Abstract
Long‐term care facilities have been identified as a local epicenter of disease among populations vulnerable to coronavirus disease 2019 (COVID‐19). A skilled nursing facility in Washington State was the first major site of COVID‐19 infections in the United States. Many lessons were learned during the events surrounding this outbreak, including how to develop, and the importance of, a coordinated response between emergency medical services and local area hospitals. As these events came early in the U.S. pandemic, unfortunately, disease spread and mortality was high. However, these events also resulted in rapid mobilization of the regional response to the COVID‐19 pandemic. Understanding the events surrounding this outbreak demonstrate some of the challenges involved in responding to acute infectious illnesses within these unique environments and associated vulnerable populations.
Keywords: COVID‐19, Skilled Nursing Facility
1. INTRODUCTION
The coronavirus disease 2019 (COVID‐19) pandemic presents unprecedented challenges to health care systems. Many vulnerable populations—homeless, older adults, individuals with comorbidities—are at increased risk of poor outcomes because of the virulence of the disease and supportive care needs. 1 Epidemiological data demonstrate that elderly and comorbid patients are at greatest risk, warranting enhanced attention and action. Long‐term health care facilities, with dense concentrations of at‐risk individuals combined with unique institutional risk factors, pose a particular barrier to controlling the current pandemic. 2 Some specific barriers to infection control and clinical care include health care workers and visitors acting as a vectors for transmission into and outside of these facilities, high‐risk patient demographics (age, comorbidities), facility structure, and facility staffing. These multifactorial risks, which are likely additive, result from personal and environmental elements. Understanding these elements of risk is the first step to tailoring mitigation and response strategies. 3
As Washington State was the first major region in the United States to experience significant numbers of documented COVID‐19 infections, it represents an opportunity to influence how the rest of the country responds to the outbreak. Missteps, adaptive behaviors, health system change, and alternative communication strategies are all part of the story of how Washington State responded to the first and subsequent cases of COVID‐19.
These lessons learned may also inform and facilitate more effective preparation and responses to future infectious emergencies, regionally and nationally.
2. CASE DESCRIPTION
In late February, when the first cluster of cases was identified in Washington State, understanding of the pathology and virulence of COVID‐19 was still poor. 4 Data from China were inconsistent and concerns about relatability provoked conjecture globally. Severe outcomes early in the United States outbreak of COVID‐19 have been high among older adults. 5 The epidemiology of the outbreak related to the facility has been described elsewhere, and demonstrate that as of March 18 there were 167 total cases, including 50 staff members and 35 total deaths from COVID‐19 among residents, staff, and visitors at the Washington State facility. 6 , 7 This communication seeks to describe the progression of the disease within the facility, the impact on the health care system, and the region's response.
The facility houses long‐term, skilled nursing, and rehabilitation residents in a communal living setting. Resident rooming geography was not segregated by clinical needs. Large public use, rehabilitation, and working areas with a combination of private and semiprivate living quarters and a main quadrilateral hallway dominate the architectural design. The hallway also serves as the main nursing, facilities, nutrition, and transportation corridor, suggesting mechanisms for transmission (Figure 1). Before these events, the skilled nursing facility had approximately 130 residents and 170 staff. An unknown number of the staff were known to work at multiple facilities, a situation that is common to the industry. Information on changes to staffing during the events, such as restriction of outside work, was not available. It is also unclear if the facility had previous involvement in regional disaster preparation or drills, but this would be an uncommon practice. Any disaster preparation at the facility may or may not have included pandemic preparedness. Personal protective equipment (PPE) was limited to gloves and gowns and did not include use of masks and eye protection. Clinical staff and protocols at the facility were designed to respond to acute illness; for example, scheduled vital signs were obtained daily and use of non‐scheduled and/or intravenous medications was not common. The initial patient with COVID‐19 reported symptoms on February 19 and was transferred to the nearest hospital on February 24. This patient was diagnosed with COVID‐19 on February 28, soon after the COVID‐19 testing criteria were revised by the Centers for Disease Control and Prevention (CDC). During this period COVID‐19 testing was limited and was being solely conducted by the Washington State Department of Health's Public Health Laboratories.
FIGURE 1.
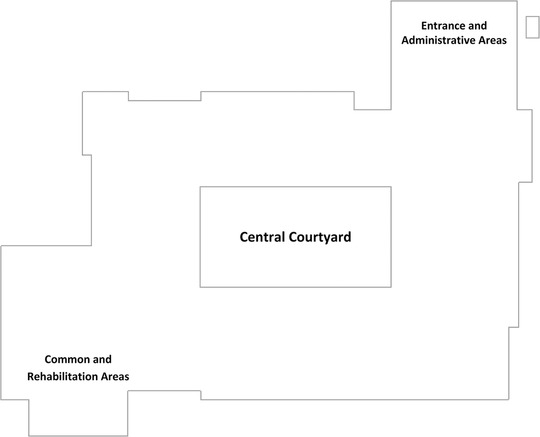
Diagram of the facility
As an early indicator of the rising burden of disease, during the week of February 23–February 29, there was a substantial increase in emergency medical services (EMS) responses to the facility. The city's EMS systems is a 2‐tiered system utilizing public fire‐based initial response staffed by paramedics and transportation of non‐critical patients by private ambulance staffed by emergency medical technicians. The average number of weekly 911 initiated EMS responses from January 1 to February 22 was 1.6 but increased to 11 responses during the week of February 23–February 29 and 27 responses during the first 4 days of the following week. 8
This observation caused local fire department EMS leaders to activate the region's Disaster Medical Coordination Center (DMCC) on March 4. The DMCC is an established county‐level medical operations coordinating cell functioning under the Washington State Department of Health (WA DOH). The DMCC is managed by the regional level 1 trauma center's emergency department staff and acts as a coordination service between EMS and regional health care entities.
Following the DMCC activation, the regional health care coalition conducted a call with area leaders and with staff members from the facility who voiced concern regarding the number of staff becoming ill, the burden of disease within the facility, and their ability to manage the outbreak. At the time, the facility felt they had sufficient short‐term staff for the next 12–24 hours. During this call, coordination with the CDC and the Department of Health and Human Services (HHS) teams was discussed. These teams had been dispatched to the facility to provide assistance with the outbreak; however, the arrival and composition of these teams were uncertain.
On March 5, local fire department‐based EMS leadership reviewed the recent events including additional 911 calls and requested the DMCC assist with further distribution of patients. In the prior 10 days, 33 of 37 patients transported from the facility had gone to 1 local hospital that was now experiencing a shortage of critical care resources. The local fire department and private ambulance EMS agencies had been following the local practice of facilitating the request of the sending facility in determining hospital destination. They had not been asked to divert or change this practice before that time. On a March 6 follow‐up coordination call with area leaders, it was determined that further staff illness had resulted in insufficient existing staffing for the number of residents at the facility. At that point, it was determined that an assessment team would be needed to identify any acutely ill residents within the facility. The goal was to identify those who may benefit from acute hospitalization and to restore staffing ratios by reducing the number of patients. The final determination was based upon the assessment that in order to provide a community‐level standard of medical care for the remaining residents, some would need to be sent to acute care hospitals.
Shortly thereafter, a call was convened by the coalition to discuss patient distribution with senior health care system leadership throughout the region. At the time, only 2 hospitals in the region had cared for COVID‐19 patients. Despite this, health system partners willingly agreed to assist. Near the time of this call, a general solicitation was made for volunteer physicians to enter the facility and determine the extent of illness among residents as well as provide an assessment of staff capabilities and resilience to provide care. A team consisting of an emergency physician from UW Medicine (a regional health care system affiliated with the University of Washington) and 2 Public Health Seattle King County physicians evaluated 28 residents within the facility. They identified 16 symptomatic residents for dispersal to area hospitals. Federal clinical support teams arrived at the facility on March 7 (Table 1).
TABLE 1.
Timeline of critical events, COVID‐19 outbreak in a skilled nursing facility, Washington State
| Date (2020) | Event |
|---|---|
| February 19 | First patient identified as symptomatic |
| February 24 | First patient transported to area hospital |
| February 27 | Public Health Seattle/King County notified of patient meeting revised testing criteria for COVID‐196 |
| February 28 | Diagnosis of COVID‐19 in first patient and beginning of epidemiological investigation by public health and CDC |
| February 29th | Approximate date of initiation of facility staff augmentation, just in time training, patient cohorting, and PPE acquisition and stockpiling. |
| February 23–February 29 (7 days) | 11 EMS responses to facility (average weekly 1.6) |
| March 1‐4 (4 days) | 27 EMS responses to facility |
| March 4 | DMCC begins regional response |
| March 5 | DMCC begins work with EMS to coordinate patient distribution |
| March 6–7 | 16 patients transported to regional hospitals assisted by local clinical support |
| March 7 | Federal clinical support arrives at the facility |
CDC, Centers for Disease Control and Prevention; DMCC, Disaster Medical Coordination Center; EMS, emergency medical services.
The DMCC command structure was initiated and contact with local EMS established. The DMCC consisted of a team of physicians and nurses working in collaboration. The DMCC physicians worked with the physician team at the facility to triage residents identified for transport. Once patients were identified, nurses at the DMCC worked to establish contact with area hospitals that had agreed to accept these patients. As these patients were being sent from a skilled nursing facility with known COVID‐19 disease, each hospital was notified of the likelihood of COVID‐19 illness. The receiving hospital chose to receive these patients differently with some directly admitting them to an inpatient COVID‐19 unit and some asking they be evaluated in the emergency department.
Local EMS provided a senior‐level supervisor for coordination between the DMCC and EMS ground units. As patients and hospital destinations were identified over a period of hours, basic life support and advanced life support units were called for transportation as indicated by the severity of illness. A total of 13 hospitals across 2 counties received patients.
Multiple interventions were necessary to stabilize the facility. These included assistance with PPE supply and training, cohorting of patients within the facility, active surveillance of EMS activity and destination hospitals, assistance from outside entities (Public Health Seattle King County, UW Medicine, CDC, and HHS), and central coordination of patient movement, the situation at the facility became more stabilized. Additionally, the framework established during this event continues to be utilized in the region.
3. DISCUSSION
Our experience demonstrates the risk skilled nursing facilities face for disease transmission and progression in the COVID‐19 pandemic (Table 2). Many factors contribute to this including basic infection prevention, PPE utilization and training, patient cohorting, and interface challenges with the broader health care system (out‐of‐hospital, acute care, public health and federal assets).
TABLE 2.
Vulnerabilities, solutions, and recommendations from response to COVID‐19 outbreak in a skilled nursing facility, Washington State
| Identified vulnerability | Solution | Recommendations |
|---|---|---|
| Surveillance | Deployment of clinical and public health support, review of EMS runs, enhanced staff training, and increased monitoring | Engage local community (EMS, public health) and long‐term care leadership to enhance early detection of disease spread. |
| Facility | Cohorting, barriers, social distancing, enhanced nursing training. | Reorganization of flow and isolation techniques to transmission risk. |
| Staffing | Just‐in‐time training, PPE supplies, clinical and technical support through outside institutions. | Utilize available educational tools and protocols for enhancing response. |
| Communication | Establishment of communication avenues between EMS and hospitals, centralized patient distribution, involvement of public health and government institutions. | Regional engagement of involved entities with establishment of a centralized command and centralized data platform for improved situational awareness. |
EMS, emergency medical services.
As this was early in the pandemic and the first outbreak in North America, awareness regarding the importance of infection prevention strategies for severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) transmission was not common. This likely contributed to the large number of staff members (50) who would acquire COVID‐19 and affected the facilities’ ability to provide expected staffing ratios as the number of staff illnesses increased. 5 , 6 In the initial phase of the outbreak, outside medical teams provided essential infection prevention education, PPE training and assured adequate PPE supplies for remaining staff at the facility. Since the outbreak, postacute care teams from regional health systems, hospitals, and public health have supplied this education, training, and PPE coordination for all skilled nursing facilities in King County. 6 In addition, these teams have developed testing strategies of patients and staff to identify and respond to infected individuals and improve the understanding of the disease burden. 9
Facilities of this type are designed to enhance the residents’ experience through aesthetics and encourage group interaction. Cohorting of symptomatic patients to one side of the facility is an infection prevention strategy that was identified as an opportunity within this facility.
Use of temporary barriers (commercially available medical privacy screens and drapes), now common with COVID‐19 in the acute care setting, could be used for creating divided areas and isolating patients in facilities such as this. The cohorting and isolating of patients are key to identifying and isolating patients to limit exposures and allow staff to don and doff appropriate PPE.
The need for improved communication and coordination structures was an important lesson learned from these experiences. During normal circumstances, EMS, acute care, and postacute care settings in our region had not previously worked to coordinate patient movement. In the setting of an infectious outbreak, this lack of coordination resulted in significant stress to the local health care system. Early in the response the DMCC, along with public health and health care network partners, worked to level load area health systems by developing monitoring strategies of EMS activities at skilled nursing facilities and eventually all congregate housing facilities in the region. EMS activity data is now combined with COVID‐19 testing data for identification of facilities with known resident and staff cases and thus at risk for an outbreak. EMS activities at these congregate facilities are reviewed daily by the DMCC and public health partners. The DMCC has also extended its coordination efforts and established the Western Washington Regional COVID‐19 Coordination Center (RCCC) to organize and coordinate efforts across the region. The goal of the RCCC is to identify facilities at risk and to coordinate training, testing, and PPE supplies at these facilities while working to level load health system assets.
The RCCC has also worked with Microsoft, area health system partners, and the WA DOH to develop a data platform that centralizes reporting of variables crucial in assuring regional situational awareness. These include centralized reporting of available beds (critical care, acute care), PPE and ventilator supplies, staffing availability, and the number of COVID‐19 patients at each hospital across the state. The platform is now managed by the WA DOH under the name WAHealth (Figures 2 and 3). The improved situational awareness promises to assist in the RCCC's goal of equitable and level distribution of patients when outbreaks occur.
FIGURE 2.
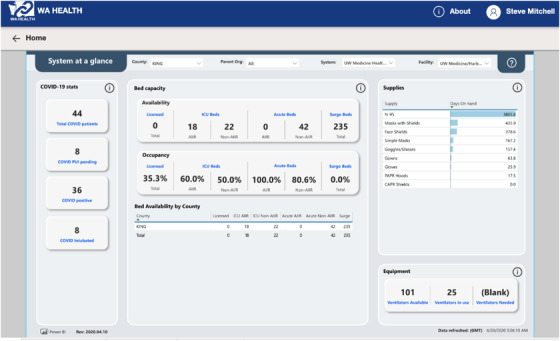
Screenshot of Washington State's online centralized data platform demonstrating bed availability and occupancy, and critical supply availability accessed by the author on April 4, 2020 during the COVID‐19 pandemic
FIGURE 3.
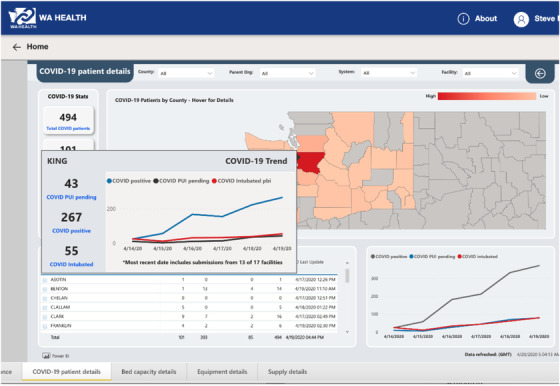
Screenshot of Washington State's online centralized data platform demonstrating graphical representation of key trends in COVID‐19 disease burden accessed by the author on April 4, 2020 during the COVID‐19 pandemic
4. CONCLUSION
Washington State was the region of the initial outbreak of COVID‐19 in the United States, with the first cluster of cases occurring in a large postacute care facility. The events surrounding this Washington State skilled nursing facility's COVID‐19 outbreak in late February and early March 2020 have had a significant impact on regional response to COVID‐19. Many of these lessons learned may be beneficial to health systems preparing for similar challenges.
CONFLICTS OF INTEREST
The authors report no conflicts of interest.
ACKNOWLEDGMENTS
The authors would like to thank UW Medicine, The Northwest Healthcare Response Network, Public Health ‐ Seattle & King County, King County Medic One, the regional hospitals and public and private EMS of Seattle‐King County, for their extraordinary efforts on the part of the people they served and continue to serve before, during and after the COVID‐19 pandemic.
Morris SC, Resnick AT, England SA, Stern SA, Mitchell SH. Lessons learned from COVID‐19 outbreak in a skilled nursing facility, Washington State. JACEP Open. 2020;1:563–568. 10.1002/emp2.12137
Supervising Editor: David Wampler, PhD.
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
REFERENCES
- 1. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID‐19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054‐1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dosa D, Feng Z, Hyer K, Brown LM, Thomas K, Mor V. Effects of Hurricane Katrina on nursing facility resident mortality, hospitalization, and functional decline. Disaster Med Public Health Prep. 2010;4(Suppl 1):S28‐S32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Pierce JR, Morley SK, West TA, Pentecost P, Upton LA, Banks L. Improving long‐term care facility disaster preparedness and response: a literature review. Disaster Med Public Health Prep. 2017;11(1):140‐149. [DOI] [PubMed] [Google Scholar]
- 4.Additional cases of COVID‐19 in Washington State. https://www.doh.wa.gov/Newsroom/Articles/ID/1103/Additional-Cases-of-COVID-19-in-Washington-State. Accessed June 6, 2020.
- 5. COVID, C., & Team, R. Severe outcomes among patients with coronavirus disease 2019 (COVID‐19)—United States, February 12–March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(12):343‐346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McMichael TM, Currie DW, Clark S, et al. Epidemiology of covid‐19 in a long‐term care facility in King County, Washington. N Engl J Med. 2020;382:2005‐2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. McMichael TM, Clark S, Pogosjans S, et al. COVID‐19 in a long‐term care facility—King County, Washington, February 27–March 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:339‐342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fields A, Hudetz M. Coronavirus spread at Life Care Center of Kirkland for weeks, while response stalled. Seattle Times. 2020. https://www.seattletimes.com/seattle-news/times-watchdog/coronavirus-spread-in-a-kirkland-nursing-home-for-weeks-while-response-stalled/. Accessed June 6, 2020. [Google Scholar]
- 9. Kimball A. Asymptomatic and presymptomatic SARS‐CoV‐2 infections in residents of a long‐term care skilled nursing facility—King County, Washington, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69:377‐381. [DOI] [PMC free article] [PubMed] [Google Scholar]


