Abstract
Most patients with primary central system lymphoma (PCNSL) have immune dysfunction. PCNSL without immune dysfunction is rare and extremely challenging to diagnose. Here, we report the case of a 52-year-old woman without immune dysfunction who presented with PCNSL. The patient died a few months after diagnosis and during treatment. A review of this PCNSL patient’s case highlighted that poor interpretation of imaging features and the poor correlation of laboratory test results with clinical findings led to a difficulty in making a diagnosis and administering the best treatment. For an accurate diagnosis of early stage PCNSL, positron-emission tomography computed tomography and corticosteroids should be used cautiously before stereotactic biopsy.
Keywords: Primary central nervous system lymphoma, case report, diagnosis, immune dysfunction, imaging, positron-emission tomography computed tomography, corticosteroids, stereotactic biopsy
Introduction
Primary central nervous system lymphoma (PCNSL) is rare. About 90% of PCNSLs are diffuse large B-cell lymphomas, and PCNSLs account for 2% to 3% of all brain tumors and less than 1% of all non-Hodgkin lymphomas.1 Immune dysfunction is the only known risk factor,2 and immunodeficient individuals are more susceptible to PCNSLs, especially HIV-positive populations, who have a high incidence of PCNSL.1 The present case report describes a woman with PCNSL without any immune dysfunction. This case can provide valuable clinical insights for the early and accurate diagnosis of PCNSL.
Case report
A 52-year-old woman presented to our hospital because of a 1-month history of weakness in the right limbs along with mental decline. One month before attending the hospital, the patient suddenly developed weakness and numbness of her right limbs, followed by slow responses and speech. While walking, her right lower limb would drag. She also experienced dysphagia, coughing, irritability, and apathy. An examination revealed impaired orientation, memory, and cognition, slow pharyngeal reflex, grade 5 muscle strength in both left limbs and the right upper limb, and grade 4 muscle strength in the right lower limb. The patient had carried her father’s decaying body to another grave site 2 weeks before the onset of the symptoms. The patient was admitted to the Department of Neurology of our hospital. A magnetic resonance imaging (MRI) examination (Figure 1a–1d) showed multiple abnormal signals in the brain, suggesting the possibility of infectious lesions. Cerebrospinal fluid examination showed the following: clear, colorless fluid; qualitative protein test (−); white blood cell count, 17 × 106/L; and cerebrospinal fluid biochemistry, fungal smear, Mycobacterium tuberculosis, and other bacterial culture, no abnormalities. No abnormalities were detected on whole blood cell analysis, liver- and kidney-function tests, tests for electrolytes, coagulation function, hepatitis B, HIV, myocardial injury markers, and autoantibodies (antineutrophil cytoplasmic antibodies, antistreptolysin O antibodies, rheumatic factor, immunoglobulins, and complement C3 and C4), electrocardiography, and electroencephalography. The provisional diagnosis was a viral infection. There was no significant change in the patient’s condition after 11 days of treatment with acyclovir (2 g daily) and dexamethasone (30 mg daily).
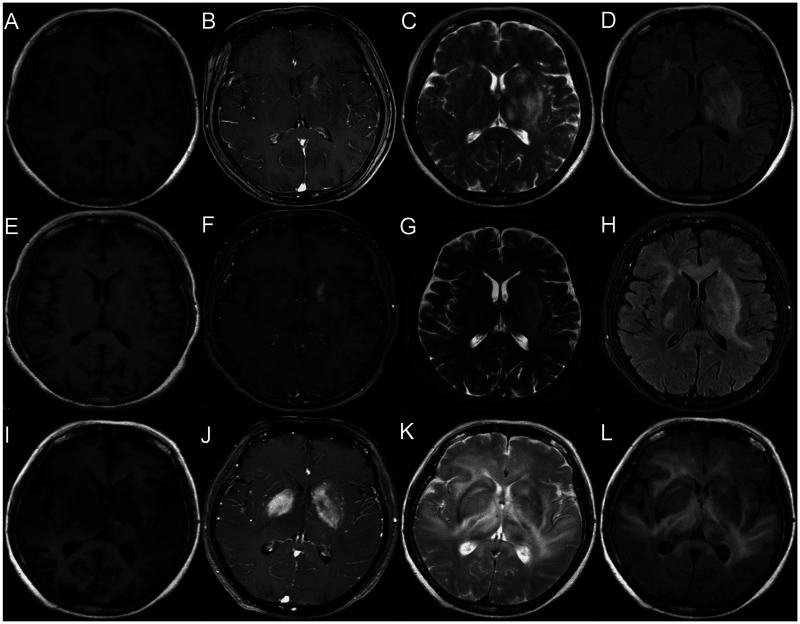
Figure 1.
Brain magnetic resonance imaging (MRI): (a–d) The first, (e–h) second, and (i–l) third brain MRI examinations of the patient. (a, e, i) T1-weighted images. (b, f, j) Enhanced T1-weighted images. (c, g, k) T2-weighted images. (d, h, l) Fluid-attenuated inversion recovery images.
On day 13, the patient was transferred to another large hospital for neurology treatment, where she underwent tests for parasites, Epstein–Barr virus antibody, cytomegalovirus antibody, cerebrospinal fluid immunoglobulins, enhanced computed tomography (CT) of the chest, abdomen, and pelvis, and enhanced cervical MRI. The second MRI (Figure 1e–1h) suggested the possibility of poisoning, degeneration, hypoxia, or infectious or inflammatory lesions. A positron-emission tomography (PET)-CT examination suggested that a multifocal abnormal increase of glucose metabolism with edema in the brain tissue might be diagnosed as lymphoma, and no lesions were found outside the skull. After 1 month of treatment, the patient’s diagnosis was still unclear. During this period, we suggested that the patient undergo a stereotactic biopsy, but the patient’s family refused, so only nutritional support treatment was given. Unfortunately, the patient’s condition deteriorated, and she developed dizziness and disordered consciousness. The muscle strength in her right limbs progressively weakened, and higher brain functions gradually declined.
On day 45, the patient was transferred back to our hospital and another MRI scan was performed (Figure 1i–1l), which suggested that the range of the intracranial lesions had increased compared with the earlier MRI. An infectious lesion was still considered to be the most likely diagnosis. The patient’s condition continued to deteriorate because no new treatment was administered.
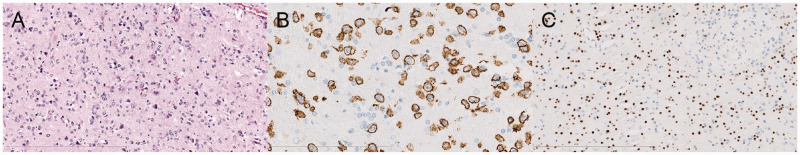
On day 57, the patient underwent a stereotactic biopsy of the right temporal lobe via neurosurgery. During the subsequent hospitalization, the patient’s condition deteriorated further, and she was transferred to the intensive care unit. However, the disease progression could not be controlled, and the patient died after 1 week. At 1 week after her death, this patient’s case had been repeatedly discussed in the pathology department. The final diagnosis was non-Hodgkin lymphoma, specifically, an invasive, primary, diffuse large B-cell lymphoma of the central nervous system. Application of the Hans algorithm suggested a non-germinal center, B cell-derived tumor. The tumor was a double-expressor lymphoma that expressed myc and BCL2 (Figure 2).
Figure 2.
Pathological biopsy: (a) Lymphoma cells and glioma cell proliferation (hematoxylin and eosin). (b, c) Immunohistochemical staining showing (b) CD20 (+), (c) Oligo II (+), and proliferating cells derived from B lymphocytes instead of glioma cells.
Discussion
The clinical manifestations of PCNSL are non-specific, with the most common symptoms being cognitive decline and gait disturbance,3 which are similar to our patient’s initial presentation. The MRI appearance of PCNSL is characterized by iso- or hypointense signals on T1-weighted images, iso- or slightly hyperintense signals on T2-weighted images, hyperintense signals on fluid-attenuated inversion recovery images, and plaque enhancement4 on contrast-enhanced images. The early MRI features of our patient were atypical. Additionally, the patient had a special medical history of exposure to decomposing corpses before symptom onset, and multiple MRI examinations suggested an intracranial infection; therefore, we considered that a viral infection was likely. Thus, we treated the patient with acyclovir, but this was the wrong decision because the MRIs had consistently shown localized lesions, which are less likely caused by viral infections. With few exceptions, viral infections are not likely to manifest with focal deficits, and they usually manifest with global symptoms. Therefore, a bacterial infection was more likely compared with a viral infection in our patient. However, there was no evidence of bacterial, fungal, viral, or parasitic infection on multiple tests. The patient had bilateral paraventricular lesions on MRI and PET-CT, which suggested a diagnosis of lymphoma. Because of the clinical history and imaging findings, the diagnosis should have been PCNSL with a differential diagnosis of demyelination, vasculitis, or an infective lesion, although the patient did not have any systemic symptoms such as fever. This point was not taken into account in the management of the patient, and it resulted in the patient not being accurately diagnosed and treated. Because of the low incidence of PCNSL in immunocompetent patients and the lack of specific clinical manifestations and positive auxiliary examinations, the disease was easily missed and misdiagnosed.
Several inferences about the diagnosis and treatment of PCNSL were made based on this patient’s case, and they are discussed below.
First, the overall incidence of PCNSL has recently increased, and the 5-year and 10-year survival rates for PCNSL are 29.9% and 22.2%, respectively.5 A clear diagnosis requires a histopathological biopsy. Therefore, in patients with an unclear diagnosis of central nervous system diseases and a strong suspicion of PCNSL, a stereotactic biopsy should be performed as soon as possible to confirm the diagnosis. In cases where the imaging is deemed to be obscure, a biopsy is mandatory for evidence-based treatment. A timely biopsy will allow sufficient time to administer radiotherapy and chemotherapy, and thereby increase the chances of a good response to treatment.
Second, PET-CT is more accurate than MRI for diagnosing PCNSL. Statistical analyses have found that 18-FDG PET-CT imaging is helpful for the differential diagnosis of PCNSLs and other tumors, and that this test is superior to MRI.6 In our patient, PET-CT that was performed early in the course of the disease suggested the possibility of lymphoma, so we believe that PET-CT is of greater value than MRI for the early diagnosis of PCNSLs.
Third, corticosteroids should be used with caution before the diagnosis of central nervous system diseases because in patients with PCNSL, corticosteroid therapy may inhibit tumor growth or even cause the tumor to subside, thus affecting the accuracy of the biopsy.7 Usually, a diagnosis should be obtained before any kind of treatment is administered. In our patient, histopathological interpretation was difficult because dexamethasone treatment resulted in tumor tissue necrosis, and accurate histopathological diagnosis took 2 weeks in this case.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Ethics
Consent was obtained from the patient’s son to publish this patient’s case. The manuscript does not disclose the patient’s private information.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iD
Ligang Chen https://orcid.org/0000-0003-0516-4496
References
- 1.Jaffe E, Swerdlow SHCE, Campo E, et al. WHO Classification of Tumours of the Haematopoietic and Lymphoid Tissues, 2008.
- 2.Bathla G, Hegde A. Lymphomatous involvement of the central nervous system. Clin Radiol 2016; 71: 602–609. [DOI] [PubMed] [Google Scholar]
- 3.Izquierdo C, Velasco R, Vidal N, et al. Lymphomatosis cerebri: a rare form of primary central nervous system lymphoma. Analysis of 7 cases and systematic review of the literature. Neuro Oncol 2016; 18: 707–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sutherland T, Yap K, Liew E, et al. Primary central nervous system lymphoma in immunocompetent patients: a retrospective review of MRI features. J Med Imaging Radiat Oncol 2012; 56: 295–301. [DOI] [PubMed] [Google Scholar]
- 5.Ostrom QT, Gittleman H, Fulop J, et al. CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2008-2012. Neuro Oncol 2015; 17: iv1–iv62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lewerenz J, Ding XQ, Matschke J, et al. Dementia and leukoencephalopathy due to lymphomatosis cerebri. BMJ Case Rep 2009; 2009: r8-r2008. DOI: 10.1136/bcr.08.2008.0752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fox CP, Phillips EH, Smith J, et al. Guidelines for the diagnosis and management of primary central nervous system diffuse large B-cell lymphoma. Br J Haematol 2019; 184: 348–363. [DOI] [PubMed] [Google Scholar]