Abstract
Background:
A variety of thrower’s exostoses are grouped under the term Bennett lesion, which makes understanding diagnosis and treatment difficult.
Purpose:
To identify all types of reported thrower’s and overhead athlete’s exostoses and categorize them into a classification system to allow a morphology-based classification.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A systematic review of all articles pertaining to Bennett lesions and thrower’s exostosis was performed. The classification and treatments were evaluated to describe the types, proposed causes, diagnosis, and treatment options.
Results:
A total of 27 studies were included in the systematic review. The anatomic locations referenced in the study demonstrated posteroinferior, posterior, and posterosuperior glenoid lesions. Aggregate radiographic data demonstrated 158 of 306 patients (52%) with a thrower’s exostosis of any type and location. Of these 158 patients with a radiographic lesion, 119 (75%) patients were symptomatic. The locations were posteroinferior in 110 patients (70%), directly posterior in 2 patients (1.3%), posterosuperior in 44 patients (28%), and unknown in 2 patients (1.3%). Avulsed lesions were present in 9 (5.7%) posteroinferior lesions, 0 direct posterior lesions, and 2 (1.3%) posterosuperior lesions. Treatment plans included both nonoperative and operative strategies, but operative intervention was more commonly reported for detached lesions. After operative intervention, only 61% of reported athletes returned to preinjury performance.
Conclusion:
Based on a comprehensive review of the literature, we identified several anatomic locations for a thrower’s exostosis beyond the classic Bennett lesion. We categorized the reported exostoses into a new classification system for description of location and type (subperiosteal or free fragment) of the thrower’s exostosis, which may be used to study future treatments. Current treatment strategies recommend that surgical treatment of thrower’s exostosis is considered only after exhausting nonoperative management because reported return to sport is variable after surgery. The effectiveness of excision or repair for both subperiosteal and detached lesions has not been established.
Keywords: Bennett lesion, thrower’s exostosis, overhead athlete, glenohumeral internal rotation deficit (GIRD), posterosuperior impingement, treatment, classification
Thrower’s exostosis is a calcification found in the posterior region of the glenoid. The lesion was first described in professional baseball pitchers by George E. Bennett in 1941 as a posteroinferior lesion of the glenoid.4 He stated it was one of the distinctive lesions of the shoulder that could end a professional pitcher’s career.5 This pathology has a more recently reported prevalence of 22% in 55 asymptomatic major league pitchers.34 Numerous types of thrower’s exostosis have been categorized as a Bennett lesion; however, these lesions differ in both presentation and treatment.#
The anatomic differences and variability in presentation are further compounded by a lack of consensus on the most effective treatment approach for thrower’s exostosis. Inconsistent treatment strategies are underscored by only a 55% to 69% rate of return to the same level sport after treatment.22,35 Thrower’s exostosis is commonly associated with concomitant intra-articular pathology, especially posterior labral injury and undersurface rotator cuff tears.16,22 The heterogeneity in location and treatment precludes definitive recommendations or a treatment algorithm. A systematic analysis of the thrower’s exostosis has not been reported. To improve treatment of thrower’s exostosis, it is important to first identify the anatomic variants and clarify presentation and current treatment strategies.
The purpose of this study was to identify all types of reported thrower’s exostoses and categorize them into a classification system that will allow future treatment strategies to be compared and followed. We also sought to identify the success of return to throwing as reported in the literature after treatment for Bennett lesion. Our hypothesis was that lesions termed Bennett lesions have differing locations and presentations and have been treated by various strategies.
Methods
This systematic review and meta-analysis adhered to the principles outlined in the handbook of the Cochrane Collaboration15 and the established guidelines from PRISMA-DTA (Preferred Reporting Items for a Systematic Review and Meta-Analysis of Diagnostic Test Accuracy Studies).21
Search Strategy
We conducted an electronic literature search using PubMed/MEDLINE (1900-2019), Google Scholar (1900-2019), and the Cochrane Library (2019) using the following search strategy: “Bennett’s” OR “Bennett” OR “lesion” OR “glenoid exostosis”; “shoulder” was also included with search terms in repeated searches. The aforementioned controlled vocabulary was used when available, and reference tracking was performed to identify any potentially missed articles through the database search. Our inclusion criteria were studies published in a searchable database, prospective or retrospective series, studies of shoulder pathology, and studies that reported clinical outcome measures. Articles were excluded if they were editorials, descriptions of the Bennett fracture of the hand (fracture at the carpometacarpal joint), or articles written in languages other than English.
Study Selection and Data Extraction
Three reviewers (M.T.F., S.M., A.V.S.) independently performed the search. The reference lists of all selected publications were checked. Gray literature, systematic reviews, meta-analyses, and guidelines on shoulder clinical tests were searched to retrieve relevant publications not identified in the electronic search. Selection of relevant articles was performed first through titles and then through abstracts. Full-text articles were retrieved if the abstract provided insufficient information to establish eligibility or if the article passed the first eligibility screening. Disagreements among the reviewers were discussed and resolved by consensus.
Statistical Analysis
Patient demographics, lesion location, treatments (if reported), and outcomes were compiled. All findings were descriptive in nature. Results were tabulated in Microsoft Excel (Microsoft Corp), and descriptive statistics were completed.
Results
Systematic Review
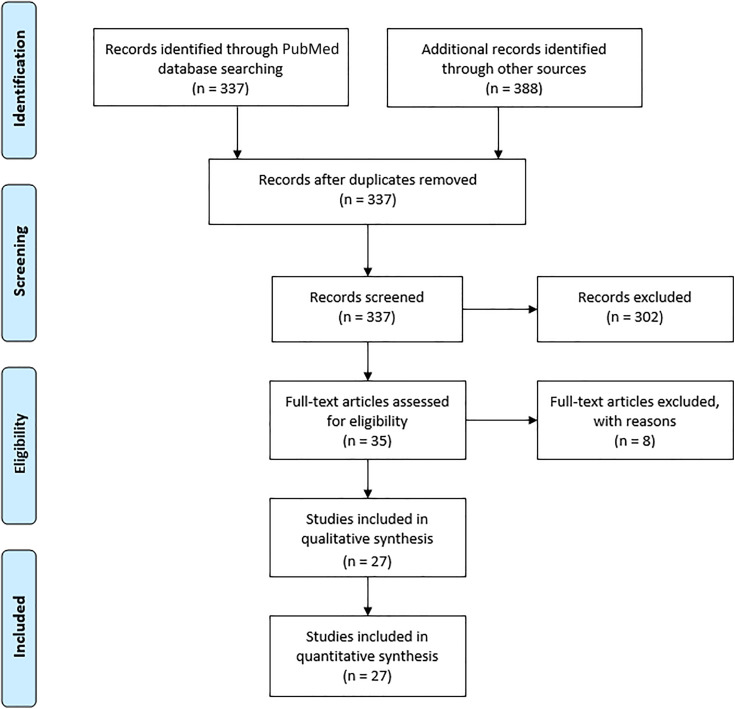
A total of 27 studies were included in the analysis (Figure 1). Of these 27 studies, 14 (52%) described orthopaedic treatment and outcomes of patients with a Bennett lesion (Table 1). The remaining 13 were radiographic or general diagnostic descriptions. In the orthopaedic treatment studies, 5 studies were level 3 evidence, and 9 studies were level 4 evidence. All of the early descriptions of Bennett lesion in general surgical or medical journals were level 5 evidence. The radiographic descriptions included 2 level 3 studies, 1 level 4 study, and 3 level 5 studies.
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) diagram for systematic review of Bennett lesions.
Table 1.
Overview of Thrower’s Exostosis Literaturea
| Lead Author (Year) | Article Title | Journal | LOE | Patients, n | Diagnostic (Tests and Views) | Type of Bennett Lesion | Treatment Recommendations |
|---|---|---|---|---|---|---|---|
| Orthopaedic Journals | |||||||
| Park (2016)29 | Bennett lesions in baseball players detected by magnetic resonance imaging: assessment of association factors | J Shoulder Elbow Surg | 3 | 388 | Physical examination and MRI | Excrescence bump at the posteroinferior aspect of the glenoid rim at insertion of the posterior joint capsule | Diagnostic and overview of pathophysiology; identified longer baseball career at time of MRI associated with greater prevalence of Bennett lesions |
| Levigne (2012)19 | Surgical technique: arthroscopic posterior glenoidplasty for posterosuperior glenoid impingement in throwing athletes | Clin Orthop Relat Res | 4 | 27 | Radiograph, CT arthrogram | Bony changes on posterior glenoid rim | Operative: arthroscopic resection of the bony prominence attributing to posterosuperior glenoid impingement |
| Nakagawa (2007)24 | Superior Bennett lesion: a bone fragment at the posterosuperior glenoid rim in 5 athletes | Arthroscopy | 4 | 5 | Radiograph (AP, axial, scapular Y, and 45° craniocaudal views), CT scan, arthroscopy | Bony spur at posterosuperior glenoid rim or classic posteroinferior glenoid rim | Diagnostic and overview of pathophysiology; nonoperative: relief with local anesthetic injection; operative: shoulder arthroscopy; all patients had torn posterosuperior labral tears and associated posterior capsular tightness; all Bennett fragments were excised arthroscopically with no labral or capsular repair |
| Nakagawa (2006)25 | Posterior shoulder pain in throwing athletes with a Bennett lesion: factors that influence throwing pain | J Shoulder Elbow Surg | 3 | 51 | Radiograph (AP, internal/external rotation, Bennett, and maximal elevation stress views), CT | Posteroinferior bony spur on inferior border of glenoid | Diagnostic and overview of pathophysiology; operative: resection of painful avulsed Bennett fragment, resection recommended (repair of posterior capsule or labrum) |
| Yoneda (2006)36 | Arthroscopic capsular release for painful throwing shoulder with posterior capsular tightness | Arthroscopy | 4 | 16 | Not specifically described | Bony spur on the posteroinferior glenoid rim that causes throwing pain | Operative: arthroscopic resection of exostosis with no capsular or labral repair |
| Andrews (2004)1 | The thrower’s exostosis pathophysiology and management | Tech Shoulder Elbow Surg | 5 | 22 | Radiograph (AP shoulder with internal/external rotation, West Point axillary, Stryker notch, and Bennett views), CT scan, MRI | Osteophyte found on posteroinferior rim of glenoid | Nonoperative: addressing mechanical flaw in throwing motion, adequate rest, increasing flexibility with progressive stabilization focusing on dynamic stability and neuromuscular control; operative: arthroscopic removal of Bennett lesion, no capsular or labral repair |
| Wright (2004)34 | Prevalence of the Bennett lesion of the shoulder in major league pitchers | Am J Sports Med | 3 | 55 | Radiograph (AP, axillary, modified Bennett views) | Mineralization of posteroinferior glenoid | Nonoperative |
| Connor (2003)9 | Magnetic resonance imaging of the asymptomatic shoulder of overhead athletes: a 5-year follow-up study | Am J Sports Med | 3 | 20 | MRI | Not specifically described | Diagnostic and overview of pathophysiology |
| Bowen (2002)7 | Shoulder injury—football | Med Sci Sports Exerc | 4 | 1 | Radiograph (complete shoulder views), CT scan, MRI arthrogram | Extra-articular posterior ossification involving posterior glenoid and posterior labral injury | Operative: surgical treatment addressing posterior instability/labral stabilization without specific mention of Bennett lesion being addressed or debrided |
| Yoneda (2002)35 | Arthroscopic removal of symptomatic Bennett lesions in the shoulders of baseball players: arthroscopic Bennett-plasty | Am J Sports Med | 4 | 16 | Radiograph, CT scan | Radiographic criteria: bony spur at posterior glenoid rim; clinical criteria: posterior shoulder pain during throwing (especially follow-through), tenderness at posteroinferior glenohumeral joint, and reduced throwing pain with lidocaine injection into Bennett lesion | Operative: all-arthroscopic “Bennett-plasty” lesion excision: resection alone, resection and capsular repair, or resection and labral reattachment |
| Pearce (2000)30 | The pitcher’s mound: a late sequela of posterior type II SLAP lesions | Arthroscopy | 4 | 3 | Radiograph, MRI | Posterosuperior glenoid osteophyte | Diagnostic and overview of pathophysiology; operative: Bennett lesion was never addressed; SLAP repaired occasionally |
| Meister (1999)22 | Symptomatic thrower’s exostosis: arthroscopic evaluation and treatment | Am J Sports Med | 3 | 22 | Radiograph (AP, internal/external rotation, West Point axillary, and Stryker notch views), CT, MRI | Posterior glenoid osteophyte | Operative: arthroscopic rotator cuff debridement and labral debridement for patients with pain during late cocking, acceleration, or follow-through |
| Ferrari (1994)12 | Posterior ossification of the shoulder: the Bennett lesion, Etiology, diagnosis, and treatment | Am J Sports Med | 4 | 7 | Radiograph (standard, Bennett, and Stryker notch views), CT arthrogram, MRI | Crescent mineralization emanating from posteroinferior glenoid, extra-articular posterior ossification | Operative: arthroscopic debridement of posterior labrum and rotator cuff if affected in all; no repairs of labrum or capsule or Bennett lesion in any case |
| Ozaki (1992)28 | Surgical treatment for posterior ossifications of the glenoid in baseball players | J Shoulder Elbow Surg | 4 | 7 | Radiograph; radiographic shoulder arthrogram | Ossification on infraglenoid tubercle or posteroinferior glenoid rim | Diagnostic and overview of pathophysiology; operative: open surgical resection of Bennett lesion and axillary neurolysis |
| Walch (1992)33 | Impingement of the deep surface of the supraspinatus tendon on the posterosuperior glenoid rim: an arthroscopic study | J Shoulder Elbow Surg | 4 | 17 | Radiograph (AP, internal/external rotation, lateral glenoid views), radiographic arthrogram, CT arthrogram, MRI, ultrasonography | Osteophyte on the posterior border of the glenoid fossa | Diagnostic and overview of pathophysiology |
| Barnes (1978)2 | An analysis of 100 symptomatic baseball players | Am J Sports Med | 3 | 8 | Radiograph (AP, internal/external rotation, axillary, AP glenoid, Bennett views), radiographic arthrogram | Glenoid exostosis in posteroinferior position | Nonoperative with rehabilitation; operative: open excision of Bennett lesion |
| Lombardo (1977)20 | Posterior shoulder lesions in throwing athletes | Am J Sports Med | 4 | 4 | Radiograph | Ossification on the posteroinferior glenoid area | Operative: open posterior approach: Bennett lesion open resection, with capsule reapproximated or no capsular work or capsule reattached to posterior glenoid or resection of posterior adhesions and capsule |
| Radiology Journals | |||||||
| Karcich (2019)17 | Bennett lesions in overhead athletes and associated shoulder abnormalities on MRI | Skeletal Radiol | 3 | 70 | MRI | Posteroinferior glenoid exostosis | Comparison of concurrent shoulder pathology identified on MRI in overhead athletes with and without Bennett lesions |
| Del Grande (2016)11 | High-resolution 3-T magnetic resonance imaging of the shoulder in nonsymptomatic professional baseball pitcher draft picks | J Comput Assist Tomogr | 4 | 19 | 3.0-T MRI | Crescent-shaped ossification at the posteroinferior glenoid | Diagnostic and overview of pathophysiology; examined frequency of Bennett lesion and other shoulder abnormalities in asymptomatic professional pitching draft picks |
| Cohn (2012)8 | The throwing shoulder: the orthopedist perspective | Magn Reson Imaging Clin N Am | 5 | 0 | Radiograph (Stryker notch view), CT arthrography, MRI | Extra-articular calcification of posteroinferior glenoid | Diagnostic and overview of pathophysiology; nonoperative: rest, NSAIDs, and PT to increase strength; operative: can debride Bennett lesion but should also address labrum and partial cuff tear; use caution to address not only the Bennett lesion but also other shoulder pathology |
| Bennett (2005)3 | Update of imaging of sports injuries to the upper extremity: shoulder and elbow | Imaging Decisions MRI | 5 | 0 | Radiograph (Stryker notch view), CT scan | Ossification of posteroinferior aspect of glenohumeral joint capsule, traction spur where glenohumeral joint capsule attaches to the glenoid | Diagnostic and overview of pathophysiology |
| Fujisawa (2002)13 | Diagnostic imaging for sports injuries of the shoulder and upper arm in baseball pitchers | Radiologist | 5 | 0 | Radiograph (Bennett view), CT arthrography, MRI arthrography | Crescent-shaped mineralization on posteroinferior aspect of the glenoid | Diagnostic and overview of pathophysiology; nonoperative: PT; operative: address associated posterior labral tear, rotator cuff tears, and Bennett lesion as contributions to dysfunction, fixation, and/or debridement of lesions |
| De Maeseneer (1998)10 | The Bennett lesion of the shoulder | J Comput Assist Tomogr | 3 | 3 | Radiograph (standard and Bennett views), CT, MRI | Crescent-shaped region of mineralization at the posteroinferior aspect of the glenoid rim | Diagnostic and overview of pathophysiology |
| General Surgical or Medical Journals | |||||||
| Nobuhara (2005)26 | Clinical approaches for shoulder injuries in sports | Japan Med Assoc J | 5 | 0 | Radiograph, CT, MRI | Osteophyte or bony spur on glenoid on posterior portion of joint capsule | Diagnostic and overview of pathophysiology; nonoperative: nonoperative treatment with rest for bone spur caused by triceps tendon pull on capsule and implicated brachial circumflex nerve causing pain to deltoid; operative: surgical management of associated shoulder instability |
| Bennett (1959)6 | Elbow and shoulder lesions of baseball players | Am J Surg | 5 | 0 | Radiograph (Bennett view) | Deposit of bone on posteroinferior border of glenoid fossa similar to osteoarthritis deposit | Diagnostic and overview of pathophysiology; nonoperative: recommended nonoperative treatment secondary to the previous poor results with the open resection |
| Bennett (1947)5 | Shoulder and elbow lesions distinctive of baseball players | Ann Surg | 5 | 0 | Radiograph (Bennett view of external rotation of humerus with tilt of x-ray tube 5° off the perpendicular axis of the shoulder) | Deposit on posteroinferior margin of glenoid fossa on or about attachment of the triceps tendon | Diagnostic and overview of pathophysiology; nonoperative: expert opinion that Bennett lesion does not respond well to surgery and only causes discomfort during throwing and not during activities of daily living |
| Bennett (1941)4 | Shoulder and elbow lesions of the professional baseball pitcher | JAMA | 5 | 0 | Radiograph (Bennett view) | Deposit of bone on posteroinferior border of the glenoid fossa “strikingly similar to osteoarthritic deposit” | Diagnostic and overview of pathophysiology; operative: open removal of the exostosis |
aAP, anteroposterior; CT, computed tomography; LOE, level of evidence; MRI, magnetic resonance imaging; NSAID, nonsteroidal anti-inflammatory drug; PT, physical therapy; SLAP, superior labrum anterior and posterior.
Location
Bennett4 first described a “posteroinferior bone deposit on or about the triceps resulting from an abnormal strain on the tendon.” Similar descriptions of posteroinferior exostoses were reported by Lombardo et al20 and Meister et al.22 The exostosis has since been reported to be both subperiosteal attached to the glenoid and a free bony fragment.2,25 Subperiosteal lesions have similarly been reported at the long head of the muscle origin.4,28
Exostoses occurring in the region of the posterior or posterosuperior glenoid rim were described by Walch et al.33 These lesions differ from a conventional Bennett lesion in location and in that they can be a free or attached ossification occurring in the region of the posterosuperior glenoid rim (Table 1). Nakagawa et al24 reported on the fragmented variety. Posterosuperior exostoses are morphologically similar to the “pitcher’s mound” osteophyte described by Pearce and Burkhart30 at the posterosuperior glenoid rim associated with type II superior labrum anterior and posterior tears.
Etiological Factors
The original calcified lesion described by Bennett4 was believed to be attributed to a traction injury from the long head of the triceps during the follow-through phase of pitching. The traction phenomenon theory proposes a secondary reaction to repetitive microtrauma with tearing of the posterior capsule off of its glenoid insertion and subsequent reactive calcification.10,20,23 The location of the lesion is the region of attachment on the posterior band of the inferior glenohumeral ligament.27 Of the 23 (85%) articles found on Bennett lesions, 15 articles1-6,8,10,12,13,20,24,25,28,36 described the lesion in this posteroinferior position (Table 1). Debatably, the repetitive stresses of throwing potentially serve as the stimulus for the reactive changes in the posterior capsule. Histological analysis confirmed reactive bone formation after excision.20
For posterosuperior exostoses, other theories have been proposed.4,5 These include posterior impingement of the humeral head and posterior capsule on the glenoid rim during late cocking,12,18,28,33 traction of the posterior capsule at the glenoid interface during follow-through,16,20,23 and the wringing action of the capsule that occurs throughout the phases of throwing.28 All the proposed mechanisms could potentially be responsible for the variety of lesions along the posterior glenoid (Table 1).
Associated Pathologies
Thrower’s exostoses are associated with intra-articular pathology, especially posterior labral injury and undersurface rotator cuff tears.16,22 Meister et al22 reported 95% (21/22) undersurface cuff tears and 68% (15/22) posterior labral pathology in throwers with Bennett lesions. These associated lesions may be secondary to posterosuperior impingement, with exostosis being a reactive formation on the posterior glenoid.
History and Physical Examination
Posterior shoulder pain is the primary concern of throwers with a posteriorly located exostosis.4,20,28 Affected throwers are often asymptomatic at rest or when throwing at a moderate speed; however, increases in throwing velocity are associated with increases in pain.5,20,22,28 A specific inciting event has been reported, but this association is limited in the literature.4 The lack of association with an inciting event is supported, as this pathology has a more recently reported prevalence of 22% in 55 asymptomatic major league pitchers.34
The painful phase of throwing may help distinguish a potential lesion of the more traditional inferior location in contrast to the superior region. Certain throwers may report pain throughout the throwing cycle, which confounds the history.22,28 Pain during the follow-through phase is associated with the classic Bennett lesion,4,25 whereas pain with late cocking and early acceleration is found with posterosuperior exostosis.24 Walch et al33 described the pathological contact of the posterosuperior glenoid (labrum) and the articular-sided rotator cuff and greater tuberosity during late cocking, known as internal impingement, which may accentuate the pain of a posterosuperior lesion. Additionally, the presence of a posteroinferior subperiosteal lesion could cause a deficit of internal rotation and worsening of posterosuperior humeral head migration with throwing.14 The occurrence of both painful and asymptomatic thrower’s exostosis increases significantly with advanced age and duration of pain.12 This pain may be secondary to posterosuperior impingement of the humeral head and posterior capsule abutting against the glenoid rim in the case of a more superior-based lesion. These physical examination findings were present in all patients undergoing operative treatment for a posterosuperior lesion in throwing athletes as reported by Levigne et al.19
The range of motion limitations vary with thrower’s exostosis. In a cohort of 5 patients who had superior Bennett lesions (all of which were isolated bony fragments), Nakagawa et al24 reported a glenohumeral internal rotation deficit (GIRD) measuring a mean of 35°. Of these 5 patients, 3 patients also presented with a classic Bennett lesion in addition to the superior lesions, which may have contributed to decreased internal rotation. Meister et al23 found gains in external rotation and loss of internal rotation for all 22 athletes in their series. Nakagawa et al25 reported a GIRD of only 10° in 31% of the group who had a painful classic Bennett lesion and in 73% of asymptomatic patients who had a classic Bennett lesion. Full symmetric motion was observed in the 3 patients with pitcher’s mound lesions reported by Pearce and Burkhart.30 Athletes with symptomatic Bennett lesions also demonstrated substantial posterior laxity.30 Nakagawa et al25 reported that patients with painful avulsion or a free fragment Bennett lesion were more likely to have posterior joint laxity. Meister et al22 reported that 68% (15/22) of throwers with Bennett lesions had posterior labral pathology and posited that this could explain the posterior laxity. Nakagawa et al24 reported a positive O’Brien test and posterior pain elucidated with forced external rotation at 90° of abduction in all 5 patients with a posterosuperior exostosis.
Radiographic Imaging and Diagnosis
A thrower’s exostosis may be a subtle finding on plain film radiography and may depend on the lesion location. Views commonly used include true anteroposterior, Grashey, Stryker notch, axillary, and Neer (outlet) shoulder views (Tables 1 and 2, Figure 2). Bennett’s4 technique placed the radiographic beam 5° cephalad with the arm in 90° of abduction and 90° of external rotation. Wright and Paletta’s34 modified Bennett view with the beam angled 5° cephalad and the arm in 45° of abduction provided a successful alternative imaging technique. Nakagawa et al25 described an anteroposterior view with the shoulder in maximum elevation to provide additional radiographic information. Yoneda et al35 described criteria for diagnosing a painful Bennett lesion, which included radiographic detection of the spurring or lesion on the posterior rim of the glenoid in the presence of posterior shoulder pain with throwing, and tenderness to palpation at the posteroinferior aspect of the glenohumeral joint. The authors recommended that the radiographic lesion be confirmed as symptomatic by injection of xylocaine around the lesion.25 The injection was performed under fluoroscopic guidance with a 2- to 3-mL injection of local anesthetic (ie, xylocaine) to the lesion. If pain was decreased by more than 50% or throwing ability was improved, the outcome of the test was considered positive.35 Ultrasonography can additionally be used to facilitate a diagnosis of associated rotator cuff or labral lesions.31
Table 2.
Types of Thrower’s Exostosisa
| Lead Author (Year) | Pts, n | Pts With Exostosis, n | Pts With Symptomatic Exostosis, n | Op Lesions | Type 1A | Type 1B | Type 2A | Type 2B | Type 3A | Type 3B | Unknown | 1A Op | 1B Op | 2A Op | 2B Op | 3A Op | 3B Op |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Levigne (2012)19 | 27 | 27 | 27 | 27 | 0 | 0 | 0 | 0 | 27 | 0 | 0 | 0 | 0 | 0 | 0 | 27 | 0 |
| Nakagawa (2007)24 | 5 | 5 | 5 | 5 | 0 | 0 | 0 | 0 | 0 | 5 | 0 | 0 | 0 | 0 | 0 | 0 | 5 |
| Nakagawa (2006)25 | 51 | 24 | 13 | 13 | 20 | 4 | 0 | 0 | 0 | 0 | 0 | 9 | 4 | 0 | 0 | 0 | 0 |
| Yoneda (2006)36 | 16 | 8 | 8 | 8 | 8 | 0 | 0 | 0 | 0 | 0 | 0 | 8 | 0 | 0 | 0 | 0 | 0 |
| Wright (2004)34 | 55 | 12 | 0 | 0 | 12 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Connor (2003)9 | 20 | 5 | 0 | 0 | 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Yoneda (2002)35 | 16 | 16 | 16 | 16 | 11 | 5 | 0 | 0 | 0 | 0 | 0 | 11 | 5 | 0 | 0 | 0 | 0 |
| Pearce (2000)30 | 3 | 3 | 3 | 3 | 0 | 0 | 1 | 0 | 2 | 0 | 0 | 0 | 0 | 1 | 0 | 2 | 0 |
| Meister (1999)22 | 22 | 22 | 11 | 11 | 22 | 0 | 0 | 0 | 0 | 0 | 0 | 11 | 0 | 0 | 0 | 0 | 0 |
| Ferrari (1994)12 | 7 | 7 | 7 | 7 | 7 | 0 | 0 | 0 | 0 | 0 | 0 | 7 | 0 | 0 | 0 | 0 | 0 |
| Ozaki (1992)28 | 7 | 7 | 7 | 5 | 5 | 0 | 0 | 0 | 0 | 0 | 2 | 5 | 0 | 0 | 0 | 0 | 0 |
| Walch (1992)33 | 17 | 11 | 11 | 0 | 0 | 0 | 1 | 0 | 10 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Barnes (1978)2 | 56 | 8 | 8 | 8 | 8 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 |
| Lombardo (1977)20 | 4 | 3 | 3 | 3 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 |
| Total | 306 | 158 | 119 | 106 | 101 | 9 | 2 | 0 | 39 | 5 | 2 | 56 | 9 | 1 | 0 | 29 | 5 |
aOp, operatively treated; Pts, patients.
Figure 2.
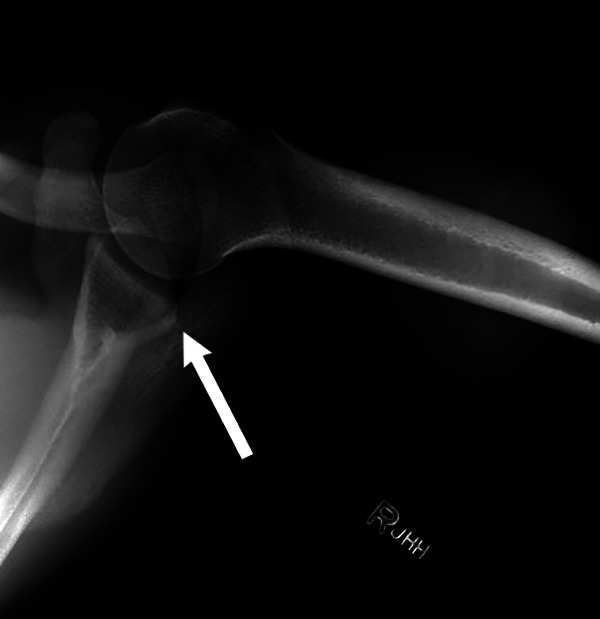
Axillary radiograph revealing a region of hyperdensity in the posteroinferior soft tissues. Arrow: posteroinferior density of Bennett lesion that is subperiosteal and free.
Current techniques for further evaluating a thrower’s exostosis and concomitant shoulder pathology rely on computed tomography (CT) and magnetic resonance imaging (MRI) with or without arthrography (Tables 1 and 2, Figures 3 and 4). These studies have demonstrated a calcification adjacent to the posterior glenoid or in the adjacent capsular tissues.10,16 CT imaging can be used to determine the size and type (spurring or free fragment) of the lesion (Figures 3 and 4). The largest spur or fragment is identified, measured, and compared with the width of the glenoid fossa. The lesion is considered small if less than 10% of the glenoid fossa width, medium if 10% to 20%, and large if greater than 20%.25
Figure 3.
Computed tomography (CT) arthrogram of a throwing athlete demonstrating a posteroinferior glenoid exostosis. (A) Axial CT arthrogram demonstrating the lesion (arrow). (B) Sagittal CT arthrogram demonstrating the posteroinferior extent of the exostosis. (Images courtesy of Michael T. Freehill.) A, anterior; P, posterior; H, head; F, foot.
Figure 4.

Sagittal reconstructed computed tomography image demonstrating Bennett lesion in the left shoulder. Arrow: Bennett lesion. C, clavicle; G, glenoid; SS, scapular spine.
MRI demonstrates a Bennett lesion as a region of very low signal adjacent to the posterior glenoid.9 MRI with or without arthrography offers the advantage of enabling better evaluation of nonosseous structures and associated periarticular shoulder pathology; however, a small bony lesion may be interpreted as labrum in this region (Tables 1 and 2).9
Aggregate radiographic data demonstrated 158 of 306 patients (52%) with a thrower’s exostosis of any type and location (Table 2, Appendix Table A1). Of these 158 patients with a radiographic lesion, 119 (75%) patients were symptomatic. The locations were posteroinferior in 110 patients (70%), directly posterior in 2 patients (1.3%), posterosuperior in 44 patients (28%), and unknown in 2 patients (1.3%). Avulsed lesions were present in 9 (5.7%) posteroinferior lesions, zero direct posterior lesions, and 2 (1.3%) posterosuperior lesions. When examining the reported lesion location, we categorized them into 3 types based on anatomic location (shown in Figure 5): posteroinferior (type 1), posterior (type 2), and posterosuperior (type 3). These types were subclassified by the stability of the exostosis: stable/intact (type A) or unstable/detached (type B).
Figure 5.
Classification of glenoid thrower’s exostosis. Location and descriptions of the types of thrower’s exostosis. Type 1, classic Bennett lesion; type 2, posterior exostosis; type 3, posterosuperior exostosis. The “A” modifier represents a stable lesion (attached), whereas “B” indicates an unstable lesion (fragment).
Treatment
The most effective treatment of a thrower’s exostosis is unknown (Tables 1 and 2). Determining a course of action is further complicated by reviewing the results of classic type 1 lesions versus type 2 and 3 lesions and free fragments versus spurring or osteophytic attached lesions. In the earliest accounts, Bennett originally supported surgical resection of the lesion if necessary, but after poor surgical outcomes, he later recommended nonoperative management.4–6 Current treatment recommendations are initial nonoperative management with stretching of the posterior capsule and strengthening of the rotator cuff. Wright and Paletta34 recommended nonsurgical management, and none of the pitchers they studied required surgical intervention for the lesion during their time with the respective baseball organization. Of 12 pitchers studied by Wright and Paletta, 2 pitchers (17%) required time on the disabled list; however, neither individual had symptoms or concerns of posterior shoulder pain.
Surgery was performed on 84% (100/119) of the symptomatic lesions. Of the reported postoperative return to play, 29 of 47 (62%) patients returned to preinjury performance levels.
Early attempts at surgical intervention consisted of open excision of the lesion.4,20,28 Lombardo et al20 reported their results on 3 professional pitchers after open excision with a rongeur and capsular approximation or repair to the glenoid. All ossifications were in the posteroinferior position, but the authors did not report whether the exostosis was still attached or free from the glenoid. In this limited cohort, all 3 pitchers returned to their preinjury level of professional baseball; however, the duration of this return was not disclosed. In contrast, Barnes and Tullos2 openly excised a posteroinferior exostosis in 2 pitchers, and neither returned to throwing. Ozaki et al28 described performing an open excision of an attached posteroinferior ossification as well as addressing a torn posterior labrum without repair. All 7 pitchers returned to “satisfactory” levels of competition. Ozaki et al concluded that their outcomes may have been superior to those in other open excision reports because the approach was performed by splitting the posterior deltoid in line with its fibers and preserving the deltoid on the scapular spine.2,4
Current literature supports arthroscopic intervention after failure of nonoperative management and inability to return to competitive throwing. The best arthroscopic management of the thrower’s exostosis is still unclear. Some authors have proposed addressing exclusively the intra-articular pathology and intentionally not addressing the Bennett lesion proper,32 whereas others have advocated for simple arthroscopic removal of the symptomatic, isolated Bennett lesions.12,35 Glenoidplasty can result in complete relief of symptoms35 and improve the likelihood of resuming a former sport level.21,35
Ferrari et al,12 who studied 7 pitchers (6 professional, 1 collegiate), concluded that Bennett lesions are extra-articular ossifications at the posteroinferior glenoid. The authors reported that these lesions were associated with posterior labral tears, undersurface rotator cuff tears, and possible posterior subluxation, and they recommended debridement of the intra-articular pathology alone. Only 1 of the 6 posterior labral tears in this study was stated to be detached, which suggests that the other 5 may have been principal fraying of the labrum not requiring repair. Of the 7 pitchers, 6 pitchers (86%) returned to their previous baseball level or a higher level. A difference in the pathology was that ossification was not identified in any patient at the time of arthroscopy and lesion size was not reported from imaging. The authors concluded that the bone formation was not the principal factor in the pain but rather a marker for associated pathology in the shoulder.12 Warren, in his commentary of the article, noted that if posterior labral injury is present with posterior humeral head subluxation, the capsule/labrum should be repaired.12
Yoneda et al35 developed a protocol of 3 months of nonoperative management and recommended arthroscopy if symptoms persisted. The authors described arthroscopically excising symptomatic Bennett lesions in 16 baseball players. Although 11 of the 16 players (69%) returned to their preinjury level of competition at a minimum of 1 year, only 1 participant was a professional baseball player, and half of the cohort were recreational players. Meister et al22 reported debridement of only the associated pathology and only attached exostosis lesions in the posteroinferior position in 22 throwing athletes. The exostosis was addressed only when readily identified and accessible through a small incision off the posteroinferior glenoid rim with a bur (50%). The investigators noted a trend toward a poor result when the exostosis was larger than 100 mm2; however, the outcome did not differ between debridement versus no intervention for the exostosis. Of the 22 participants, 11 (50%) had a successful outcome of return to preinjury level of competition for at least 1 year.
Nakagawa et al24 reported on 5 patients with detachment of the posterosuperior labrum and associated exostotic lesions. Arthroscopic excision took place in all patients, revealing mobile and unstable bone fragments. At a minimum 2-year follow-up, all athletes returned to their preinjury performance level. No mention was made of repair of the labrum or capsule. Levigne et al19 also reported on the posterosuperior lesion in throwing athletes. All 27 patients with symptomatic posterosuperior lesions were treated with arthroscopic resection of the bony prominence attributed to posterosuperior glenoid impingement.
For stable posteroinferior lesions (type 1A), 56 of 101 lesions (55%) required operative intervention. For the unstable type IB lesions, 9 of 9 (100%) were managed surgically. Only two type 2 lesions were reported; both were stable, but 1 lesion (50%) was managed operatively. Type 3A lesions were treated surgically in 29 of 39 cases (74%), and 5 of 5 type 3B lesions (100%) underwent surgical management. The small sample size precludes further analysis.
Discussion
Our systematic review of the literature demonstrates that many glenoid exostoses are referred to as “Bennett lesions”; however, the natural history and treatment of these lesions are unclear. The principle finding of our study was that there are 3 anatomic lesions that can be classified under thrower’s exostoses as reported in the literature to date. Our analysis of the reported methods identified the classic posteroinferior Bennett lesion, the direct posterior exostosis, and the posterosuperior exostosis. All reported exostoses fit these 3 types in our proposed classification system. To better understand the reported location and the associated treatments, we subdivided each type as stable (type A) or unstable/detached (type B). The subcategory was defined to better track future treatment strategies.
The majority of the symptomatic exostoses were treated surgically; however, the strategies differed regarding the location and the stability. Classically defined Bennett lesions were treated surgically more commonly if they were unstable. The literature supports that exostoses that remain attached are more often not painful but may be related to decreased range of motion. When the exostoses become detached, the lesion becomes painful, while range of motion improves. These findings support the development of a classification that differentiates between stable (attached) and unstable (detached) lesions to help determine operative treatment. Because pain is an operative indication for the Bennett lesion but loss of range of motion is not, this subclassification of lesions as attached versus free is helpful.24,35
Although the Bennett lesion is classically defined as an inferior glenoid lesion, the direct posterior and superior lesions are reported in overhead athletes, and we classified these lesions based on the anatomic location. An improved organization of the lesion location can be used to identify underlying pathobiology or pathomechanics and resolve past discrepancies. One such discrepancy is the so-called pitcher’s mound lesion, which is reported in the posterosuperior region, but this is arguably a misnomer because all patients and baseball players described were older than 51 years.1 The posterosuperior exostosis that was reported by Levigne et al19 was determined to be the source of pain through an impingement mechanism. Although these lesions were stable, the location was thought to be the primary source of shoulder pain with posterosuperior glenoid impingement. These lesions, unlike the classic Bennett posteroinferior lesions, were surgically treated more commonly despite being attached.
Although investigators have observed that lesions appear larger when painful, the size and necessity for removal have not been documented. No statistical differences between small and large and between painful and nonpainful Bennett lesions have been reported.25 Identifying which lesions are painful and which lesions are not helps guide surgical treatment versus additional physical therapy and stretching for posterior capsular tightness. Improved classification and its association with pain may also help to guide treatment if the lesions are present with concomitant pathology so that additional surgical dissection is not performed unnecessarily.
Our study carries several limitations. The first and most important limitation is the available literature for review. The reports on Bennett lesions in the English-language literature over the past 80 years provide few clinical and outcome data, and the quality of the studies is generally low. Our study highlights the need for more complete data collection and especially the need for prospective data. The reported treatment strategies did not offer reliable outcome reporting—if the outcomes were reported at all. The goal of this study was not to analyze treatment efficacy but to establish the anatomic lesions and report aggregate strategies to treat them. The data are far too limited to discern the superiority of any individual treatment strategy. Future studies may examine cohorts of pitchers with asymptomatic Bennett lesions to identify when the lesions become pathological. An additional limitation of our study is the small sample size secondary to the available literature for review. Although the lesion is reported to be common in overhead athletes, the population as a whole is relatively small. Future sample sizes may be increased with prospective cohort studies that can better define the natural history of the disease.
Conclusion
Based on a comprehensive review of the literature, we identified several anatomic locations for a thrower’s exostosis beyond the classic Bennett lesion. We categorized the reported exostoses into a new classification system for description of location and type (subperiosteal or free fragment) of the thrower’s exostosis, which may be used to study future treatments. Current treatment strategies recommend that surgical treatment of thrower’s exostosis is considered only after all nonoperative management strategies have been attempted because reported return to sport is variable after surgery. The effectiveness of excision or repair for both subperiosteal and detached lesions has not been established.
APPENDIX
Table A1.
Operative Treatment of Thrower’s Exostosisa
| Lead Author (Year) | LOE | Patients, n | Operative Treatment of Bennett Lesion | Additional Surgical Treatments | Operative Results |
|---|---|---|---|---|---|
| Cohn (2012)8 | 5 | 0 | Excision (did not specify open vs arthroscopic) | Recommended addressing labrum and rotator cuff (eg, other shoulder pathology) | None described |
| Levigne (2012)19 | 4 | 27 | Arthroscopic excision | None | Of 26 patients available for final follow-up, 18 patients returned to their former level of sport; 2 patients did not improve |
| Nakagawa (2007)24 | 4 | 5 | Arthroscopic excision | Shoulder arthroscopy, no labral or capsular repair | Bennett lesion and associated symptoms in 5 athletes (3 baseball, 1 volleyball, 1 quarterback), who returned to their preinjury sports activity at the same performance level |
| Nakagawa (2006)25 | 3 | 51 | Arthroscopic excision | Repair of posterior capsule and labrum | None described |
| Yoneda (2006)36 | 4 | 16 | Arthroscopic excision | No capsular or labral repair, posterior capsular release | No results specific to Bennett group, but 1 patient who had Bennett excision with posterior capsule release had an aggravation of anterior shoulder instability and was dissatisfied |
| Nobuhara (2005)26 | 5 | 0 | Not addressed | Surgical management of shoulder instability | None described |
| Bowen (2002)7 | 4 | 1 | Not addressed | Addressed posterior instability/labral stabilization | None described |
| Fujisawa (2002)13 | 5 | 0 | Fixation vs debridement of lesion (did not specify open vs arthroscopic) | Addressed associated posterior labral tear, rotator cuff tear | None described |
| Yoneda (2002)35 | 4 | 16 | Arthroscopic excision | Associated capsular repair or labral repair | All-arthroscopic “Bennett-plasty” lesion excision; resection alone in 2 of the 16 patients, resection and capsular repair in 10 patients, and resection and labral reattachment in 4 patients; pain disappeared with throwing in 10 patients, and pain was mitigated in 6 patients; 11 patients returned to baseball at their previous level of competition |
| Pearce (2000)30 | 4 | 3 | Not addressed | Occasional SLAP repair | The authors hypothesized that an unstable posterosuperior labrum results in posterior superior glenoid osteophyte formation; they termed this lesion a “pitcher’s mound”; the case series documented middle-aged patients in whom the osteophyte may stabilize the detached torn labrum by filling the torn space; thus, the authors concluded that the SLAP tear does not have to be repaired; the lesion was never addressed; SLAP was repaired in 1 patient; patients were able to return to recreational and work activities |
| Meister (1999)22 | 3 | 22 | Not addressed | Arthroscopic rotator cuff debridement and labral debridement | Arthroscopic rotator cuff debridement (21/22 patients) and posterior labral debridement (15/22) with no repair of capsule, labrum, or rotator cuff; posterior osteophyte resection (11/22); mean follow-up was 6.3 y, and 55% of patients returned to premorbid throwing level; the authors did not analyze return of patients who had Bennett osteophyte resection vs those who did not |
| Ferrari (1994)12 | 4 | 7 | Not addressed | Arthroscopic debridement of labrum and rotator cuff | Case series following 7 elite baseball players (3 major league, 3 minor league, 1 college); 6 patients had posterior labral tears; 5 patients had posterosuperior position labral tears; 1 posterior labrum was completely detached; 4 patients had rotator cuff fibrillation; Bennett lesion was not seen during any arthroscopy; 6 patients returned to baseball at the same level or higher; 1 patient did not return to baseball |
| Ozaki (1992)28 | 4 | 7 | Open excision | Axillary neurolysis (open) | Mean 5-y follow-up (range, 3-9.2 y) of 7 symptomatic baseball players who had posterior Bennett lesions, after open surgical resection of the osteophyte and axillary neurolysis; improved postoperative pain, sensation, muscle strength, and throwing distance; return to satisfactory competitive levels |
| Barnes (1978)2 | 3 | 8 | Open excision | None | 100 consecutive baseball players were reviewed over a 10-y period; 8 of those players had symptomatic Bennett lesion, and 2 of those 8 players underwent open excision of exostosis and the labrum; neither pitcher returned to throwing |
| Lombardo (1977)20 | 4 | 4 | Open excision | Open capsule reapproximation, no capsular work, capsule reattached to posterior glenoid, or resection of posterior adhesions and capsule | Case series of 4 baseball players; 3 players had posteroinferior Bennett lesion; 1 player had adhesions of the posterior glenoid; all players returned to throwing, and all had satisfactory competitive levels |
| Bennett (1941)4 | 5 | 0 | Open excision | None | None described |
aLOE, level of evidence; SLAP, superior labrum anterior and posterior.
Footnotes
Final revision submitted January 13, 2020; accepted February 26, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: M.T.F. has received grant support from DJO, consulting fees from DePuy/Medical Device Business Services and Smith & Nephew, speaking fees from Integra and Smith & Nephew, and hospitality payments from Wright Medical. S.M. has received educational support from Arthrex, DJO, and Smith & Nephew. L.D.H. has received educational support from Arthrex and Kairos Surgical, consulting fees from Arthrex, and hospitality payments from Arthrex and Ethicon. A.V.S. has received institutional and fellowship educational grants from Arthrex, Medwest, and Smith & Nephew; consulting fees from Allosource; and hospitality payments from Stryker and Wright Medical. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Andrews JR, Dugas JR, Hackel JG, Reinold MM, Wilk KE. The thrower’s exostosis pathophysiology and management. Tech Shoulder Elbow Surg. 2004;5(1):44–50. [Google Scholar]
- 2. Barnes DA, Tullos HS. An analysis of 100 symptomatic baseball players. Am J Sports Med. 1978;6(2):62–67. [DOI] [PubMed] [Google Scholar]
- 3. Bennett DL, El-Khoury GY. Update of imaging of sports injuries to the upper extremity: shoulder and elbow. Imaging Decisions MRI. 2005;9(3):32–38. [Google Scholar]
- 4. Bennett GE. Shoulder and elbow lesions of the professional baseball pitcher. JAMA. 1941;117:510–514. [Google Scholar]
- 5. Bennett GE. Shoulder and elbow lesions distinctive of baseball players. Ann Surg. 1947;126(1):107–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bennett GE. Elbow and shoulder lesions of baseball players. Am J Surg. 1959;98:484–492. [DOI] [PubMed] [Google Scholar]
- 7. Bowen JD, Bonner KF. Shoulder injury—football. Med Sci Sports Exerc. 2002;34(5):S211. [Google Scholar]
- 8. Cohn RM, Jazrawi LM. The throwing shoulder: the orthopedist perspective. Magn Reson Imaging Clin N Am. 2012;20(2):261–275. [DOI] [PubMed] [Google Scholar]
- 9. Connor PM, Banks DM, Tyson AB, Coumas JS, D’Alessandro DF. Magnetic resonance imaging of the asymptomatic shoulder of overhead athletes: a 5-year follow-up study. Am J Sports Med. 2003;31(5):724–727. [DOI] [PubMed] [Google Scholar]
- 10. De Maeseneer M, Jaovisidha S, Jacobson JA, et al. The Bennett lesion of the shoulder. J Comput Assist Tomogr. 1998;22(1):31–34. [DOI] [PubMed] [Google Scholar]
- 11. Del Grande F, Aro M, Jalali Farahani S, Cosgarea A, Wilckens J, Carrino JA. High-resolution 3-T magnetic resonance imaging of the shoulder in nonsymptomatic professional baseball pitcher draft picks. J Comput Assist Tomogr. 2016;40(1):118–125. [DOI] [PubMed] [Google Scholar]
- 12. Ferrari JD, Ferrari DA, Coumas J, Pappas AM. Posterior ossification of the shoulder: the Bennett lesion. Etiology, diagnosis, and treatment. Am J Sports Med. 1994;22(2):171–176. [DOI] [PubMed] [Google Scholar]
- 13. Fujisawa H, Kushihashi T, Ukisu R, et al. Diagnostic imaging for sports injuries of the shoulder and upper arm in baseball pitchers. Radiologist. 2002;9(2):101. [Google Scholar]
- 14. Grossman MG, Tibone JE, McGarry MH, Schneider DJ, Veneziani S, Lee TQ. A cadaveric model of the throwing shoulder: a possible etiology of superior labrum anterior-to-posterior lesions. J Bone Joint Surg Am. 2005;87(4):824–831. [DOI] [PubMed] [Google Scholar]
- 15. Higgins JPT, Green S; Cochrane Collaboration Cochrane Handbook for Systematic Reviews of Interventions. Wiley-Blackwell; 2008. [Google Scholar]
- 16. Jobe CM. Posterior superior glenoid impingement: expanded spectrum. Arthroscopy. 1995;11(5):530–536. [DOI] [PubMed] [Google Scholar]
- 17. Karcich J, Kazam JK, Rasiej MJ, Wong TT. Bennett lesions in overhead athletes and associated shoulder abnormalities on MRI. Skeletal Radiol. 2019;48(8):1233–1240. [DOI] [PubMed] [Google Scholar]
- 18. Lädermann A, Chague S, Kolo FC, Charbonnier C. Kinematics of the shoulder joint in tennis players. J Sci Med Sport. 2016;19(1):56–63. [DOI] [PubMed] [Google Scholar]
- 19. Levigne C, Garret J, Grosclaude S, Borel F, Walch G. Surgical technique: arthroscopic posterior glenoidplasty for posterosuperior glenoid impingement in throwing athletes. Clin Orthop Relat Res. 2012;470(6):1571–1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lombardo SJ, Jobe FW, Kerlan RK, Carter VS, Shields CL., Jr Posterior shoulder lesions in throwing athletes. Am J Sports Med. 1977;5(3):106–110. [DOI] [PubMed] [Google Scholar]
- 21. McInnes MDF, Moher D, Thombs BD, et al. Preferred Reporting Items for a Systematic Review and Meta-Analysis of Diagnostic Test Accuracy studies: the PRISMA-DTA statement. JAMA. 2018;319(4):388–396. [DOI] [PubMed] [Google Scholar]
- 22. Meister K, Andrews JR, Batts J, Wilk K, Baumgarten T. Symptomatic thrower’s exostosis: arthroscopic evaluation and treatment. Am J Sports Med. 1999;27(2):133–136. [DOI] [PubMed] [Google Scholar]
- 23. Meister K, Day T, Horodyski M, Kaminski TW, Wasik MP, Tillman S. Rotational motion changes in the glenohumeral joint of the adolescent/Little League baseball player. Am J Sports Med. 2005;33(5):693–698. [DOI] [PubMed] [Google Scholar]
- 24. Nakagawa S, Yoneda M, Hayashida K, Mizuno N, Take Y. Superior Bennett lesion: a bone fragment at the posterosuperior glenoid rim in 5 athletes. Arthroscopy. 2007;23(10):1135.e1131-1134. [DOI] [PubMed] [Google Scholar]
- 25. Nakagawa S, Yoneda M, Hayashida K, Mizuno N, Yamada S. Posterior shoulder pain in throwing athletes with a Bennett lesion: factors that influence throwing pain. J Shoulder Elbow Surg. 2006;15(1):72–77. [DOI] [PubMed] [Google Scholar]
- 26. Nobuhara K. Clinical approaches for shoulder injuries in sports. Japan Med Assoc J. 2005;48(1):6–10. [Google Scholar]
- 27. O’Brien SJ, Neves MC, Arnoczky SP, et al. The anatomy and histology of the inferior glenohumeral ligament complex of the shoulder. Am J Sports Med. 1990;18(5):449–456. [DOI] [PubMed] [Google Scholar]
- 28. Ozaki J, Tomita Y, Nakagawa Y, Tamai S. Surgical treatment for posterior ossifications of the glenoid in baseball players. J Shoulder Elbow Surg. 1992;1(2):91–97. [DOI] [PubMed] [Google Scholar]
- 29. Park JY, Noh YM, Chung SW, et al. Bennett lesions in baseball players detected by magnetic resonance imaging: assessment of association factors. J Shoulder Elbow Surg. 2016;25(5):730–738. [DOI] [PubMed] [Google Scholar]
- 30. Pearce CE, Burkhart SS. The pitcher’s mound: a late sequela of posterior type II SLAP lesions. Arthroscopy. 2000;16(2):214–216. [DOI] [PubMed] [Google Scholar]
- 31. Plomb-Holmes C, Clavert P, Kolo F, Tay E, Lädermann A; French Arthroscopic Society. An orthopaedic surgeon’s guide to ultrasound imaging of the healthy, pathological and postoperative shoulder. Orthop Traumatol Surg Res. 2018;104(8)(suppl):S219–S232. [DOI] [PubMed] [Google Scholar]
- 32. Riand N, Boulahia A, Walch G. Posterosuperior impingement of the shoulder in the athlete: results of arthroscopic debridement in 75 patients [in French]. Rev Chir Orthop Reparatrice Appar Mot. 2002;88(1):19–27. [PubMed] [Google Scholar]
- 33. Walch G, Boileau P, Noel E, Donell ST. Impingement of the deep surface of the supraspinatus tendon on the posterosuperior glenoid rim: an arthroscopic study. J Shoulder Elbow Surg. 1992;1(5):238–245. [DOI] [PubMed] [Google Scholar]
- 34. Wright RW, Paletta GA., Jr Prevalence of the Bennett lesion of the shoulder in major league pitchers. Am J Sports Med. 2004;32(1):121–124. [DOI] [PubMed] [Google Scholar]
- 35. Yoneda M, Nakagawa S, Hayashida K, Fukushima S, Wakitani S. Arthroscopic removal of symptomatic Bennett lesions in the shoulders of baseball players: arthroscopic Bennett-plasty. Am J Sports Med. 2002;30(5):728–736. [DOI] [PubMed] [Google Scholar]
- 36. Yoneda M, Nakagawa S, Mizuno N, et al. Arthroscopic capsular release for painful throwing shoulder with posterior capsular tightness. Arthroscopy. 2006;22(7):801.e801-805. [DOI] [PubMed] [Google Scholar]