Abstract
Objectives
There are concerns that public anxiety around COVID‐19 discourages patients from seeking medical help. The aim of this study was to see how lockdown due to the pandemic affected the number of admissions of acute stroke.
Methods
All patients discharged from Akershus University Hospital with a diagnosis of transient ischemic attack (TIA) or acute stroke were identified by hospital chart review. January 3 to March 12 was defined as before, and March 13 to April 30 as during lockdown.
Results
There were 21.8 admissions/week before and 15.0 admissions/week during the lockdown (P < .01). Patients had on average higher NIHSS during the lockdown than before (5.9 vs. 4.2, P = .041). In the multivariable logistic regression model for ischemic stroke (adjusted for sex, age, living alone and NIHSS ≤ 5), there was an increased OR of 2.05 (95% CI 1.10‐3.83, P = .024) for not reaching hospital within 4.5 hours during the lockdown as compared to the period before the lockdown.
Conclusion
There was a significant reduction in number of admissions for stroke and TIAs during the lockdown due to the COVID‐19 pandemic in Norway.
Keywords: emergency care, healthcare planning, pandemic, stroke, stroke pathways
1. INTRODUCTION
The COVID‐19 declared pandemic by the World Health Organization (WHO) in March 2020 challenges healthcare systems and societies worldwide. 1 , 2 Many health professionals have questioned whether the public anxiety around COVID‐19 discourages some patients from contacting the healthcare system. After the pandemic lockdown in the UK, there was a 25% fall in emergency room attendances the first week. 3 If this fall continues, it may be asked whether a substantial proportion of the population are missing treatment opportunities with potentially long‐term harm as a consequence. Rapid admission to hospital following stroke is vital in ensuring patients have timely access to treatments such as thrombolysis and endovascular treatment. 4 The effect of acute stroke treatment is highly time dependent with late admission being an independent predictor of worse outcome. 5 , 6 , 7 , 8 It is therefore feared that a large number of stroke patients are at increased risk of dependency or death if they do not seek emergency help.
During the pandemic, there have been many anecdotal reports that the number of stroke patients seen in the emergency department has dropped considerably. However, rigorous studies on this subject have not yet been published. 4 In Norway, lockdown due to the pandemic was decided on March 12. We hypothesized that the lockdown and pandemic influence stroke patient's decision to seek help. The aim of this “Stroke during a pandemic (StrokePan) study” was to see how lockdown due to the COVID‐19 pandemic affected the admissions of transient ischemic attack (TIA) and acute stroke (ischemic and hemorrhagic) in Norway.
2. MATERIAL AND METHODS
2.1. Setting
All patients discharged from Akershus University Hospital with a diagnosis of TIA or acute stroke, both ischemic and hemorrhagic (G45.9, I61.x and I63.x) were identified by review of the hospital diagnosis registry for patients admitted between January 1 and April 30, 2020. Akershus University Hospital is Norway's largest emergency care hospital. It is located about 20 km outside of the capital Oslo with a catchment area that consists of a mixed urban and rural population. Norwegian hospitals are almost exclusively publicly financed, and Norway has an all‐covering national health insurance. Thus, all patients enter the hospital´s emergency ward on the same conditions and with the same threshold for further in‐patient admission. Akershus University Hospital is the only hospital in the catchment area covering a population of 570.000 which is approximately 10% of Norway's population. The maximum prehospital transfer time to the hospital is approximately 90 minutes. The hospital's stroke unit is classified as a comprehensive stroke center which includes endovascular therapy.
2.2. Outcomes
To describe the long‐term trend of admissions due to acute cerebrovascular diseases, we compared the monthly admissions between January 2015 and December 2019 and between January and May 2020. To evaluate the potential differences in relation to the lockdown, we compared weekly admissions between January 2020 and May 2020. The period from January 3 to March 12 was defined as before lockdown (week 1‐10) and the period from March 13 to April 30 was defined as lockdown (week 11‐17).
2.3. Ethics approval
The Regional Committee for Medical Research Ethics South‐East (2020/136724) and the Data Protection Officer at Akershus University Hospital approved the study. In accordance with the approval from the Regional Committee for Medical Research Ethics and the Norwegian law on medical research, the project did not require a written patient consent.
2.4. Statistics
For descriptive data, proportions, median, means, and SDs are given. Groups (before and during lockdown) were compared using the t test or Wilcoxon (continuous data) or the chi‐squared test (categorical data). Multivariable logistic regression of predictors for not reaching hospital within 4.5 hours of onset (yes or no, as the dependent variable) was performed. Sex (women vs. men), age, living alone (yes vs no), mild stroke (National Institute of Health Stroke Scale (NIHSS) ≤5 yes vs no), and time period (before vs. lockdown) were used as independent variables. Significance levels were set at P < .05, using two‐sided test. Statistical analyses were performed using SPSS 26.00 (SPSS Inc, Chicago, IL, USA).
3. RESULTS
The overall trend for admissions due to stroke or TIAs to our hospital between January 2015 and April 2020 is shown in Figure 1. There is an all‐time low in admission rates in March and April 2020 compared to all previous months. A more detailed description of the type of stroke and admissions (N = 323) before and during lockdown are given in Table 1 and Figure 2. The numbers and characteristics of the sample from the period before the lockdown (week 1‐10) have also been compared to the period December 2018‐April 2019 with no differences (data not shown).
FIGURE 1.
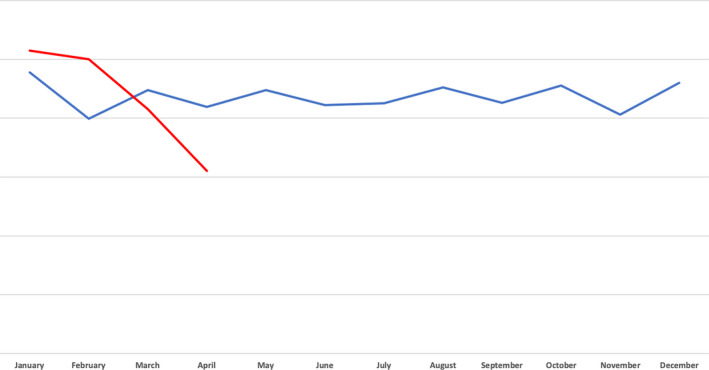
Month by month trend for admissions due to acute stroke and transient ischemic attacks. Blue line—2015‐2019 (average). Red line—2020
TABLE 1.
Description of the total sample
|
Before lockdown January 1‐March 12 N = 218 |
Lockdown March 12‐April 30 N = 105 |
Total January 1‐April 30 N = 323 |
P‐value* | |
|---|---|---|---|---|
| Age, mean years (SD) | 73.5 (12.1) | 75.0 (11.9) | 74.0 (12.1) | .31 |
| Age ≥ 80 y, n (%) | 73 (33) | 45 (43) | 118 (37) | .10 |
| Sex, women, n (%) | 99 (45) | 51 (49) | 150 (46) | .59 |
| Living alone, n (%) | 77 (35) | 39 (37) | 116 (36) | .75 |
| NIHSS at admission | ||||
| Median (IQR) | 2 (6) | 2 (6) | 2 (6) | .94 |
| Mean (SD) | 4.2 (6.1) | 5.9 (8.6) | 4.7 (7.1) | .041 |
| NIHSS > 5 at admission, n (%) | 55 (25) | 33 (31) | 88 (27) | .13 |
| Reaching hospital within 4.5 h after onset, n (%) | 102 (47) | 41 (39) | 143 (44) | .18 |
| Proportion of those with ischemic stroke reaching hospital within 4.5 h after onset, n (%) | 65 (45) | 23 (30) | 88 (40) | .029 |
| Proportion of those with ischemic stroke that received thrombolysis, n (%) | 36 (25) | 14 (18) | 50 (29) | .26 |
| Discharge diagnosis, n (%) | ||||
| Ischemic stroke | 143 (66) | 76 (72) | 219 (68) | .22 |
| Hemorrhagic stroke | 29 (13) | 10 (9) | 39 (12) | .18 |
| Transient ischemic attack | 46 (21) | 19 (18) | 65 (20) | .53 |
| Length of hospital stay, mean days (SD) | 5.7 (3.7) | 5.0 (3.7) | 5.5 (3.8) | .10 |
| In‐hospital mortality, n (%) | 12 (6) | 5 (5) | 17 (5) | .34 |
Abbreviation: NIHSS, National Institute of Health Stroke Scale.
Lockdown compared to before lockdown.
FIGURE 2.
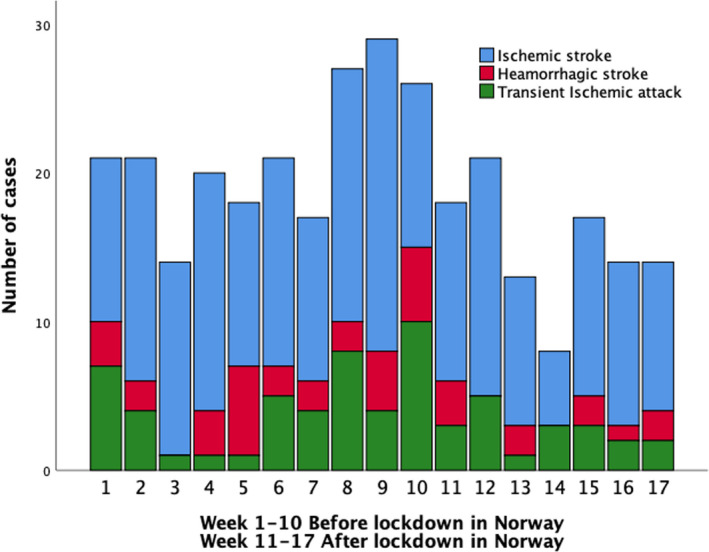
Weekly admission rates for transient ischemic attack, ischemic stroke, and hemorrhagic stroke before and during lockdown in 2020
There were 21.8 (SD 4.7, range 29‐14) admissions weekly before the lockdown and 15.0 (SD 4.2, range 21‐8) admissions weekly during the lockdown (t test, P = .008).
Patients with strokes or TIAs had on average higher NIHSS at admission during the lockdown as compared to before lockdown (5.9 vs 4.2, t test, P = .041).
The proportion of those with ischemic stroke reaching hospital within 4.5 hours (thrombolysis) was significantly higher before than during lockdown (45% vs 30%, χ 2‐test P = .029). The proportion receiving thrombolysis if admitted within 4.5 hours did not differ before and during lockdown.
In the multivariable logistic regression model (Table 2) for ischemic stroke, there was an increased OR of 2.05 (95% CI 1.10‐3.83, P = .024) for not reaching hospital within 4.5 hours during the lockdown as compared to period before the lockdown.
TABLE 2.
Multivariable logistic regression. Predictors for not reaching hospital within 4.5 h of onset among those with ischemic stroke (N = 219)
| Outside 4.5 h | ||||
|---|---|---|---|---|
| N | Odds ratio | 95% CI | P‐value | |
| Sex | ||||
| Men | 124 | 1 | ||
| Women | 95 | 1.86 | 1.01‐3.43 | .045 |
| Age | 219 | 1.00 | 0.97‐1.02 | .74 |
| Living alone | ||||
| No | 139 | 1 | ||
| Yes | 80 | 1.45 | 0.79‐2.68 | .23 |
| NIHSS ≤ 5 | ||||
| No | 141 | 1 | ||
| Yes | 78 | 2.70 | 1.47‐4.97 | .01 |
| COVID‐19 period | ||||
| Before lockdown | 143 | 1 | ||
| After lockdown | 76 | 2.05 | 1.10‐3.83 | .024 |
| Constant | 0.2 | .13 | ||
4. DISCUSSION
We found a 32% reduction in the weekly number of admissions for stroke (29%) and TIAs (41%) during the first seven weeks of the pandemic lockdown in Norway. Patients admitted during the lockdown had on average almost two points higher NIHSS scores. Overall, there were no significant differences between the proportion reaching hospital within the timeframe of thrombolysis or not. However, a much larger proportion of those with ischemic stroke seemed to miss the opportunity for thrombolysis during the lockdown compared to before.
After the lockdown in Norway, mass media and politicians reported worries that hospitals would struggle with possible overcrowding and not be able to provide treatment to all patients during the pandemic. Thus, stances were taken to increase the capacity to handle a substantial number of patients needing intensive care. The COVID‐19 pandemic has been fairly well controlled in Norway, and by May 12, Norway had among the lowest mortality rates reported worldwide with overall 228 COVID‐19‐related deaths in 5.4 million inhabitants. 9 This scenario could of course change, but until now, patients with COVID‐19 have not overcrowded the hospitals. During the lockdown, primary care physicians and hospitals have expressed their worries about their impression that fewer people have sought medical help. This has led to several official requests by the Minister of Health that people must seek health care in the same way as before the pandemic.
Based on the monthly comparison of the admissions over the previous 5 years (Figure 1), we suggest that there is a real and highly relevant reduction in admissions for stroke and TIAs during the lockdown. We have no other reasonable explanation than the effect of the lockdown for this decrease in admission rates. The reasons why 30% less stroke and TIA patients have been hospitalized during the pandemic lockdown are unknown. The Emergency Department and Stroke Unit at our hospital have not changed their criteria for stroke admissions. All treatment options have been available as before the lockdown. The finding that a similar proportion of ischemic stroke patients actually received thrombolysis if admitted within 4.5 hours concur with the hypothesis that the reasons are mostly outside the hospital system. It is previously shown that hurdles for acute stroke patients to seek immediate help include lack of knowledge, problems with identifying stroke symptoms, a wait‐and‐see attitude, a hope that symptoms will resolve, misunderstanding the importance of acute treatment but also fear to unnecessary increase the burden of health services and not wanting to use resources unwisely. 10 , 11 , 12 The mass media coverage of the worries that hospitals would struggle with possible overcrowding may have contributed to fewer stroke patients seeking help. In addition, patients might be uneasy of possible exposure for coronavirus within the hospital. Hence, in particular patients with minor strokes and TIAs possibly could decide not to be hospitalized. The fact that our patients had on average 2 points higher NIHSS score during the pandemic support this. Admission of more severe strokes is probably not affected by the lack of knowledge of stroke symptoms or not understanding the need of hospitalization. Previous stroke may increase knowledge about the disease and thus potentially lead to earlier hospitalization if recurrent stroke. However, information about this was unfortunately not available in the present study. Milder stroke and living alone have previously been associated with delayed admission. 13 , 14 , 15 The consequences of fewer admissions during the lockdown are still not known. However, delayed admission for ischemic stroke as in the present study has been found to be an independent predictor of worse outcome in studies not related to the pandemic. 5 , 6 If increased dependency and more years lived with disability are the results for the stroke patients, then it may be questioned if the pandemic has much larger and broader effect than only the COVID‐19 related diseases. This may be an even larger public health problem in countries more affected by the pandemic than Norway with its relatively low COVID‐19 burden. The main limitations to our study are that it is a single‐center retrospective study. However, Akershus University Hospital is Norway´s largest hospital covering approximately 10% of Norway's population and is the only hospital in the catchment area, leaving the population unselected. The population is also reasonable representative of the total Norwegian population.
Norway is a country with large geographical differences, and our findings may be different in more rural and remote areas with even longer transfer to hospitals.
As far as we know, this is the first study to report on how lockdown due to the COVID‐19 pandemic affected the admissions of TIA and acute stroke (ischemic and hemorrhagic).
For future outbreaks, the healthcare system should be aware that people tend to avoid seeking medical care during a pandemic. The healthcare system must communicate clearly the capacity to handle medical emergencies in treatment chains with low risk of transmission of infectious disease. Further, people with acute stroke‐like symptoms should be encouraged to seek medical care immediately despite minor or temporary symptoms. More research on people's healthcare seeking behavior and their prognosis during long‐term lockdown is warranted.
CONFLICTS OF INTERESTS
None.
Kristoffersen ES, Jahr SH, Thommessen B, Rønning OM. Effect of COVID‐19 pandemic on stroke admission rates in a Norwegian population. Acta Neurol Scand. 2020;142:632–636. 10.1111/ane.13307
Funding information
The study was funded by Akershus University Hospital.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on reasonable request from the corresponding author.
REFERENCES
- 1. Heymann DL, Shindo N. COVID‐19: what is next for public health? Lancet. 2020;395:542‐545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lipsitch M, Swerdlow DL, Finelli L. Defining the epidemiology of covid‐19 ‐ studies needed. N Engl J Med. 2020;382:1194‐1196. [DOI] [PubMed] [Google Scholar]
- 3. Thornton J. Covid‐19: A&E visits in England fall by 25% in week after lockdown. BMJ. 2020;369:m1401. [DOI] [PubMed] [Google Scholar]
- 4.On Behalf of The American Heart Association/American Stroke Association Stroke Council Leadership . Temporary emergency guidance to US stroke centers during the COVID‐19 pandemic. Stroke. 2020;51:1910–1912. https://www.ahajournals.org/doi/10.1161/STROKEAHA.120.030023. [DOI] [PubMed] [Google Scholar]
- 5. Silvestrelli G, Parnetti L, Paciaroni M, et al. Early admission to stroke unit influences clinical outcome. Eur J Neurol. 2006;3:250‐255. [DOI] [PubMed] [Google Scholar]
- 6. Lees KR, Bluhmki E, von Kummer R, et al. Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet. 2010;375:1695‐1703. [DOI] [PubMed] [Google Scholar]
- 7. Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large‐vessel ischaemic stroke: a meta‐analysis of individual patient data from five randomised trials. Lancet. 2016;387:1723‐1731. [DOI] [PubMed] [Google Scholar]
- 8. Sun H, Liu Y, Gong P, et al. Intravenous thrombolysis for ischemic stroke with hyperdense middle cerebral artery sign: a meta‐analysis. Acta Neurol Scand. 2020;141:193‐201. [DOI] [PubMed] [Google Scholar]
- 9. Norwegian Institute of Public Health . Daily report and statistics about coronavirus and COVID‐19 2020 [Accessed 12th May 2020]. Available from: https://www.fhi.no/en/id/infectious‐diseases/coronavirus/daily‐reports/daily‐reports‐COVID19/
- 10. Lecouturier J, Murtagh MJ, Thomson RG, et al. Response to symptoms of stroke in the UK: a systematic review. BMC Health Serv Res. 2010;10:157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Teuschl Y, Brainin M. Stroke education: discrepancies among factors influencing prehospital delay and stroke knowledge. Int J Stroke. 2010;5:187‐208. [DOI] [PubMed] [Google Scholar]
- 12. Le Bonniec A, Haesebaert J, Derex L, et al. Why patients delay their first contact with health services after stroke? A qualitative focus group‐based study. PLoS One. 2016;11:e0156933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Faiz KW, Sundseth A, Thommessen B, et al. Factors related to decision delay in acute stroke. J Stroke Cerebrovasc Dis. 2014;23:534‐539. [DOI] [PubMed] [Google Scholar]
- 14. Jorgensen HS, Nakayama H, Reith J, et al. Factors delaying hospital admission in acute stroke: the Copenhagen Stroke Study. Neurology. 1996;47:383‐387. [DOI] [PubMed] [Google Scholar]
- 15. Wester P, Rådberg J, Lundgren B, et al. Factors associated with delayed admission to hospital and in‐hospital delays in acute stroke and TIA: a prospective, multicenter study. Seek‐ Medical‐Attention‐in‐Time Study Group. Stroke. 1999;30:40‐48. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on reasonable request from the corresponding author.


