Abstract
Objective
The social and economic consequences of COVID‐19 and related public health interventions aimed at slowing the spread of the virus have been proposed to increase suicide risk. However, no research has examined these relations. This study examined the relations of two COVID‐19 consequences (i.e., stay‐at‐home orders and job loss) to suicide risk through thwarted belongingness, perceived burdensomeness, and loneliness.
Method
Online data from a nationwide community sample of 500 adults (mean age = 40) from 45 states were collected between March 27 and April 5, 2020. Participants completed measures assessing thwarted belongingness, perceived burdensomeness, loneliness, and suicide risk, as well as whether they (a) were currently under a stay‐at‐home order and (b) had experienced a recent job loss due to the pandemic.
Results
Results revealed a significant indirect relation of stay‐at‐home order status to suicide risk through thwarted belongingness. Further, whereas recent job loss was significantly correlated with suicide risk, neither the direct relation of job loss to suicide risk (when accounting for their shared relations to perceived burdensomeness) nor the indirect relation through perceived burdensomeness was significant.
Conclusions
Results highlight the potential benefits of interventions targeting thwarted belongingness and perceived burdensomeness to offset suicide risk during this pandemic.
INTRODUCTION
Emerging infectious diseases, such as HIV and 2009’s pandemic influenza A (H1N1), can have significant economic, social, and medical costs (Danziger, 1994; Gasparini, Amicizia, Lai, & Panatto, 2012; Meltzer, Cox, & Fukuda, 1999; Shrestha et al., 2011; Szucs, 1999). In late 2019, an emerging disease called coronavirus 2019 (COVID‐19) rapidly spread across the globe and became an unprecedented public health event (Centers for Disease Control and Prevention [CDC], 2020; World Health Organization [WHO], 2020). Indeed, in 4 months’ time, COVID‐19—which is caused by the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2; Lu et al., 2020; Zhou et al., 2020)—has infected over 2 million people and caused nearly 150,000 deaths across 185 countries (CDC, 2020; Dong, Du, & Gardner, 2020). The U.S. has been among the most highly affected countries to date, accounting for approximately 30% of infections and 20% of deaths worldwide (CDC, 2020; Dong et al., 2020). Moreover, due to a combination of COVID‐19’s long incubation period, ease of transmission, relatively high mortality rate (compared to the seasonal flu), and lack of pharmacological interventions (Linton et al., 2020; Rajgor, Lee, Archuleta, Bagdasarian, & Quek, 2020; Shereen, Khan, Kazmi, Bashir, & Siddique, 2020), extraordinary social distancing interventions have been implemented in many states to slow the spread of the virus, including relatively restrictive shelter‐in‐place or stay‐at‐home orders issued in 42 states, the District of Columbia, and Puerto Rico (Mervosh, Lu, & Swales, 2020). These orders, which have shuttered schools, universities, and nonessential businesses, urge individuals to stay at home unless it is absolutely necessary to leave, and promote strict physical distancing to slow the spread of the virus (CDC, 2020).
From a public health perspective, the reasoning behind such interventions is clear: Physically separating people is an effective strategy for preventing infectious diseases from spreading (Ahmed, Zviedrite, & Uzicanin, 2018; Jackson, Mangtani, Hawker, Olowokure, & Vynnycky, 2014; Qualls et al., 2017), including COVID‐19 (Flaxman et al., 2020; Thakkar, Burstein, Hu, Selvajar, & Klein, 2020). Yet, despite the necessity of stay‐at‐home orders and other social distancing interventions from a disease prevention perspective, these measures are likely to have numerous unintended social and economic consequences that may adversely affect psychological outcomes during this time (Galea, Merchant, & Lurie, 2020; Reger, Stanley, & Joiner, 2020; Thunström, Newbold, Finnoff, Ashworth, & Shogren, 2020).
Indeed, pandemics of this nature have well‐documented economic and social consequences (Chen, Huang, Chuang, Chiu, & Kuo, 2011; Reger et al., 2020; Thunström et al., 2020)—some of which have been linked to psychological difficulties (Montemurro, 2020; Wang et al., 2020), including suicide risk (see Reger et al., 2020). Currently, in the United States, beyond the immediate physical health consequences of COVID‐19 (and related fear and distress associated with these consequences), two consequences of the COVID‐19 pandemic that stand out as particularly relevant to suicide risk are the social isolation related to stay‐at‐home orders and the widespread job loss related to the current economic crisis—both of which have been theoretically and/or empirically linked to suicide risk (e.g., Classen & Dunn, 2012; Oyesanya, Lopez‐Morinigo, & Dutta, 2015; Reger et al., 2020). For example, with regard to the economic consequences of this pandemic, both theory and research support an association between involuntary job loss and suicide risk (Classen & Dunn, 2012; Milner et al., 2014), with recent job loss from mass‐layoffs in particular (comparable to what is occurring currently in the United States) associated with increased suicide risk (Classen & Dunn, 2012).
Likewise, the widespread social distancing interventions implemented to slow the spread of the virus (of which stay‐at‐home orders are the most restrictive) have been proposed to increase suicide risk by increasing social isolation and loneliness (Reger et al., 2020). Specifically, although stay‐at‐home orders are designed to increase physical distancing in particular (and need not negatively impact social connections and connectedness through remote or virtual means), researchers have suggested that an unintended consequence of social distancing interventions may be an increase in social isolation and related feelings of loneliness (Reger et al., 2020). Loneliness, in turn, is a well‐documented suicide risk factor (e.g., Calati et al., 2019; Joiner, Ribeiro, & Silva, 2012; Li, Dorstyn, & Jarmon, 2020) that evidences strong associations with suicidal ideation, suicide attempts, and suicide risk (e.g., Calati et al., 2019; Chang et al., 2017; Li et al., 2020; Stickley & Koyanagi, 2016; Stravynski & Boyer, 2001).
Beyond just examining the relations of pandemic‐related stay‐at‐home orders and job loss to suicide risk, research is needed to clarify the factors that may account for these relations. The Interpersonal Psychological Theory of Suicide (ITS; Van Orden et al., 2010) provides a particularly useful framework in this regard. According to this theory, the desire for suicide is driven by perceived burdensomeness (i.e., perceptions of being a burden to others) and thwarted belongingness (i.e., feeling disconnected from and lacking meaningful relationships with others). Notably, although thwarted belongingness overlaps with loneliness, it is a broader construct that also captures the nature and extent of supportive and reciprocal interpersonal relationships. A recent meta‐analysis provides empirical support for this theory and the proposed relations of perceived burdensomeness and thwarted belongingness to suicidal desire (Chu et al., 2017). With regard to the relevance of these factors to the relations of interest in this study, thwarted belongingness would be expected to play a particularly important role in the relation of stay‐at‐home orders to suicide risk, capturing the proposed unintended negative consequences of social distancing interventions on social connectedness (Reger et al., 2020). Conversely, although a recent job loss could also contribute to thwarted belongingness (particularly if that job was a primary source of social connection), theory suggests the particular relevance of perceived burdensomeness to the relation between job loss and suicide risk. Specifically, the inability to provide for loved ones or support oneself financially could increase the experience of being a burden on others, which, in turn, would increase the desire for suicide and suicide risk (Cukrowicz, Cheavens, Van Orden, Ragain, & Cook, 2011; Van Orden et al., 2010).
The present study examined the relations of COVID‐19‐related stay‐at‐home orders and job loss to suicide risk, both directly and indirectly through thwarted belongingness and perceived burdensomeness. Given that social distancing and related social isolation have been proposed to increase suicide risk through loneliness, we also examined the indirect relation of stay‐at‐home orders in particular to suicide risk through loneliness. We hypothesized that both recent job loss and stay‐at‐home order status would be associated with increased suicide risk. We also hypothesized the differential relevance of thwarted belongingness and perceived burdensomeness to the relations of stay‐at‐home order status and pandemic‐related job loss, respectively, to suicide risk. Specifically, we hypothesized that stay‐at‐home order status would be indirectly related to suicide risk through thwarted belongingness and loneliness, whereas recent job loss would be indirectly related to suicide risk through perceived burdensomeness.
Method
Participants
Participants included a nationwide community sample of 500 adults from 45 states in the United States who completed online measures through an Internet‐based platform (Amazon’s Mechanical Turk; MTurk) from March 27, 2020, through April 5, 2020. The study was posted to MTurk via CloudResearch (cloudresearch.com), an online crowdsourcing platform linked to MTurk that provides additional data collection features (e.g., creating selection criteria; Chandler, Rosenzweig, Moss, Robinson, & Litman, 2019). MTurk is an online labor market that provides “workers” with the opportunity to complete different tasks in exchange for monetary compensation, such as completing questionnaires for research. Data provided by MTurk‐recruited participants have been found to be as reliable as data collected through more traditional methods (Buhrmester, Kwang, & Gosling, 2011). Likewise, MTurk‐recruited participants have been found to perform better on attention check items than college student samples (Hauser & Schwarz, 2016) and comparably to participants completing the same tasks in a laboratory setting (Casler, Bickel, & Hackett, 2013). Studies also show that MTurk samples have the advantage of being more diverse than other Internet‐recruited or college student samples (Buhrmester et al., 2011; Casler et al., 2013). For the present study, inclusion criteria included (a) U.S. resident, (b) at least a 95% approval rating as an MTurk worker, (c) completion of at least 5,000 previous MTurk tasks (referred to as Human Intelligence Tasks), and (d) valid responses on questionnaires (i.e., assessed by accurate completion of multiple attention check items).
Participants (47% women; 51.8% men; 0.2% transgender; 0.6% nonbinary; 0.4% other) ranged in age from 20 to 74 years (M age = 40.0 ± 11.6). All states in the United States were represented, with the exception of Delaware, New Hampshire, North Dakota, Vermont, and West Virginia (see Table 1 for the distribution of participants across states). Most participants identified as White (85%), followed by Black/African‐American (8.4%), Asian/Asian‐American (6.6%), Latinx (1.9%), and Native American (1.6%). Regarding educational attainment, 11.8% had completed high school or received a GED, 35.6% had attended some college or technical school, 43% had graduated from college, and 9.6% had advanced graduate/professional degrees. Most participants were employed full‐time (69.2%), followed by employed part‐time (16.2%) and unemployed (14.6%). Annual household income varied, with 30.6% of participants reporting an income of <$35,000, 33.6% reporting an income of $35,000 to $64,999, and 35.8% reporting an income of ≥$65,000. With regard to participants’ household composition, 58.6% reported living alone and the remaining 41.4% reported living with at least one other person (ranging from 2–8; mean = 3.2 ± 1.1). Very few participants reported having sought out testing for COVID‐19 (1%) or having been infected with COVID‐19 (0.8%).
Table 1.
Distribution of participants across the United States (N = 500)
| State of residence | % (n) | State of residence | % (n) |
|---|---|---|---|
| Alabama | 1.4% (7) | Montana | 0.2% (1) |
| Alaska | 0.2% (1) | Nebraska | 0.2% (1) |
| Arizona | 1.8% (9) | Nevada | 1.2% (6) |
| Arkansas | 1.5% (5) | New Hampshire | — |
| California | 8.6% (43) | New Jersey | 2.2% (11) |
| Colorado | 1.2% (6) | New Mexico | 0.8% (4) |
| Connecticut | 1.6% (8) | New York | 5.4% (27) |
| Delaware | — | North Carolina | 4.6% (23) |
| Florida | 11.2% (56) | North Dakota | — |
| Georgia | 2.4% (12) | Ohio | 4.0% (20) |
| Hawaii | 0.8% (4) | Oklahoma | 1.8% (9) |
| Idaho | 0.4% (2) | Oregon | 2.2% (11) |
| Illinois | 3.4% (17) | Pennsylvania | 6.0% (30) |
| Indiana | 1.8% (9) | Rhode Island | 0.6% (3) |
| Iowa | 0.6% (3) | South Carolina | 1.6% (8) |
| Kansas | 0.6% (3) | South Dakota | 0.4% (2) |
| Kentucky | 1.8% (9) | Tennessee | 2.6% (13) |
| Louisiana | 1.4% (7) | Texas | 5.6% (28) |
| Maine | 0.4% (2) | Utah | 0.6% (3) |
| Maryland | 0.6% (3) | Vermont | — |
| Massachusetts | 1.8% (9) | Virginia | 2.0% (10) |
| Michigan | 4.4% (22) | Washington | 3.0% (15) |
| Minnesota | 1.6% (8) | West Virginia | — |
| Mississippi | 1.0% (5) | Wisconsin | 2.6% (13) |
| Missouri | 1.6% (8) | Wyoming | 0.8% (4) |
Procedure
All procedures received approval from the university’s Institutional Review Board. To ensure the study was not being completed by a bot (i.e., an automated computer program used to complete simple tasks), participants first responded to a Completely Automatic Public Turing test to Tell Computers and Humans Apart (CAPTCHA) prior to providing informed consent. On the consent form, participants were also informed that “…we have put in place a number of safeguards to ensure that participants provide valid and accurate data for this study. If we have strong reason to believe your data are invalid, your responses will not be approved or paid and your data will be discarded.” Data were collected in blocks of nine participants at a time, and all data, including attention check items and geolocations (i.e., geographical coordinates used to identify participants outside of the United States and/or in locations determined to be “bot farms” within the MTurk community; see Kennedy, Clifford, Burleigh, Jewell, & Waggoner, 2018), were examined by researchers before compensation was provided. Attention check items included three explicit requests embedded within the questionnaires (e.g., “If you are paying attention, choose ‘2’ for this question”), two multiple‐choice questions (e.g., “How many words are in this sentence?”), a math problem (e.g., “What is 4 plus 2”), and a free‐response item (e.g., “Please briefly describe in a few sentences what you did in this study”). Participants who failed one or more attention check items were removed from the study (n = 53 of 553 completers). Workers who completed the study and whose data were considered valid (based on attention check items and geolocations; N = 500) were compensated $3.00 for their participation.
Measures
COVID‐19‐related experiences and stressors were assessed via a 20‐item measure developed for this study. Participants were asked about a variety of relevant experiences related to the pandemic. Of interest to the present study were questions assessing whether they were currently under a stay‐at‐home order (“Do you live in a state that has instituted a stay‐at‐home order?” [0 = no; 1 = yes]) and whether they had experienced a recent job loss as a result of the pandemic (“Have you experienced a recent job loss due to the pandemic?” [0 = no; 1 = yes]).
The Interpersonal Needs Questionnaire (INQ; Van Orden, Cukrowicz, Witte, & Joiner, 2012) is a 15‐item self‐report measure with subscales assessing thwarted belongingness and perceived burdensomeness. The 15‐item iteration of the INQ was used due to research demonstrating that it outperforms other versions of this measure (Hill et al., 2015). Items assessing thwarted belongingness (e.g., “These days, I feel disconnected from other people.”) and perceived burdensomeness (e.g., “These days I think my death would be a relief to the people in my life.”) are rated on a 7‐point Likert‐type scale ranging from 1 (not at all true for me) to 7 (very true for me). Higher scores on each subscale are indicative of greater thwarted belongingness and perceived burdensomeness. Research provides support for the reliability and convergent and divergent validity of both subscales (Hallensleben, Spangenberg, Kapusta, Forkmann, & Glaesmer, 2016; Marty, Segal, Coolidge, & Klebe, 2012; Van Orden et al., 2012). Internal consistency of both subscales in the current sample was acceptable (αs > 0.91).
The UCLA Loneliness Scale—version 3 (ULS‐3; Russell, 1996; Russell, Peplau, & Cutrona, 1980) is a 20‐item self‐report measure of perceptions of loneliness and social isolation. Participants rate items (e.g., “No one really knows me well;” I lack companionship;” “There are people I feel close to [reverse scored]”) based on how often they apply to themselves on a 4‐point Likert‐type scale ranging from 1 (never) to 4 (often). Higher scores are indicative of greater loneliness. The ULS‐3 has demonstrated adequate test–retest reliability and good construct validity (Russell, 1996). Internal consistency in the present sample was acceptable (α = 0.94).
The Depression Symptom Index‐Suicide Subscale (DSI‐SS; Metalsky & Joiner, 1997) was used to measure current suicide risk. The DSI‐SS is a 4‐item screening measure that assesses the frequency and intensity of suicidal thoughts, plans, and impulses over the past 2 weeks. Scores on this measure have been found to be positively associated with depression symptoms (Cukrowicz et al., 2011; Joiner, Pfaff, & Acres, 2002) and to be higher among individuals with (vs. without) a history of suicide attempts (Capron et al., 2012). For the present study, a continuous variable assessing the severity of current suicide risk was calculated by summing all four items (α = 0.94 in this sample).
RESULTS
Preliminary analyses
At the time of data collection, 82.4% (n = 412) of participants were under a stay‐at‐home order and 11% (n = 55) reported a recent job loss related to the pandemic. On the DSI‐SS, 11.6% (n = 58) of participants were classified as having high suicide risk (operationalized as a score of ≥3 on this measure; Joiner et al., 2002). Descriptive data for and correlations among the primary variables of interest are presented in Table 2. Results revealed significant positive zero‐order associations between recent job loss (0 = no; 1 = yes) and both suicide risk and perceived burdensomeness. Stay‐at‐home order status (0 = no; 1 = yes) was not significantly correlated with suicide risk; however, it was significantly positively correlated with thwarted belongingness and loneliness.
Table 2.
Descriptive data for and correlations among the primary variables of interest (N = 500)
| Variable | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1. Recent job loss | — | .028 | .116** | .056 | .068 | .117** |
| 2. Stay‐at‐home order status | — | .045 | .105* | .126** | −.042 | |
| 3. Perceived burdensomeness | — | .459*** | .425*** | .532*** | ||
| 4. Thwarted belongingness | — | .861*** | .315*** | |||
| 5. Loneliness | — | .299*** | ||||
| 6. Suicide risk | — | |||||
| Mean or % indicating “yes” | 11% | 82.4% | 9.72 | 25.66 | 2.01 | 4.46 |
| Standard deviation | — | — | 7.13 | 13.62 | 0.66 | 1.48 |
Recent job loss and stay‐at‐home order status are dichotomous variables, scored such that 0 = no and 1 = yes.
p < .05.
p < .01.
p < .001.
Primary analyses
The PROCESS (version 3.3) macro for SPSS (Model 4; Hayes, 2017) was used to examine the indirect relations of (a) recent job loss to suicide risk through perceived burdensomeness (thwarted belongingness and loneliness were not examined in this model due to their lack of significant associations with recent job loss); and (b) stay‐at‐home order status to suicide risk through thwarted belongingness and loneliness (perceived burdensomeness was not examined in this model due to its lack of significant association with stay‐at‐home order status). In both models, age, sex, racial/ethnic background, income, and household composition (lives alone vs. lives with other people) were included as covariates, given their relevance to suicide risk and/or pandemic‐related outcomes. All indirect relations were evaluated using bias‐corrected 95% confidence intervals based on 10,000 bootstrap samples.
With regard to the analysis examining the indirect relation of recent job loss to suicide risk through perceived burdensomeness, the overall model was significant, accounting for 29% of the variance in suicide risk, F (7, 492) = 28.62, p < .001. Although the total relation of recent job loss to suicide risk (including both the direct relation and the indirect relation through perceived burdensomeness, represented in Figure 1 as path c) was significant, the direct relation of recent job loss to suicide risk (i.e., the remainder of the relation not accounted for by the indirect relation through perceived burdensomeness, represented in Figure 1 as c’; Preacher & Hayes, 2008) was not significant. Further, although recent job loss was significantly associated with perceived burdensomeness and perceived burdensomeness was significantly associated with suicide risk in the model, the indirect relation of recent job loss to suicide risk through perceived burdensomeness was not significant (see Figure 1).
Figure 1.
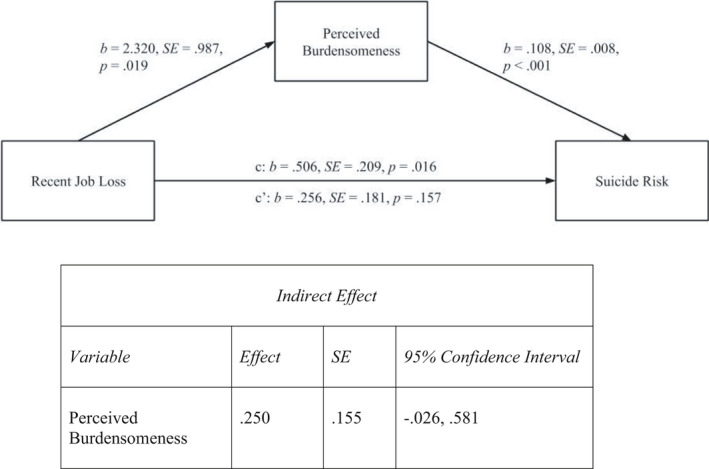
Indirect relation of recent job loss to suicide risk through perceived burdensomeness. Note. Covariates included in the model were age, sex, racial/ethnic background, income, and whether participants lived alone
As for the analysis examining the indirect relation of stay‐at‐home order status to suicide risk through thwarted belongingness and loneliness, the overall model was significant, accounting for 12% of the variance in suicide risk, F (8, 491) = 8.21, p < .001. Of note, although stay‐at‐home order status was significantly uniquely associated with both thwarted belongingness and loneliness, only thwarted belongingness (and not loneliness) was significantly uniquely associated with suicide risk. In addition, results revealed a significant indirect relation of stay‐at‐home order status to suicide risk through thwarted belongingness, but not loneliness (see Figure 2).
Figure 2.
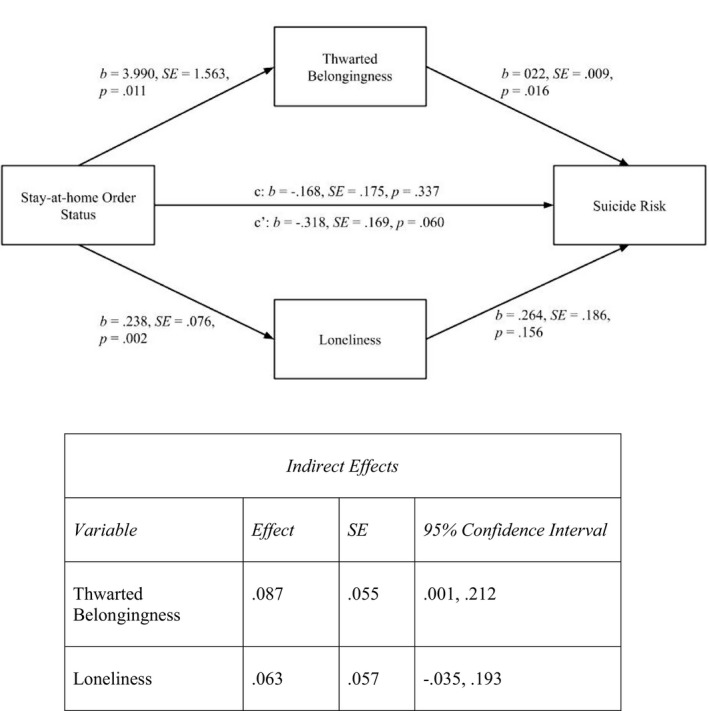
Indirect relations of stay‐at‐home order status to suicide risk through thwarted belongingness and loneliness. Note. Covariates included in the model were age, sex, racial/ethnic background, income, and whether participants lived alone
DISCUSSION
The results of this study provide preliminary empirical support for the theorized relations of COVID‐19–related social and economic consequences to increased suicide risk (Reger et al., 2020). Specifically, the results of this study highlight the differential relevance of thwarted belongingness and perceived burdensomeness to the relations of stay‐at‐home orders and pandemic‐related job loss, respectively, to suicide risk. Providing partial support for study hypotheses, although the presence of a stay‐at‐home order was not significantly associated with greater suicide risk at a zero‐order level, it was indirectly related to suicide risk through greater thwarted belongingness. These findings suggest that any association of stay‐at‐home orders (at least in the short‐term) to suicide risk is due to the association these orders have with increased social disconnection (Reger et al., 2020). Interestingly, although the presence of a stay‐at‐home order was significantly uniquely associated with both loneliness and thwarted belongingness, only thwarted belongingness was uniquely associated with suicide risk and explained the relation of stay‐at‐home order status to suicide risk in this sample. Together, these results suggest that although stay‐at‐home orders may very well increase the potential for loneliness among adults in the United States, it is not loneliness specifically but a broader sense of disconnection and absence of meaningful relationships that accounts for the relation of stay‐at‐home orders to greater suicide risk.
Results of this study also provide partial support for study hypotheses pertaining to the relation of pandemic‐related job loss to suicide risk. Specifically, although recent job loss evidenced a significant zero‐order correlation with suicide risk, it was not uniquely associated with suicide risk when perceived burdensomeness was included in the model. Likewise, results provided no support for an indirect relation of job loss to suicide risk through perceived burdensomeness. These findings are most consistent with a proxy risk factor model (see Kraemer, Stice, Kazdin, Offord, & Kupfer, 2001), suggesting that the total relation of recent job loss to suicide risk is due to their shared association with perceived burdensomeness. Although inconsistent with our hypotheses, these results are not without support in the literature, as there is some evidence to suggest that involuntary job loss in general is not associated with increased suicide risk in the short‐term, outside of mass‐layoff events (see Classen & Dunn, 2012). Instead, evidence suggests that the duration of time spent unemployed following a job loss may be more strongly associated with suicide risk (Classen & Dunn, 2012). Thus, it may be that the strength of the relation of pandemic‐related job loss to suicide risk will increase over time if new employment is not obtained and financial strain continues.
Several limitations warrant consideration. First, the use of cross‐sectional data precludes any conclusions about the precise nature or direction of the associations examined here. In particular, although theory and research suggest that both job loss and social isolation may increase suicide risk (Classen & Dunn, 2012; Oyesanya et al., 2015; Reger et al., 2020), our data cannot rule out the possibility that elevations in suicide risk reported in this study preceded or occurred concurrently with (but unrelated to) these factors. Prospective, longitudinal studies are needed to clarify the extent to which the social and economic consequences of COVID‐19 and related stay‐at‐home orders increase suicide risk, as well as the mechanisms underlying these relations. Another limitation is the exclusive reliance on self‐report questionnaire data, which may be influenced by social desirability biases or recall difficulties. Future research should incorporate structured clinical interviews and/or timeline follow‐back procedures to assess suicide risk and its temporal relation to social distancing and economic difficulties. Likewise, although the use of a diverse nationwide community sample is a strength of this study, the generalizability of our findings to particular at‐risk groups (e.g., hospitalized patients, individuals with chronic medical conditions, health care workers) remains unclear. Future research is needed to examine the relations of COVID‐19 and related social and economic consequences to suicide risk within these vulnerable groups in particular.
Finally, it is important to note that the results of this study speak to only the early associations of stay‐at‐home orders and COVID‐19–related job loss to suicide risk among individuals in the United States. However, it is likely that the consequences and psychological impact of these factors may change over time. For example, and consistent with the proposed mechanisms through which stay‐at‐home orders and other social distancing interventions are thought to increase suicide risk (Reger et al., 2020), the psychological impact and negative consequences of these orders may intensify over time, with suicide risk increasing as the duration of these orders increases. Likewise, research suggests that the duration of unemployment following an involuntary job loss is more strongly associated with suicide risk than the initial job loss (Classen & Dunn, 2012); thus, it is likely that the relation between pandemic‐related job loss and suicide risk may increase over time, particularly in the context of the current economic crisis and ongoing stay‐at‐home and shelter in place orders (which decrease the likelihood of obtaining a new job in the near future). Although research examining the early impact of this pandemic and associated factor on suicide risks is important, it is imperative that research continues to track these relations as the pandemic and related public health interventions persist over time.
Despite these limitations, the results of this study highlight the potential impact of COVID‐19 social and economic consequences on suicide risk among adults in the United States, as well as the relevance of thwarted belongingness and perceived burdensomeness to these associations. These results are consistent with theory and research highlighting the relevance of thwarted belongingness and perceived burdensomeness to suicide risk (e.g., Chu et al., 2017; Van Orden et al., 2010), and suggest that these may be important factors to target in the context of focused interventions aimed at decreasing suicide risk during this time. In the absence of effective COVID‐19 infection prevention efforts and/or pharmacological interventions (e.g., vaccines), large‐scale public health interventions such as social distancing or stay‐at‐home orders are necessary to reduce the spread of the virus and infection‐related mortality. However, in the context of these necessary public health interventions, our results speak to the need to also implement interventions aimed at mitigating the negative psychological consequences of both the social isolation and economic problems that can arise from or be exacerbated by stay‐at‐home orders.
Specifically, our results provide further support for recent suggestions to focus on increasing social connection and connectedness in the context of stay‐at‐home orders and other social distancing interventions, in an effort to offset the isolation, loneliness, and disconnection that may inadvertently accompany these orders (see Reger et al., 2020). Likewise, among individuals who have experienced a job loss during this time, our findings suggest that interventions aimed at decreasing perceived burdensomeness and increasing individuals’ awareness of and connection to their contributions to the lives of others may help to decrease suicide risk among this vulnerable population. Finally, given both theoretical and emerging empirical literature suggesting increased suicide risk during this pandemic, it is important that crisis call centers continue to be funded and staffed to ensure that individuals who may have limited social contacts are able to seek help in emergency situations. Likewise, it is imperative that evidence‐based tele‐mental health services are made available and accessible to vulnerable individuals throughout the duration of stay‐at‐home orders and other social distancing interventions (Reger et al., 2020).
REFERENCES
- Ahmed, F. , Zviedrite, N. , & Uzicanin, A. (2018). Effectiveness of workplace social distancing measures in reducing influenza transmission: A systematic review. BMC Public Health, 18, 518. 10.1186/s12889-018-5446-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buhrmester, M. , Kwang, T. , & Gosling, S. D. (2011). Amazon's Mechanical Turk: A new source of inexpensive, yet high‐quality, data? Perspectives on Psychological Science, 6, 3–5. 10.1177/1745691610393980 [DOI] [PubMed] [Google Scholar]
- Calati, R. , Ferrari, C. , Brittner, M. , Oasi, O. , Olié, E. , Carvalho, A. F. , & Courtet, P. (2019). Suicidal thoughts and behaviors and social isolation: A narrative review of the literature. Journal of Affective Disorders, 245, 653–667. 10.1016/j.jad.2018.11.022 [DOI] [PubMed] [Google Scholar]
- Capron, D. W. , Fitch, K. , Medley, A. , Blagg, C. , Mallott, M. , & Joiner, T. (2012). Role of anxiety sensitivity subfactors in suicidal ideation and suicide attempt history. Depression and Anxiety, 29, 195–201. 10.1002/da.20871 [DOI] [PubMed] [Google Scholar]
- Casler, K. , Bickel, L. , & Hackett, E. (2013). Separate but equal? A comparison of participants and data gathered via Amazon’s MTurk, social media, and face‐to‐face behavioral testing. Computers in Human Behavior, 29, 2156–2160. 10.1016/j.chb.2013.05.009 [DOI] [Google Scholar]
- Centers for Disease Control and Prevention (2020). Coronavirus (COVID‐19). Retrieved from https://www.cdc.gov/coronavirus/2019‐ncov/index.html. [Google Scholar]
- Chandler, J. , Rosenzweig, C. , Moss, A. J. , Robinson, J. , & Litman, L. (2019). Online panels in social science research: Expanding sampling methods beyond Mechanical Turk. Behavior Research Methods, 51, 2022–2038. 10.3758/s13428-019-01273-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang, E. C. , Wan, L. , Li, P. , Guo, Y. , He, J. , Gu, Y. U. , … Hirsch, J. K. (2017). Loneliness and suicidal risk in young adults: Does believing in a changeable future help minimize suicidal risk among the lonely? The Journal of Psychology, 15, 453–463. 10.1080/00223980.2017.1314928 [DOI] [PubMed] [Google Scholar]
- Chen, W. C. , Huang, A. S. , Chuang, J. H. , Chiu, C. C. , & Kuo, H. S. (2011). Social and economic impact of school closure resulting from pandemic influenza A/H1N1. Journal of Infection, 62, 200–203. 10.1016/j.jinf.2011.01.007 [DOI] [PubMed] [Google Scholar]
- Chu, C. , Buchman‐Schmitt, J. M. , Stanley, I. H. , Hom, M. A. , Tucker, R. P. , Hagan, C. R. , … Joiner, T. E. (2017). The interpersonal theory of suicide: A systematic review and meta‐analysis of a decade of cross‐national research. Psychological Bulletin, 143, 1313–1345. 10.1037/bul0000123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Classen, T. J. , & Dunn, R. A. (2012). The effect of job loss and unemployment duration on suicide risk in the United States: A new look using mass‐layoffs and unemployment duration. Health Economics, 21, 338–350. 10.1002/hec.1719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cukrowicz, K. C. , Cheavens, J. S. , Van Orden, K. A. , Ragain, R. M. , & Cook, R. L. (2011). Perceived burdensomeness and suicide ideation in older adults. Psychology and Aging, 26, 331–338. 10.1037/a0021836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danziger, R. (1994). The social impact of HIV/AIDS in developing countries. Social Science & Medicine, 39, 905–917. 10.1016/0277-9536(94)90203-8 [DOI] [PubMed] [Google Scholar]
- Dong, E. , Du, H. , & Gardner, L. (2020). An interactive web‐based dashboard to track COVID‐19 in real time. The Lancet Infectious Diseases, 20(5), 533–534. 10.1016/S1473-3099(20)30120-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flaxman, S. , Mishra, S. , Gandy, A. , Unwin, H. J. T. , Coupland, H. , Mellan, T. , Bhatt, S. (2020). Estimating the number of infections and impact of non‐pharmaceutical interventions on COVID‐19 in 11 European countries. Imperial College COVID‐19 Response Team, London, March 30. 10.25561/77731. [DOI] [Google Scholar]
- Galea, S. , Merchant, R. M. , & Lurie, N. (2020). The mental health consequences of COVID‐19 and physical distancing: The need for prevention and early intervention. Journal of the American Medical Association: Internal Medicine, 180(6), 817. 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- Gasparini, R. , Amicizia, D. , Lai, P. L. , & Panatto, D. (2012). Clinical and socioeconomic impact of seasonal and pandemic influenza in adults and the elderly. Special Focus Review, 8, 21–28. 10.4161/hv.8.1.17622 [DOI] [PubMed] [Google Scholar]
- Hallensleben, N. , Spangenberg, L. , Kapusta, N. D. , Forkmann, T. , & Glaesmer, H. (2016). The German version of the Interpersonal Needs Questionnaire (INQ)–Dimensionality, psychometric properties and population‐based norms. Journal of Affective Disorders, 195, 191–198. 10.1016/j.jad.2016.01.045 [DOI] [PubMed] [Google Scholar]
- Hauser, D. J. , & Schwarz, N. (2016). Attentive Turkers: MTurk participants perform better on online attention checks than do subject pool participants. Behavior Research Methods, 48, 400–407. 10.3758/s13428-015-0578-z [DOI] [PubMed] [Google Scholar]
- Hayes, A. F. (2017). Introduction to mediation, moderation, and conditional process analysis: A regression‐based approach. New York, NY: Guilford Press. [Google Scholar]
- Hill, R. M. , Rey, Y. , Marin, C. E. , Sharp, C. , Green, K. L. , & Pettit, J. W. (2015). Evaluating the Interpersonal Needs Questionnaire: Comparison of the reliability, factor structure, and predictive validity across five versions. Suicide and Life‐Threatening Behavior, 45, 302–314. 10.1111/sltb.12129 [DOI] [PubMed] [Google Scholar]
- Jackson, C. , Mangtani, P. , Hawker, J. , Olowokure, B. , & Vynnycky, E. (2014). The effects of school closures on influenza outbreaks and pandemics: Systematic review of simulation studies. PLoS One, 9, e97297. 10.1371/journal.pone.0097297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joiner, T. E. Jr , Pfaff, J. J. , & Acres, J. G. (2002). A brief screening tool for suicidal symptoms in adolescents and young adults in general health settings: Reliability and validity data from the Australian National General Practice Youth Suicide Prevention Project. Behaviour Research and Therapy, 40, 471–481. [DOI] [PubMed] [Google Scholar]
- Joiner, T. A. , Ribeiro, J. D. , & Silva, C. (2012). Nonsuicidal self‐injury, suicidal behavior, and their co‐occurrence as viewed through the lens of the interpersonal theory of suicide. Current Directions in Psychological Science, 21, 342–347. 10.1177/0963721412454873 [DOI] [Google Scholar]
- Kennedy, R. , Clifford, S. , Burleigh, T. , Jewell, R. , & Waggoner, P. (2018). The Shape of and Solutions to the MTurk Quality Crisis. 10.2139/ssrn.3272468 [DOI]
- Kraemer, H. C. , Stice, E. , Kazdin, A. , Offord, D. , & Kupfer, D. (2001). How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. American Journal of Psychiatry, 158, 848–856. 10.1176/appi.ajp.158.6.848 [DOI] [PubMed] [Google Scholar]
- Li, W. , Dorstyn, D. S. , & Jarmon, E. (2020). Identifying suicide risk among college students: A systematic review. Death Studies, 44(7), 450–458. 10.1080/07481187.2019.1578305. [DOI] [PubMed] [Google Scholar]
- Linton, N. M. , Kobayashi, T. , Yang, Y. , Hayashi, K. , Akhmetzhanov, A. R. , Jung, S.‐M. , … Nishiura, H. (2020). Incubation period and other epidemiological characteristics of 2019 novel coronavirus infections with right truncation: A statistical analysis of publicly available case data. Journal of Clinical Medicine, 9, 538. 10.3390/jcm9020538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu, R. , Zhao, X. , Li, J. , Niu, P. , Yang, B. O. , Wu, H. , … Tan, W. (2020). Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. The Lancet, 395, 565–574. 10.1016/S0140-6736(20)30251-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marty, M. A. , Segal, D. L. , Coolidge, F. L. , & Klebe, K. J. (2012). Analysis of the psychometric properties of the Interpersonal Needs Questionnaire (INQ) among community‐dwelling older adults. Journal of Clinical Psychology, 68, 1008–1018. 10.1002/jclp.21877 [DOI] [PubMed] [Google Scholar]
- Meltzer, M. I. , Cox, N. J. , & Fukuda, K. (1999). The economic impact of pandemic influenza in the United States: Priorities for intervention. Emerging Infectious Disease, 5, 659–671. 10.3201/eid0505.990507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mervosh, S. , Lu, D. , & Swales, V. (2020, April 7). See which states and cities have told residents to stay at home. The New York Times. Retrieved from https://www.nytimes.com/interactive/2020/us/coronavirus‐stay‐at‐home‐order.html.
- Metalsky, G. I. , & Joiner, T. E. (1997). The hopelessness depression symptom questionnaire. Cognitive Therapy and Research, 21, 359–384. [Google Scholar]
- Milner, A. , Page, A. , Morrell, S. , Hobbs, C. , Carter, G. , Dudley, M. , … Taylor, R. (2014). The effects of involuntary job loss on suicide and suicide attempts among young adults: Evidence from a matched case‐control study. Australian & New Zealand Journal of Psychiatry, 48, 333–340. 10.1177/0004867414521502 [DOI] [PubMed] [Google Scholar]
- Montemurro, N. (2020). The emotional impact of COVID‐19: From medical staff to common people. Brain, Behavior, and Immunity, 19, 23–24. 10.1016/j.bbi.2020.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oyesanya, M. , Lopez‐Morinigo, J. , & Dutta, R. (2015). Systematic review of suicide in economic recession. World Journal of Psychiatry, 5, 243–254. 10.5498/wjp.v5.i2.243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher, K. J. , & Hayes, A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40, 879–891. 10.3758/BRM.40.3.879 [DOI] [PubMed] [Google Scholar]
- Qualls, N. , Levitt, A. , Kanade, N. , Wright‐Jegede, N. , Dopson, S. , Biggerstaff, M. , … Reed, C. (2017). Community mitigation guidelines to prevent pandemic influenza – United States, 2017. Morbidity & Mortality Weekly Report Recommendations & Reports, 66, 1–34. 10.15585/mmwr.rr6601a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reger, M. A. , Stanley, I. H. , & Joiner, T. E. (2020). Suicide mortality and coronavirus disease 2019 – A perfect storm? JAMA Psychiatry, published online April 10, 2020. doi: 10.1001/jamapsychiatry.2020.1060. [DOI] [PubMed] [Google Scholar]
- Russell, D. W. (1996). UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. Journal of Personality Assessment, 66, 20–40. 10.1207/s15327752jpa6601_2 [DOI] [PubMed] [Google Scholar]
- Russell, D. , Peplau, L. A. , & Cutrona, C. E. (1980). The revised UCLA Loneliness Scale: Concurrent and discriminant validity evidence. Journal of Personality and Social Psychology, 39, 472–480. 10.1037/0022-3514.39.3.472 [DOI] [PubMed] [Google Scholar]
- Shereen, M. A. , Khan, S. , Kazmi, A. , Bashir, N. , & Siddique, B. (2020). COVID‐19 infection: Origin, transmission, and characteristics of human coronaviruses. Journal of Advances Research, 24, 91–98. 10.1016/j.jare.2020.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrestha, S. S. , Swerdlow, D. L. , Borse, R. H. , Prabhu, V. S. , Finelli, L. , Atkins, C. Y. , … Meltzer, M. I. (2011). Estimating the burden of 2009 pandemic influenza A (H1N1) in the United States (April 2009‐April 2010). Clinical Infectious Diseases, 52, S75–S82. 10.1093/cid/ciq012 [DOI] [PubMed] [Google Scholar]
- Stickley, A. , & Koyanagi, A. (2016). Loneliness, common mental disorders and suicidal behavior: Findings from a general population survey. Journal of Affective Disorders, 197, 81–87. 10.1016/j.jad.2016.02.054 [DOI] [PubMed] [Google Scholar]
- Stravynski, A. , & Boyer, R. (2001). Loneliness in relation to suicide ideation and parasuicide: A population‐wide study. Suicide and Life‐Threatening Behavior, 31, 32–40. 10.1521/suli.31.1.32.21312 [DOI] [PubMed] [Google Scholar]
- Szucs, T. (1999). The socio‐economic burden of influenza. Journal of Antimicrobial Chemotherapy, 44, 11–15. 10.1093/jac/44.suppl_2.11 [DOI] [PubMed] [Google Scholar]
- Thakkar, N. , Burstein, R. , Hu, H. , Selvajar, P. , & Klein, D. (2020). Social distancing and mobility reductions have reduced COVID‐19 transmission in King County, WA. Report prepared by Institute for Disease Modeling. Published online March 29, 2020. Retrieved from https://covid.idmod.org/data/Social_distancing_mobility_reductions_reduced_COVID_Seattle.pdf.
- Thunström, L. , Newbold, S. C. , Finnoff, D. , Ashworth, M. , & Shogren J. F. (2020). The benefits and costs of using social distancing to flatten the curve for COVID‐19. Journal of Benefit‐Cost Analysis, 1–17. 10.1017/bca.2020.12 [DOI] [Google Scholar]
- Van Orden, K. A. , Cukrowicz, K. C. , Witte, T. K. , & Joiner, T. E. (2012). Thwarted belongingness and perceived burdensomeness: Construct validity and psychometric properties of the Interpersonal Needs Questionnaire. Psychological Assessment, 24, 197–215. 10.1037/a0025358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden, K. A. , Witte, T. K. , Cukrowicz, K. C. , Braithwaite, S. , Selby, E. A. , & Joiner, T. E. (2010). The interpersonal theory of suicide. Psychology and Aging, 117, 575–600. 10.1037/a0018697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, C. , Pan, R. , Wan, X. , Tan, Y. , Xu, L. , Ho, C. S. , & Ho, R. C. (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID‐19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17, 1729. 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2020). Rolling updates on coronavirus disease (COVID‐19). Retrieved from https://www.who.int/emergencies/diseases/novel‐coronavirus‐2019/events‐as‐they‐happen. [Google Scholar]
- Zhou, P. , Yang, X.‐L. , Wang, X.‐G. , Hu, B. , Zhang, L. , Zhang, W. , … Shi, Z.‐L. (2020). A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature, 579(7798), 270–273. 10.1038/s41586-020-2012-7 [DOI] [PMC free article] [PubMed] [Google Scholar]


