Abstract
Background
The COVID‐19 pandemic has presented veterinary emergency hospitals with unique challenges. Rapid online surveys represent an efficient way of collating responses to rapidly shifting circumstances.
Methods
Fifty, 24‐h small animal emergency veterinary hospital representatives were recruited to participate in weekly surveys in April 2020 to catalog changes due to COVID‐19 pandemic.
Key findings
The majority of emergency veterinary hospitals surveyed reported significant changes to day‐to‐day operations as a result of the COVID‐19 pandemic.
Significance
Reporting of weekly survey results provides useful information on how emergency veterinary hospitals with similar challenges are responding to the COVID‐19 pandemic.
Abbreviation
- CDC
Centers for Disease Control
1. INTRODUCTION
The COVID‐19 pandemic has presented 24‐h emergency small animal veterinary hospitals with unique and unprecedented challenges. Rapid online surveys represent a viable way to collect and disseminate real time data that may be useful for veterinary practices to understand how their colleagues are responding and how responses might adapt over time.
In late 2019, COVID‐19 began spreading in Wuhan, China and rapidly became a global pandemic. In March 2020, COVID‐19 was recognized as rapidly spreading throughout the United States with almost all 50 states implementing some form of “stay at home” order in March or April. 1 The Centers for Disease Control (CDC) published an Interim Infection Prevention and Control Guidance for Veterinary Clinics Treating Companion Animals During the COVID‐19 Response 2 that broadly outlined recommendations for veterinarians in the US, which included postponing elective surgeries, procedures and non‐urgent visits. However, interpretation, implementation, and experiences vary greatly. In addition, emergency veterinary hospitals have some unique challenges as compared to primary care practices that are not directly addressed in the CDC guidance. The purpose of this series of surveys conducted during the COVID‐19 pandemic was to characterize and report the changes implemented by veterinary emergency hospitals.
2. METHODS
Responders were recruited via the American College of Veterinary Emergency and Critical Care (ACVECC) and American College of Veterinary Internal Medicine (Small Animal) (ACVIM‐SA) listserves. An electronic survey created with commercial software * was distributed weekly for 3 consecutive weeks starting April 6, 2020. Responders could participate in all 3, 2, or just 1 survey. Descriptive statistics were tabulated using commercially available software. † The study protocol was reviewed by the Tufts Institutional Review Board (IRB) and exempt status was granted.
3. RESULTS
A total of 67 representatives were recruited. In week 1, representatives from 45 hospitals responded, 36 in week 2, and 38 in week 3 (response rate 54‐67%). Over 3 weeks, a total of 50 unique hospitals were represented in at least 1 of the surveys. Table 1 shows the distribution of types of hospitals responding. The map in Figure 1 shows the distribution of 46 hospitals in the United States. An additional 4 hospitals with respondents were located outside the United States.
TABLE 1.
Distribution of 50 hospitals responding to survey regarding changes due to COVID‐19 in April 2020
| Type of hospital | Count |
|---|---|
| Corporately owned emergency vet hospital | 23 |
| Non‐profit emergency vet hospital | 3 |
| Privately owned emergency vet hospital | 16 |
| Academic teaching hospital with emergency services | 8 |
FIGURE 1.
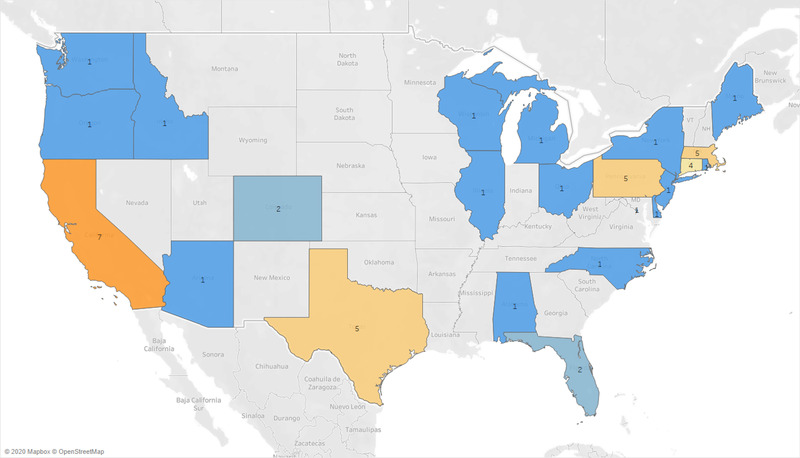
Map showing location of 46 hospitals represented in the US that responded to surveys. Four additional responding hospitals are located outside the United States
3.1. Respondents
Thirteen of 50 (26%) respondents were hospital directors and an additional 21 (42%) have a leadership role. Thirty‐four hospitals currently have special teams dedicated to the COVID‐19 response effort and 28 respondents are on the special team if it exists in their hospital. Eleven of 50 (22%) responders are not on a specific team but are spending more than 25% of their time on aspects related to COVID‐19 response.
3.2. Prior preparations
Prior to the COVID‐19 pandemic, only 12 of 50 (24%) hospitals had a full business continuity or disaster plan. Twenty‐two of 50 (44%) had contingency plans in place for anticipated short‐term disruptions, such as snow days, while 16 (32%) had no plans for either short‐ or long‐term disruptions or disasters.
3.3. Hospital operations
Most respondents report major changes to hospital operations with only 6 of 50 (12%) running as usual and 6 of 50 (12%) were only seeing emergency cases. Thirty‐three of 50 (66%) were limiting caseload to some extent and 5 of 50 (10%) reported some other changes. Determining what represents an emergency case was deemed a challenge, particularly without a clear end‐date to the pandemic state. Table 2 represents sample scenarios to provide more clarity on how hospitals were classifying emergency or essential cases in the initial phases of COVID‐19. Most hospitals were restricting client access to hospitals, with 37 only allowing access for euthanasia, 3 allowing visitors with restrictions, and 7 not permitting visits even for euthanasia/end of life decisions. Twelve hospitals (24%) responding had instituted “all in, all out” scheduling protocols with rotating teams of people that switch on and off working, while the remaining 76% had another type of schedule. Thirty‐four of 38 (89%) responding hospitals were re‐assigning staff to work outside their normal work space.
TABLE 2.
Responses by emergency hospitals when asked how they would handle specific case scenarios in the emergency room during April 2020 in response to COVID‐19
| Minimal treatment/diagnostics and tell owner to call back if pet gets sicker or hospital resumes seeing non‐essential/urgent/emergent cases | Operate or pursue additional diagnostics as soon as possible | Refer back to primary care veterinarian or other urgent care clinic | Case is triaged away on arrival and not seen by our emergency service | Other | |
|---|---|---|---|---|---|
| 2 year male neutered Labrador presents acutely lame. | (9) 33.33% | (8) 29.63% | (3) 11.11% | (2) 7.41% | (5) 18.52% |
| 10 year male German Shepherd Dog seen by primary care veterinarian for one episode of vomiting. Physical exam reveals a large abdominal mass. Dog is otherwise stable. | (4) 14.81% | (22) 81.48% | 0.00% | (1) 3.70% | 0.00% |
| 3 year male neutered Dalmatian with bladder stones presents obstructed. | 0.00% | (26) 96.30% | 0.00% | 3.70% | 0.00% |
| 5 year female neutered mixed breed dog referred for further work‐up of suspected protein losing enteropathy (Albumin 1.2 mg/dL). Dog is clinically doing well but has diarrhea and has had some weight loss over the last 6 weeks. | (8) 29.63% | (11) 40.74% | 3.70% | 11.11% | (4) 14.81% |
| 12 year male neutered golden retriever presents with 2 week history of mucopurulent nasal discharge and decreased appetite, although still eating and no weight loss. Bloodwork unremarkable and met check clear at primary care veterinarian. | (11) 40.74% | (11) 40.74% | 3.70% | 7.41% | 7.41% |
3.4. COVID‐19 positive individuals
As of April 13, 2020, 9 (18%) responding hospitals had at least 1 employee test positive for COVID‐19. The response to a positive test result was to clean the hospital and isolate specific employees in close contact with positive individuals and no additional changes in hospital function in 5 hospitals (56%), close the part of the hospital the employee worked in 1 (11%) and some other response in 3 (33%). None reported that they closed the entire hospital. Of the 36 hospitals that answered, 12 (33%) were screening employee temperatures prior to reporting for an assigned shift. Animals seen from known or suspected COVID‐19 positive households were treated in a variety of ways as shown in Table 3.
TABLE 3.
Changes in how animals were handled at emergency hospitals in response to COVID‐19 in April 2020
| How are you handling OUT‐patients from COVID+ or suspect COVID+ households? | |
|---|---|
| Animals are bathed or wiped down with cleaning product, then treated as usual (no additional precautions or Personal Protective Equipment) | 8 |
| Animals are seen and treated by staff in full Personal Protective Equipment | 17 |
| No additional precautions | 1 |
| Other | 8 |
| We will not see these pets at all | 2 |
| Total | 36 |
| How are you handling IN‐patients from COVID+ or suspect COVID+ households? | |
|---|---|
| Animals are admitted to isolation and only handled with full Personal Protective Equipment | 22 |
| Animals are admitted to wards and handled with Personal Protective Equipment | 3 |
| No additional precautions | 2 |
| Not allowing these animals to be admitted | 1 |
| Other | 8 |
| Total | 36 |
| Have you changed how you handle cats due to COVID‐19? | |
|---|---|
| All cats are put into isolation or only handled with full Personal Protective Equipment | 1 |
| Cats with clinical signs (cough, fever) are put into isolation or only handled with full Personal Protective Equipment | 15 |
| No changes | 17 |
| Other | 3 |
| Total | 36 |
| Have you changed how you handle ferrets (for hospitals that see ferrets) due to COVID‐19? | |
|---|---|
| All ferrets are put into isolation or handled only with full PPE | 1 |
| Ferrets with clinical signs (cough, fever) are put into isolation or only handled with full PPE | 2 |
| No changes | 4 |
| Other | 4 |
| Total | 11 |
3.5. Shortages
Nineteen hospitals experienced drug shortages and 35 reported technical staff shortages related to COVID‐19 in April. Most hospitals (39/50, 78%) reported a shortage of personal protective equipment (PPE) at some time point in April, but only 3 (6%) reported that it affected ability to function normally.
3.6. Financial implications
On April 13, 2020 (survey week 2), when asked if euthanasia rates had increased as compared to pre‐COVID‐19 (as percentage of cases compared to February 2020 or the same week in 2019), 15 of 36 (53%) said it was about the same, 11 of 36 (31%) did not know or have access to data, 1 (2%) said decreased by more than 25%, and 9 (25%) reported an increase by more than 25%. Subjectively 26 of 36 (72%) respondents thought clients had more financial limitations than before the COVID‐19 pandemic with 3 (8%) responders unsure and 7 (19%) had not appreciated a difference. Eight (22%) of 37 practices had placed individuals on unpaid leave/furlough. Two (5%) of 36 practices had laid off individuals in response to the COVID‐19 pandemic. Five (14%) of practices were providing “hazard” pay for employees, while 31(86%) were not providing additional pay.
3.7. Employee support
Most hospitals responding (35/43, 81%) reported they were doing something to help employees deal with added stress related to COVID‐19. Specific answers varied but included online resources including counseling or access to social workers, increased check ins with staff, games, handing out individually wrapped meals or snacks, emails on self‐care, regular “town halls” to disseminate information and answer questions, being understanding and flexible for childcare/eldercare needs or immunocompromised family members, “COVID bonuses” for staff working in the clinic and providing cloth masks.
3.8. Plan to resume operations
Most hospitals (20/37; 54%) are planning a slow ramp up with attempts to maintain social distancing and keep as few people in the building as possible, 9 of 37 (24%) plan to continue to not allow clients in the building but otherwise planning to return to normal as fast as possible, while only 1 (3%) responder said they were returning to pre‐pandemic clinic activities as fast as possible. Four clinics had other plans and 9 (24%) said they were still running pretty close to normal. When asked how hospitals are deciding which services to resume first, 9 said revenue was primarily driving decisions and 9 said ability to enable social distancing with another 15 using other criteria such as a combination of the 2 or having enough PPE.
4. DISCUSSION
Veterinary emergency hospitals provide essential services to people and their animals, and continuing to provide care during the COVID‐19 pandemic presents unique challenges. Facilities face difficulties around remaining open, being able to provide adequate and appropriate services while keeping staff safe and healthy in the midst of imperfect and ever‐changing data are vast and variable. Survey data can provide colleagues with data on how others are handling similar challenges.Independent Vets, a company that employs relief veterinarians and matches them with hospitals in need, has conducted similar serial surveys of more than 300 general small animal veterinary practices, with a disproportionate (2/3) number from the northeast United States. Their surveys in March and April similarly showed that approximately 60% of practices had made changes in operating hours, most (more than 85%) are not allowing clients in the building, most (approximately 75%) had reduced staff, with main drivers being caring for a child(ren) at home or employees unwilling to work. 3
Only 24% of hospitals surveyed here had full business continuity or disaster plans in place prior to COVID‐19. The American Veterinary Medical Association recommends all small animal hospitals have disaster plans in place. 4 The prolonged nature of COVID‐19 is unique compared to many other disasters, but planning provides a framework from which to adjust for specific situations. COVID‐19 may encourage more veterinary hospitals to create business continuity or disaster plans.
Burnout and stress among veterinarians prior to COVID‐19 were common. 5 , 6 The stressors related to COVID‐19 only serve to further strain veterinarians and their staff and in particular those providing 24‐h emergency care. It is clear that COVID‐19 will have sustained financial impacts on hospitals. Employers should actively explore ways to reduce stress on teams and promote positive work environments.
These data highlight that 24‐hr emergency veterinary practices have been massively disrupted by COVID‐19. Significant stressors are likely to continue to impact veterinary hospitals and their staffs for some time. The continuation of surveying emergency veterinary hospitals and dissemination of timely information is planned for remainder of the COVID‐19 pandemic.
CONFLICT OF INTEREST
The authors declare no conflict of interests.
Wayne AS, Rozanski EA. Cataloguing the response by emergency veterinary hospitals during the COVID‐19 pandemic via weekly surveys. J Vet Emerg Crit Care. 2020;30:493–497. 10.1111/vec.12974
ENDNOTES
Qualtrics XM, Qualtrics, Provo, UT
Microsoft Excel (Version 16.36), Microsoft Corporation, Redmond, WA
REFERENCES
- 1. Avilia Y, Harvey B, Matthew AL, et al. Which states are reopening and which are still shut down. New York Times. 2020. Available at: https://www.nytimes.com/interactive/2020/us/states-reopen-map-coronavirus.html. Accessed May 5, 2020.
- 2. Centers for Disease Control (CDC) . Interim Infection Prevention and Control Guidance for Veterinary Clinics Treating Companion Animals During the COVID‐19 Response. Available at: https://www.cdc.gov/coronavirus/2019-ncov/community/veterinarians.html. Accessed May 5, 2020.
- 3.Independent Vets COVID‐19 veterinary hospital survey data. Available at: https://static1.squarespace.com/static/59d28522d55b41fdb4e75415/t/5e9a0474009ad16ead29b37c/1587151990990/IndeVets+-+Week+5+COVID+Hospital+Survey+Comparitive+Analysis.pdf. Accessed May 5, 2020.
- 4. American Veterinary Medical Association (AVMA) . Disaster Preparedness. Available at: https://www.avma.org/resources-tools/animal-health-and-welfare/disaster-preparedness. Accessed May 14, 2020.
- 5. Hayes GM, LaLonde‐Paul DF, Perret JL, et al. Investigation of burnout syndrome and job related risk factors in veterinary technicians in specialty teaching hospitals: a multicenter cross‐sectional study. J Vet Emerg Crit Care. 2020;30:18‐27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kim RW, Patterson G, Naha VK, Sharma M. Toward an evidence‐based approach to stress management for veterinarians and veterinary students. J Am Vet Med Assoc. 2017;251:1002‐1004. [DOI] [PubMed] [Google Scholar]


