To the Editor,
A novel strain of human coronaviruses, the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), named by the International Committee on Taxonomy of Viruses (ICTV), 1 has recently emerged and caused an infectious disease. This disease is referred to as the “coronavirus disease 2019” (COVID‐19) by the World Health Organization (WHO). 2
The US Centers for Disease Control and Prevention (CDC) have proposed that “People with moderate to severe asthma may be at higher risk of getting very sick from COVID‐19. COVID‐19 can affect your respiratory tract (nose, throat, lungs), cause an asthma attack and possibly lead to pneumonia and acute respiratory disease.” (May 24, 2020). (https://www.cdc.gov/coronavirus/2019‐ncov/need‐extra‐precautions/asthma.html) On the other hand, in the UK, NICE proposes rapid guidelines for severe asthma (https://www.guidelines.co.uk/covid‐19‐rapid‐guideline‐severe‐asthma/455275.article).
An ARIA‐EAACI statement has been devised to make recommendations on asthma, and not necessarily on severe asthma, based on a consensus from its members.
It is difficult in many studies to clearly assess the prevalence of asthma on COVID‐19 since most patients are older adults and probably have multimorbidities. Most studies do not clarify whether asthmatic patients with COVID‐19 have isolated asthma or asthma as a multimorbidity, particularly in the context of hypertension, obesity and diabetes. In particular, obesity is a significant risk factor for COVID‐19 and its severity, 3 and may be intertwined with asthma.
In some studies, showing data mostly on critically ill patients, there does not appear to be an increased prevalence of asthma. 4 , 5 , 6 , 7 In Wuhan, the prevalence of asthma in COVID‐19 patients was 0.9%, markedly lower than that of the general adult population of this city. 8 Differently, in New York, among 5,700 hospitalized patients with COVID‐19, asthma prevalence was 9% and COPD 4.5%. 9 In California, 7.4% of the 377 hospitalized patients had asthma or COPD. 10 The US CDC reported that between March 1st and 30th 2020, among COVID‐NET hospitals from 99 counties and 14 states (an open source neural network for COVID‐19 infection), chronic lung disease (primarily asthma) was the second most prevalent comorbid condition for hospitalized patients aged 18‐49 years with laboratory‐confirmed COVID‐19. 11 Among the 17% of COVID‐19‐positive patients with an underlying history of asthma, the incidence was at its highest in younger adults (27% in the 18‐ to 49‐year‐old group). The UK experience on over 20, 133 hospitalized cases shows that 14% of admissions were patients with asthma. 12 In the OpenSAFELY Collaborative Study (UK), an increased risk of severe COVID‐19, including death, was found in patients with asthma, particularly related with a recent use of oral corticosteroid. 13 A review with all identified studies up to 5 May 2020 is available. 14 However, low socioeconomic status, obesity, non‐white ethnicity, chronic respiratory disease and diabetes had stronger signals.
Some anti‐asthma medications, such as ciclesonide, might have a beneficial effect on COVID‐19. 15
Thus, whether patients with asthma are at a higher or lower risk of acquiring COVID‐19 may depend on geography, age, other multimorbidities, different air quality, 16 genetic predispositions, ethnicity, social behaviour, access to health care or other factors. Moreover, the current information is obtained mainly from hospitalization or intensive care unit data. Real‐life data in a non‐selected population of asthmatics are needed to better understand the links between asthma and SARS‐Cov‐2 in terms of both incidence and severity.
Asthma does not seem to be a risk factor for severe COVID‐19 but patients treated with oral corticosteroids may be at a higher risk of severe COVID‐19. 14 However, a large study is needed to fully appreciate the relationship between COVID‐19 and severe asthma.
According to the IPCRG (International Primary Care Respiratory Group), patients are still struggling to differentiate their symptoms between asthma flare‐ups and COVID‐19. They may therefore delay seeking care for asthma or COVID‐19. Interestingly, clarity does not appear to have improved as the weeks have passed. People have recurrences or waves of repeated symptoms, and it is difficult to understand whether the symptoms are related to an asthma exacerbation or to COVID‐19.
According to the IPCRG, many clinicians tend to prescribe antibiotics to people who they believe are having asthma exacerbations “just to be safe.” They focus on the potential infection element of the trigger more than the asthma management itself. It would seem that COVID‐19 might exacerbate this behaviour, not improve it.
In areas where COVID‐19 is prevalent, GPs are still very concerned about oral—and, to a certain degree, inhaled—corticosteroids, possibly because they use remote models of care. They are reluctant to prescribe higher doses of ICS or OCS as they fear they cannot tell the difference between a flare‐up and COVID‐19.
The extent of expression in the upper and lower airways of the SARS‐CoV‐2 entry receptors, angiotensin‐converting enzyme 2 (ACE2) and TMPRSS2, might impact the clinical severity of COVID‐19. ACE‐2 was found to be decreased in patients with allergic asthma 17 or in those receiving inhaled corticosteroids. 18 These data suggest that this expression may be a potential contributor, among several other factors, to reduced COVID‐19 severity in patients with T2 inflammation. 17 , 19 However, ACE‐2 expression in asthma patients was increased in African Americans, in males and in association with diabetes.
Finally, a recent study which analysed the nasal transcriptome of 695 children suggested that the strongest determinants of airway ACE2 and TMPRSS2 expression are T2 inflammation and viral‐induced interferon inflammation. However, this study specifically showed that T2 inflammation (via IL‐13) impacted differentially on ACE2 and TMPRSS2, with a T2‐high phenotype being associated with a highly significant decrease in the former and a significant decrease in the latter receptor. Thus, although SARS‐CoV‐2‐specific analyses and experiments are lacking, the differential effects of T2‐inflammation on ACE2 and TMPRSS2 reported in this study warrant further research on whether T2‐high and T2‐low asthma phenotypes may be associated with differential susceptibility to severe COVID‐19.
The first author developed seven recommendations that were sent for comment to 105 experts around the world . 69 answers were received within 48 hours, and the comments were considered. Where experts suggested modification of the recommendations, a discussion was initiated and recommendations modified until consensus was reached. After these modifications, a total of 9 recommendations were proposed for a second round. In the second round, 145 experts were invited to comment on and approve or reject the recommendations. 78 answers were received within 48 hours and, when an agreement of over 80/100 was reached, the question was included in the statement.
The same approach was used for the research questions. Two research needs were dropped.
The geographic distribution of the experts is given in Figure 1. They were from 43 countries.
FIGURE 1.
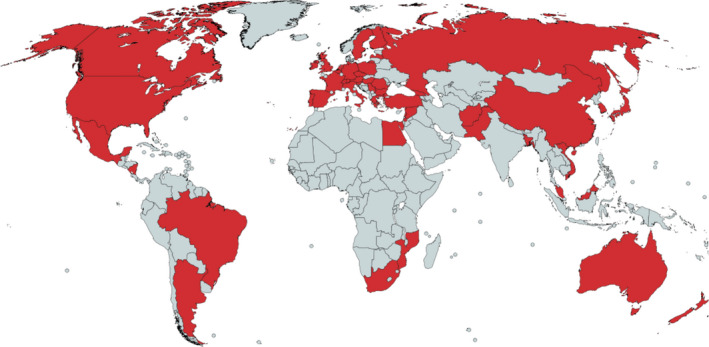
Geographic representation of the experts
ARIA‐EAACI statement (Table 1).
Table 1.
ARIA‐EAACI statement
| 1 | In areas where COVID‐19 is prevalent, screening protocols for COVID‐19 should be applied to anyone having worsening respiratory symptoms, and personal protective equipment should be used. |
| 2 | In areas where COVID‐19 is prevalent, lung function testing procedures should be postponed if not deemed absolutely necessary; portable personal devices measuring PEF and FEV1 can be used in the meantime to monitor asthma control using the telemedicine approach. |
| 3 | In accordance with the Global Initiative for Asthma (GINA) (https://ginasthma.org/recommendations‐for‐inhaled‐asthma‐controller‐medications/), patients with asthma should not stop their prescribed inhaled corticosteroid controller medication (or prescribed oral corticosteroids). Stopping inhaled corticosteroids may have serious consequences. |
| 4 | Long‐term oral corticosteroids may sometimes be required to treat severe asthma, and it may be dangerous to stop them suddenly (GINA). |
| 5 | Oral steroids should continue to be used to treat severe asthma exacerbations. |
| 6 | In patients infected by SARS‐CoV‐2 (symptomatic or asymptomatic), nebulization (which increases the risk of deposition of the virus into the lower airways) should be replaced by spacers of large capacity. |
| 7 |
In accordance with the NICE, in non‐SARS‐CoV‐2 infected patients, we propose(https://www.nice.org.uk/guidance/ng166/chapter/3‐Treatment#patients‐having‐biological‐treatment):
|
| 8 | In SARS‐CoV‐2‐infected patients, in accordance with the EAACI, we propose to cease the treatment until resolution of the disease is established. Thereafter, the administration of the biological should be re‐initiated. |
ARIA‐EAACI research questions (Table 2).
Table 2.
ARIA‐EAACI research questions
| Real‐world studies need to be carried out on a large number of unselected patients to assess | |
|---|---|
| 1 | Impact of COVID‐19 on asthma control |
| 2 | Impact of COVID‐19 respiratory symptoms on severe asthma |
| 3 | Impact of severe asthma on COVID‐19 occurrence and/or severity of pneumonia |
| 4 | Impact of multimorbidities on asthmatic patients for the control of asthma during COVID‐19 |
| 5 | Serologic studies should be performed to assess whether seroconversion and its duration differ in asthmatic and non‐asthmatic subjects |
| 6 | The phenotype of asthma (allergic, neutrophilic, age….) should be studied |
| 7 | In adult patients, studies should clarify whether asthmatic patients with COVID‐19 have isolated asthma or asthma in the context of multimorbidity, particularly in the context of high blood pressure, obesity and diabetes mellitus |
| 8 | Role of pollen season on COVID‐19 severity |
This view is pragmatic, cautious and based upon expert opinion. However, it is likely to require modifications as further evidence is gathered. These recommendations are conditional and should be adapted regularly on the basis of evolving clinical evidence.
CONFLICTS OF INTEREST
IA reports and Associate Editor of Allergy. CA reports grants from Allergopharma, Idorsia, Swiss National Science Foundation, Christine Kühne‐Center for Allergy Research and Education, European Commission's Horison's 2020 Framework Programme, Cure, Novartis Research Institutes, Astra Zeneca, Scibase, advisory role in Sanofi/Regeneron. IA reports personal fees from Mundipharma, Roxall, Sanofi, MSD, Faes Farma, Hikma, UCB, Astra Zeneca, Stallergenes, Abbott, Bial. EB is a member of the Science Committee and Board of the Global Initiative for Asthma (GINA). SBA reports grants from TEVA, personal fees from TEVA, AstraZeneca, Boehringer Ingelheim, GSK, Sanofi, Mylan. JPB reports grants from AstraZeneca, Boston Scientific, GSK, Hoffman La Roche, Ono Pharma, Novartis, Sanofi, Takeda, Boehringer‐Ingelheim, Merck, personal fees from AstraZeneca, GSK, Merck, Metapharm, Novartis, Takeda, other from AstraZeneca, Boehringer‐Ingelheim, GSK, Merck, Novartis. JB reports personal fees from Chiesi, Cipla, Hikma, Menarini, Mundipharma, Mylan, Novartis, Purina, Sanofi‐Aventis, Takeda, Teva, Uriach, other from KYomed‐Innov. RB reports grants to Mainz University and personal fees from Boehringer Ingelheim, GlaxoSmithKline, Novartis, and Roche, as well as personal fees from AstraZeneca, Chiesi, Cipla, Sanofi, and Teva. VC reports personal fees from ALK, Allergopharma, Allergy Therapeutics, Diater, LETI, Thermo Fisher, Stallergenes. RSC reports grants from NIAID, CoFAR, Aimmune, DBV Technologies, Astellas, Regeneron, an Advisory member for Alladapt, Genentech, Novartis, and receives personal fees from Before Brands. AC reports grants and personal fees from GSK, SANOFI, Boehringer‐Ingelheim, Astrazeneca, Mantecorp, MYLAN, Novartis, personal fees and non‐financial support from CHIESI. SdG reports personal fees from AstraZeneca, Chiesi, Menarini, grants and personal fees from GSK, Novartis. DH reports personal fees from AstraZeneca, Chiesi, GSK, Pfizer, personal fees and non‐financial support from Boehringer Ingelheim, Novartis. TE reports other from DBV, Regeneron, grants from Innovation fund Denmark and Co‐I or scientific lead in three investigator initiated oral immunotherapy trials supported by the Allergy and Anaphylaxis Program Sickkids and serve as associate editor for Allergy. Advisory board ALK. JF reports personal fees from AstraZeneca, GSK, undipharma, grants and personal fees from Novartis. MG reports grants and personal fees from Elpen, Novartis, Menarini, grants from Galapagos, personal fees from BMS, MSD. TH reports personal fees from GSK, Mundipharma, OrionPharma. MH reports personal fees and non‐financial support from GlaxoSmithKline, personal fees from Astrazeneca, Novartis, Roche, Sanofi, Teva. JCI reports personal fees from Faes Farma, Eurofarma Argentina, other from Laboratorios Casasco, Sanofi. GJ reports grants from AstraZeneca, Chiesi, personal fees from Bayer, Eureca vzw, Teva, grants and personal fees from GlaxoSmithKline. MJ reports personal fees from ALK‐Abello, Allergopharma, Stallergenes, Anergis, Allergy Therapeutics, Circassia, Leti, Biomay, from HAL, Astra‐Zeneka, GSK, Novartis, Teva, Vectura, UCB, Takeda, Roche, Janssen, Medimmune, Chiesi, LK reports grants and personal fees from Allergopharma, LETI Pharma, MEDA/Mylan, Sanofi, personal fees from HAL Allergie, Allergy Therapeut., grants from ALK Abelló, Stallergenes, Quintiles, ASIT biotech, grants from Lofarma, AstraZeneca, GSK, Inmunotk and Membership: AeDA, DGHNO,Deutsche Akademie für Allergologie und klinische Immunologie, HNO‐BV GPA,EAACI. PK reports personal fees from Astra, Boehringer Ingelheim, Berlin Chemie Menarini, GSK, Lekam, Novartis, Polpharma, Mylan, Orion, Teva, Adamed. VK reports personal fees from GSK, non‐financial support from StallergenGreer, AstraZeneca, Norameda, DIMUNA. DLL reports personal fees from Allakos, Amstrong, Astrazeneca, Boehringer Ingelheim, Chiesi, DBV Technologies, Grunenthal, GSK, MEDA, Menarini, MSD, Novartis, Pfizer, Novartis, Sanofi, Siegfried, UCB, Alakos, Gossamer, grants from Sanofi, Astrazeneca, Novartis, UCB, GSK, TEVA, Boehringer Ingelheim, Chiesi, Purina institute. RL reports grants and personal fees from AZ, GSK, Novartis, grants from Chiesi, JM reports personal fees and other from SANOFI‐GENZYME & REGENERON, NOVARTIS, ALLAKOS, grants and personal fees from MYLAN Pharma, URIACH Group, personal fees from Mitsubishi‐Tanabe, Menarini, UCB, AstraZeneca, GSK, from MSD, outside the submitted work. KN reports grants and other from NIAID, FARE, personal fees and other from Regeneron, grants from EAT, other from Sanofi, Astellas, Nestle, BeforeBrands, Alladapt, ForTra, Genentech, AImmune Therapeutics, DBV Technologies, personal fees from Astrazeneca, ImmuneWorks, Cour Pharmaceuticals, grants from Allergenis, Ukko Pharma, Novartis,AnaptysBio, Adare Pharmaceuticals, Stallergenes‐Greer, NHLBI, NIEHS, EPA, WAO Center of Excellence, Iggenix, Probio, Vedanta, Centecor, Seed, Immune Tolerance Network, NIH,; In addition, Dr Nadeau has a patent Inhibition of Allergic Reaction to Peanut Allergen using an IL‐33 Inhibitor pending, a patent Special Oral Formula for Decreasing Food Allergy Risk and Treatment for Food Allergy pending, a patent Basophil Activation Based Diagnostic Allergy Test pending, a patent Granulocyte‐based methods for detecting and monitoring immune system disorders pending, a patent Methods and Assays for Detecting and Quantifying Pure Subpopulations of White Blood Cells in Immune System Disorders pending, a patent Mixed Allergen Compositions and Methods for Using the Same pending, and a patent Microfluidic Device and Diagnostic Methods for Allergy Testing Based on Detection of Basophil Activation pending. YO reports personal fees from Shionogi Co., Ltd., Torii Co., Ltd., GSK, MSD, Eizai Co.,Ltd., grants and personal fees from Kyorin Co., Ltd., Tiho Co., Ltd., grants from Yakuruto Co., Ltd., Yamada Bee Farm. ROB reports grants and personal fees from AstraZeneca, GSK, grants from Novartis, Medimmune, Bayer. YO reports personal fees from Shionogi Co., Ltd., Torii Co., Ltd., GSK, MSD, Eizai Co.,Ltd., grants and personal fees from Kyorin Co., Ltd., Tiho Co., Ltd., grants from Yakuruto Co., Ltd., Yamada Bee Farm, outside the submitted work. NP reports personal fees from Novartis, Nutricia, HAL, MENARINI/FAES FARMA, SANOFI, MYLAN/MEDA, BIOMAY, AstraZeneca, GSK, MSD, ASIT BIOTECH, Boehringer Ingelheim, grants from Gerolymatos International SA, Capricare. OP reports grants and personal fees from Anergis SA, ALK‐Abelló, Allergopharma, Stallergenes Greer, HAL Allergy Holding BV/HAL Allergie GmbH, Bencard Allergie GmbH/Allergy Therapeutics, Lofarma, ASIT Biotech Tools SA, Laboratorios LETI/LETI Pharma, grants from Biomay, Glaxo Smith Kline Circassia, personal fees from MEDA Pharma/MYLAN, Mobile Chamber Experts (a GA2LEN Partner), Indoor Biotechnologies, Astellas Pharma Global, EUFOREA, ROXALL, NOVARTIS, SANOFI AVENTIS, Med Update Europe GmbH, streamedup! GmbH. FP reports sanofi, novartis, teva, astrazeneca, glaxosmithkline, menarini, mundipharma, guidotti, malesci, chiesi, valeas, allergy therapeutics, almirall, personal fees from boehringer Ingelheim. FR reports personal fees from AstraZeneca, Novartis, Lusomedicamenta, Sanofi, GSK. JS reports other from MEDA, grants and personal fees from SANOFI, personal fees from GSK, NOVARTIS, ASTRA ZENECA, MUNDIPHARMA, FAES FARMA. JSchwarze reports personal fees from MYLAN, outside the submitted work. ASheikh reports support of the Asthma UK Centre for Applied Research. RS reports grants from São Paulo Research Foundation, MSD,grants and personal fees from Novartis, grants, personal fees and non‐financial support from AstraZeneca, Chiesi, Boehringer Ingelheim. IT reports grants from GSK Hellas, ELPEN, personal fees from Boehringer Ingelheim, Novartis, Astra Zeneca, GSK. TZ reports Organizational affiliations: Committee member: WHO‐Initiative "Allergic Rhinitis and Its Impact on Asthma" (ARIA); Member of the Board: German Society for Allergy and Clinical Immunology (DGAKI); Head: European Centre for Allergy Research Foundation (ECARF); President: Global Allergy and Asthma European Network (GA2LEN); Member: Committee on Allergy Diagnosis and Molecular Allergology, World Allergy Organization (WAO). The other authors have no COI to declare.
ACKNOWLEDGMENT
Open access funding enabled and organized by Projekt DEAL.
REFERENCES
- 1. Coronaviridae Study Group of the International Committee on Taxonomy of Viruses . The species Severe acute respiratory syndrome‐related coronavirus: classifying 2019‐nCoV and naming it SARS‐CoV‐2. Nat Microbiol. 2020;5: 536–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bousquet J, Akdis C, Jutel M, et al. Intranasal corticosteroids in allergic rhinitis in COVID‐19 infected patients: An ARIA‐EAACI statement. Allergy. 2020;75: 2440–2444. 10.1111/all.14302 [DOI] [PubMed] [Google Scholar]
- 3. Wadhera RK, Wadhera P, Gaba P, et al. Variation in COVID‐19 hospitalizations and deaths across New York City boroughs. JAMA. 2020;323(21):2192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Grasselli G, Zangrillo A, Zanella A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS‐CoV‐2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323(16):1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zhao Q, Meng M, Kumar R, et al. The impact of COPD and smoking history on the severity of Covid‐19: a systemic review and meta‐analysis. J Med Virol. 2020. 10.1002/jmv.25889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zhang JJ, Cao YY, Dong X, et al. Distinct characteristics of COVID‐19 patients with initial rRT‐PCR‐positive and rRT‐PCR‐negative results for SARS‐CoV‐2. Allergy. 2020;75:1809–1812. 10.1111/all.14316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dong X, Cao YY, Lu XX, et al. Eleven Faces of Coronavirus Disease 2019. Allergy. 2020;75:1699–1709. 10.1111/all.14289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Li X, Xu S, Yu M, et al. Risk factors for severity and mortality in adult COVID‐19 inpatients in Wuhan. J Allergy Clin Immunol. 2020. 10.1016/j.jaci.2020.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized With COVID‐19 in the New York City area. JAMA. 2020;323(20):2052‐2059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Parodi SM, Liu VX. From Containment to Mitigation of COVID‐19 in the US. JAMA. 2020;323(15):1441. [DOI] [PubMed] [Google Scholar]
- 11. Garg S, Kim L, Whitaker M, et al. Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory‐Confirmed Coronavirus Disease 2019 ‐ COVID‐NET, 14 States, March 1–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(15):458‐464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Docherty A, Harrison E, Green C, et al. Features of 16,749 hospitalised UK patients with COVID‐19 using the ISARIC WHO Clinical Characterisation Protocol. 10.1101/2020.04.23.20076042 [DOI] [PMC free article] [PubMed]
- 13. Collaborative TO, Williamson E, Walker A, et al. OpenSAFELY: factors associated with COVID‐19‐related hospital death in the linked electronic health records of 17 million adult NHS patients. MedRIX. 2020. 10.1101/2020.05.06.20092999. https://www.medrxiv.org/content/10.1101/2020.04.23.20076042v1.full.pdf [DOI] [Google Scholar]
- 14. Morais‐Almeida M, Pité H, Aguiar R, Ansotegui I, Bousquet J. Asthma and the COVID‐19 pandemic: literature review. Int Allergy Immunol. 2020; 10.1159/000509057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jeon S, Ko M, Lee J, et al. Identification of antiviral drug candidates against SARS‐CoV‐2 from FDA‐approved drugs. Antimicrob Agents Chemother. 2020. 10.1128/AAC.00819-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wu X, Nethery R, Sabath B, Braun D, Dominici F. Exposure to air pollution and COVID‐19 mortality in the United States: A nationwide cross‐sectional study. medRxiv and. BioRxiv. 2020. https://www.medrxiv.org/content/10.1101/2020.04.05.20054502v2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jackson D, Busse W, Bacharier L, et al. Association of respiratory allergy, asthma and expression of the SARS‐CoV‐2 receptor, ACE2. J Allergy Clin Immunol. 2020; 10.1164/rccm.202003-0821OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Peters MC, Sajuthi S, Deford P, et al. COVID‐19 related genes in sputum cells in asthma: relationship to demographic features and corticosteroids. Am J Respir Crit Care Med. 2020. 10.1164/rccm.202003-0821OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sajuthi S, DeFord P, Jakcson N, et al. Type 2 and interferon inflammation strongly regulate SARS‐CoV‐2 related gene expression in the airway epithelium. bioRxiv. 2020. 10.1101/2020.04.09.034454 [DOI] [PMC free article] [PubMed] [Google Scholar]


