy in the time of COVID‐19. Allergy. 2020;75(9):2399–2402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Licari A, Votto M, Brambilla I, et al. Allergy and asthma in children and adolescents during the COVID outbreak: What we know and how we could prevent allergy and asthma flares. Allergy. 2020;75(9):2402–2405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bousquet J, Akdis CA, Jutel M, et al. Intranasal corticosteroids in allergic rhinitis in COVID‐19 infected patients: An ARIA‐EAACI statement. Allergy. 2020;75(10):2440–2444. [DOI] [PubMed] [Google Scholar]
- 22. Klimek L, Jutel M, Akdis C, et al. Handling of allergen immunotherapy in the COVID-19 pandemic: An ARIA-EAACI statement. Allergy. 2020;75(7):1546–1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Pfaar O, Klimek L, Jutel M, et al. COVID‐19 pandemic: Practical considerations on the organization of an allergy clinic ‐ an EAACI/ARIA Position Paper. Allergy. 2021;76:648–676. 10.1111/all.14453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Brough HA, Kalayci O, Sediva A, et al. Managing childhood allergies and immunodeficiencies during respiratory virus epidemics ‐ The 2020 COVID‐19 pandemic: a statement from the EAACI‐section on pediatrics. Pediatr Allergy Immunol. 2020;31(5):442–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Klimek L, Jutel M, Bousquet J, et al. Management of patients with chronic rhinosinusitis during the COVID‐19 pandemic ‐ An EAACI Position Paper. Allergy. 2021;76:677–688. 10.1111/all.14629. [DOI] [PubMed] [Google Scholar]
- 26. Gelincik A, Brockow K, Çelik GE, et al. Diagnosis and management of the drug hypersensitivity reactions in Coronavirus disease 19: An EAACI Position Paper. Allergy. 2020;75(11):2775–2793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Vultaggio A, Agache I, Akdis CA, et al. Considerations on Biologicals for Patients with allergic disease in times of the COVID‐19 pandemic: an EAACI Statement. Allergy. 2020;75(11):2764–2774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Riggioni C, Comberiati P, Giovannini M, et al. A compendium answering 150 questions on COVID‐19 and SARS‐CoV‐2. Allergy. 2020;75(10):2503–2541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Allergy homepage . https://journalallergy.com/#JMA. Accessed on 16 Jun 2020


