Abstract
Background:
Superior labral anterior-posterior (SLAP) lesions are common among elite gymnasts and throwing athletes. Although SLAP lesions in throwers are well-described in the literature, no study has described the characteristics of SLAP lesions in gymnasts. We aimed to reveal the characteristics of SLAP lesions in gymnasts by comparing the location and extension of these lesions between gymnasts and throwers.
Hypothesis:
The location and arc of SLAP lesions in gymnasts will be different from those in throwing athletes.
Study Design:
Case series; Level of evidence, 4.
Methods:
This study included 27 shoulders in 20 males and 3 females with a mean ± SD age of 20 ± 2.5 years (range, 16-25 years). We performed debridement alone for shoulders with a stable lesion. Anterior and/or posterior labral repair was added for unstable SLAP lesions depending on the extension and stability of the lesions. We investigated symptoms, onset, return to sport (based on patient records), and subjective shoulder values. SLAP lesions were evaluated through use of the Snyder classification. The location and arc of SLAP lesions were determined from surgical records and videos and described by use of the right shoulder clockface method. During the same period, 65 baseball players (65 shoulders; all males; mean age, 23 ± 7.0 years; range, 16-44 years) underwent arthroscopic SLAP surgery. We compared the location and arc of SLAP lesions between gymnasts and baseball players.
Results:
Symptoms during gymnastics included pain (100%), apprehension (48%), or catching (11%). We found that 20 shoulders had symptom onset during gymnastics, most commonly during rings events. Type II SLAP lesions were found in 17 shoulders, type III in 2 shoulders, and type IV in 8 shoulders. The mean center of SLAP lesions was at the 11:40 clockface position in 27 gymnasts and 10:40 clockface position in 65 baseball players, and the difference was statistically significant (P < .001). The mean arc of SLAP lesions was 125° in gymnasts and 140° in baseball players, and the difference was not significant. We performed debridement in 2 shoulders (7%) and labral repair in 25 shoulders (93%). After surgery, all patients returned to gymnastics. The mean subjective shoulder value was 35 (range, 10-90) preoperatively and 76 (range, 40-100) postoperatively.
Conclusion:
SLAP lesions in gymnasts were significantly located anteriorly compared with those in baseball players. All patients returned to gymnastics after arthroscopic surgery. Secure repair of SLAP lesions may be important for good surgical outcomes, because 50% of patients experienced preoperative shoulder apprehension.
Keywords: gymnast, SLAP lesion, arthroscopic surgery, return to sport, SLAP location
Superior labral anterior-posterior (SLAP) lesions are frequently observed among throwing athletes. Many authors have reported on the surgical options (including debridement, repair, and even biceps tenodesis), surgical outcomes, and return to sport in throwers.1,8 Repetitive overhead throwing is recognized as the primary cause of SLAP lesions in throwing athletes.2,3,10 SLAP lesions are also common among elite gymnasts. De Carli et al6 reported that 16 of 36 (44%) shoulders of elite gymnasts had findings consistent with SLAP lesions on magnetic resonance imaging. However, because only a few published studies have described SLAP lesions in gymnasts, the causes, symptoms, location and arc, and treatment are still unclear.4,5
Over the years, the authors have treated a substantial number of throwing athletes and gymnasts with shoulder problems. We observed that the onset of the lesion had an acute and traumatic nature in many gymnasts. We also noticed that the location and arc of SLAP lesions might be different between throwing athletes and gymnasts. The differences in location may be associated with the pathogenesis of the lesions, and the treatment strategy should be altered according to the pathology. Burkhart and Morgan2 divided type II SLAP lesions into 3 subtypes and reported that repetitive throwing was the possible cause of posterior lesions and that acute trauma was the cause of anterior lesions. It is our suspicion that the difference in onset might be associated with the difference in the location of SLAP lesions between throwing athletes and gymnasts; however, no study has examined the differences in the location of SLAP lesions between gymnasts and throwing athletes.
The purpose of this study was to retrospectively investigate the location and extension of SLAP lesions in gymnasts and to compare these data with findings in throwing athletes. We also aimed to assess the surgical outcomes after SLAP repair in gymnasts, especially return to sport and patient satisfaction. We hypothesized that the location and extension of SLAP lesions in gymnasts would be different from those in throwing athletes.
Methods
Patients
From January 2006 to December 2017, a consecutive series of 29 gymnasts (34 shoulders) underwent arthroscopic surgery for SLAP lesions. Our surgical indication was the presence of refractory symptoms even after intensive physiotherapy including correction of scapular dyskinesis. SLAP lesion was diagnosed on the basis of magnetic resonance arthrography results. We excluded from this study 7 shoulders in 6 gymnasts with frank dislocation. Thus, we included 27 shoulders in 20 male and 3 female patients with a mean ± SD age of 20 ± 2.5 years (range, 16-25 years). There were 17 right and 10 left shoulders, and 4 patients had bilateral involvement. All surgeries were performed by 1 of 3 senior surgeons (H.S., N.T., K.M.). The institutional review board of our hospital approved this study.
Surgical Procedures
Patients were placed in the beach-chair position under general anesthesia. The affected upper limb was sterilely prepared and placed in the arm holder. A routine diagnostic arthroscopic examination was carried out via a standard posterior portal. An anterior portal was then established superior to the subscapularis and lateral to the conjoined tendon through use of the outside-in technique.12
The extension of SLAP lesions was then assessed. The free edge of the labrum was debrided with a shaver and forceps, and the stability of the lesion was estimated. The lesion was determined to be unstable when the superior labrum was subluxated into the joint space and could be reduced with a probe (Figure 1).
Figure 1.
Unstable superior labral anterior-posterior lesion (right shoulder, view from the posterior portal). (A) After debridement of the frayed labrum, the superior labrum was subluxated into the joint space. (B) The labrum could be reduced by pulling up with a probe (arrow) introduced through the anterior portal. G, glenoid; L, labrum; dotted line, glenoid edge.
For shoulders with a stable lesion, we performed only debridement (Figure 2); however, we added labral repair based on the extension of the lesion and stability for shoulders with an unstable lesion. Anterosuperior labral repair was performed for anterior type II SLAP lesions by inserting suture anchors from the anterior portal (Figure 3). However, if the lesion was extended posteriorly, a trans-cuff portal was established just lateral to the acromion to insert a suture anchor into the posterosuperior glenoid, and suture placement and knot tying were performed through this portal. Then, anterosuperior labral repair was performed by use of the anterior portal (Figure 4).
Figure 2.

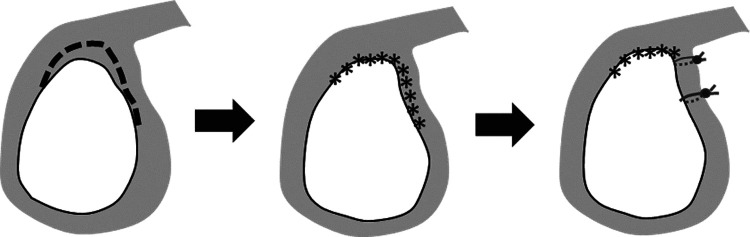
Surgical procedure for stable superior labral anterior-posterior lesions. Debridement of the frayed labrum was performed without fixation. Black dashed line, frayed labral lesion. Asterisk line, labral edge after debridement.
Figure 3.
Surgical procedure for anteriorly extended, unstable, superior labral anterior-posterior lesions. After debridement, the anterior labrum was repaired through use of 1 or 2 suture anchors. Black dashed line, frayed labral lesion. Asterisk line, labral edge after debridement.
Figure 4.
Surgical procedure for extensive, unstable, superior labral anterior-posterior lesions. After debridement, the anterior and posterior labrum was repaired through use of 2 or 3 suture anchors. Black dashed line, frayed labral lesion. Asterisk line, labral edge after debridement.
For type IV SLAP lesions, the long head of the biceps (LHB) was repaired by use of sutures (No. 2 Ethibond [Ethicon]). Then we assessed the stability of the lesion and repaired the labrum (Figure 5).
Figure 5.
Repair of type IV superior labral anterior-posterior (SLAP) lesion. (A) Type IV SLAP lesion. (B) Image taken after debridement, showing that the long head of the biceps (LHB) was torn. (C) After the LHB was repaired with sutures, the anteroposterior labrum was repaired with suture anchors. Dotted line, biceps base.
Postoperative Protocol
Shoulders with debridement alone were not immobilized, and physiotherapy was initiated 1 day postoperatively. Full return to gymnastics practice was allowed at 1 month after surgery, according to the functional recovery of each patient.
Shoulders treated with SLAP repair were immobilized with a sling for 3 weeks. Passive and assisted-active range of motion exercises were initiated the day after surgery, while avoiding provocation of pain. Patients were permitted to start practice at 3 months after surgery. Full return to competition was allowed after 4 to 6 months, according to the functional recovery of each patient.
Assessment of SLAP Lesions
SLAP lesions were classified on the basis of intraoperative findings through use of the Snyder classification.11 The location and extension of SLAP lesions were assessed during surgery by operating surgeons and recorded in surgical records. Data were collected from the surgical records for this study and confirmed with videotapes of the surgery. The location and extension of lesions were described using the right shoulder clockface method (Figure 6). The superior pole of the glenoid was defined as 12:00 and the inferior pole as 6:00 or 18:00. The location of SLAP lesions was described as between 6:00 and 18:00. We used the center (middle point) of the lesion and the arc (the angle between the most anterior and posterior points of the lesion) for comparison.
Figure 6.

Right shoulder clockface method. The superior pole of the glenoid was defined as 12:00 and the inferior pole as 6:00 or 18:00. The location of superior labral anterior-posterior lesions was described as between 6:00 and 18:00.
During the same period, 65 baseball players (65 shoulders) underwent arthroscopic SLAP surgery. They were all men, with a mean age of 23 ± 7.0 years (range, 16-44 years). There were 58 right and 7 left shoulders. We investigated the location and extension of SLAP lesions in baseball players for comparison with gymnasts.
Clinical Evaluation
We investigated the patients’ symptoms and their onset. We also investigated their return to sport including the required time to return to practice or competition. The mean follow-up duration for gymnasts was 18 ± 18.9 months (range, 12-77 months). We also assessed the patients by telephone using a subjective outcome measure questionnaire. This questionnaire included questions on return levels, subjective shoulder values (SSVs),7 and whether the respondents would recommend surgery to other gymnasts. We categorized return to sport into 3 levels: higher than, same as, and lower than the preinjury level. The preoperative and postoperative SSVs were obtained through use of the following question: “How normal does your shoulder feel on a scale from 1 to 100 (1, completely normal; 100, completely abnormal) during gymnastics?” The question on the recommendation of surgery was “Would you recommend the surgery to other gymnasts with the same injuries?”
Statistical Analysis
Statistical analysis was performed with the Mann-Whitney U test to compare the center and arc of SLAP lesions between gymnasts and baseball players. The Wilcoxon signed-rank test was used to compare the preoperative and postoperative SSVs. The level of significance was set at P < .05.
Results
The symptoms during gymnastics included pain (all shoulders; 100%), apprehension (13 shoulders; 48%), and catching (3 shoulders; 11%). We noted that 23 shoulders (85%) had symptom onset during gymnastics (Table 1), most commonly during the rings event (10 shoulders; 37%).
Table 1.
Onset of Shoulder Symptoms
| Catalyst of Symptoms | No. of Shoulders | % |
|---|---|---|
| Rings | 10 | 37 |
| Horizontal bar/uneven bars | 8 | 30 |
| Parallel bars | 3 | 11 |
| Pommel horse | 1 | 4 |
| Floor exercise/balance beam | 1 | 4 |
| Vault | 0 | 0 |
| Chronic/others | 4 | 15 |
Type II SLAP lesions were found in 17 shoulders, type III in 2 shoulders, and type IV in 8 shoulders. The mean center of SLAP lesions was located at 11:40 (range, 10:30-13:30) in 27 gymnasts and at 10:40 (range, 8:30-13:00) in 65 baseball players, and the difference was statistically significant (P < .001). The mean arc of SLAP lesions was 125° (range, 60°-180°) in gymnasts and 140° in baseball players (range, 60°-210°), and the difference was not significant (P = .09). SLAP lesions were located more anteriorly in gymnasts than in baseball players (Figure 7).
Figure 7.
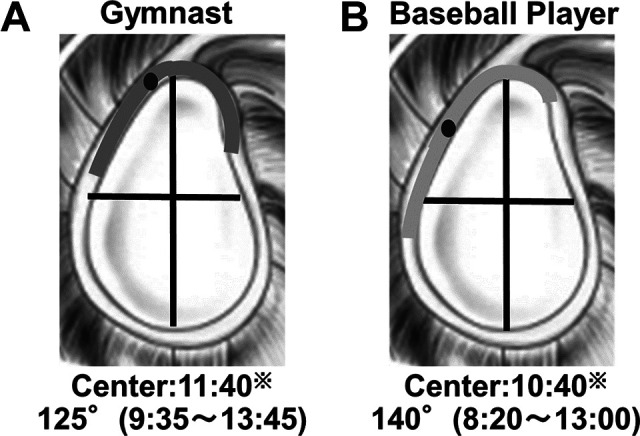
Location and extension of superior labral anterior-posterior (SLAP) lesions. (A) In gymnasts, the mean center of SLAP lesions was located at 11:40, and the mean arc was 125° (9:35-13:45). (B) In baseball players, the mean center was at 10:40, and the mean arc was 140° (8:20-13:00). The difference of center location was statistically significant (P < .001).
We performed arthroscopic debridement in 2 shoulders (7%) and arthroscopic labral repair in 25 shoulders (93%). The anterior labrum alone was repaired in 7 shoulders (26%), and both the anterior and posterior labrum were repaired in 18 shoulders (67%). After surgery, all patients returned to practice at a mean of 4 months (range, 1-9 months) and to competition at a mean of 9 months (range, 2-12 months).
We obtained answers to the questionnaire for 19 shoulders in 15 patients (70%). In total, 8 shoulders returned to their preinjury level, and 11 shoulders had a lower level than their preinjury level. The mean preoperative SSV was 35 (range, 10-90), and the mean postoperative SSV was 76 (range, 40-100) (Figure 8). SSV was improved significantly after surgery (P = .002). A total of 13 patients (87%) answered that they would recommend the surgery to other gymnasts with the same injuries.
Figure 8.

Postoperative changes in subjective shoulder value (SSV). Postoperative SSV was improved in all but 2 shoulders (gray lines).
Discussion
This study showed that SLAP lesions are located more anteriorly in gymnasts than in baseball players. In more than half of the gymnasts, suspension events (eg, rings, horizontal bars, and uneven bars) were responsible for the onset of symptoms. After arthroscopic surgery, all gymnasts returned to practice and competition; however, the postoperative SSV was not sufficiently high at a mean of 76.
Consistent with our reported finding, De Carli et al6 found that SLAP lesions were most frequent during the rings event. Caraffa et al5 reported that the traction force to the intra-articular structure reaches the maximum level during the rings event. We presume that the traction force to the LHB during suspension events may be associated with the occurrence of SLAP lesions in gymnasts. Traction force to the superior direction may be applied to the superior labrum through the LHB during the state of being suspended from the rings or bars and can lead to the development of a SLAP lesion extending both anteriorly and posteriorly. This mechanism is different from that in throwing athletes, in whom SLAP lesions are believed to be caused by repetitive throwing motion and internal impingement.13 This difference might result in the difference in the location of SLAP lesions between throwers and gymnasts.
In our study, almost half of the patients reported apprehension in addition to pain. Patzer et al9 reported that SLAP lesions led to increased glenohumeral translation. Thus, the superior labrum is important for the stability of the glenohumeral joint. The shoulders of gymnasts receive traction, rotation, and weightbearing forces during gymnastics and require a stable glenohumeral joint. Secure fixation of the superior labrum may be vital for the shoulders of gymnasts.
In this study, the return-to-sport rate was 100%, and most gymnasts (87%) answered that they would recommend the surgery to other gymnasts; however, the mean postoperative SSV was only 76. This may indicate that the gymnasts were satisfied with the surgery but perceived a gap between actual postoperative shoulder function and expected performance. Anxiety about reinjury might be associated with the lower shoulder function. Another factor related to this issue might be insufficient postoperative physiotherapy. Some gymnasts returned to practice or competition earlier than we had planned. We should have managed the gymnasts more strictly to achieve better shoulder function. Further studies are needed to clarify the relationship between postoperative treatment and shoulder function in gymnasts.
This study has several limitations. First, this was a retrospective case series study with a small sample size. Second, the location of SLAP lesions was intraoperatively determined and described by surgeons using a clockface method. Although this method is widely used and easy to understand, it may pose some inaccuracies. Third, we did not assess functional outcomes such as range of motion or clinical scores. However, the shoulder function must have been good because all patients returned to gymnastics. Fourth, we evaluated only shoulders that required surgical treatment. The location of SLAP lesions might be different in shoulders that did not require surgery. We believe that despite these limitations, this study provides very important information on the pathology and treatment of shoulder disorders in gymnasts.
Conclusion
SLAP lesions in gymnasts were significantly located anteriorly compared with those in baseball players. Most SLAP lesions in the shoulders of gymnasts had symptom onset during suspension events such as rings or bars, and half of the gymnasts reported shoulder apprehension in addition to pain. Fixation of both the anterior and posterior labrum was performed in 63% of the patients, and all patients returned to gymnastics after arthroscopic surgery. Secure repair of SLAP lesions may be important for good surgical outcomes because gymnasts require a stable glenohumeral joint.
Footnotes
Accepted for presentation at the Annual Meeting of the AOSSM, July 2020.
Final revision submitted November 26, 2019; accepted December 3, 2019.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Funabashi Orthopaedic Hospital (study No. 2019022).
References
- 1. Braun S, Kokmeyer D, Millett PJ. Shoulder injuries in the throwing athlete. J Bone Joint Surg Am. 2009;91(4):966–978. [DOI] [PubMed] [Google Scholar]
- 2. Burkhart SS, Morgan CD. The peel-back mechanism: its role in producing and extending posterior type II SLAP lesions and its effect on SLAP repair rehabilitation. Arthroscopy. 1998;14(6):637–640. [DOI] [PubMed] [Google Scholar]
- 3. Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology, part II: evaluation and treatment of SLAP lesions in throwers. Arthroscopy. 2003;19(5):531–539. [DOI] [PubMed] [Google Scholar]
- 4. Caine DJ, Nassar L. Gymnastics injuries. Med Sport Sci. 2005;48:18–58. [DOI] [PubMed] [Google Scholar]
- 5. Caraffa A, Cerulli G, Rizzo A, Buompadre V, Appoggetti S, Fortuna M. An arthroscopic and electromyographic study of painful shoulders in elite gymnasts. Knee Surg Sports Traumatol Arthrosc. 1996;4(1):39–42. [DOI] [PubMed] [Google Scholar]
- 6. De Carli A, Mossa L, Larciprete M, Ferretti M, Argento G, Ferretti A. The gymnast’s shoulder MRI and clinical findings. J Sports Med Phys Fitness. 2012;52(1):71–79. [PubMed] [Google Scholar]
- 7. Gilbart MK, Gerber C. Comparison of the subjective shoulder value and the Constant score. J Shoulder Elbow Surg. 2007;16(6):717–721. [DOI] [PubMed] [Google Scholar]
- 8. Gilliam BD, Douglas L, Fleisig GS, et al. Return to play and outcomes in baseball players after superior labral anterior-posterior repairs. Am J Sports Med. 2018;46(1):109–115. [DOI] [PubMed] [Google Scholar]
- 9. Patzer T, Habermeyer P, Hurschler C, et al. Increased glenohumeral translation and biceps load after SLAP lesions with potential influence on glenohumeral chondral lesions: a biomechanical study on human cadavers. Knee Surg Sports Traumatol Arthrosc. 2011;19(10):1780–1787. [DOI] [PubMed] [Google Scholar]
- 10. Shepard MF, Dugas JR, Zeng N, Andrews JR. Differences in the ultimate strength of the biceps anchor and the generation of type II superior labral anterior posterior lesions in a cadaveric model. Am J Sports Med. 2004;32(5):1197–1201. [DOI] [PubMed] [Google Scholar]
- 11. Snyder SJ, Karzel RP, Del Pizzo W, Ferkel RD, Friedman MJ. SLAP lesions of the shoulder. Arthroscopy. 1990;6(4):274–279. [DOI] [PubMed] [Google Scholar]
- 12. Sugaya H, Kon Y, Tsuchiya A. Arthroscopic Bankart repair in the beachchair position: a cannulaless method using an intra-articular suture relay technique. Arthroscopy. 2004;20(suppl 2):116–120. [DOI] [PubMed] [Google Scholar]
- 13. Walch G, Boileau P, Noel E, Donell ST. Impingement of the deep surface of the supraspinatus tendon on the posterosuperior glenoid rim: an arthroscopic study. J Shoulder Elbow Surg. 1992;1:238–245. [DOI] [PubMed] [Google Scholar]