Abstract
BACKGROUND/OBJECTIVES
Coronavirus disease 2019 (COVID‐19) has pushed many geriatric healthcare providers to attempt video visits for the first time. Although the Veterans Health Administration (VA) is a pioneer in telemedicine, rapid shifts to nearly exclusive use of telehealth for healthcare delivery and changes regarding trainee engagement in telehealth served as the impetus for rapidly assessing telehealth training needs.
DESIGN
National needs assessment (online survey) of associated health trainees and medical fellows affiliated with Geriatric Research Education and Clinical Centers (GRECCs).
SETTING
National GRECC network ‐‐ 20 VA centers of excellence focused on supporting Veterans as they age. Each GRECC is affiliated with a school of medicine at a major university.
PARTICIPANTS
Trainees (n = 89) representing 12 disciplines.
RESULTS
Two‐thirds of participants had received some telehealth training. However, most had never done a video‐to‐home visit, and, regardless of telehealth experience, they reported low confidence. Based on open‐ended questions exploring training needs, educational resources were rapidly developed and disseminated.
INTERVENTION
Within 1 week of the assessment, a nuts‐and‐bolts guide regarding remote access, technology requirements, video‐conferencing platforms, and managing emergencies was sent to the national network of GRECC associate directors for education for dissemination among discipline‐specific training directors at their sites. This resource was subsequently submitted to the national VA COVID Strong Practices SharePoint site. An interdisciplinary team of geriatric specialists with extensive video‐to‐home experience also organized a national webinar that peaked at just over 700 participants. GRECC Connect, a network of geriatric specialty teams funded to improve care access for rural older veterans using telehealth and associated health training programs at each GRECC facilitated rapid development and dissemination of both resources.
CONCLUSION
We quickly identified and responded to telehealth training needs of geriatrics trainees to optimize care for rural older adults as part of a rapid response to COVID‐19. Although the webinar and nuts‐and‐bolts resources were developed within the VA context, they have demonstrated high demand and broader applicability. Results should continue to inform curriculum development efforts to address telehealth training gaps within and outside the VA.
Keywords: COVID‐19, telehealth, video‐to‐home visits, training, GRECC
The coronavirus disease 2019 (COVID‐19) pandemic has forced the U.S. healthcare system suddenly and dramatically to change how care is delivered. Elective procedures have been postponed, intensive care capacity has been increased, and clinicians have been encouraged to convert as many outpatient visits as possible to telephone or video‐to‐home formats. Clinical trainees, an important component of many hospital workforces, have been asked to adapt to these changes.
The COVID‐19 pandemic has exacerbated the challenges that many older patients face in having access to appropriate care. Clinicians with geriatric specialty training are a scarce resource and generally concentrated in urban medical centers. Given that older patients are at highest risk of poor outcomes with COVID‐19 infection, it is imperative that we optimize the care provided remotely for this population. To increase access to care for rural older patients and others for whom a trip to the clinic is challenging, we need to train the next generation of geriatric specialists to use these technological tools effectively with an older population with possible limitations that challenge their ability to use these tools.
Most of today's trainees would be considered digital natives, but it is unclear how well prepared they are to pivot to providing care through telehealth modalities. Geriatric Research Education and Clinical Center (GRECC) Connect, an initiative funded by the Veterans Health Administration (VA) Office of Rural Health that expands access to geriatric specialty care for rural older veterans via telehealth services and education for rural clinicians via national webinars on aging‐related topics1, 2 sought to rapidly assess telehealth training gaps near the onset of the COVID‐19 crisis. Specifically, we surveyed trainees affiliated with VA geriatric centers of excellence. This article presents the results of the rapid assessment and two educational resources developed in response (Figure 1).
Figure 1.
Visual abstract depicting the capacity of the Geriatric Research Education and Clinical Center (GRECC) Connect network to respond to the COVID‐19 crisis.
VA and GRECC as Clinical Education Leaders
The VA provides more geriatric training of healthcare professionals than any other entity nationally, 3 , 4 with its 20 GRECCs serving as leaders in geriatric‐specific interprofessional education. GRECCs are centers of excellence established by Congress in 1975 to improve the health of older veterans. 5 They have three main missions: (1) to build new knowledge through aging‐related research, (2) to improve health care through the development of new clinical programs in geriatric specialty care, and (3) to ensure that VA trainees and staff are educated about aging‐related issues. 6 Each GRECC is affiliated with a major academic medical center and has an associated health training program that collectively trains more than 800 trainees (interns, externs, residents, and fellows) annually across 15 different disciplines. 7
GRECC Connect: Using Telehealth to Serve Rural Older Veterans
Recognizing that a higher percentage of veterans in rural areas are older, have multiple chronic conditions, 8 and select the VA for their health care, 9 the VA Office of Rural Health leveraged the capacity of the GRECC network to launch GRECC Connect in 2014. Given extremely limited geriatric resources both within and outside the VA in rural areas, 10 GRECC Connect uses video telehealth and electronic consultation mechanisms to increase access to geriatric specialty care to rural patients. Each of the 15 GRECC Connect hubs supports older veterans in rural areas by providing care through affiliated satellite outpatient clinics and to veterans' homes using a variety of telehealth modalities. 1 , 2 , 11
GRECC Connect: Existing Geriatric Care Infrastructure and Capacity for Rapid Response to COVID‐19
GRECC Connect engages interprofessional teams, often including geriatricians, nursing professionals, social workers, pharmacists, psychologists (gero‐ and neuro‐psychologists), and rehabilitation practitioners, as well as administrative support professionals (e.g., telehealth technicians and schedulers). 2 GRECC Connect teams typically integrate medical (e.g., geriatric medicine fellows) and associated health trainees (e.g., pharmacy and optometry). Consequently, some trainees receive unique opportunities for competency‐based training in telehealth, modeled by geriatric specialists experienced in telehealth.
However, access to telehealth training varies across the VA system, even among the 20 GRECCs. For those sites with a geriatrics team experienced in using telehealth modalities, such as those affiliated with a GRECC Connect hub, there is variability regarding the extent to which they deliver formal telehealth training. Furthermore, most geriatric video telehealth services have been delivered via “clinical video telehealth,” in which a veteran at a satellite outpatient clinic has a video visit with a geriatric specialty care provider or team based at a VA medical center. Therefore, trainees' exposure to telehealth may not have included video‐to‐home visits. These considerations served as the impetus for conducting a rapid assessment of GRECC‐supported trainees' telehealth training needs and dissemination of responsive resources through GRECC Connect. This article highlights the training needs identified through our rapid assessment and resulting educational products to support the unprecedented shift from in‐person to video‐to‐home visits.
METHODS
Survey Instrument
To assess telehealth training needs systematically across the 20 GRECCs, we (L.M., K.N., M.G., and J.M.) developed a brief web‐based needs assessment using XM Qualtrics software. The intent of the survey was quality improvement and educational program development rather than research. Accordingly, we designed the anonymous survey to assess trainees' prior telehealth training experiences, experience conducting video‐to‐home visits, degree of comfort or confidence conducting a video‐to‐home visit, perceptions regarding the importance of video‐to‐home visits as part of the COVID‐19 response and to their future practice, and training needs.
We also collected two respondent demographics: clinical discipline and stage of training. On March 24, 2020, members of the GRECC Connect Education Core (K.N. and L.M.) reached out to the 20 GRECC associate directors for education and evaluation asking that they forward the rapid assessment (GRECC Telehealth Training Needs Assessment) to their associated health trainees and other fellows (e.g., geriatric medicine and GRECC advanced research fellows) who participate in core didactics and clinical rotations as part of interprofessional training. We also asked that they report to us the total number of trainees/fellows to whom they forwarded the survey so we could have an accurate indication of the reach and denominator for calculating the survey response rate.
The GRECC Connect Education Core discussed the results of the rapid assessment on April 2, 2020. Together, we made decisions regarding what resources to develop and disseminate through GRECC educational leaders in direct response to the findings. We disseminated one resource that addressed trainee needs immediately via e‐mail on April 6, 2020. We also planned a national webinar, featuring a multidisciplinary panel experienced in geriatric specialty care and the nuanced application of telehealth modalities for geriatric populations, scheduled for May 7, 2020.
Results of Rapid Assessment
Data collected within 10 days of the initial outreach to associate directors are reported here. Thirteen of 20 GRECCs reported forwarding the survey to a total of 89 medical and associated health trainees including 70 associated health trainees, 15 medicine fellows, and 4 advanced research fellows. Of these 89 trainees, 66 completed the survey (74% response rate). Most respondents were residents and fellows (46% and 32%, respectively). Respondents represented 12 disciplines (Figure 2). Nearly two‐thirds (63% [n = 41]) reported that they had received telehealth training. Of those who had received telehealth training, most had received this training through the VA, with web‐based Talent Management System asynchronous learning modules (n = 17) and in‐person GRECC training (n = 9) the most common.
Figure 2.
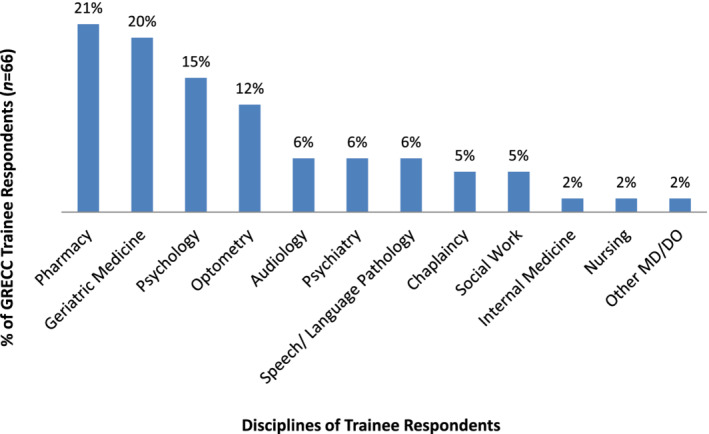
Overview of the various disciplines among the Geriatric Research Education and Clinical Center (GRECC) trainee respondents to the web‐based needs assessment. Other = Psychiatry and Palliative Care [written in response]. MD, medical doctor, DO, doctor of osteopathic medicine.
The survey asked respondents whether they had ever done a medical video visit into the home of a patient. More than one‐half (56%) said no. More than one‐third (36%) indicated they had experience conducting video‐to‐home visits before COVID‐19. Only 8% indicated that they had only done video visits into the home in direct response to COVID‐19.
We asked how comfortable the respondent felt (or would feel) doing video visits into the home of a patient. On average, those with prior experience reported a higher level of comfort compared with those with no experience (M = 4.75 compared with 3.54, respectively, on a 7‐point scale). Further, comfort level among those with no experience was more variable, spanning the entire scale (Figure 3).
Figure 3.
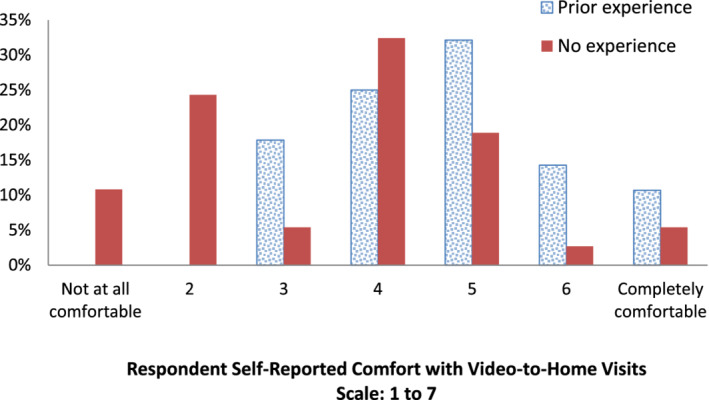
Survey responses from Geriatric Research Education and Clinical Center (GRECC) trainees related to their comfort level conducting video visits, comparing trainees with and without prior experience.
Regardless of experience, we designed the survey to probe further regarding desired training or resources if the respondent rated their level of comfort 1 (not at all comfortable) to 4. Thematic analysis of open‐ended responses surfaced important differences in perspectives between those with or without experience. Specifically, of those with experience and relatively low comfort delivering video visits to home (n = 9), five noted that in‐person training with a supervisor/preceptor would be valuable. One respondent wrote, “I think it would be helpful to have practice simulation with ‘patients’ in order to practice how to connect, use resources during the visit, and to practice documentation.” In contrast, those with no experience and relatively low comfort (n = 21) tended to indicate a desire for training and resources that focused on nuts‐and bolts issues, such as equipment/software, establishing the necessary infrastructure to do video visits from home, and how to address issues such as scheduling and billing. Comments pertaining to equipment and software included requests for “in‐person trainings showing how to log in and set up the telehealth session with a mock patient” and “types of requirements (equipment/software) for home office setup.”
Nearly two‐thirds (65% [n = 43]) of all respondents expressed that video‐to‐home visits were an extremely important part of the COVID‐19 response (M = 6.14 on a 7‐point scale; range = 3–7). However, when asked how likely they were to incorporate video visits into their future practice, only 35% (n = 23) indicated “extremely likely” (M = 5.26 on a 7‐point scale; range = 1–7).
Educational Resources to Meet Telehealth Training Needs during COVID‐19
In response to the identified gaps in knowledge, we leveraged the existing training and clinical capacity of GRECC Connect to rapidly develop and deploy two resources to enhance telehealth capabilities and optimize the provision of geriatric specialty care for older adults through video visits. These resources were (1) a pragmatic educational resource that addressed the nuts‐and‐bolts logistics of providing medical video visits from a trainee's home to a veteran's home, and (2) a nationally broadcast webinar focused on practical tips for delivering telehealth to rural older adults, targeting an interdisciplinary audience. Each of these products is described in detail here.
Instructing Trainees Regarding Establishing Telehealth Capabilities
The VA has been a pioneer in developing telehealth programs and, because of its licensure requirements, has long allowed many disciplines to practice across state lines. In response to COVID‐19, the VA made changes to telehealth policies including some specific to clinical training. For example, supervising clinicians are no longer required to be physically co‐located with trainees during telehealth encounters. These changes, along with guidance that many trainees work remotely (e.g., from their homes rather than from a medical center), likely influenced the needs that surfaced in the rapid assessment and led us to develop a brief nuts‐and‐bolts video‐to‐home educational resource tailored for medical and associated health trainees.
Starting with a 69‐slide educational presentation prepared by the VA Office of Connected Care and the VA Office of Mental Health & Suicide Prevention, GRECC Connect team members from the Bedford VA Medical Center (L.M., J.M., and M.G.) modified content specifically to assist trainees. Specific topics included how to access required VA‐specific web‐based telehealth trainings from home, how to access the VA network from home, technology requirements, how to conduct prescheduled versus unscheduled visits, alternative (non‐VA hosted) video‐conferencing platforms, and instructions for handling emergencies. This resource highlighted requirements for conducting video visits from the trainee's home rather than from VA clinical space.
The resultant 28‐slide educational presentation was beta tested by two medical doctor trainees and their feedback incorporated. The final presentation was shared with GRECC educational directors, inviting them to distribute it to trainees. This comprehensive resource, directed particularly to those trainees without prior telehealth experience, reached 20 VA medical centers with large academic trainee populations within 10 days of the rapid assessment. We subsequently submitted the resource to the VA for consideration as a COVID strong practice for inclusion on the associated SharePoint site accessible to all VA employees. For those outside the VA, an excerpt of this nuts‐and‐bolts resource, which may be used as a model for other healthcare systems, is available through the GRECC Connect website, https://www.gerischolars.org/mod/page/view.php?id=1508.
Interprofessional Team Training Webinar
The GRECC Connect education subcommittee (including all authors and led by H.L.) simultaneously began organizing a national webinar: “Practical Tips for Telehealth for Older Rural Adults.” The webinar was designed to feature a series of brief high‐yield presentations focused on how to assess whether the older veteran's needs can be served more effectively via telephone or a video visit; prepare older veterans for successful telehealth visits; adapt telehealth visits to meet older adult functional needs; conduct medication reconciliation and brief cognitive assessments via telehealth; engage caregivers via telehealth; and identify and address social isolation. In addition to brief didactics, the webinar included a question‐and‐answer session with a panel involving all speakers (five of the seven speakers were H.L., W.H., S.D., M.G., and L.M.). The interdisciplinary nature of the webinar, with speakers representing geriatrics, occupational therapy, geropsychology, behavioral neurology, and geriatric psychiatry, helped address the needs of a broad range of clinical trainees and practitioners and allowed us to offer continuing education credits to a range of disciplines.
GRECC Connect's existing monthly webinar infrastructure and network of experts with as many as 7 years of experience providing geriatric care via video‐to‐home visits enabled us to offer this programming within weeks of the rapid assessment. Although monthly GRECC Connect webinars routinely reach more than 100 attendees, our capacity capped with 300 VA and non‐VA clinicians pre‐enrolling in this webinar within 24 hours of it being announced. Actual attendance peaked at just over 700 participants. The demand for this webinar, within and outside of the VA, underscores the need for such education in the face of COVID‐19. The recorded webinar and Q&A transcript are available on the GRECC Connect website, https://www.gerischolars.org/mod/page/view.php?id=1508. The direct link to the webinar is https://va-eerc-ees.adobeconnect.com/_a1089657440/pbko0s5zyz3s.
DISCUSSION
In this unprecedented time of rapid changes to our healthcare delivery systems, providers are being asked to shift from in‐person to video‐to‐home visits to reduce the spread of COVID‐19. Further, we anticipate that the rapid push to video visits will change the landscape of future care, even as the crisis abates. Clinical trainees across multiple disciplines are an important part of this shift because they are also being asked to help with patient care via video visits. Yet many of them may not have received telehealth training previously and/or may not have received sufficient training in the nuances involved in providing geriatric specialty care through telehealth modalities. The responses of geriatrics trainees to our rapid assessment demonstrate that they need both nuts‐and‐bolts technical instruction as well as clinical guidance regarding how to conduct video visits with older patients. This article described the GRECC Connect network's rapid response to the telehealth training needs of its affiliated interprofessional trainees, as well as nonaffiliated trainees and clinicians in the VA and beyond.
The nuts‐and‐bolts resource we were able to develop and disseminate offers guidance specific to the VA with its particular regulations and video‐conferencing platform, but the need for similar detailed instruction is likely universal. Although details about documentation requirements and precisely which websites to visit are clinically not the most important aspect of these encounters, trainees and clinicians new to video telehealth can be particularly anxious about these details. Being less anxious about the mechanics of conducting a video‐to‐home visit can help trainees and other providers focus on aspects of patient care. Help with navigating nuts‐and‐bolts issues can help them achieve “web‐side manner” and respond to the physical and emotional needs of their patients.
Successfully connecting with a patient via video telehealth is just the first step in a clinical encounter; tips and examples regarding how to best conduct the visits with older patients are also crucial. Our webinar delivered practical recommendations about how to establish “web‐side manner” in general and with older patients in particular.
Although the just‐in‐time resources we developed reflected VA‐specific policies and programs, the topics addressed (e.g., steps in accessing relevant technology, emergency procedures, strategies for resident/clinical educator supervision, patient communication, federal guidelines for prescribing across state lines, and mental health considerations) are relevant beyond the VA and clearly in high demand. Further, our rapid assessment provides valuable guidance regarding desired future steps in developing telehealth training that could include a suite of video visit simulations and side‐by‐side demonstrations of best practices. The unprecedented shifts in healthcare delivery driven by COVID‐19 are likely to result in a so called “new normal,” with one of the hallmarks an increased reliance on telehealth modalities as standard practice. The rapid assessment suggests that future trainees will continue to need both nuts‐and‐bolts instruction, as well as clinical telehealth training and skills development. To continue to inform efforts to prepare the workforce to care well for older adults today and in the future, we plan to survey GRECC‐affiliated trainees again in 6 months to assess the reach and effectiveness of the nuts‐and‐bolts resource described here, as well as emerging needs of the field.
ACKNOWLEDGMENTS
We would like to acknowledge and thank the Geriatric Research Education and Clinical Center (GRECC) associate directors for education and evaluation for their assistance in disseminating the rapid assessment and associated resources to training directors and trainees at their respective sites. The rapid response to COVID‐19 and efforts to enhance capacity to care for older adults via telehealth would not have been possible without their assistance and partnership. We would also like to acknowledge the contributions of Joe Huggins, webmaster and data analyst affiliated with the Eastern Colorado VA GRECC, who created the visual abstract (Figure 1) for this article.
Financial Disclosure
This manuscript was supported with funding provided by the U.S. Department of Veterans Affairs Office of Rural Health to the Geriatric Research Education and Clinical Center Connect (GRECC Connect) national dissemination project. Funding was also provided by the U.S. Department of Veterans Affairs Office of Geriatrics and Extended Care to support the national network of GRECCs, centers of excellence dedicated to supporting veterans as they age.
Conflict of Interest
The authors have declared no conflicts of interest for this article.
Author Contributions
All authors contributed significantly to this work. Conceived needs assessment effort: McLaren. Designed the trainee telehealth needs assessment: Nearing, Moo and McLaren. Substantial feedback/input: Gately, Moo and McLaren. Coordinated survey administration: Nearing and Moo. Analyzed and reported needs assessment results: Nearing. Led manuscript development: Nearing, Moo, Dang, and Powers. Created the nuts‐and‐bolts resource: McLaren, Gately, and Moo. Led the GRECC Connect webinar: Lum, Hung, Dang, Gately, and Moo. Led efforts to post resources to the GRECC Connect website: Hung, Lum, and Moo.
Sponsor's Role
The sponsors provided funding support for the education, training and career development efforts, as well as clinical innovation through telehealth modalities, featured as responses to COVID‐19. We thank the US Department of Veterans Affairs Office of Geriatrics and Extended Care and the US Department of Veterans Affairs Office of Rural Health for their ongoing support of GRECC and GRECC Connect, respectively, which make possible this enhanced capacity to care for older Veterans.
REFERENCES
- 1. Pimentel CB, Gately M, Barczi SR, et al. GRECC Connect: geriatrics telehealth to empower health care providers and improve management of older veterans in rural communities. Fed Pract. 2019;36(10):464‐470. [PMC free article] [PubMed] [Google Scholar]
- 2. Lum H, Nearing KA, Pimentel C, Levy C, Hung W. Anywhere to anywhere: use of telehealth to increase health care access for older rural veterans. Public Policy Aging Rep. 2020;30(1):12‐18. [Google Scholar]
- 3. U.S. Department of Veterans Affairs . Eldercare Workforce Alliance Issue Brief: Supporting the Geriatric Workforce and Older Veterans (online). Available at: https://eldercareworkforce.org/wp-content/uploads/2018/03/VA_Issue_Brief_FINAL.pdf. Accessed April 14, 2020.
- 4. U.S. Department of Veterans Affairs . Office of Academic Affiliations Academic Year 18‐19 Statistics: Health Professions Trainees (online). Available at: https://www.va.gov/OAA/docs/OAA_Statistics_2019.pdf. Accessed April 14, 2020.
- 5. Supiano MA, Alessi C, Chernoff R, et al. Department of Veterans Affairs geriatric research, education and clinical centers: translating aging research into clinical geriatrics. J Am Geriatr Soc. 2012;60(7):1347‐1356. [DOI] [PubMed] [Google Scholar]
- 6. U.S. Department of Veterans Affairs . VHA Handbook 1140.08. Veterans Health Administration Transmittal Sheet Washington, DC 20420 (online). Available at: https://www.va.gov/vhapublications/publications.cfm?Pub=2. Accessed July 6, 2020.
- 7. U.S. Department of Veterans Affairs . Office of Geriatrics and Extended Care. FY 19 GRECC Aggregated Annual Report. VHA Office of Geriatrics and Extended Care program analyst email communication. Accessed February 18, 2020.
- 8. U.S. Department of Veterans Affairs . Office of Rural Health. Rural Veterans. https://www.ruralhealth.va.gov/aboutus/ruralvets.asp. Updated January 28, 2020. Accessed April 14, 2020.
- 9. Cowper Ripley DC, Ahern JK, Litt ER, Wilson LK. Chapter 3: Veteran population, enrollees and patients. Rural Veterans Health Care Atlas, 2nd ed. FY 2015. Washington, DC: VHA Office of Rural Health Department of Veterans Affairs; 2017. https://www.ruralhealth.va.gov/docs/atlas/CHAPTER_03_Vets_Enrollees_Pts.pdf. Accessed April 14, 2020.
- 10. Peterson LE, Bazemore A, Bragg EJ, Xierali I, Warshaw GA. Rural‐urban distribution of the U.S. geriatrics physician workforce. J Am Geriatr Soc. 2011;59(4):699‐703. [DOI] [PubMed] [Google Scholar]
- 11. Hung WW, Rossi M, Thielke S, et al. A multisite geriatric education program for rural providers in the Veteran Health Care System (GRECC Connect). Gerontol Geriatr Educ. 2014;35(1):23‐40. [DOI] [PubMed] [Google Scholar]


