Dear Edi__tor,
Reports on COVID‐19 in children are limited. Despite new data emerging, and understanding of the disease improves rapidly, there are as yet several features and complications related to the disease that remain unknown. Herein, we report the first case of a child with chilblains and retinal vasculitis related to COVID‐19.
An 11‐year‐old patient arrived at the Dermatology Emergency Department with a 2‐week history of asymptomatic plaques on his toes. He did not complain of fever, respiratory symptoms (as cough or dyspnoea), headache, malaise, sore throat, nasal congestion or diarrhoea. He had no history of family exposure, and he was taking strict social distancing measures due to the Spanish Government restrictions applied on 13 March 2020. Physical examination showed oedematous and erythematous to violaceous plaques on the dorsal toes of both feet (Fig. 1). These lesions were clinically compatible with chilblains. A nasopharyngeal sample was obtained, and a reverse transcription polymerase chain reaction (RT‐PCR) was negative for SARS‐CoV‐2. Serologic tests (both immunochromatographic and chemiluminescence immunoassay) showed negative SARS‐CoV‐2 IgM with positive IgG antibodies. Complementary studies, including autoimmune panel (rheumatoid factor, lupus anticoagulant, antinuclear, antineutrophil cytoplasmic, anti‐Ro/SSA, anti‐La/SSB and anticardiolipin antibodies), serum proteinogram, C‐reactive protein, coagulation studies, cryoglobulins and D‐dimer were normal. Other common viral infections were ruled out by laboratory investigation.
Figure 1.

Erythematous to violaceous plaques on the dorsal toes of both feet compatible with chilblains.
Due to known potential thromboembolic complications related to COVID‐19, the patient was referred to the Ophthalmology Department, despite being visually asymptomatic and not reporting any ocular complaint. An ophthalmologic examination was performed: his visual acuity was 1 in both eyes, and the pupils were reactive and symmetric. The slit lamp examination showed no pathological findings. An examination of the ocular fundus showed retinal vasculitis located on the equator of the left eye, as well as one perivascular infiltrate as well and extended retinal exudates (Fig. 2a,b). The vitreous was clear, and the macular structure was preserved on the optical tomography image. No retinal inflammation was found in the right eye. These findings were compatible with retinal vasculitis.
Figure 2.
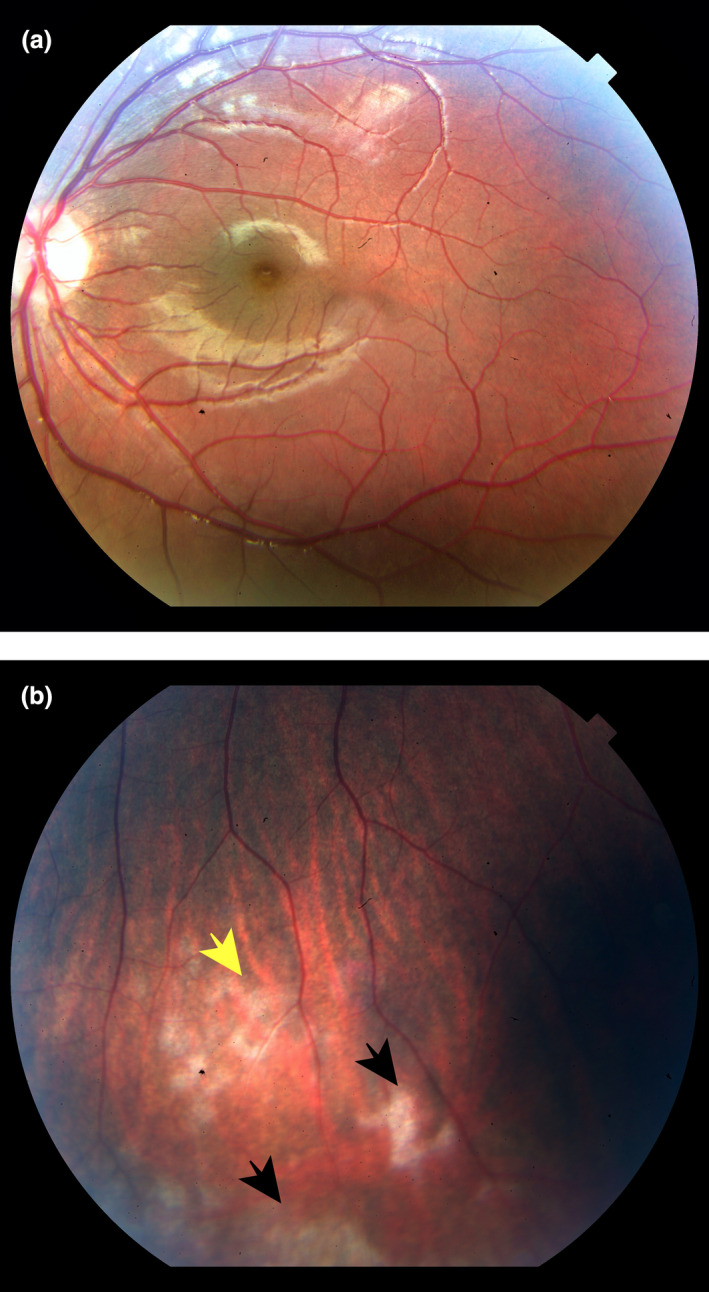
Funduscopic examination. The image does not show significant pathologic features on right eye (a). Retinal vasculitis with perivascular infiltrate (yellow arrow) and retinal exudates (black arrows) on retinal equator of left eye (b).
Several studies have reviewed the symptoms and characteristics of children with COVID‐19. Most authors have concluded that the disease course in paediatric patients is milder than that in adults and that they have a better prognosis. One of the largest studies 1 suggested that more than 90% of paediatric cases with microbiological confirmation in their case series (n = 2143) had asymptomatic, mild or moderate disease. Respiratory, constitutional and gastrointestinal symptoms do not differ much from symptoms observed in adults with mild disease.
Concerning ocular manifestations, to the best of our knowledge, this is the first case report of retinal vasculitis in a patient with SARS‐CoV‐2 infection. As far as we know, COVID‐19 ocular manifestations remain unclear, with acute conjunctivitis the most frequent. 2 , 3
Regarding cutaneous manifestations, a recent outbreak of chilblains in patients has been associated with COVID‐19 infection. These lesions typically occur in asymptomatic and healthy children and young adults. In these patients, chilblains mainly affect the feet, although they can also appear on the hands. Dorsal toes are the most frequently affected, and lesions are described as rounded, well‐circumscribed erythematous to violaceous plaques or nodules. They can sometimes become bullous. Most of these lesions are asymptomatic; however, some patients have reported pain or pruritus. We suspected these chilblains could be related to COVID‐19 because they had arisen along with warm springtime and in clusters during this COVID‐19 pandemic.
Chilblains might be the only symptom in these patients. Fever, cough and malaise can be absent. Due to the microbiologic results observed in some of these patients (RT‐PCR negative and IgG+), we can presume that these type of symptoms occurs in a convalescent and non‐infectious phase of the disease. In contrast with our patient, there have also been reports of patients with coronavirus infection presenting chilblains in the acute phase of the disease. 4 Further investigations and prospective studies are needed to confirm this hypothesis. Meanwhile, dermatologists and other physicians must be alerted to these clinical presentations of COVID‐19 infection. These patients need to be immediately tested and isolated to prevent transmission until we can explain the nature of these findings.
To date, the pathogenic origin of these types of lesions remains unknown. Due to the clinical and histopathological similarities to chilblains in lupus erythematosus (LE), some authors have mentioned an autoimmune pathogenic mechanism of these COVID‐19 features. Some studies in the literature have sustained this autoimmune theory. Recently, a case series of Guillain–Barré Syndrome associated with SARS‐CoV‐2 infection strengthens the link between COVID‐19 and autoimmunity. 5 Another possible pathogenic mechanism related to these features is the type I interferon (IFN‐I) response to coronavirus infection. This type I IFN response is observed in other viral infections, in LE, and in some auto‐inflammatory interferonopathies. Among these syndromes, we would like to highlight Aicardi–Goutières syndrome, STING‐associated vasculopathy with onset in infancy, familial chilblain lupus, retinal vasculopathy with cerebral leukodystrophy and overlap related syndromes. All share the same pathogenic pathway and some clinical manifestations, including chilblains and retinal vasculopathy. In addition, this type I IFN response produces microvascular injury, 6 which has already been reported to be related to COVID‐19 infection, and it could explain both chilblains and retinal vasculitis. Also, Kawasaki disease can share some similarities with COVID‐19 infection. Both cause acral skin lesions, vasculitis and show increased serum interleukin 6 (IL‐6) related to the immune response to the disease. 7 Also, there are other viral infections associated with Kawasaki disease, including other species of human coronaviruses. 8
Other types of acral cutaneous lesions apart from chilblains have been reported in patients with COVID‐19. This group includes cyanosis, blisters and gangrene in the feet and hands, primarily in adults. Nonetheless, these types of manifestations appear to be related to coagulation disorders in severe cases of COVID‐19, and most carry poor prognosis. 9 Our analytical study was rigorously normal, with no poor prognostic data.
In summary, special attention should be devoted to children, despite most remaining asymptomatic in the early stages of the infection. Currently, we do not know whether there will be any other complications in the late stages of the disease and what is the real meaning of the described features. However, these types of manifestations in children appear to occur in the convalescence phase of the infection. Further studies are needed to provide more specific preventive measures and to standardize the short‐ and middle‐term follow‐up of these patients.
Conflict of interest
The other authors have no conflicts of interest to disclose.
Funding source
No funding was secured for this study.
Financial disclosure
All of the authors that appear and have contributed to this article have not any financial relationship relevant to this article to disclose.
Author contributions
Drs Quintana‐Castanedo Feito‐Rodríguez and Mayor‐Ibarguren conceptualized and designed the study, coordinated and drafted the initial manuscript, and reviewed and revised the manuscript. Drs Fernández‐Alcalde, Granados‐Fernández, Montero‐Vega and de Lucas‐Laguna designed the data collection instruments, collected data, carried out the initial analyses, and reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
The patient in this manuscript has given written informed consent to publication of their case details.
References
- 1. Epidemiological Characteristics of 2143 Pediatric Patients With 2019 Coronavirus Disease in China ‐ Search Results. URL https://pubmed.ncbi.nlm.nih.gov/?term=Epidemiological+Characteristics+of+2143+Pediatric+Patients+With+2019+Coronavirus+Disease+in+China. (last accessed: 20 April 2020).
- 2. Ocular manifestations of a hospitalised patient with confirmed 2019 novel coronavirus disease. URL https://www.ncbi.nlm.nih.gov/pubmed/32265202. (last accessed: 22 April 2020). [DOI] [PMC free article] [PubMed]
- 3. Cheema M, Aghazadeh H, Nazarali S et al. Keratoconjunctivitis as the initial medical presentation of the novel coronavirus disease 2019 (COVID‐19). Can J Ophthalmol 2020; 1–5. [Epub ahead of print] 10.1016/j.jcjo.2020.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kolivras A, Dehavay F, Delplace D et al. Coronavirus (COVID‐19) infection‐induced chilblains: a case report with histopathological findings. JAAD Case Rep 2020. 10.1016/j.jdcr.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Toscano G, Palmerini F, Ravaglia S et al. Guillain‐Barré syndrome associated with SARS‐CoV‐2. N Engl J Med 2020; 382: 2574–2576. 10.1056/NEJMc2009191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Magro C, Mulvey JJ, Berlin D et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID‐19 infection: a report of five cases. Transl Res 2020; 220: 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gomez‐Moyano E, Casaño AV, Camacho J, Trelles AS, Crespo‐Erchiga V. Kawasaki disease complicated by cutaneous vasculitis and peripheral gangrene. J Am Acad Dermatol 2011; 64: e74–e75. [DOI] [PubMed] [Google Scholar]
- 8. Turnier JL, Anderson MS, Heizer HR, Jone P‐N, Glodé MP, Dominguez SR. Concurrent respiratory viruses and Kawasaki disease. Pediatrics 2015; 136: e609–e614. [DOI] [PubMed] [Google Scholar]
- 9. Zhang Y, Cao W, Xiao M et al. Clinical and coagulation characteristics of 7 patients with critical COVID‐2019 pneumonia and acro‐ischemia. Zhonghua Xue Ye Xue Za Zhi 2020; 41: E006. [DOI] [PubMed] [Google Scholar]


