Abstract
Background:
Although patients have experienced significant improvements after hip arthroscopy for femoroacetabular impingement (FAI), prior studies suggest that women have worse outcomes than men. These previous studies lack comparisons of patient-reported outcome (PRO) scores based on gender with respect to clinical significance measurements, including the minimal clinically important difference (MCID) and patient acceptable symptom state (PASS).
Purpose:
To evaluate outcomes after hip arthroscopy for FAI based on patient gender by prospectively assessing changes in PRO scores, MCID, and PASS.
Study Design:
Cohort study; Level of evidence, 2.
Methods:
Women and men undergoing hip arthroscopy for FAI were prospectively enrolled, and preoperative radiographic and intraoperative findings were collected. Patients completed the following PRO surveys before surgery and 2 years postoperatively: modified Harris Hip Score (mHHS), Hip disability and Osteoarthritis Outcome Score (HOOS), and 12-Item Short Form Health Survey. Mean scores and percentage of patients reaching MCID and PASS were analyzed.
Results:
A total of 131 hips were included (72 women, 59 men). Women had smaller preoperative alpha angles (59.1° vs 63.7°, respectively; P < .001) and lower acetabular cartilage injury grade (6.9% vs 22.0% with grade 4 injury, respectively; P = .013). Both women and men achieved equivalent significant improvements in PRO scores after surgery (scores increased 18.4 to 45.1 points for mHHS and HOOS). Women and men reached PASS for mHHS at similar rates (76.4% and 77.2%, respectively; P = .915). MCID was also achieved at similar rates between women and men for all scores (range, 61.4%-88.9%) except the activities of daily living subscale of the HOOS, in which a greater percentage of women reached MCID compared with men (79.2% vs 62.7%, respectively; P = .037). Additional stratification by age group using the median cohort age of 34 years showed no significant differences in PRO improvement based on age group for each gender.
Conclusion:
Women can achieve clinically meaningful improvements in PRO scores after hip arthroscopy for FAI. Compared with men, women demonstrated equivalent high rates of achieving MCID and PASS at 2 years after surgery.
Keywords: hip arthroscopy, femoroacetabular impingement (FAI), gender, patient outcomes, minimal clinically important difference (MCID), patient acceptable symptomatic state (PASS)
Hip arthroscopy is a minimally invasive procedure used to treat a variety of conditions such as femoroacetabular impingement (FAI), labral tears, and cartilage injury.3,14,33 The incidence of hip arthroscopy procedures and the number of surgeons performing such procedures have rapidly increased in the past decade, making hip arthroscopy a topic of significant interest with regard to patient outcomes.2,3,33 In general, patients do well after hip arthroscopy for FAI and show significant improvements in patient-reported outcome (PRO) scores evaluating hip pain, function, activities of daily living, quality of life, and sport-specific activities.9,11,14 These patients typically meet the minimal clinically important difference (MCID) and patient acceptable symptom state (PASS) early in the postoperative course and may continue to show progress at 1- and 2-year follow-up.5,11,28
Previous studies have reported that within FAI cohorts, there are differences based on patient sex with regard to presentation, radiographic results, and intraoperative findings.12,14,16,25,30,32,34 Female patients typically have smaller cam lesions as measured by alpha angle, as well as increased incidence of global acetabular retroversion and acetabular dysplasia.16,25,32,34 Nepple et al25 compared intraoperative cartilage differences and found a lower incidence of advanced acetabular cartilage changes in female versus male patients. In terms of outcomes, although both female and male patients improve after hip arthroscopy, previous studies have described differences in patient outcomes based on sex.12,14,30 Two large reviews described female sex as a significant predictor of revision surgery and conversion to total hip arthroplasty.21,23 Additionally, in an analysis of more than 700 primary hip arthroscopies, female sex was an associated risk factor for revision surgery.14 However, a population-based study did not find female sex associated with an increased risk of revision surgery, which differs from the previous studies mentioned.10
Prior studies have also shown that women reported poorer preoperative disability and function on PRO surveys compared with men.16,18,25,32 In a matched-group analysis, Frank et al12 examined female and male patients’ postoperative outcomes at 2 years after hip arthroscopy for FAI. Both female and male groups improved significantly from preoperative to postoperative assessments, but at 2-year follow-up, female patients older than 45 years had lower scores compared with younger female groups and with all male patient groups.12 Although these studies show significant PRO improvements in both groups, women have demonstrated lower baseline scores and have decreased improvement compared with men after hip arthroscopy for FAI.12
Threshold PRO score values such as the MCID and PASS have been increasingly defined and reported for patients undergoing FAI hip arthroscopy.5,20,22,28 The MCID represents the threshold change in PRO score beyond which patients can be considered to have seen clinically significant improvements.20,22,28 PASS is typically a higher numeric score, as it constitutes the PRO score at which patients are satisfied with their symptoms and function.5,22 Use of MCID and PASS has improved the interpretation of postoperative data by standardizing the definition of clinically important improvements rather than relying solely on statistical significance which may not truly represent meaningful change. As Chahal et al5 described, the MCID measures the concept of improvement or “feeling better,” whereas the PASS can be used to assess the concept of well-being or “feeling good.”5
The purpose of this study was to evaluate outcomes after hip arthroscopy for FAI based on patient gender by assessing changes in pre- to postoperative PRO score, MCID, and PASS. To our knowledge, previous research has not assessed gender differences in adult patients using MCID and PASS after hip arthroscopy. We hypothesized that both women and men will achieve significant clinical improvements and that women will reach MCID and PASS at similar rates compared with men at 2 years after hip arthroscopy for FAI.
Methods
Patient Selection and Data Collection
An institutional review board reviewed and approved the study protocol, and all patients gave written informed consent before enrollment. Patients with FAI undergoing hip arthroscopy were prospectively enrolled. A single sports medicine surgeon (A.L.Z.), who is fellowship trained with a focus on hip arthroscopy, performed all surgical procedures. Inclusion criteria included patients with symptomatic cam and/or pincer-type FAI with failure of nonoperative treatment including physical therapy and activity modification. Exclusion criteria included age younger than 18 or older than 60 years at the time of surgery, revision surgery, non-FAI primary procedure, osteoarthritis (Tönnis grade ≥2), hip dysplasia (lateral center-edge angle [LCEA] <25°), and hypermobility (Beighton score ≥4). Intra-articular injections for diagnostic and therapeutic purposes before hip arthroscopy were not a strict inclusion criterion, because some patients refused injections and chose surgical intervention after nonoperative treatment with physical therapy had failed.
Baseline preoperative PRO surveys were collected before surgery, and patients also completed PRO surveys at 2 years postoperatively. A total of 147 patients were enrolled, but 16 did not complete 2-year postoperative PRO surveys, giving a 2-year follow-up rate of 89.1%. The final cohort consisted of 131 hips (59 men and 72 women). Patient demographics including age, gender, and body mass index were recorded. The cohort was stratified based on self-identified patient gender. Because of the inclusion of transgender individuals in this study (which accounted for <5% of the cohort), we used the term gender as well as the terms women and men to describe our patients as opposed to the term sex and the terms female and male. Patients underwent pre- and postoperative radiographs of the pelvis in the supine anterior-posterior plane, Dunn lateral 45°, and false profile views, in addition to preoperative magnetic resonance imaging of the affected hip.29 Radiographic measurements, including alpha angle, LCEA, and Tönnis grade, were recorded preoperatively.
Surgical Treatment and Rehabilitation
All procedures were performed in the ambulatory surgery center of a tertiary-referral academic medical center. Two arthroscopic portals (anterolateral and midanterior) and a periportal capsulotomy was used.6,24 Based on the classification by Beck et al,1 the acetabular cartilage, femoral cartilage, and labral condition were recorded. Procedure time from incision to closure, and traction time were recorded. An acetabuloplasty followed by labral repair and femoroplasty were performed if indicated, as standard treatment based on FAI type. Further procedures were performed if indicated, including microfracture, iliotibial band release, and chondroplasty. Capsular closure was performed on patients who were at risk for postoperative instability or who had greater joint laxity. Intra- and postoperative complications were recorded.
Patients were limited to touch-down weightbearing with crutches for 2 weeks postoperatively and after 2 weeks were advanced to weightbearing as tolerated. For rehabilitation and strengthening, a comprehensive physical therapy program was used with progression to a running program at 3 months after surgery and return to sports at 5 to 6 months after surgery.
Patient-Reported Outcomes
Patients completed 3 PRO surveys preoperatively and at 2 years postoperatively: the modified Harris Hip score (mHHS), the Hip disability and Osteoarthritis Outcome Score (HOOS), and the 12-Item Short Form Health Survey (SF-12). These surveys are validated and widely used outcome measures in hip arthroscopy to assess a patient’s symptoms, pain, functional status, and quality of life (QoL).20,31 The mHHS provides a single score out of 100, assessing hip pain and function.4,15 The HOOS is divided into 5 subsection scores: symptoms, pain, activities of daily living (ADL), sports, and QoL.26,27 The SF-12 survey contains a physical component score (PCS) and a mental component score (MCS) to assess physical and mental health–related QoL.13,17,19,35 Additionally, patients rated their pain pre- and postoperatively on a visual analog scale from 0 to 10, with 0 referring to no pain and 10 referring to the most painful. All data were collected in REDCap (v 8.10.11).
Statistical Analysis
An a priori power calculation was performed from a previous study of hip arthroscopy for FAI using preoperative and 2-year postoperative mHHS scores9; this calculation indicated that 42 hips were needed to adequately power the study to 1-β = 0.95. A post hoc power analysis conducted for mHHS scores revealed a power of 99.8% for this cohort. A chi-square test was used to evaluate statistical significance for categorical variables. To evaluate improvement from preoperative to 2-year postoperative scores within the cohorts of women and men, a paired Student t test was used. To evaluate baseline and 2-year statistical differences between the cohorts of women and men, an unpaired Student t test was used. The change in PRO score (defined as the 2-year score minus the preoperative score) was used to quantify patient improvement. An unpaired Student t test was used to evaluate statistical differences between the change in PRO scores between women and men.
Previously published MCID and PASS values for hip arthroscopy surgery were used to determine the number of patients who met MCID and/or PASS in our cohort at 2 years postoperatively.5,20 The MCID values were as follows: mHHS, 8; HOOS-symptoms, 9; HOOS-pain, 9; HOOS-ADL, 6; HOOS-sports, 10; and HOOS-QoL, 11.20 If the change in score was equal to or greater than the MCID value, the patient was classified as meeting the MCID. The PASS value for mHHS was 74.5 If the patient’s score at 2 years postoperatively was equal to or greater than 74, the patient was classified as meeting the PASS. To our knowledge, there is currently no defined PASS for HOOS with respect to hip arthroscopy for FAI in the literature. To explore patient gender and age, we stratified the cohorts of women and men by median age and analyzed the change in PRO score between the groups using a 1-way analysis of variance (ANOVA). P < .05 was considered statistically significant for all calculations. All statistical analyses were conducted in StatPlus: mac (v 6.7.1.0; AnalystSoft Inc). SF-12 scores were calculated, with permission, via the Veterans RAND 12-Item Health Survey scoring programs in R software (v 3.4.0; R Foundation for Statistical Computing).
Results
Demographic and Radiographic Findings
Demographics for the 72 women and 59 men are provided in Table 1. The mean ± SD age for women and men was 34.2 versus 35.8 years, respectively (P = .347), and body mass index was 24.9 versus 25.5 kg/m2, respectively (P = .379). The median age of the cohort was 34 years. Percentages of Tönnis grades 0 and 1 for women and men were 65.2% and 34.7% versus 44.1% and 55.9%, respectively (P = .015). The mean alpha angle for women and men was 59.1° versus 63.7°, respectively (P < .001) and the LCEA was 33.9° versus 33.3°, respectively (P = .543).
Table 1.
Patient Demographicsa
| Characteristics | Women | Men | P Value |
|---|---|---|---|
| Age, y (median age 34 y) | 34.2 ± 9.5 | 35.8 ± 10.3 | .347b |
| Age <34 y, n | 39 | 26 | .250c |
| Age ≥34 y, n | 33 | 33 | |
| Body mass index, kg/m2 | 24.9 ± 4.4 | 25.5 ± 3.3 | .379b |
| Left side involved, n | 36 | 25 | .384c |
| Right side involved, n | 36 | 34 | |
| Tönnis grade, % | .015 c,d | ||
| Grade 0 | 65.2 | 44.1 | |
| Grade 1 | 34.7 | 55.9 | |
| Alpha angle, deg | 59.1 ± 5.0 | 63.7 ± 5.2 | <.001 b |
| Lateral center-edge angle, deg | 33.9 ± 6.3 | 33.3 ± 6.1 | .543b |
| Crossover sign, % | 47.2 | 40.7 | .453c |
aValues are expressed as mean ± SD unless otherwise noted. Bolded P values indicate statistically significant differences between groups (P < .05).
bUnpaired Student t test.
cChi-square test.
d P value for between-group differences in Tönnis grades 0 and 1.
Intraoperative Findings
Intraoperative findings are provided in Table 2. The procedure time for women and men was 89.9 versus 97.0 minutes, respectively (P = .090), and traction time was 56.6 versus 56.6 minutes, respectively (P = .985). Women had a higher percentage of grade 2 acetabular cartilage condition than men (42.7% vs 22.0%, respectively; P = .017) and a lower percentage of grade 4 acetabular cartilage condition (6.9% vs 22.0%, respectively; P = .013). All 72 women and 59 men underwent femoroplasty, and 65.3% of women and 66.1% of men underwent acetabuloplasty. The majority of patients from both groups underwent labral repair, with only 1 woman and 1 man receiving labral debridement. There were 14 capsular repairs for women and 1 capsular repair for men.
Table 2.
Intraoperative Findingsa
| Intraoperative Findings | Women | Men | P Valueb |
|---|---|---|---|
| Procedure time, min, mean ± SD | 89.9 ± 25.8 | 97.0 ± 22.1 | .090 |
| Traction time, min, mean ± SD | 56.6 ± 19.6 | 56.6 ± 17.5 | .985 |
| Wave sign positive, % | 77.8 | 47.5 | |
| Femoroplasty (cam resection), % | 100.0 | 100.0 | |
| Acetabuloplasty (pincer resection), % | 65.3 | 66.1 | |
| Labral tear, n | 72 | 58 | |
| Labral repair, n | 71 | 57 | |
| Labral debridement, n | 1 | 1 | |
| Microfracture, n | 4 | 4 | |
| IT band release, n | 3 | 0 | |
| Chondroplasty, n | 4 | 7 | |
| Capsule repair, n | 14 | 1 | |
| Beck acetabular cartilage condition, % | P Valuec | ||
| 0 (normal) | 2.8 | 1.7 | .680 |
| 1 (malacia) | 4.2 | 8.5 | .306 |
| 2 (debonding) | 42.7 | 22.0 | .017 |
| 3 (cleavage) | 44.4 | 45.8 | .197 |
| 4 (defect) | 6.9 | 22.0 | .013 |
| Beck femoral cartilage condition, % | |||
| 0 (normal) | 9.7 | 3.4 | .154 |
| 1 (malacia) | 41.7 | 35.6 | .478 |
| 2 (debonding) | 29.2 | 33.9 | .981 |
| 3 (cleavage) | 15.3 | 27.1 | .095 |
| 4 (defect) | 4.2 | 0.0 | .113 |
| Beck labral classification, % | |||
| 0 (normal) | 0.0 | 1.7 | .271 |
| 1 (degeneration) | 4.2 | 1.7 | .413 |
| 2 (full thickness tear) | 44.4 | 33.9 | .220 |
| 3 (detachment) | 51.4 | 62.7 | .193 |
| 4 (ossification) | 0.0 | 0.0 |
aBolded P values indicate statistically significant differences between groups (P < .05).
bUnpaired Student t test.
cChi-square test.
Patient Outcomes
No major complications were noted in this cohort. Minor complications included neurapraxias, which resolved by 3 to 4 weeks: 4 in women (2 pudendal and 2 lateral femoral cutaneous nerve) and 3 in men (lateral femoral cutaneous nerve). No patients required revision arthroscopy surgery. There were 2 patients who converted to total hip arthroplasty (1 woman at 15 months after arthroscopy and 1 man at 17 months after arthroscopy, both aged >34 years).
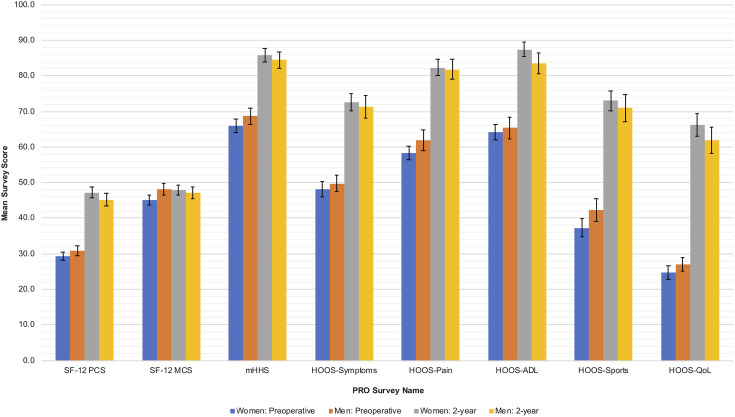
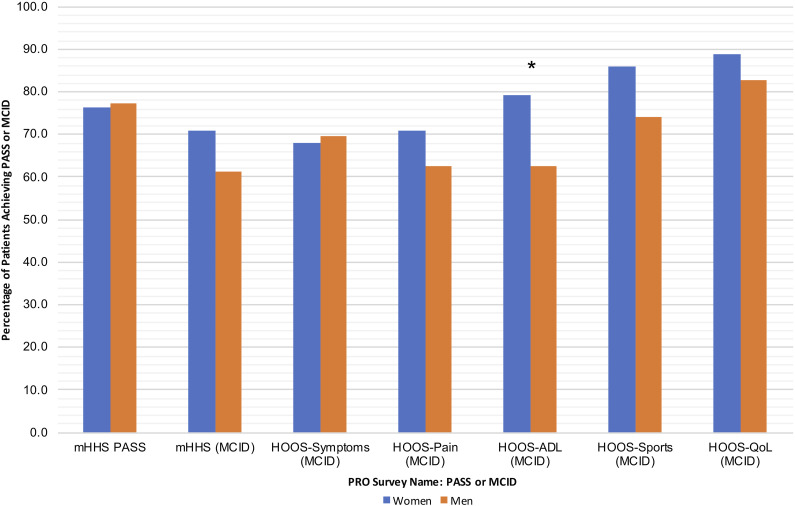
Baseline preoperative and 2-year postoperative PRO scores for women versus men are shown in Table 3 and Figure 1; no statistically significant differences were found between the two groups. Table 4 shows the preoperative versus 2-year postoperative PRO scores for women and for men. All PRO scores showed statistically significant improvement in women and men (P < .001 for all; women SF-12 MCS, P = .046) except the SF-12 MCS scores in the men (P = .581). Table 5 compares the change in preoperative and 2-year postoperative scores in women versus men; there were no statistically significant differences. The percentage and number of patients who met the MCID and PASS for mHHS and the MCID for HOOS subsections are provided in Table 6 and Figure 2. The percentage of women who met HOOS-ADL MCID (79.2%) was significantly greater than that of men (62.7%; P = .037). No statistically significant differences were noted between women and men in PASS for mHHS or MCID for mHHS, HOOS-symptoms, HOOS-pain, HOOS-sports, or HOOS-QoL. Table 7 shows the change in PRO scores in groups of women and men stratified by the median age of 34 years. No statistically significant differences were found between the 4 groups.
Table 3.
Comparison of Preoperative and 2-Year Postoperative Scores in Women Versus Mena
| Preoperative | 2 Years | |||||
|---|---|---|---|---|---|---|
| PRO Measure | Women | Men | P Valueb | Women | Men | P Valueb |
| VAS pain | 4.7 ± 2.4 | 4.2 ± 2.6 | .292 | 2.0 ± 2.5 | 1.9 ± 2.3 | .877 |
| SF-12 | ||||||
| PCS | 29.3 ± 9.0 | 30.9 ± 10.9 | .388 | 47.2 ± 12.6 | 45.1 ± 13.9 | .382 |
| MCS | 45.1 ± 12.5 | 48.2 ± 12.8 | .163 | 47.9 ± 12.2 | 47.1 ± 12.7 | .712 |
| mHHS | 65.9 ± 16.4 | 68.7 ± 17.6 | .342 | 85.8 ± 16.1 | 84.4 ± 17.6 | .631 |
| HOOS | ||||||
| Symptoms | 48.1 ± 17.7 | 49.7 ± 17.9 | .601 | 72.6 ± 19.9 | 71.3 ± 23.8 | .736 |
| Pain | 58.2 ± 16.2 | 61.9 ± 22.0 | .296 | 82.3 ± 19.8 | 81.8 ± 21.8 | .891 |
| ADL | 64.1 ± 18.2 | 65.3 ± 23.1 | .747 | 87.4 ± 17.4 | 83.6 ± 22.4 | .298 |
| Sports | 37.3 ± 22.0 | 42.3 ± 23.7 | .219 | 73.0 ± 23.6 | 70.9 ± 29.7 | .655 |
| QoL | 24.7 ± 17.1 | 26.9 ± 14.8 | .433 | 66.2 ± 27.5 | 61.9 ± 28.8 | .380 |
aValues are expressed as mean ± SD. ADL, activities of daily living; HOOS, Hip disability and Osteoarthritis Outcome Score; MCS, mental component score; mHHS, modified Harris Hip Score; PCS, physical component score; PRO, patient-reported outcome; QoL, quality of life; SF-12, 12-Item Short Form Health Survey; VAS, visual analog scale.
bUnpaired Student t test.
Figure 1.
Comparison of the baseline preoperative and 2-year postoperative patient-reported outcome (PRO) scores for women and men. No statistically significant differences were found in baseline preoperative scores or 2-year postoperative scores between women and men for the 12-Item Short Form Health Survey (SF-12) physical component score (PCS) or mental component score (MCS); the modified Harris Hip Score (mHHS); or the Hip disability and Osteoarthritis Outcome Score (HOOS) subscales for symptoms, pain, activities of daily living (ADL), sports, and quality of life (QoL) (P > .05 for all). Error bars represent SE.
Table 4.
Comparison of Preoperative Versus 2-Year Postoperative Values in Women and Mena
| Women | Men | |||||
|---|---|---|---|---|---|---|
| PRO Measure | Preoperative | 2 Years | P Valueb | Preoperative | 2 Years | P Valueb |
| VAS pain | 4.7 ± 2.4 | 2.0 ± 2.5 | <.001 | 4.2 ± 2.6 | 1.9 ± 2.3 | <.001 |
| SF-12 | ||||||
| PCS | 29.4 ± 9.1 | 46.9 ± 12.5 | <.001 | 30.8 ± 11.0 | 45.2 ± 14.0 | <.001 |
| MCS | 45.0 ± 12.7 | 48.3 ± 11.7 | .046 | 48.3 ± 12.8 | 47.2 ± 12.8 | .581 |
| mHHS | 65.9 ± 16.3 | 85.8 ± 16.1 | <.001 | 68.4 ± 17.9 | 84.4 ± 17.6 | <.001 |
| HOOS | ||||||
| Symptoms | 48.1 ± 17.7 | 72.6 ± 19.9 | <.001 | 49.7 ± 17.9 | 71.3 ± 23.8 | <.001 |
| Pain | 58.2 ± 16.2 | 82.3 ± 19.8 | <.001 | 61.9 ± 22.0 | 81.8 ± 21.8 | <.001 |
| ADL | 64.1 ± 18.2 | 87.4 ± 17.4 | <.001 | 65.3 ± 23.1 | 83.6 ± 22.4 | <.001 |
| Sports | 37.3 ± 22.0 | 73.0 ± 23.6 | <.001 | 42.3 ± 23.7 | 70.7 ± 30.0 | <.001 |
| QoL | 24.7 ± 17.1 | 66.2 ± 27.5 | <.001 | 26.9 ± 14.8 | 61.9 ± 29.1 | <.001 |
aValues are expressed as mean ± SD. Bolded P values indicate statistically significant differences between groups (P < .05). ADL, activities of daily living; HOOS, Hip disability and Osteoarthritis Outcome Score; MCS, mental component score; mHHS, modified Harris Hip Score; PCS, physical component score; PRO, patient-reported outcome; QoL, quality of life; SF-12, 12-Item Short Form Health Survey; VAS, visual analog scale.
bPaired Student t test.
Table 5.
Comparison of Change in Postoperative PRO Scores Between Women and Mena
| PRO Measure | Women | Men | P Valueb |
|---|---|---|---|
| VAS pain | –2.7 ± 3.2 | –2.3 ± 2.3 | .415 |
| SF-12 | |||
| PCS | 17.5 ± 14.2 | 14.3 ± 15.3 | .241 |
| MCS | 3.4 ± 13.8 | –1.1 ± 14.9 | .086 |
| mHHS | 19.9 ± 18.7 | 15.9 ± 20.5 | .256 |
| HOOS | |||
| Symptoms | 24.5 ± 22.8 | 21.5 ± 22.2 | .456 |
| Pain | 24.1 ± 21.1 | 20.0 ± 24.1 | .305 |
| ADL | 23.3 ± 19.3 | 18.4 ± 24.0 | .205 |
| Sports | 35.7 ± 28.9 | 28.4 ± 31.8 | .177 |
| QoL | 41.5 ± 27.4 | 34.9 ± 27.9 | .180 |
aValues are expressed as mean ± SD. ADL, activities of daily living; HOOS, Hip disability and Osteoarthritis Outcome Score; MCS, mental component score; mHHS, modified Harris Hip Score; PCS, physical component score; PRO, patient-reported outcome; QoL, quality of life; SF-12, 12-Item Short Form Health Survey; VAS, visual analog scale.
bUnpaired Student t test.
Table 6.
Comparison of the Percentage of Patients Reaching PASS and MCID Between Women and Mena
| PRO Measure | Women | Men | P Valueb |
|---|---|---|---|
| mHHS (PASS = 74) | 76.4 (55/72) | 77.2 (44/57) | .915 |
| mHHS (MCID = 8) | 70.8 (51/72) | 61.4 (35/57) | .259 |
| HOOS | |||
| Symptoms (MCID = 9) | 68.1 (49/72) | 69.5 (41/59) | .860 |
| Pain (MCID = 9) | 70.8 (51/72) | 62.7 (37/59) | .325 |
| ADL (MCID = 6) | 79.2 (57/72) | 62.7 (37/59) | .037 |
| Sports (MCID = 10) | 86.1 (62/72) | 74.1 (43/58) | .085 |
| QoL (MCID = 11) | 88.9 (64/72) | 82.8 (48/58) | .314 |
aValues are expressed as percentage and number of patients out of total eligible. Bolded P values indicate statistically significant differences between groups (P < .05). ADL, activities of daily living; HOOS, Hip disability and Osteoarthritis Outcome Score; MCID, minimally clinical important difference; mHHS, modified Harris Hip Score; PASS; patient acceptable symptom state; PRO, patient-reported outcome; QoL, quality of life.
bChi-square test.
Figure 2.
Comparison of the percentage of women and men achieving the patient acceptable symptom state (PASS) for the modified Harris Hip Score (mHHS) and the minimal clinically meaningful difference (MCID) for mHHS and the Hip Osteoarthritis Outcome Score (HOOS) subscales for symptoms, pain, activities of daily living (ADL), sports, and quality of life (QoL). *The percentage of women who achieved MCID for HOOS-ADL was greater than that for men (P = .037). PRO, patient-reported outcome.
Table 7.
Comparison of the Change in Postoperative Score Stratified by Median Age of 34 Years and Gendera
| PRO Measure | Women <34 y | Women ≥34 y | Men <34 y | Men ≥34 y | P Valueb |
|---|---|---|---|---|---|
| VAS pain | –2.4 ± 3.2 | –2.9 ± 3.3 | –2.7 ± 2.3 | –1.9 ± 2.4 | .497 |
| SF-12 | |||||
| PCS | 18.5 ± 14.8 | 16.3 ± 13.5 | 14.6 ± 16.1 | 14.1 ± 14.9 | .614 |
| MCS | 2.9 ± 14.7 | 3.9 ± 12.9 | 1.5 ± 16.6 | –3.2 ± 13.2 | .207 |
| mHHS | 19.5 ± 19.0 | 20.4 ± 18.7 | 18.4 ± 20.3 | 14.0 ± 20.7 | .563 |
| HOOS | |||||
| Symptoms | 29.1 ± 24.5 | 19.1 ± 19.6 | 26.1 ± 21.0 | 17.9 ± 22.8 | .110 |
| Pain | 26.2 ± 21.1 | 21.6 ± 21.2 | 23.0 ± 25.9 | 17.6 ± 22.7 | .448 |
| ADL | 24.0 ± 20.0 | 22.5 ± 18.7 | 18.2 ± 24.4 | 18.5 ± 24.1 | .625 |
| Sports | 33.0 ± 33.2 | 39.0 ± 22.6 | 36.6 ± 30.9 | 22.2 ± 31.5 | .122 |
| QoL | 43.9 ± 28.9 | 38.6 ± 25.6 | 43.5 ± 27.5 | 27.9 ± 26.6 | .070 |
aValues are expressed as mean ± SD. ADL, activities of daily living; HOOS, Hip disability and Osteoarthritis Outcome Score; MCS, mental component score; mHHS, modified Harris Hip Score; PCS, physical component score; PRO, patient-reported outcome; QoL, quality of life; SF-12, 12-Item Short Form Health Survey; VAS, visual analog scale.
bOne-way analysis of variance.
Discussion
The purpose of this study was to evaluate preoperative and 2-year postoperative outcomes after hip arthroscopy for FAI based on patient gender using PRO and clinically meaningful improvement measurements. In this prospective cohort of 131 hips with 89% 2-year follow-up, we found that women achieved significant improvements in multiple PRO scores and reached MCID and PASS at high rates after hip arthroscopy for FAI. Further, the improvements achieved by women were equivalent to those seen in men. The results of this study may be important, as previous studies have shown female patients to have a higher risk of revision surgery and less improvement after hip arthroscopy for FAI compared with male patients.12,14,21,23 As these previous findings may potentially lead to bias in recommendation of surgery based on patient sex or gender, it is necessary to accrue additional data on this issue.
In this study, women demonstrated equivalent PRO findings compared with men. The women in this study did not have statistically significantly lower preoperative scores compared with men, which differed from previous studies indicating that women had worse baseline disability and function.16,18,25,32 When comparing 2-year postoperative scores, we found that women in our study reached similar outcomes compared with men, which agreed with the findings of Joseph et al.18 However, our results differed from those of Frank et al,12 who found worse final postoperative outcomes in female patients older than 45 years compared with male patients and with younger females. We also found no significant differences in amount of PRO score improvement in women and men. Joseph et al showed that women had statistically significantly greater improvement in Hip Outcome Score ADL (HOS-ADL) and International Hip Outcome Tool compared with men, which is reasonable given the lower baseline preoperative scores in women within that study.
Interestingly, a larger percentage of women met the MCID for HOOS-ADL compared with men in our current study. Otherwise, there was no difference in the percentage of women versus men who met the MCID and PASS. In a study evaluating outcomes after hip arthroscopy for FAI in adolescents, Cvetanovich et al8 also found no gender-based differences in MCID and PASS outcomes. To our knowledge, no previous studies have used MCID and PASS scores to compare results based on gender in adults undergoing hip arthroscopy. Therefore, the MCID and PASS may be better indicators of clinical significance in pain and function after hip arthroscopy compared with final postoperative PRO values.5,20,22,28
Further analysis of patient outcomes from this cohort showed that both women and men had statistically significant improvements in PRO scores from preoperative to 2-year postoperative, which is similar to past studies. The change in mHHS scores for women and men in our study was comparable with the finding of Cvetanovich et al9 in adults (19.9 and 15.0 vs 18.0, respectively). The current study had higher preoperative mHHS for women and for men when compared with Frank et al12 (65.9 vs 58.4 and 68.7 vs 59.3, respectively) but the 2-year postoperative scores in this study were comparable with those of Frank et al (women: 85.8 vs 80.4 and men: 84.4 vs 83.4, respectively). Compared with women and men in this study, Cooper et al7 described similar improvements in HOOS scores at latest follow-up (minimum 9 months) in patients older than 25 years: symptoms (24.5 and 21.5 vs 23.6), pain (24.1 and 20.0 vs 20.1), ADL (23.3 and 18.4 vs 22.4), sports (35.7 and 28.4 vs 23.3), and QoL (41.5 and 34.9 vs 22.2), respectively. The larger increases we saw in HOOS-sports and QoL may be because these scores continue to increase until 2-year follow-up based on a prior study,11 and Cooper et al had a minimum 9-month follow-up. The percentage of women who reached the MCID for the mHHS was similar in this study compared with all patients in the Cvetanovich et al9 study (70.8% vs 74.3%, respectively), but a smaller percentage of men met the MCID for mHHS (61.4% vs 74.3%). However, in this study, a greater percentage of women and men met PASS for the mHHS compared with Cvetanovich et al9 (76.4% and 77.2% vs 68.0%).
Our preoperative radiographic findings revealing smaller alpha angles in women and similar LCEA between genders were comparable with prior studies comparing women and men. Hetsroni et al,16 Nepple et al,25 and Salvo et al32 showed that women had smaller alpha angles compared with men (47.8° vs 63.6°, 57.6° vs 70.8°, and 59.5° vs 67.6°, respectively; all P < .001), which were similar to alpha angle findings in our study (59.1° vs 63.7°, respectively; P < .001).16,25,32 These findings suggest that women may have smaller or less obvious cam deformities than men. In the studies by Hetsroni et al, Nepple et al, and Salvo et al and in our study, the LCEAs between women and men were not statistically significantly different (33.1° vs 32.9°, 28.9° vs 30.0°, 32.4° vs 33.4°, and 33.9° vs 33.3°, respectively; all P > .05), demonstrating that the presentation of pincer-type impingement based on LCEA may not be different between women and men.16,25,32 In our study, men had a higher incidence of Tönnis grade 1 findings, and intraoperatively, men had more severe cartilage condition scores, which were similar to findings presented by Nepple et al.
The average ages of the women and men in this cohort were not statistically different, but to further explore association of age and outcome, we conducted a 1-way ANOVA using a 4-group stratification based on median age of 34 years and patient gender. We found no significant differences in PRO score improvement between the gender and age groups, demonstrating that men and women both younger and older than 34 years improved similarly. Although the number of hips in each age and gender group was unequal, this study was well-powered, with more than 42 hips for an a priori analysis power of 1-β = 0.959 and a post hoc power analysis of 99.8%. The similar improvements in age and gender groups found in this study may be because we excluded patients older than 60 years and those with Tönnis grade ≥2 radiographic findings. In patients in their 30s to 50s however, improvements can be attained after hip arthroscopy for FAI if in the absence of significant osteoarthritis or joint space narrowing on radiographs.
Differences in outcomes between this study and prior studies may be attributable to patient selection, surgical technique, and/or postoperative rehabilitation. This study excluded patients older than 60 years, patients with significant osteoarthritis, patients with dysplasia, and patients with revision surgery. Acetabular dysplasia is more common in women, and this exclusion criterion could account for some of our study findings. Additionally, the surgeon used a periportal capsulotomy technique that limits extensive capsule opening. More women had capsular closures in this study compared with men (14 vs 1), indicating that the surgeon more often believed that capsular closure was necessary to provide stability in women. This limited capsulotomy and repair may have helped women at risk of instability achieve acceptable postoperative outcomes.
Limitations of this study include analysis of patient outcomes from a single surgeon at a single institution, which may limit generalizability based on surgical technique, technical proficiency, and patient volume. Additionally, there may be demographic differences in patients who are referred to or who present to a tertiary medical center for treatment of FAI compared with community or rural hospital settings. In terms of FAI, we did not assess sagittal plane balance and femoral version in this group but used clinical and radiographic indicators for FAI. As mentioned above, there were varying numbers of patients in each group when stratifying by median age, but our study was well-powered for this subanalysis. Similar to Frank et al,12 we were limited by our ability to stratify age and gender groups further, because of the limited number of patients who could meet each age group.12 However, future studies with a larger number of patients should be conducted to further explore age and gender outcomes.
Because we used 2-year follow-up data, we are unable to comment on the long-term outcomes after hip arthroscopy, such as the rates of hip revision surgeries or total hip arthroplasty between women and men. No patients required a revision arthroscopy surgery, and 1 woman and 1 man converted to a total hip arthroplasty in this follow-up time frame. A goal for future studies is to further analyze this cohort as follow-up length after surgery increases. Finally, a potentially controversial aspect of this study is our stratification of patients based on self-identified gender rather than innate sex. As there are inherent differences in anatomic characteristics between females and males, using gender to stratify patients may be less accurate for this comparison. However, in our opinion it is appropriate to include patients in research based on their self-identified gender. Further, transgender patients represented less than 5% of this cohort, and any differences in their results are unlikely to statistically affect the overall similarities in outcomes between groups whether stratified by gender or sex.
Conclusion
Women can achieve clinically meaningful improvements in PRO scores after hip arthroscopy for FAI. Compared with men, women in this study demonstrated equivalent high rates of achieving MCID and PASS at 2 years after surgery.
Footnotes
Final revision submitted October 10, 2019; accepted October 18, 2019.
Accepted for presentation at the Annual Meeting of the AOSSM, July 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: C.C.C. has received educational support from Gemini Medical and Stryker. A.L.Z. has received consulting fees from Stryker and research support from Zimmer. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the University of California, San Francisco (IRB approval No. 14-14742).
References
- 1. Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7):1012–1018. [DOI] [PubMed] [Google Scholar]
- 2. Bonazza NA, Homcha B, Liu G, Leslie DL, Dhawan A. Surgical trends in arthroscopic hip surgery using a large national database. Arthroscopy. 2018;34(6):1825–1830. [DOI] [PubMed] [Google Scholar]
- 3. Bozic KJ, Chan V, Valone FH, Feeley BT, Vail TP. Trends in hip arthroscopy utilization in the United States. J Arthroplasty. 2013;28(8):140–143. [DOI] [PubMed] [Google Scholar]
- 4. Byrd JWT. Hip arthroscopy: patient assessment and indications. Instr Course Lect. 2003;52:711–719. [PubMed] [Google Scholar]
- 5. Chahal J, Van Thiel GS, Mather RC, et al. The patient acceptable symptomatic state for the modified Harris Hip Score and Hip Outcome Score among patients undergoing surgical treatment for femoroacetabular impingement. Am J Sports Med. 2015;43(8):1844–1849. [DOI] [PubMed] [Google Scholar]
- 6. Chambers CC, Monroe EJ, Flores SE, Borak KR, Zhang AL. Periportal capsulotomy: technique and outcomes for a limited capsulotomy during hip arthroscopy. Arthroscopy. 2019;35(4):1120–1127. [DOI] [PubMed] [Google Scholar]
- 7. Cooper AP, Basheer SZ, Maheshwari R, Regan L, Madan SS. Outcomes of hip arthroscopy: a prospective analysis and comparison between patients under 25 and over 25 years of age. Br J Sports Med. 2013;47(4):234–238. [DOI] [PubMed] [Google Scholar]
- 8. Cvetanovich GL, Weber AE, Kuhns BD, et al. Clinically meaningful improvements after hip arthroscopy for femoroacetabular impingement in adolescent and young adult patients regardless of gender. J Pediatr Orthop. 2018;38(9):465–470. [DOI] [PubMed] [Google Scholar]
- 9. Cvetanovich GL, Weber AE, Kuhns BD, et al. Hip arthroscopic surgery for femoroacetabular impingement with capsular management: factors associated with achieving clinically significant outcomes. Am J Sports Med. 2018;46(2):288–296. [DOI] [PubMed] [Google Scholar]
- 10. Degen RM, Pan TJ, Chang B, et al. Risk of failure of primary hip arthroscopy—a population-based study. J Hip Preserv Surg. 2017;4(3):214–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Flores SE, Sheridan JR, Borak KR, Zhang AL. When do patients improve after hip arthroscopy for femoroacetabular impingement? A prospective cohort analysis. Am J Sports Med. 2018;46(13):3111–3118. [DOI] [PubMed] [Google Scholar]
- 12. Frank RM, Lee S, Bush-Joseph CA, Salata MJ, Mather RC, Nho SJ. Outcomes for hip arthroscopy according to sex and age: a comparative matched-group analysis. J Bone Joint Surg. 2016;98(10):797–804. [DOI] [PubMed] [Google Scholar]
- 13. Gill SC, Butterworth P, Rodgers B, Mackinnon A. Validity of the mental health component scale of the 12-item Short-Form Health Survey (MCS-12) as measure of common mental disorders in the general population. Psychiatry Res. 2007;152(1):63–71. [DOI] [PubMed] [Google Scholar]
- 14. Gupta A, Redmond JM, Stake CE, Dunne KF, Domb BG. Does primary hip arthroscopy result in improved clinical outcomes? 2-year clinical follow-up on a mixed group of 738 consecutive primary hip arthroscopies performed at a high-volume referral center. Am J Sports Med. 2016;44(1):74–82. [DOI] [PubMed] [Google Scholar]
- 15. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty: an end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737–755. [PubMed] [Google Scholar]
- 16. Hetsroni I, Dela Torre K, Duke G, Lyman S, Kelly BT. Sex differences of hip morphology in young adults with hip pain and labral tears. Arthroscopy. 2013;29(1):54–63. [DOI] [PubMed] [Google Scholar]
- 17. Jones D, Kazis L, Lee A, et al. Health status assessments using the Veterans SF-12 and SF-36: methods for evaluating outcomes in the Veterans Health Administration. J Ambul Care Manage. 2001;24(3):68–86. [DOI] [PubMed] [Google Scholar]
- 18. Joseph R, Pan X, Cenkus K, Brown L, Ellis T, Di Stasi S. Sex differences in self-reported hip function up to 2 years after arthroscopic surgery for femoroacetabular impingement. Am J Sports Med. 2016;44(1):54–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kazis LE, Miller DR, Skinner KM, et al. Patient-reported measures of health: the Veterans Health Study. J Ambul Care Manage. 2004;27(1):70–83. [DOI] [PubMed] [Google Scholar]
- 20. Kemp JL, Collins NJ, Roos EM, Crossley KM. Psychometric properties of patient-reported outcome measures for hip arthroscopic surgery. Am J Sports Med. 2013;41(9):2065–2073. [DOI] [PubMed] [Google Scholar]
- 21. Kester BS, Capogna B, Mahure SA, Ryan MK, Mollon B, Youm T. Independent risk factors for revision surgery or conversion to total hip arthroplasty after hip arthroscopy: a review of a large statewide database from 2011 to 2012. Arthroscopy. 2018;34(2):464–470. [DOI] [PubMed] [Google Scholar]
- 22. Levy DM, Kuhns BD, Chahal J, Philippon MJ, Kelly BT, Nho SJ. Hip arthroscopy outcomes with respect to patient acceptable symptomatic state and minimal clinically important difference. Arthroscopy. 2016;32(9):1877–1886. [DOI] [PubMed] [Google Scholar]
- 23. Malviya A, Raza A, Jameson S, James P, Reed MR, Partington PF. Complications and survival analyses of hip arthroscopies performed in the national health service in England: a review of 6,395 cases. Arthroscopy. 2015;31(5):836–842. [DOI] [PubMed] [Google Scholar]
- 24. Monroe EJ, Chambers CC, Zhang AL. Periportal capsulotomy: a technique for limited violation of the hip capsule during arthroscopy for femoroacetabular impingement. Arthrosc Tech. 2019;8(2):e205–e208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Nepple JJ, Riggs CN, Ross JR, Clohisy JC. Clinical presentation and disease characteristics of femoroacetabular impingement are sex-dependent. J Bone Joint Surg Am. 2014;96(20):1683–1689. [DOI] [PubMed] [Google Scholar]
- 26. Nilsdotter A, Bremander A. Measures of hip function and symptoms: Harris Hip Score (HHS), Hip Disability and Osteoarthritis Outcome Score (HOOS), Oxford Hip Score (OHS), Lequesne Index of Severity for Osteoarthritis of the Hip (LISOH), and American Academy of Orthopedic Surgeons (AAOS) Hip and Knee Questionnaire. Arthritis Care Res (Hoboken). 2011;63(suppl 11):S200–S207. [DOI] [PubMed] [Google Scholar]
- 27. Nilsdotter AK, Lohmander LS, Klässbo M, Roos EM. Hip disability and Osteoarthritis Outcome Score (HOOS)—validity and responsiveness in total hip replacement. BMC Musculoskelet Disord. 2003;4:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Nwachukwu BU, Fields K, Chang B, Nawabi DH, Kelly BT, Ranawat AS. Preoperative outcome scores are predictive of achieving the minimal clinically important difference after arthroscopic treatment of femoroacetabular impingement. Am J Sports Med. 2017;45(3):612–619. [DOI] [PubMed] [Google Scholar]
- 29. Pfirrmann CWA, Mengiardi B, Dora C, Kalberer F, Zanetti M, Hodler J. Cam and pincer femoroacetabular impingement: characteristic MR arthrographic findings in 50 patients. Radiology. 2006;240(3):778–785. [DOI] [PubMed] [Google Scholar]
- 30. Poehling-Monaghan KL, Krych AJ, Levy BA, Trousdale RT, Sierra RJ. Female sex is a risk factor for failure of hip arthroscopy performed for acetabular retroversion. Orthop J Sports Med. 2017;5(11):2325967117737479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Renouf J, Pergaminelis N, Tran P, Tirosh O, Fary C. Prevalence and trends of patient-reported outcome measures used in hip arthroscopy. Orthopedics. 2019;42(3):e305–e308. [DOI] [PubMed] [Google Scholar]
- 32. Salvo JP, Nho SJ, Wolff AB, et al. Sex-dependent differences in preoperative, radiographic, and intraoperative characteristics of patients undergoing hip arthroscopy: results from the multicenter arthroscopic study of the hip group. Arthroscopy. 2018;34(3):844–852. [DOI] [PubMed] [Google Scholar]
- 33. Sing DC, Feeley BT, Tay B, Vail TP, Zhang AL. Age-related trends in hip arthroscopy: a large cross-sectional analysis. Arthroscopy. 2015;31(12):2307–2313. [DOI] [PubMed] [Google Scholar]
- 34. Tannenbaum EP, Zhang P, Maratt JD, et al. A computed tomography study of gender differences in acetabular version and morphology: implications for femoroacetabular impingement. Arthroscopy. 2015;31(7):1247–1254. [DOI] [PubMed] [Google Scholar]
- 35. Ware J, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. [DOI] [PubMed] [Google Scholar]