Abstract
In March 2020, coronavirus disease 2019 (COVID-19) spread rapidly nationally, causing widespread emergent changes to the health system. Our goal was to understand the impact of the epidemic on kidney transplantation (KT), at both the national and center levels, accounting statistically for waitlist composition. Using Scientific Registry of Transplant Recipients data, we compared data on observed waitlist registrations, waitlist mortality, and living-donor and deceased-donor kidney transplants (LDKT/DDKT) March 15-April 30, 2020 to expected events calculated from preepidemic data January 2016-February 2020. There were few changes before March 15, at which point the number of new listings/DDKT/LDKT dropped to 18%/24%/87% below the expected value (all P < .001). Only 12 centers performed LDKT March 15-31; by April 30, 40 centers had resumed LDKT. The decline in new listings and DDKT was greater among states with higher per capita confirmed COVID-19 cases. The number of waitlist deaths was 2.2-fold higher than expected in the 5 states with highest COVID-19 burden (P < .001). DCD DDKT and regional/national imports declined nationwide but most steeply in states with the highest COVID-19 burden. The COVID-19 epidemic has resulted in substantial changes to KT; we must adapt and learn rapidly to continue to provide safe access to transplantation and limit the growing indirect toll of an already deadly disease.
KEYWORDS: clinical research/practice, donors and donation: deceased, donors and donation: living, health services and outcomes research, infection and infectious agents – viral, infectious disease, kidney transplantation/nephrology, organ transplantation in general, patient survival, registry/registry analysis
Abbreviations: AKI, acute kidney injury; COVID-19, coronavirus disease 2019; DCD, donation after circulatory death; DDKT, deceased-donor kidney transplantation; DGF, delayed graft function; ESRD, end-stage renal disease; HRSA, Health Resources and Services Administration; ICU, intensive care unit; IRR, incidence rate ratio; KT, kidney transplant; LDKT, living-donor kidney transplantation; OPTN, Organ Procurement and Transplantation Network; OR, operating room; PMP, per million population; SRTR, Scientific Registry of Transplant Recipients
1. INTRODUCTION
Since late December 2019, when a cluster of cases of pneumonia was reported in Wuhan, China, the spread of coronavirus disease 2019 (COVID-19) and subsequent effects on the world’s health care systems have been explosive and wide ranging.1 The effects have varied by region, as have the responses to the epidemic, with certain countries and areas reacting with strict shelter-in-place orders and others observing a rapid escalation of cases and deaths due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). In some states, health care resources have been stretched thin and overwhelmed with the number of cases outstripping the number of hospital beds and intensive care resources. Organ transplantation is a resource-intensive endeavor, and thus the potential effects of the epidemic on transplantation in the United States are profound.
COVID-19 has affected virtually all aspects of kidney transplantation (KT),2, 3, 4, 5, 6, 7, 8, 9 including the donor supply and both candidates and recipients.10, 11, 12, 13 Early reports demonstrate variable severity in patients with end-stage renal disease (ESRD) and KT, ranging from asymptomatic to fulminant respiratory failure and death.14 Furthermore, COVID-19 has been associated with acute kidney injury (AKI), which may predispose KT recipients to increased morbidity.15, 16, 17 Previous experience with related viruses, SARS-CoV in 200318 and Middle East respiratory syndrome-related coronavirus (MERS-CoV) in 2015,19 demonstrated that immunosuppressed KT recipients may be anticipated to have prolonged viral shedding, potentially increasing transmissibility, morbidity, and mortality.7 , 20
In a national survey of US transplant centers in the last week of March 2020, 72% of centers reported that they had suspended living-donor KT (LDKT) and 84% reported restrictions to deceased-donor KT (DDKT); more stringent restrictions were associated with higher regional incidence of COVID-19.21 Restrictions varied by center; for example, some centers reported transplanting highly sensitized patients and those without dialysis access, whereas others reported transplanting those with the lowest risk of delayed graft function (DGF), prolonged hospital stay, or readmission.
These actions were taken in the context of immense uncertainty, during an epidemic that was at one point doubling every 2 days, and in the context of an emergency national diversion of hospital resources to address the anticipated burden of COVID-19 on the medical system. However, simulation data suggest that even a temporary suspension of KT may lead to greater risk of death for waitlist registrants.22 The early effect of the epidemic on access to KT in the United States has not been quantified. Given the variation in incidence of COVID-19 across the United States, limited knowledge about COVID-19 prevalence among the general population, and ongoing diversion of healthcare resources, we hypothesized that COVID-19’s impact on KT might also be center dependent and associated with geographic incidence of COVID-19.
To address this knowledge gap, using data from the SRTR, we conducted a retrospective study of changes to KT waitlist registration, waitlist deaths, and rates of DDKT and LDKT March-April 2020. We examined rates of these waitlist events among the overall patient population and among key patient subgroups and stratified by state-level burden of COVID-19 infection.
2. METHODS
2.1. DATA source
This study used data from the Scientific Registry of Transplant Recipients (SRTR). The SRTR data system includes data on all donor, wait-listed candidates, and transplant recipients in the United States, submitted by the members of the Organ Procurement and Transplantation Network (OPTN), and has been described elsewhere.23 The Health Resources and Services Administration (HRSA), US Department of Health and Human Services provides oversight to the activities of the OPTN and SRTR contractors.
2.2. State-level cumulative incidence of COVID-19 per million population
To examine the relationship between COVID-19 burden and waitlist events (new listings, DDKT, and deaths), we calculated cumulative incidence of reported COVID-19 cases per million population (PMP) at the state level (including the District of Columbia and Puerto Rico) on March 25, 2020, using data from http://covidtracking.com/. States were classified by COVID-19 burden as “low” (<50 cases PMP: 13 states), “medium” (50-100 cases PMP: 15 states), “high” (100-300 cases PMP: 15 states), and “very high” (300-1584 cases PMP: Louisiana, Michigan, New Jersey, New York, and Washington state).
2.3. Daily counts of waitlist changes
For each day between February 1 and April 30, 2020, we plotted daily counts of new waitlist registrations, newly inactive patients, and waitlist removals due to DDKT, LDKT, death, or deteriorating condition, with a Lowess smooth. For new waitlist registrations, LDKT, and newly inactive registrants, only weekdays were included, because between January 2016 and February 2020 >98.5% of these events occurred on weekdays. We made similar plots for daily counts of donation after circulatory death (DCD), DDKT, and regional and national imports. Because LDKT decreased abruptly after March 15, we plotted of center-level counts of LDKT between March 15 and April 30, 2020 by state-level cumulative incidence of COVID-19 PMP.
2.4. Calculating center-level expected numbers of waitlist events
A raw count of center-level waitlist events fails to take into account potential differences in a center’s waitlist population over time. To address this, for each of the waitlist events described, we modeled the number of outcomes per center per month between January 2016 and February 2020 using multilevel Poisson regression, with a center-level random intercept and adjusting for center-level distribution of candidate characteristics: age, sex, prior transplant, race/ethnicity, history of diabetes, insurance type, time on dialysis, and ABO blood type. We then used these models to predict the expected number of outcomes per month in March-April 2020. We made these predictions overall and for subgroups of patients based on candidate characteristics.
2.5. Comparing observed to expected center-level numbers of waitlist events
For each type of waitlist event, we compared observed to expected counts using χ2 tests, overall and for various patient subgroups. Additionally, to compare differences in observed vs expected events among centers in states with different levels of COVID-19 burden, we used Poisson regression. Specifically, we modeled the observed counts, including the log of expected counts in the model with the coefficient constrained to 1 and adjusting for state-level COVID-19 burden. The incidence rate ratios (IRRs) from this model represent the observed counts as a proportion of expected counts.
2.6. Statistical analysis
Confidence intervals are reported as per the method of Louis and Zeger.24 All analyses were performed using Stata 16.1/MP for Linux.
3. RESULTS
3.1. Daily counts of waitlist changes
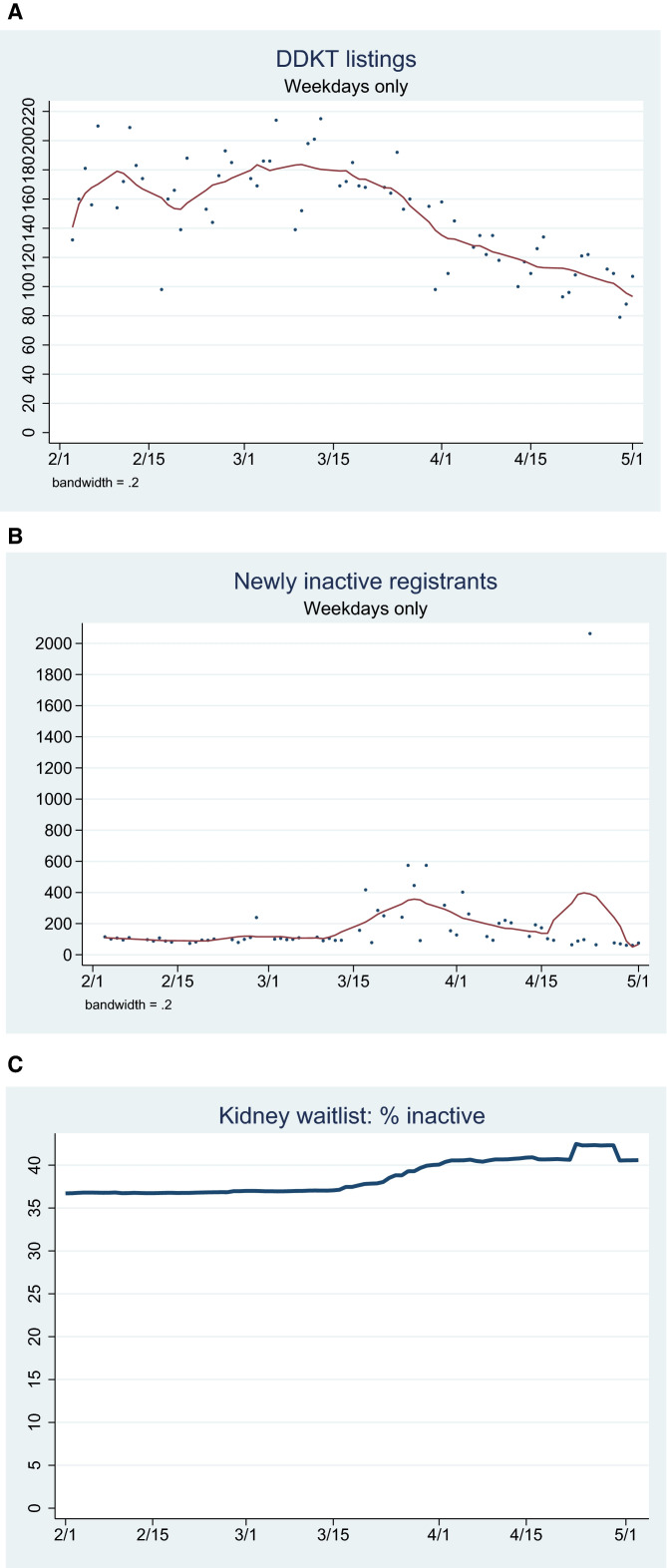
Between February 1 and March 1, 2020, on average there were 168 new registrations per weekday; this declined to 158 per weekday by April 1 and 107 on May 1 ( Figure 1A). The number of newly inactive patients averaged 102 per weekday from February 1 to mid-March, before climbing to 385 per day in the week of March 23-27 and 192 per day between April 1-15 (Figure 1B). There is an odd spike because 1 center changed its entire waitlist to inactive on April 23 and then back to active on April 30.
FIGURE 1.
Kidney transplant (KT) waitlist registrations and active status, February-April 2020. Counts of new deceased-donor kidney transplantation (DDKT) waitlist registrations (A) and patients moved to inactive status (B) per day, with Lowess smooth; (C) proportion of prevalent waitlist list listed as inactive per day [Color figure can be viewed at wileyonlinelibrary.com]
The proportion of the waitlist that was inactive rose gradually from 36.7% on February 1 to 37.1% on March 15, to 40.4% by April 2 and 40.5% by May 1 (Figure 1C).
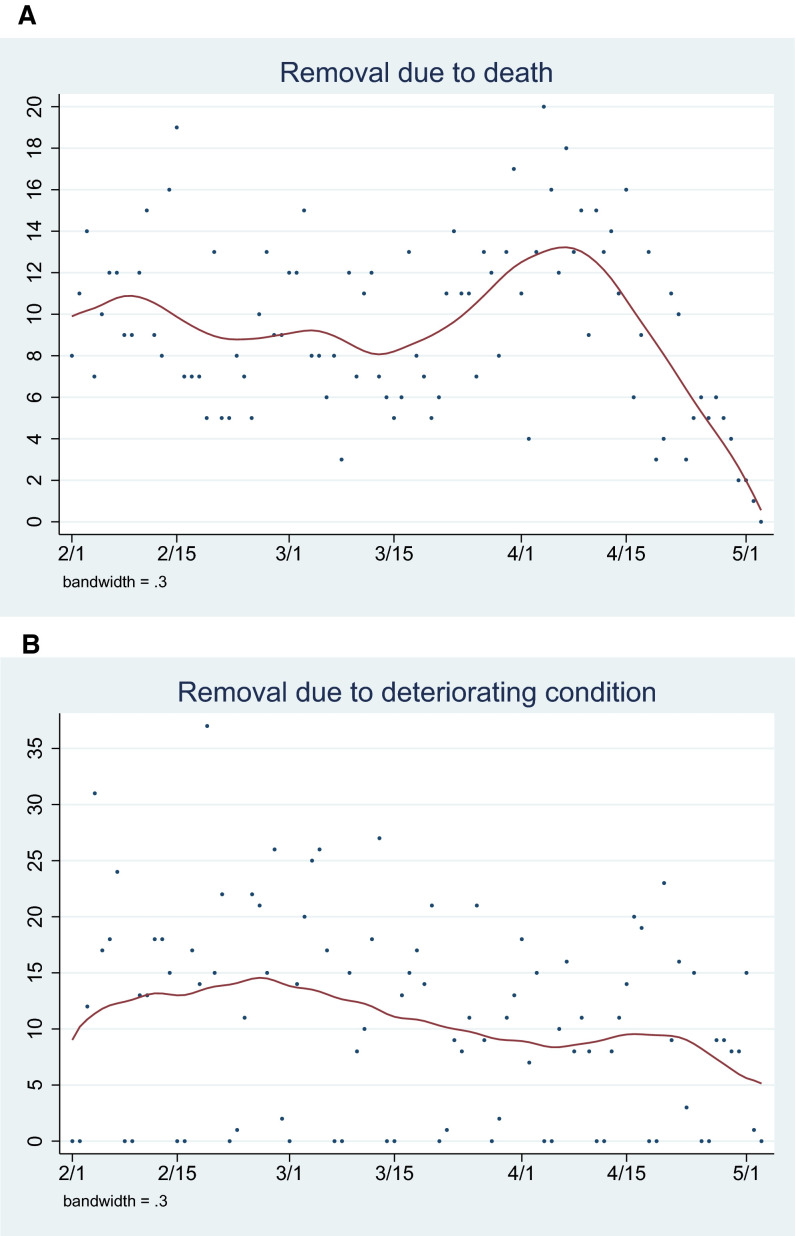
The number of waitlist removals due to death and deteriorating condition averaged 9.3 and 12.5 per day, respectively ( Figure 2A,B).
FIGURE 2.
Counts of kidney transplant (KT) waitlist outcomes per day, February-April 2020, with Lowess smooth: (A) removals due to death; (B) removals due to deteriorating condition [Color figure can be viewed at wileyonlinelibrary.com]
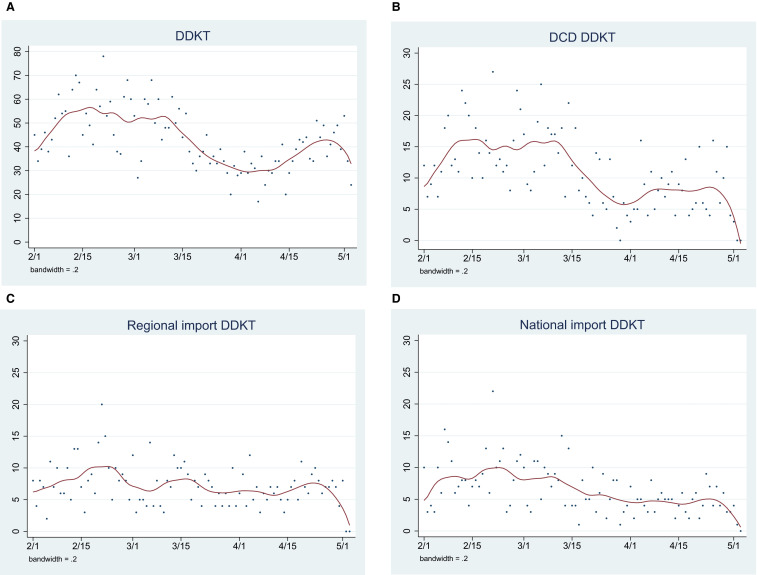
The number of DDKT averaged 51 per day; this number declined from 47 on March 15 to 29 on April 1, and was 53 on May 1 ( Figure 3A). The number of DCD DDKT declined from 12 on March 15 to 3 on April 1 and 3 on May 1 (Figure 3B). The number of regional and national imports declined over the same interval (Figure 3C,D).
FIGURE 3.
Counts of deceased-donor kidney transplantation (DDKT) per day, February-April 2020, with Lowess smooth: (A) all DDKT, (B) donation after cardiac death (DCD), (C) regional imports, (D) national imports [Color figure can be viewed at wileyonlinelibrary.com]
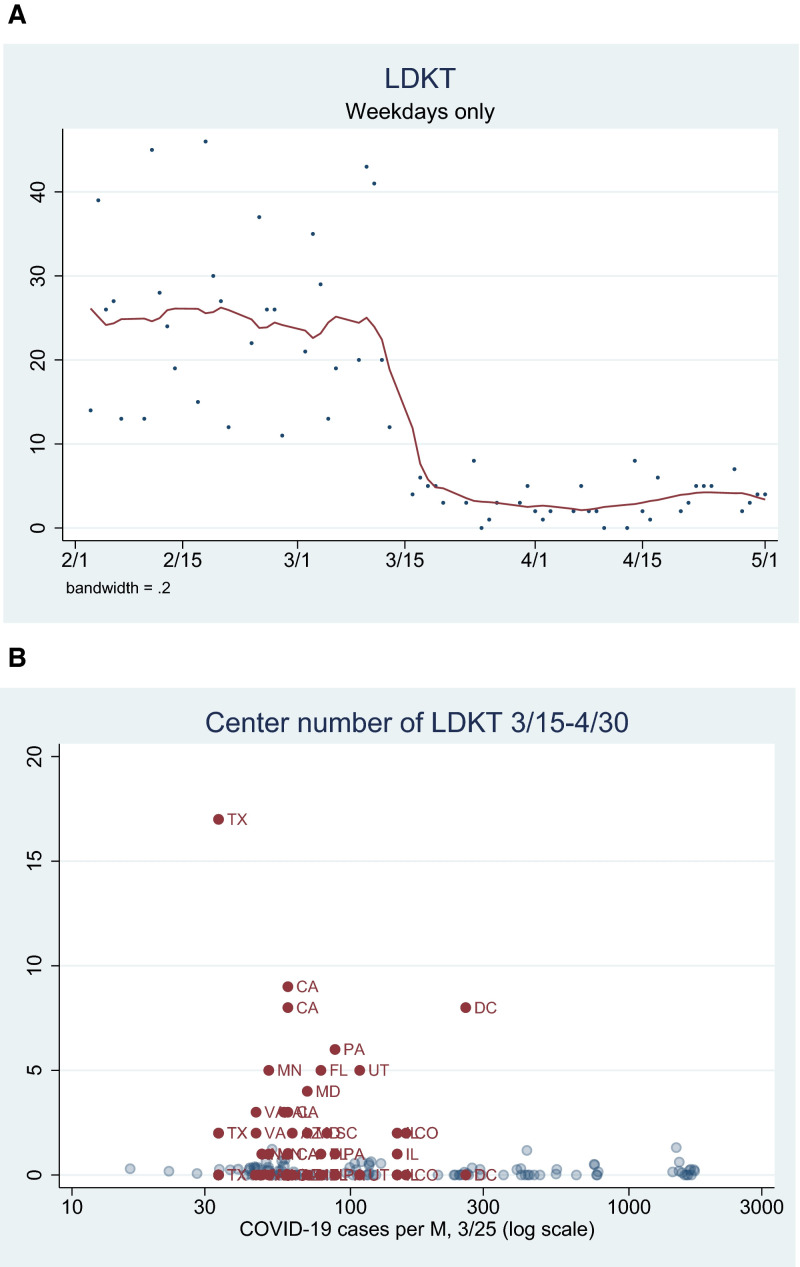
The average number of LDKT per day declined sharply after March 15 ( Figure 4A). Only 12 centers performed LDKT between March 15 and March 31, of which only 6 performed more than 2 LDKTs. Between March 15 and April 30, 40 centers performed LDKT, of which 12 performed more than 2 LDKTs. None of the 40 centers were in states with more than 300 COVID-19 cases PMP (Figure 4B).
FIGURE 4.
Living-donor kidney transplantation (LDKT), February-April 2020. (A) Counts of LDKT per day, February-March 2020, with Lowess smooth. (B) Center-level LDKT, February-April 2020, by coronavirus disease 2019 (COVID-19) prevalence per million population. Centers from states where more than 1 LDKT was performed are marked in dark red [Color figure can be viewed at wileyonlinelibrary.com]
3.2. Comparing observed to expected counts of waitlist events
Overall, the observed number of DDKT between March 15-April 30 (1673) was 23.9% lower than the expected number (2197.8), a statistically significant difference (P < .001) ( Table 1). Similarly, the observed number of LDKT (114) was 87.2% lower than expected (888.2, P < .001) ( Table 2). The observed number of waitlist deaths (453) was 6.5% higher than expected (425.3, P = .2) ( Table 3).
TABLE 1.
Observed and expected DDKT counts, March 15-April 30, 2020
| Category | Expected | Observed | % change | P |
|---|---|---|---|---|
| Overall | 2197.8 | 1673 | −23.9 | <.001 |
| Age: 0-11 | 25.5 | 11 | −56.9 | |
| Age: 12-17 | 34.9 | 26 | −25.5 | |
| Age: 18-29 | 135.5 | 144 | 6.3 | |
| Age: 30-39 | 260.6 | 236 | −9.4 | <.001 |
| Age: 40-49 | 431.4 | 360 | −16.6 | |
| Age: 50-59 | 602.7 | 443 | −26.5 | |
| Age: 60-69 | 580.0 | 375 | −35.3 | |
| Age: 70+ | 145.9 | 78 | −46.5 | |
| Prior tx: no | 1911.1 | 1480 | −22.6 | .4 |
| Prior tx: yes | 274.6 | 193 | −29.7 | |
| Race/ethnicity: white | 827.9 | 596 | −28.0 | |
| Race/ethnicity: black | 717.5 | 569 | −20.7 | |
| Race/ethnicity: Hispanic | 436.8 | 344 | −21.2 | .7 |
| Race/ethnicity: Asian | 159.8 | 123 | −23.0 | |
| Race/ethnicity: other nonwhite | 52.0 | 41 | −21.2 | |
| DM: no | 1368.7 | 1056 | −22.8 | .7 |
| DM: yes | 831.6 | 616 | −25.9 | |
| Pay: private | 799.3 | 687 | −14.0 | |
| Pay: Medicaid | 207.6 | 144 | −30.6 | |
| Pay: Medicare | 1073.8 | 769 | −28.4 | <.001 |
| Pay: other pub | 25.6 | 25 | −2.3 | |
| Pay: other | 69.3 | 29 | −58.2 | |
| Male | 1331.7 | 1078 | −19.1 | <.01 |
| Female | 862.5 | 595 | −31.0 |
Abbreviations: DDKT, deceased-donor kidney transplantation; DM, diabetes mellitus.
TABLE 2.
Observed and expected LDKT counts, March 15-April 30, 2020
| Category | Expected | Observed | % change | P |
|---|---|---|---|---|
| Overall | 888.2 | 114 | −87.2 | <.001 |
| Age: 0-11 | 13.9 | 4 | −71.2 | |
| Age: 12-17 | 11.6 | 1 | −91.4 | |
| Age: 18-29 | 93.6 | 9 | −90.4 | |
| Age: 30-39 | 125.8 | 13 | −89.7 | .2 |
| Age: 40-49 | 171.8 | 29 | −83.1 | |
| Age: 50-59 | 212.9 | 30 | −85.9 | |
| Age: 60-69 | 189.2 | 25 | −86.8 | |
| Age: 70+ | 68.7 | 3 | −95.6 | |
| Prior tx: no | 790.3 | 103 | −87.0 | >.9 |
| Prior tx: yes | 90.7 | 11 | −87.9 | |
| Race/ethnicity: white | 563.1 | 74 | −86.9 | |
| Race/ethnicity: black | 115.7 | 14 | −87.9 | |
| Race/ethnicity: Hispanic | 130.3 | 15 | −88.5 | .5 |
| Race/ethnicity: Asian | 55.3 | 11 | −80.1 | |
| Race/ethnicity: other nonwhite | 15.3 | 0 | −100.0 | |
| DM: no | 627.5 | 79 | −87.4 | >.9 |
| DM: yes | 259.5 | 35 | −86.5 | |
| Pay: private | 532.7 | 76 | −85.7 | |
| Pay: Medicaid | 56.3 | 6 | −89.3 | |
| Pay: Medicare | 250.5 | 26 | −89.6 | .7 |
| Pay: other pub | 4.7 | 0 | −100.0 | |
| Pay: other | 41.8 | 4 | −90.4 | |
| Male | 552.2 | 78 | −85.9 | .4 |
| Female | 330.0 | 36 | −89.1 |
Abbreviations: LDKT, living-donor kidney transplantation.
TABLE 3.
Observed and kidney waitlist deaths, March 15-April 30, 2020
| Category | Expected | Observed | % change | P |
|---|---|---|---|---|
| Overall | 425.3 | 453 | 6.5 | .2 |
| Age: 0-11 | 0.4 | 2 | 400.0 | |
| Age: 12-17 | 1.6 | 2 | 25.0 | |
| Age: 18-29 | 10.2 | 7 | −31.4 | |
| Age: 30-39 | 25.1 | 30 | 19.5 | .03 |
| Age: 40-49 | 71.5 | 71 | -0.7 | |
| Age: 50-59 | 129.2 | 161 | 24.6 | |
| Age: 60-69 | 155.1 | 143 | −7.8 | |
| Age: 70+ | 29.3 | 37 | 26.3 | |
| Prior tx: no | 353.6 | 386 | 9.2 | .7 |
| Prior tx: yes | 69.3 | 67 | −3.3 | |
| Race/ethnicity: white | 179.9 | 167 | −7.2 | |
| Race/ethnicity: black | 123.8 | 152 | 22.8 | |
| Race/ethnicity: Hispanic | 78.0 | 82 | 5.1 | .2 |
| Race/ethnicity: Asian | 32.1 | 42 | 30.8 | |
| Race/ethnicity: other nonwhite | 9.5 | 10 | 5.3 | |
| DM: no | 153.4 | 161 | 5.0 | .9 |
| DM: yes | 267.1 | 291 | 8.9 | |
| Pay: private | 157.5 | 171 | 8.6 | |
| Pay: Medicaid | 32.3 | 61 | 88.9 | |
| Pay: Medicare | 219.1 | 212 | −3.2 | <.001 |
| Pay: other pub | 5.6 | 4 | −28.6 | |
| Pay: other | 8.7 | 3 | −65.5 | |
| Male | 266.3 | 316 | 18.7 | .01 |
| Female | 156.8 | 137 | −12.6 |
Abbreviations: DM, diabetes mellitus.
The center-level observed number of new listings, DDKT, and LDKT March 15-April 30 was lower than the expected number across all categories of COVID-19 burden ( Table 4A). Among centers in states with low COVID-19 rates, there were 9% fewer new listings than expected (IRR 0.850.910.96). The proportional drop in new listings was steeper at centers in states with higher COVID-19 rates (eg, IRR in “very high” states = 0.540.590.64). Similarly, the IRR for observed vs expected DDKT ranged from 0.720.790.87 in states with low COVID-19 rates to 0.330.390.46 in states with very high COVID-19 rates. Among centers in states with low COVID-19 rates, there were 84% fewer LDKT than expected (IRR = 0.110.160.23); among centers in states with very high COVID-19 rates, there were 99% fewer LDKT than expected (IRR = 0.000.010.05). Centers in states with very high COVID-19 rates had 2.2-fold more waitlist deaths than expected (IRR = 1.882.222.62). The decline in DDKT was greatest among patients over the age of 50 (eg, for age 70+, 78 observed vs 145.9 expected) (Table 1).
TABLE 4.
Observed center-level events as a proportion of expected events, March 15-April 30, 2020
| (A) | ||||
|---|---|---|---|---|
| COVID-19 rates | New listings | DDKT | LDKT | Waitlist death |
| Overall | 0.800.820.84 | 0.730.760.80 | 0.110.130.15 | 0.971.071.17 |
| Low (NC/TX/VA+10) | 0.850.910.96 | 0.720.790.87 | 0.110.160.23 | 0.590.771.00 |
| Medium (CA/FL/PA+12) | 0.840.870.91 | 0.870.930.99 | 0.130.170.22 | 0.700.810.95 |
| High (IL/MA/TN+12) | 0.740.790.85 | 0.580.660.74 | 0.080.110.17 | 0.861.051.29 |
| Very high (LA/MI/NJ/NY/WA) | 0.540.590.64 | 0.330.390.46 | 0.000.010.05 | 1.882.222.62 |
| (B) | |||
|---|---|---|---|
| COVID-19 rates | DCD DDKT | Regional import | National import |
| Low (NC/TX/VA+10) | 0.500.620.76 | 0.660.821.03 | 0.680.901.18 |
| Medium (CA/FL/PA+12) | 0.770.881.01 | 0.891.031.19 | 0.630.760.91 |
| High (IL/MA/TN+12) | 0.360.470.61 | 0.610.811.08 | 0.620.841.14 |
| Very high (LA/MI/NJ/NY/WA) | 0.140.210.33 | 0.140.260.48 | 0.160.250.38 |
Note. Centers in states with the lowest rates of per capita reported coronavirus disease 2019 (COVID-19) cases had 9% fewer new listings than expected (incidence rate ratio [IRR] = 0.91), 21% fewer DDKT (IRR 0.79), 84% fewer LDKT (IRR 0.16), and 23% fewer waitlist deaths (IRR = 0.77, NS). Centers in states with very high rates of COVID-19 cases had 41% fewer new listings than expected, 61% fewer DDKT, 99% fewer LDKT, and 2.2-fold more waitlist deaths. Bold denotes IRRs that are statistically significantly different from the IRR in states with the lowest per-capita reported COVID-19 cases.
Abbreviations: DCD, donation after cardiac death; DDKT, deceased-donor kidney transplantation; LDKT, living-donor kidney transplantation.
The number of DCD DDKT March 15-April 30 was lower than expected across all categories of COVID-19 burden, with the IRR ranging from 0.500.620.76 in states with low COVID-19 rates to 0.140.210.33 at centers in states with very high COVID-19 rates (Table 4B). Regional and national imports also declined at centers in states with very high COVID-19 rates (IRR = 0.140.260.48 and 0.160.250.38, respectively).
4. DISCUSSION
In this national registry study of KT waitlist registrations, waitlist mortality, and rates of transplantation using data from the SRTR in the early COVID-19 era, we found the number of new registrations dropped by 18% below expected, DDKT dropped 24% below expected, and LDKT virtually came to a standstill. Additionally, we found that, though the number of waitlist deaths nationwide was not significantly higher than expected, it was 2.2-fold higher than expected in the 5 states with highest COVID-19 burden. There was substantial geographic heterogeneity, as these drops were greater among the states with highest COVID-19 incidence. These findings represent the dramatic impact of COVID-19 on KT; ongoing data collection and reporting are critical to continue to provide safe access to transplantation and limit the indirect downstream effects of this deadly disease.
COVID-19 is a novel disease and we are learning more about its impact on KT in real time. Therefore, early and frequent reporting on waitlist registrations, removals, and rates of KT is necessary to inform evolving clinical practices.
Our findings of decreased waitlist registrations coupled with increased waitlist inactivations are consistent with findings from our national survey in which we reported reduction in transplant activity.21 The dramatic reduction in DCD KT may be reflective of limited hospital beds, limited ventilators, and limited access to intensive care units (ICUs) and operating rooms (ORs); centers may be seeking to avoid the short-term complications (eg, DGF and longer hospital stay) that can result from DCD DDKT.26 , 27 Our finding of a virtual halt of LDKT is also consistent with our survey in which we found that early in the epidemic, 72% of centers had suspended LDKT, and is likely reflective of center-level priority for urgent or emergent operations. Our findings that most of the drops in activity were heightened in areas of high COVID-19 incidence is consistent with reports of diversion of healthcare resources.
Because waitlist deaths that occur outside of the transplant center may not be reported immediately to the transplant center and then to the OPTN, it is possible that this delay may have caused us to undercount total deaths in March and April 2020. However, the difference in waitlist mortality stratified by COVID-19 incidence is striking and unlikely to be confounded by reporting delay. In fact, if there were a delay, the apparent increase we saw in waitlist mortality in the high-incidence states may be even higher than reported. Though our results did not demonstrate major differences in changes to listing in the COVID-19 era based on race/ethnicity or insurance status, additional studies will be necessary to help inform the extent to which vulnerable transplant candidates were and are particularly affected by the epidemic.25
This study must be understood in the context of its limitations. National transplant registry data are captured by centers across the United States, which may have varying reporting standards and quality control. Additionally, our use of national registry data precludes assessment of key questions such as why a particular patient became inactive on the waitlist or cause of death information. Despite this limitation, our use of national registry data facilitates broadly generalizable inferences, especially in the context of linking data to state-level COVID-19 incidence rates. Furthermore, given the rapidly changing nature of the epidemic and limits on data availability, we limited our observed data to the last 2 weeks of March and the month of April, which may have underestimated the true rates of waitlist registrations, removals, and KT. These differences may become apparent only with additional data collection and analysis. Finally, there was lack of information on true incidence of COVID-19 because of significant variations and gaps in testing capacity that was especially apparent during this early window in the epidemic; this may have led us to misclassify some states with high COVID-19 burden but poor testing capacity. Nonetheless, even without comprehensive incidence and testing data, we were able to capture an increase in all-cause mortality in states with the highest reported COVID-19 incidence, even without testing data specific to waitlist registrants.
In summary, we found that in the early COVID-19 era in the United States, access to KT has been substantially limited as evidenced by decreased waitlist registrations, increased waitlist mortality increased in states with highest COVID-19 burden, decreased DDKT, and a virtual standstill in LDKT. These findings suggest that the epidemic has had a major impact on the KT population in the United States; we must be vigilant and learn and evolve rapidly to inform transplant practices and safely facilitate a reboot of KT.
ACKNOWLEDGMENTS
This research was made possible with generous support of the Ben-Dov family. This work was supported by grant numbers T32DK007713 (Boyarsky), F32DK113719 (Jackson), F32DK117563 (Kernodle), K24DK101828 (Segev), and K01DK101677 (Massie) from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and T32AI007291 (Werbel) from the National Institute of Allergy and Infectious Diseases (NIAID) of the National Institutes of Health. The analyses described here are the responsibility of the authors alone and do not necessarily reflect the views or policies of the US Department of Health and Human Services, nor does mention of trade names, commercial products or organizations imply endorsement by the US Government. The data reported here have been supplied by the Hennepin Healthcare Research Institute (HHRI) as the contractor for the Scientific Registry of Transplant Recipients (SRTR). The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy of or interpretation by the SRTR or the US Government.
DISCLOSURE
The authors of this manuscript have no conflicts of interest to disclose as described by the American Journal of Transplantation.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the Scientific Registry of Transplant Recipients (SRTR). Restrictions apply to the availability of these data, which were used under license for this study. Data are available the corresponding author with the permission of the SRTR.
Funding information National Institute of Diabetes and Digestive and Kidney Diseases, Grant/Award Number: F32DK117563, F32DK113719, K01DK101677, K24DK101828 and T32DK007713; National Institute of Allergy and Infectious Diseases, Grant/Award Number: T32AI007291
REFERENCES
- 1.Bogoch II, Watts A, Thomas-Bachli A, Huber C, Kraemer MUG, Khan K. Pneumonia of unknown aetiology in Wuhan, China: potential for international spread via commercial air travel. J Travel Med. 2020;27(2) doi: 10.1093/jtm/taaa008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 3.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhu NA, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382(10):929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gandolfini I, Delsante M, Fiaccadori E, et al. COVID-19 in kidney transplant recipients. Am J Transplant. 2020;20(7):1941–1943. doi: 10.1111/ajt.15891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhu L, Xu X, Ma KE, et al. Successful recovery of COVID-19 pneumonia in a renal transplant recipient with long-term immunosuppression. Am J Transplant. 2020;20(7):1859–1863. doi: 10.1111/ajt.15869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Michaels MG, La Hoz RM, Danziger-Isakov L, et al. Coronavirus disease 2019: implications of emerging infections for transplantation. Am J Transplant. 2020;20(7):1768–1772. doi: 10.1111/ajt.15832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sharma S, Lawrence C, Giovinazzo F. Transplant programmes during COVID-19: unintended consequences for health inequality. Am J Transplant. 2020;20(7):1954–1955. doi: 10.1111/ajt.15931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fernández-Ruiz M, Andrés A, Loinaz C, et al. COVID-19 in solid organ transplant recipients: a single-center case series from Spain. Am J Transplant. 2020;20(7):1849–1858. doi: 10.1111/ajt.15929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wall AE, Pruett T, Stock P, Testa G. Coronavirus disease 2019: utilizing an ethical framework for rationing absolutely scarce health-care resources in transplant allocation decisions [published online ahead of print 2020]. Am J Transplant. 10.1111/ajt.15914 [DOI] [PMC free article] [PubMed]
- 13.Zhong Z, Zhang Q, Xia H, et al. Clinical characteristics and immunosuppressants management of coronavirus disease 2019 in solid organ transplant recipients. Am J Transplant. 2020;20(7):1916–1921. doi: 10.1111/ajt.15928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cheng Y, Luo R, Wang K, et al. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020;97(5):829–838. doi: 10.1016/j.kint.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Su H, Yang M, Wan C, et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int. 2020;98(1):219–227. doi: 10.1016/j.kint.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fanelli V, Fiorentino M, Cantaluppi V, et al. Acute kidney injury in SARS-CoV-2 infected patients. Crit Care. 2020;24(1):155. doi: 10.1186/s13054-020-02872-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pan XW, Xu D, Zhang H, Zhou W, Wang LH, Cui XG. Identification of a potential mechanism of acute kidney injury during the COVID-19 outbreak: a study based on single-cell transcriptome analysis. Intensive Care Med. 2020;46(6):1114–1116. doi: 10.1007/s00134-020-06026-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kumar D, Tellier R, Draker R, Levy G, Humar A. Severe Acute Respiratory Syndrome (SARS) in a liver transplant recipient and guidelines for donor SARS screening. Am J Transplant. 2003;3(8):977–981. doi: 10.1034/j.1600-6143.2003.00197.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.AlGhamdi M, Mushtaq F, Awn N, Shalhoub S. MERS CoV infection in two renal transplant recipients: case report. Am J Transplant. 2015;15(4):1101–1104. doi: 10.1111/ajt.13085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fishman JA, Grossi PA. Novel coronavirus-19 (COVID-19) in the immunocompromised transplant recipient: #Flatteningthecurve. Am J Transplant. 2020;20(7):1765–1767. doi: 10.1111/ajt.15890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boyarsky BJ, Po-Yu Chiang T, Werbel WA, et al. Early impact of COVID-19 on transplant center practices and policies in the United States. Am J Transplant. 2020;20(7):1809–1818. doi: 10.1111/ajt.15915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Massie AB, Boyarsky BJ, Werbel WA, et al. Identifying scenarios of benefit or harm from kidney transplantation during the COVID-19 pandemic: a stochastic simulation and machine learning study [published online ahead of print 2020]. Am J Transplant. 10.1111/ajt.16117 [DOI] [PMC free article] [PubMed]
- 23.Massie AB, Kucirka LM, Segev DL. Big data in organ transplantation: registries and administrative claims. Am J Transplant. 2014;14(8):1723–1730. doi: 10.1111/ajt.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Louis TA, Zeger SL. Effective communication of standard errors and confidence intervals. Biostatistics. 2009;10(1):1–2. doi: 10.1093/biostatistics/kxn014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Webb Hooper M, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA. 2020;323(24):2466. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Orandi BJ, James NT, Hall EC, et al. Center-level variation in the development of delayed graft function after deceased donor kidney transplantation. Transplantation. 2015;99(5):997–1002. doi: 10.1097/TP.0000000000000450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Locke JE, Segev DL, Warren DS, Dominici F, Simpkins CE, Montgomery RA. Outcomes of kidneys from donors after cardiac death: implications for allocation and preservation. Am J Transplant. 2007;7(7):1797–1807. doi: 10.1111/j.1600-6143.2007.01852.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the Scientific Registry of Transplant Recipients (SRTR). Restrictions apply to the availability of these data, which were used under license for this study. Data are available the corresponding author with the permission of the SRTR.