Abstract
Objectives
To investigate the mental status of pregnant women and to determine their obstetric decisions during the COVID‐19 outbreak.
Design
Cross‐sectional study.
Setting
Two cities in China––Wuhan (epicentre) and Chongqing (a less affected city).
Population
A total of 1947 pregnant women.
Methods
We collected demographic, pregnancy and epidemic information from our pregnant subjects, along with their attitudes towards COVID‐19 (using a self‐constructed five‐point scale). The Self‐Rating Anxiety Scale (SAS) was used to assess anxiety status. Obstetric decision‐making was also evaluated. The differences between cities in all of the above factors were compared and the factors that influenced anxiety levels were identified by multivariable analysis.
Main outcome measures
Anxiety status and its influencing factors. Obstetric decision‐making.
Results
Differences were observed between cities in some background characteristics and women's attitudes towards COVID‐19 in Wuhan were more extreme. More women in Wuhan felt anxious (24.5 versus 10.4%). Factors that influenced anxiety also included household income, subjective symptom and attitudes. Overall, obstetric decisions also revealed city‐based differences; these decisions mainly concerned hospital preference, time of prenatal care or delivery, mode of delivery and infant feeding.
Conclusions
The outbreak aggravated prenatal anxiety and the associated factors could be targets for psychological care. In parallel, key obstetric decision‐making changed, emphasising the need for pertinent professional advice. Special support is essential for pregnant mothers during epidemics.
Tweetable abstract
The COVID‐19 outbreak increased pregnant women's anxiety and affected their decision‐making.
Keywords: COVID‐19, obstetric decisions, prenatal anxiety
Tweetable abstract
The COVID‐19 outbreak increased pregnant women's anxiety and affected their decision‐making.
 This article includes Author Insights, a video abstract available at https://vimeo.com/rcog/authorinsights16381
This article includes Author Insights, a video abstract available at https://vimeo.com/rcog/authorinsights16381
Introduction
In late December 2019, a cluster of pneumonia caused by a novel coronavirus (2019‐nCoV) was reported. 1 This pathogen was eventually named SARS‐CoV‐2, 2 with its associated disease COVID‐19. 3 By the first quarter of 2020, the COVID‐19 epidemic had become established in China. As of 3 May, a total of 82 877 cases and 4633 deaths were confirmed by the Chinese authorities. 4 Wuhan, as the epicentre in China, accounted for 60.7% of all cases and 83.5% of deaths. 5 Currently, SARS‐CoV‐2 has undoubtedly raised ‘a very high level of global risk’ and become the ‘public enemy number one’. 6 , 7 The latest data confirmed over 3 million cases and more than 0.2 million deaths outside of China. 8 The fight against COVID‐19 has become a global priority.
The rapid transmission and life‐threatening characteristics of COVID‐19 have been reported. The public, influenced by both accurate and erroneous information, are stressed. 9 All provinces in mainland China have adopted first‐level public health emergency (PHE) responses, including travel bans and executive orders on daily life. 10 Consequently, the Chinese New Year holiday was disrupted and public anxiety was further aggravated.
Pregnant women, as a vulnerable population, 11 may be of a particular concern, as anxiety has been described as a common psychological problem during pregnancy. 12 Recent discussions of pregnancies during the COVID‐19 outbreak have mainly focused on the therapeutic aspects; 13 , 14 , 15 little is known regarding mental status and psychological needs.
Prenatal care is vital to a healthy pregnancy. 16 The emergency traffic bans have made some medical resources inaccessible and may deter women from attending routine prenatal care. 17 Obstetricians have observed a dramatic decline in prenatal care attendance and births, as well as an increase in the caesarean section rate, all of which could threaten pregnancy outcomes. Relevant risks include ectopic pregnancy, delayed detection of fetal congenital anomalies, uncontrolled hypertension and pre‐eclampsia, post‐term delivery and dystocia. 18 , 19 , 20 These adverse events may have significant consequences, possibly greater than the COVID‐19 infection itself. 9 , 21 , 22 Greater science preparedness for pregnant women during public health emergencies has been advocated 23 but we know little about women's decisions during the COVID‐19 and other PHEs.
We conducted a survey among pregnant women in Wuhan (the hardest‐hit area) and Chongqing (a neighbouring city) during the COVID‐19 outbreak, to investigate anxiety status and its influencing factors, to determine and explain key prenatal decisions and, finally, to guide social and medical practice.
Methods
Study design and participants
This is a cross‐sectional study through a self‐administered questionnaire. The anonymous survey questionnaire was designed with four modules to collect data regarding: (1) background demographic, pregnancy and COVID‐19 status; (2) attitudes towards COVID‐19; (3) anxiety status using the Self‐Rating Anxiety Scale (SAS), 24 , 25 which is widely used and which has been demonstrated to have excellent reliability and validity in pregnancy; 26 , 27 (4) obstetric decisions, defined as those pertaining to important obstetric procedures. The content of the questionnaire was reviewed and pretested by professors in Psychiatry (XYZ and his colleagues) and Obstetrics (HBQ and XL). Eventually, the validity was established following appropriate revisions. The main content of the questionnaire is shown in Figure 1 and the English version of the full questionnaire is detailed in Appendix S1.
Figure 1.
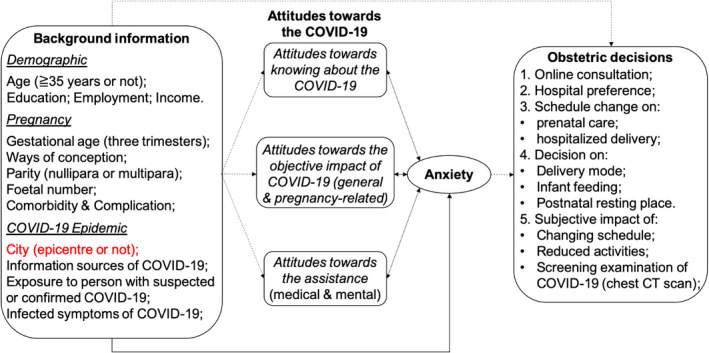
The main content of the questionnaire and the hypothesis of our study.
The questionnaires were distributed from 3 to 9 February 2020, mainly through a widely used, large data platform for pregnant mothers (YunYiTong, 28 covering more than 250 000 WeChat users nationwide), to those registered for prenatal care in hospitals in Wuhan and Chongqing. Two distribution strategies, namely, an individual WeChat message and advertising on the official accounts, were used. Additional questionnaires were distributed by obstetricians in both cities to those referred for outpatient services. Of note, a participant could only fill in this questionnaire once and only completed questionnaires could be submitted.
We followed relevant guidelines to ensure that the study was voluntary and confidential. The study was approved by the ethics committee of the First Affiliated Hospital of Chongqing Medical University, and an electronic informed consent was obtained before completing the questionnaire. The participants were not involved in the development of our study and none of the established core outcome sets has been used.
Procedures
Data cleaning
Data collection and input were automatically conducted. All data from the questionnaires were reviewed and the following subjects were excluded: (1) maternal age <14 or >60 years; (2) non‐pregnant, with the answer of ‘already delivered’ or ‘<0 or >45 weeks of gestational age’; (3) answers with wrong format; (4) illogical answers (choosing two options that contradicted each other in multiple‐choice questions). Figure 2 shows the flow chart of our study.
Figure 2.
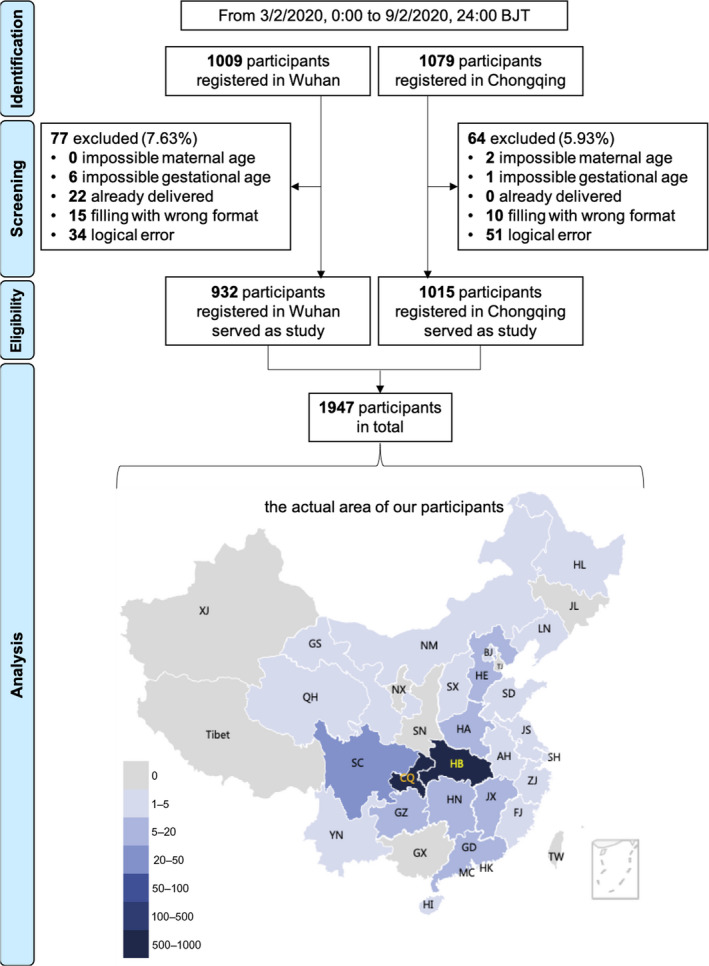
The flow chart of our study. CQ, Chongqing, an adjacent province‐level municipality of Hubei province; HB, Hubei province, the capital city of which is Wuhan.
Background information
The residency was based on both the city that the subjects registered for check‐up (Wuhan or Chongqing) and the region in which subjects actually resided at the time of survey. As a result of the Chinese Festival travel rush, these two addresses were not always the same. The registration area was used as the residency for the following analyses. As a reference, a map of the actual location of the participants is displayed in Figure 2.
We classified those aged ≥35 years as elderly gravida. Participants were assigned to one of three gestational age (GA) groups: (1) the first trimester: GA <14 complete weeks, (2) the second trimester: GA 14– 27+6 weeks, (3) the third trimester: GA ≥28 weeks. Parity was divided into nullipara and multipara. Other grouping standards are in accordance with the categorical options in the questionnaire (Appendix S1).
Assessment of attitudes towards COVID‐19
Items measuring attitudes towards COVID‐19 were designed on a five‐point scale from ‘totally disagree’ to ‘strongly agree’. Although this assessment was comprised of three sections (knowing about the COVID‐19, the objective impact of COVID‐19 and assistance given), these 11 questions were analysed separately (Appendix S1).
Assessment of anxiety status
The anxiety status was assessed using the Chinese version of the SAS, 25 and the responses to the scale were summed as a standard score and a degree of anxiety by an established method: 26 , 27 the scores from 20 items were calculated to obtain a raw score ranging from 20 to 80, and the standard score was calculated using the raw score multiplied by 1.25. A standard score ≥50 indicates anxiety status: standard scores of 50–59, 60–69 and ≥70 were considered mild, moderate and severe anxiety, respectively.
Assessment of obstetric decisions
The obstetric decisions pertained to: (1) online consultation; (2) hospital preference; (3) schedule on prenatal visit or delivery; (4) the mode of delivery, infant feeding and postnatal resting; (5) the five‐point subjective impact on pregnancy of the items including changing schedule, reduced activities, and possible screening examination of COVID‐19 (e.g. chest CT scan). These unstructured questions were analysed individually (Figure 1, Appendix S1).
Statistical analysis
We calculated the exact numbers and proportions for all variables in Wuhan and Chongqing, as well as the total for the two cities. Cronbach's alpha was used to assess the reliability of the anxiety scale. To compare the distribution of background, attitude, anxiety and obstetric decisions between the two cities, the Chi‐square test, Kruskal–Wallis test and Student's t test were used in accordance with the type of data.
All factors related to pregnant women's background and their attitude towards COVID‐19 were selected as independent variables. We used stepwise logistic regression models to estimate the effect of these factors on the anxiety status.
The Statistics Analysis Software version 9.4 (SAS Institute Inc., Cary, NC, USA) was used and a significance level set at P < 0.05 was applied. Figures presented were plotted with PRISM version 8.0 for windows (GraphPad Software Inc., San Diego, CA, USA).
The corresponding authors had full access to all of the data in the study and had the final responsibility to submit the article for publication.
Results
A total of 1947 valid questionnaires were received, 932 from Wuhan and 1015 from Chongqing. Of these women, 866 (92.9%) and 934 (92.0%) in Wuhan and in Chongqing, respectively, stayed where they were registered during the study period (Figure 2).
Background status
Participants reported diverse demographic, pregnancy and epidemic characteristics (Table S1). First, the general characteristics of their demographic background were of families with a middle‐level income and a working pregnant mother, although distribution differences existed between cities. Secondly, most pregnant women surveyed were in their second (32.8%) or third trimester (62.9%). There were more third‐trimester women in Wuhan (79.8 versus 47.4%). The majority of participants in both cities were nullipara and had experienced spontaneous singleton conception without comorbidity or complication, though Chongqing had a higher proportion of multiple pregnancies (4.4 versus 1.6%). Detailed distribution of comorbidity and complication is shown in Table S2. Third, information on COVID‐19 from official media were widely accepted during this period in both cities. The proportions of self‐reported symptoms were statistically the same in both cities, but the exposure history to diagnosed or suspected cases was more prevalent in Wuhan (4.7 versus 0.1%).
Attitudes towards COVID‐19
Attitudes towards COVID‐19 were more extreme in Wuhan, with statistically more responses of ‘totally disagree’ or ‘strongly agree’ (Figure 3). Overall, four‐fifths of mothers felt nervous about the objective impacts of COVID‐19, such as epidemic control, outdoor activity and person‐to‐person contact. Over 90% of the participants considered themselves vulnerable to this epidemic. Women in both cities held comparatively positive attitudes towards online medical consultation and psychological counselling, but differences still existed between cities (P < 0.001).
Figure 3.
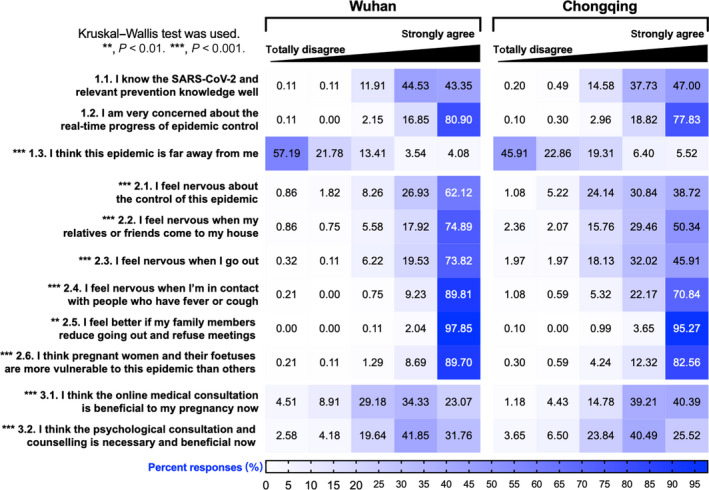
Participants' attitudes towards COVID‐19.
Prenatal anxiety and associated factors
Cronbach's alpha for the SAS was indicative of moderate‐to‐good internal reliability: 0.78. Specific details are shown in Figure S1.
As shown in Table 1, the participants in Wuhan had significantly higher anxiety scores. The mean standard score for anxiety was 43.97 (SD 8.71) for pregnant mothers in Wuhan, with a quarter of them scoring 50 or more. In Chongqing, an average score of 40.37 (SD 7.15) was reported, among whom about 90% scored lower than 50. The overall prevalence of anxiety during this period was 17.2%. Pregnant women in the epidemic hardest‐hit area (Wuhan) were much more anxious, 18.8 and 5.7% of whom underwent mild, and moderate/severe anxiety; the corresponding proportions were 9.4 and 1.1% in Chongqing, respectively. The effect of the different cities on the SAS standard score was small to medium (effect size [ES]: Cohen's d 0.44).
Table 1.
Participants' anxiety status
| City | Total (n = 1947) | t/χ2 | P‐value | ||
|---|---|---|---|---|---|
| Wuhan (n = 932) | Chongqing (n = 1015) | ||||
| Standard score * | 43.97 ± 8.71 | 40.37 ± 7.15 | 42.09 ± 8.13** | 9.9150 | <0.0001 |
| 42.50 (11.25) | 40.00 (10.00) | 41.25 (10.00) | |||
| Degree of anxiety *** | |||||
| No | 704 (75.54) | 909 (89.56) | 1613 (82.85) | 69.9681 | <0.0001 |
| Mild | 175 (18.78) | 95 (9.36) | 270 (13.87) | ||
| Moderate or severe | 53 (5.69) | 11 (1.08) | 64 (3.29) | ||
Comparations were conducted across the two cities.
Data are mean ± SD or median (IQR). Student's t‐test was used.
The Cohen's d for the SAS standard score was indicative of small‐to‐medium effect: 0.44.
Data are n (%). Kruskal–Wallis test was used.
The multivariable analysis (Table 2) showed the impact of each of the selected background or attitude factors on anxiety when controlling for all other factors. First, pregnant women from middle‐level income families were about half as likely to report anxiety than were those earning an extremely high or low wage. Second, women in Wuhan were about twice as likely to develop anxiety (odds ratio [OR] 1.83, 95% CI 1.38–2.41). Third, those who had fever, cough, diarrhoea or symptoms of suspected infection were five times as likely to have anxiety than were otherwise healthy women (OR 4.92, 95% CI 1.84–13.17).
Table 2.
Multivariable analysis of factors associated with anxiety
| Factor type | Influence factor | P‐value | OR (95% CI) |
|---|---|---|---|
| Background | Monthly household income, CNY | ||
| <5000 | 0.0238 | 1 (reference) | |
| 5000–9999 | 0.0336 | 0.6570 (0.4459–0.9680) | |
| 10 000–49 999 | 0.0027 | 0.5477 (0.3698–0.8113) | |
| 50 000 or more | 0.5673 | 0.8038 (0.3804–1.6985) | |
| Background | City (Chongqing as reference) | <0.0001 | 1.8263 (1.3814–2.4145) |
| Background | Infected symptoms (No symptom as reference) | 0.0015 | 4.9194 (1.8370–13.1737) |
| Attitude* | I know the SARS‐CoV‐2 and relevant prevention knowledge well | 0.0001 | 0.7114 (0.5988–0.8453) |
| Attitude* | I think this epidemic is a long distance from me | 0.0312 | 1.1268 (1.0108–1.2560) |
| Attitude* | I feel nervous about the control of this epidemic | 0.0222 | 1.2277 (1.0297–1.4637) |
| Attitude* | I feel nervous when I go out | 0.0061 | 1.3359 (1.0860–1.6434) |
| Attitude* | I think the online medical consultation is beneficial to my pregnancy now | <0.0001 | 0.6451 (0.5704–0.7296) |
| Attitude* | I think the psychological consultation and counselling is necessary and beneficial now | 0.0002 | 1.3145 (1.1396–1.5163) |
CI, confidence interval; CNY, Chinese yuan; OR, odds ratio.
The attitudes ranged from ‘totally disagree’ to ‘strongly agree’.
Furthermore, the attitudes towards COVID‐19 were associated with anxiety status. Those with relatively more knowledge about COVID‐19 and with a rational risk perception (not too nervous about epidemic control or going out), were less likely to be anxious. Additionally, positive attitudes towards online medical consultation demonstrated a protective feature from anxiety (OR 0.65, 95% CI 0.57–0.73), whereas those who opted for psychological consultation showed the opposite effect (OR 1.31, 95% CI 1.14–1.52).
Obstetric decisions
The participants' obstetric decisions are summarised in Table 3.
Table 3.
Participants' obstetric decisions
| City | Total | χ2 | P‐value | ||
|---|---|---|---|---|---|
| Wuhan | Chongqing | ||||
| Request of online consultation * | n = 932 | n = 1015 | n = 1947 | 8.6528 | 0.0033 |
| Yes | 703 (75.43) | 705 (69.46) | 1408 (72.32) | ||
| No | 229 (24.57) | 310 (30.54) | 539 (27.68) | ||
| Hospital preference ** | n = 932 | n = 1015 | n = 1947 | – | – |
| Refuse to go to any hospital | 390 (41.85) | 281 (27.68) | 671 (34.46) | 43.1368 | <0.0001 |
| Previous hospital of prenatal care | 319 (34.23) | 713 (70.25) | 1032 (53.00) | 253.0501 | <0.0001 |
| Hospital closer to home | 147 (15.77) | 122 (12.02) | 269 (13.82) | 5.7467 | 0.0165 |
| Large comprehensive hospital | 36 (3.86) | 107 (10.54) | 143 (7.34) | 31.8512 | <0.0001 |
| Specialized hospital of Obstetrics | 420 (45.06) | 145 (14.29) | 565 (29.02) | 223.4554 | <0.0001 |
| Prenatal care (plan, reason/way) ** | n = 499 | n = 796 | n = 1295 | – | – |
| Postponed, inconvenience | 461 (92.38) | 580 (72.86) | 1041 (80.39) | 74.1274 | <0.0001 |
| Postponed, afraid of infected | 194 (38.88) | 209 (26.26) | 403 (31.12) | 22.7947 | <0.0001 |
| As planned (on time), online | 4 (0.80) | 22 (2.76) | 26 (2.01) | 6.0026 | 0.0140 |
| As planned (on time), face‐to‐face | 13 (2.61) | 172 (21.61) | 185 (14.29) | 90.4530 | <0.0001 |
| Hospitalised delivery (plan, reason/way) ** | n = 203 | n = 87 | n = 290 | – | – |
| Postponed, inconvenience | 96 (47.29) | 27 (31.03) | 123 (42.41) | 6.5891 | 0.0103 |
| Postponed, afraid of infected (self) | 102 (50.25) | 37 (42.53) | 139 (47.93) | 1.4534 | 0.2280 |
| Postponed, afraid of infected (baby) | 104 (51.23) | 37 (42.53) | 141 (48.62) | 1.8464 | 0.1742 |
| Ahead of time, waiting for labour | 35 (17.24) | 9 (10.34) | 44 (15.17) | 2.2506 | 0.1336 |
| Ahead of time, caesarean in advance | 31 (15.27) | 6 (6.90) | 37 (12.76) | 3.8370 | 0.0501 |
| As planned (on time) | 39 (19.21) | 34 (39.08) | 73 (25.17) | 12.7634 | 0.0004 |
| Delivery mode * | n = 932 | n = 1015 | n = 1947 | 43.0645 | <0.0001 |
| Always CS | 174 (18.67) | 266 (26.21) | 440 (22.60) | ||
| Always VD | 588 (63.09) | 657 (64.73) | 1245 (63.94) | ||
| Change from CS to VD | 52 (5.58) | 31 (3.05) | 83 (4.26) | ||
| Change from VD to CS | 118 (12.66) | 61 (6.01) | 179 (9.19) | ||
| Infant feeding * | n = 932 | n = 1015 | n = 1947 | 38.4869 | <0.0001 |
| Always breastfeeding | 777 (83.37) | 919 (90.54) | 1696 (87.11) | ||
| Always bottle feeding | 23 (2.47) | 35 (3.45) | 58 (2.98) | ||
| Change from breast to bottle | 92 (9.87) | 48 (4.73) | 140 (7.19) | ||
| Change from bottle to breast | 40 (4.29) | 13 (1.28) | 53 (2.72) | ||
| Postnatal resting place * | n = 932 | n = 1015 | n = 1947 | 71.1758 | <0.0001 |
| Always home | 687 (73.71) | 847 (83.45) | 1534 (78.79) | ||
| Always PSI | 59 (6.33) | 94 (9.26) | 153 (7.86) | ||
| Change from home to PSI | 24 (2.58) | 5 (0.49) | 29 (1.49) | ||
| Change from PSI to home | 162 (17.38) | 69 (6.80) | 231 (11.86) | ||
| Impact of changing schedule *** | n = 932 | n = 1015 | n = 1947 | 191.4008 | <0.0001 |
| Completely no impact | 11 (1.18) | 12 (1.18) | 23 (1.18) | ||
| Almost no impact | 25 (2.68) | 81 (7.98) | 106 (5.44) | ||
| Slight impact | 149 (15.99) | 335 (33.00) | 484 (24.86) | ||
| Comparative impact | 378 (40.56) | 446 (43.94) | 824 (42.32) | ||
| Significant impact | 369 (39.59) | 141 (13.89) | 510 (26.19) | ||
| Impact of reduced activities *** | n = 932 | n = 1015 | n = 1947 | 113.0946 | <0.0001 |
| Completely no impact | 19 (2.04) | 24 (2.36) | 43 (2.21) | ||
| Almost no impact | 50 (5.36) | 110 (10.84) | 160 (8.22) | ||
| Slight impact | 194 (20.82) | 332 (32.71) | 526 (27.02) | ||
| Comparative impact | 371 (39.81) | 425 (41.87) | 796 (40.88) | ||
| Significant impact | 298 (31.97) | 124 (12.22) | 422 (21.67) | ||
| Impact of chest CT scan *** | n = 932 | n = 1015 | n = 1947 | 5.5295 | 0.0187 |
| Completely no impact | 9 (0.97) | 1 (0.10) | 10 (0.51) | ||
| Almost no impact | 20 (2.15) | 14 (1.38) | 34 (1.75) | ||
| Slight impact | 126 (13.52) | 99 (9.75) | 225 (11.56) | ||
| Comparative impact | 326 (34.98) | 377 (37.14) | 703 (36.11) | ||
| Significant impact | 451 (48.39) | 524 (51.63) | 975 (50.08) | ||
CS, caesarean section delivery; PSI, postnatal resting institution; VD, vaginal delivery.
Data are n (%). Comparations were conducted across the two cities.
Chi‐square test was used.
Multiple choice, Chi‐square test was used for each choice.
Kruskal–Wallis test was used.
Online consultation was requested by more than 70% of the participants, with a higher proportion in Wuhan (75.4 versus 69.5%). Absolute differences could be found between the two cities in hospital preference during this period. Of pregnant women in Wuhan, 41.9% reported refusal to go to any hospital recently, compared with 27.7% in Chongqing. Questionnaire responses revealed a general trust in previous (53.0%) and specialised (29.0%) hospitals among mothers, although differences existed in the proportion of that trust between cities (P < 0.0001).
Inconvenience caused by traffic bans raised significant concerns and, as a result, 80.4 and 42.4% of the 1947 participants in Wuhan and Chongqing, respectively, would defer their appointments for prenatal care and hospitalised delivery. These responses were more common in Wuhan than in Chongqing (92.4 versus 72.9% and 47.3 versus 31.0%, respectively). Fear of infection was another reason for delaying plans. With respect to prenatal care, a minority (16.3% in general) reported an ‘as planned’ visit. Very few mothers in Wuhan chose to complete their scheduled check online (n = 4) or face‐to‐face (2.6%). In Chongqing, however, 2.8 and 21.6% were willing to undertake their prenatal checks on time via the Internet and face‐to‐face. When it came to hospitalised delivery, 27.9% of all participants chose ‘ahead of time’; 15.2% wanted to be hospitalised earlier to wait for the onset of labour and 12.8% wanted to have a caesarean in advance. Only 25.2% of all women reported an ‘as planned’ hospitalised delivery; this proportion was higher in Chongqing (39.1 versus 19.2%).
Of pregnant women in Wuhan 12.7% would change delivery mode from vaginal delivery to caesarean section consequent upon the epidemic, whereas this proportion in Chongqing was halved (6.0%). However, the reverse change, from caesarean to vaginal delivery, was smaller (Wuhan 5.6%, Chongqing 3.1%). These city‐based differences and uneven changes in mode could also be seen in choices of infant feeding and postnatal resting. Overall, there were more women who preferred caesarean section, bottle feeding and postnatal rest at home during this period than before, especially in Wuhan.
Over 90% of pregnant women believed that there had been negative impact on their pregnancy through changing schedules and reduced activities; these subjective impacts were deemed to be more significant in Wuhan (P < 0.0001). Slightly more than half of the women (50.1%) thought the chest CT scan would significantly influence their pregnancy; this was more marked in Chongqing (51.6 versus 48.4%, P = 0.0187).
Discussion
Main findings
We report the first large cross‐sectional study of pregnant women's anxiety status and obstetric decision‐making during the outbreak of COVID‐19. We focused on the epicentre (Wuhan) and a neighbouring city (Chongqing) and involved 932 and 1015 participants, respectively.
Prenatal anxiety and associated factors
The global estimated prevalence of prenatal anxiety fluctuates between 14 and 24%. 29 , 30 , 31 Unfortunately, during the study period, the overall anxiety rate was 17.2%, with a higher rate in Wuhan (24.5%) than in Chongqing (10.4%). Such a difference was probably attributed to the higher exposure and the stricter restrictions in Wuhan.
We found that women with medium‐level incomes were protected from anxiety compared with those with high‐ or low‐level wages. No other demographic characteristics or factors related to pregnancy were found to be related to anxiety, although previous studies have suggested that age, education, occupation, parity and gestational age could influence anxiety. 31 , 32 , 33
Living in the epidemic centre and suffering subjective symptoms had major impacts on anxiety levels. We noted the high proportion of women who obtained their information through official media channels during the outbreak (84.3%), though the multivariable analysis did not show any association of information source with anxiety. There was higher frequency of exposure to COVID‐19 in the epicentre (Wuhan), although there were no differences in symptoms across cities (Table S1). However, symptoms, not exposure, were an independent influencing factor of anxiety.
Important attitudes towards COVID‐19, which were easy to manipulate psychologically (discussed below), were found to be associated with anxiety.
Our univariable analysis identified other potential factors that were correlated with anxiety (Table S3). We believe that the mechanism of epidemic on anxiety is unique, so regional differences greatly mask the effect of these conventional factors, which further reminds us to pay attention to prenatal anxiety during a PHE.
Obstetric decisions
Similar to anxiety, obstetric decisions revealed city‐based differences. Key choices changed, including the time of prenatal care or delivery, mode of delivery and infant feeding. These choices were translated into eventual outcomes, according to our clinical observations (Table S5).
Although the factors that influence obstetric decisions are difficult to determine fully, we conjecture that the severity of the epidemic is likely to be the dominant factor, although requests for online consultation and the subjective impact of chest CT scans were sensitive to gestational age (Tables 3 and S4).
Our hypothesis (Figure 1) is supported by evidence that anxiety can change prenatal decisions. 17 , 34 A mediation analysis should be conducted better to understand the pathway of prenatal anxiety to obstetric decisions during a PHE.
Strengths and limitations
Wuhan as the epidemic centre was included in our study. Chongqing, a nearby city, is a good comparison, not only because of its epidemic condition (less affected but still in the outbreak; Figure S2) but also because of the relatively high accessibility of data and the demographic comparability. Nevertheless, some limitations should be considered. First, the study design suggests the possibility of self‐report bias. Second, bias might exist, as data from uncompleted questionnaires were inaccessible. Third, the baseline was not completely balanced across cities. Efforts have been made to minimise biases: multiple centres were involved, the two cities provided a large and similar sample size, and sensitivity analysis was performed.
Our participants in Wuhan and Chongqing, generated relatively reliable and representative samples. More importantly, we hope that the real data from these two cities can serve as a reference and be promoted to more regions, especially to emerging epidemic areas worldwide. Appropriate adjustments are needed before cross‐region application. In the comparative results, Chongqing was hit harder than other regions farther away from Wuhan, which may weaken the impact gap of COVID‐19. Fortunately, descriptive parameters were recorded in each city and are likely to be accessible in cities that are the subjects of future studies.
Anxiety levels may have been underestimated. Pregnant women who are not registered on the platform or the hospital did not participate and may have a lower socio‐economic status and higher anxiety levels. 33 The inclusion of only completed questionnaires may also have led to an underestimation. In addition, the majority of pregnant women were in mid‐ or late trimester, whereas the highest level of anxiety reported previously was in early pregnancy. 33
This was a cross‐sectional study and long‐term cohort studies on post‐traumatic stress disorder or postpartum mental state are merited.
Interpretation
During an unpredictable period, such as a PHE, comprehensive recommendations on prenatal care are needed. Our findings can serve as a reference in the following aspects.
Psychological intervention
Prenatal anxiety, which may affect pregnancy outcomes, 21 , 22 , 35 , 36 should be considered carefully. Psychological intervention and corresponding public health measures during PHEs are necessary and require multidisciplinary cooperation. 9 These interventions could be: (1) to encourage the information from authoritative sources; (2) to understand correctly the susceptibility to disease; (3) to perceive the risk rationally (avoid exaggerated perception of symptoms); (4) to use online consultation and counselling.
Obstetric assistance
To prevent irreversible adverse events, deferral of prenatal visits or delivery should not be standard care. 37 Our findings also suggested that caesarean delivery and bottle feeding may have increased as women sought to avoid vertical transmission. For researchers, as new evidence comes to light, 14 , 15 , 38 such transmission is likely to be rejected. Still, lessons could be learnt from similar PHEs (SARS and MERS). 39 , 40 , 41 For obstetricians, the contingency plans should include the capacity to increase caesarean deliveries and manage potential perinatal infections; these plans need to be developed and implemented quickly. 42 Importantly, authoritative information on delivery and infant feeding should be available to prenatal mothers. The education of mothers concerning radiography during pregnancy should focus on its comparative safety and diagnostic necessity in order to decrease subjects' concerns.
Source of support
In our study, more than 70% of participants requested online support. Digital health merits increased investment.
The restrictive measures imposed, as a consequence of the crisis, have dual effects during PHEs, and a balance between epidemic control and mental pressure is required, taking into consideration the availability of medical resources. 12 , 31 , 43 Meanwhile, the rationale of opening ‘green channel’ for pregnant women has merit, as does support for this special group in the quarantine zones.
Conclusion
The outbreak aggravated prenatal anxiety, and the associated factors could be targets for psychological attention. In parallel, key obstetric decision‐making changed, emphasising the need for pertinent professional advice. Special support is essential for pregnant mothers during epidemics.
Disclosure of interests
None declared. Completed disclosure of interest forms are available to view online as supporting information.
Contribution to authorship
HBQ, XL and XYL contributed to the protocol design. MMC and GQS collected data. LS and YW analysed data. JZ, YS, HZ and PNB contributed to the interpretation of results. XYL drafted the manuscript and JHW proofread the manuscript. PNB also assisted with detailed editing of the manuscript for appropriate language. HBQ and XL revised the final version and are guarantors of this manuscript. All authors made substantial contributions to the paper and read and approved the final manuscript.
Details of ethics approval
The study was approved by the ethics committee of the First Affiliated Hospital of Chongqing Medical University on 14 February 2020 (ID:20200501). An electronic informed consent was obtained before completing the questionnaire.
Funding
This work was supported by grants from National Natural Science Foundation of China (No. 81771614 and No. 81771613), and the National Key Research and Development Program of China (No. 2016YFC1000407). The funders had no involvement in the study design, data collection and analysis, interpretation of data or preparation of the manuscript.
Data sharing
The data used and analysed during the current study are available from the corresponding author on reasonable request.
Supporting information
Figure S1. Self‐Rating Anxiety Scale (SAS).
Figure S2. The stage of the epidemic in each of the two cities.
Table S1. Participants' background of demographic, pregnancy and COVID‐19 epidemic.
Table S2. Comorbidity and complication of participants.
Table S3. Univariable analysis of background factors associated with anxiety.
Table S4. Participants' obstetric decisions (on the third trimester only).
Table S5. Current obstetric situations in two hospitals.
Appendix S1. The questionnaire.
Video S1. Author insights.
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Acknowledgements
We would like to thank Xinyu Zhou and his colleagues, professors in Psychiatry, for their advice on the questionnaire design and analysis. We also want to thank Professor Xiaoni Zhong, from the School of Public Health and Management in Chongqing Medical University, for her indispensable contributions to the statistical design and analysis. We would like to thank Dr Kim C. Liu from University of Cambridge for his proofreading and comments on the manuscript.
Liu X, Chen M, Wang Y, Sun L, Zhang J, Shi Y, Wang J, Zhang H, Sun G, Baker PN, Luo X, Qi H. Prenatal anxiety and obstetric decisions among pregnant women in Wuhan and Chongqing during the COVID‐19 outbreak: a cross‐sectional study. BJOG 2020; 127:1229–1240.
 This article includes Author Insights, a video abstract available at https://vimeo.com/rcog/authorinsights16381
This article includes Author Insights, a video abstract available at https://vimeo.com/rcog/authorinsights16381
Contributor Information
X Luo, Email: lxcqmu@outlook.com.
H Qi, Email: qihongbocy@gmail.com.
References
- 1. Wuhan Municipal Health Commission . Report of clustering pneumonia of unknown aetiology in Wuhan City. 2019. [http://wjw.wuhan.gov.cn/xwzx_28/gsgg/202004/t20200430_1199588.shtml]. Accessed 20 January 2020 (in Chinese).
- 2. Gorbalenya AE, Baker SC, Baric RS, de Groot RJ, Drosten C, Gulyaeva AA, et al. Severe acute respiratory syndrome‐related coronavirus: the species and its viruses––a statement of the Coronavirus Study Group. bioRxiv 2020. 10.1101/2020.02.07.937862 [DOI] [Google Scholar]
- 3. World Health Organization (WHO) . WHO Director‐General's remarks at the media briefing on 2019‐nCoV on 11 February 2020 [www.who.int/dg/speeches/detail/who‐director‐general‐s‐remarks‐at‐the‐media‐briefing‐on‐2019‐ncov‐on‐11‐february‐2020]. Accessed 11 February 2020.
- 4. National Health Commission of the People's Republic of China . Update on epidemic situation of novel coronavirus‐infected pneumonia (COVID‐19) by 24:00 on 2 May, 2020 [www.nhc.gov.cn/xcs/yqtb/202005/aba9ba870fed480fbc01c7d7b35eb3a7.shtml]. Accessed 3 May 2020 (in Chinese).
- 5. Health Commission of Hubei Province . Situation updates of coronavirus disease 2019 (COVID‐19) in Hubei Province by 24:00 on 2 May, 2020 [http://wjw.hubei.gov.cn/bmdt/ztzl/fkxxgzbdgrfyyq/xxfb/202005/t20200503_2258252.shtml]. Accessed 3 May 2020 (in Chinese).
- 6. World Health Organization (WHO) . WHO Emergencies Press Conference on novel coronavirus – 11 February 2020 [www.who.int/docs/default‐source/coronaviruse/transcripts/who‐audio‐emergencies‐coronavirus‐full‐press‐conference‐11feb2020‐final.pdf?sfvrsn=e2019136_2]. Accessed 20 February 2020.
- 7. World Health Organization (WHO) . WHO Director‐General's opening remarks at the media briefing on COVID‐19––28 February 2020 [www.who.int/dg/speeches/detail/who‐director‐general‐s‐opening‐remarks‐at‐the‐media‐briefing‐on‐covid‐19‐‐‐28‐february‐2020]. Accessed 3 March 2020.
- 8. World Health Organization (WHO) . Coronavirus disease 2019 (COVID‐19) situation report––103. 2 May 2020 [www.who.int/docs/default‐source/coronaviruse/situation‐reports/20200502‐covid‐19‐sitrep‐103.pdf?sfvrsn=d95e76d8_4]. Accessed 3 May 2020.
- 9. Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019‐nCoV epidemic: address mental health care to empower society. Lancet 2020;395:e37–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. China Daily . Tibet activates highest‐level public health alert. 2020. [www.chinadaily.com.cn/a/20200]. Accessed 4 February 2020.
- 11. National Health Commission of the People's Republic of China [www.nhc.gov.cn/fys/s7902/202002/de2d62a5711c41ef9b2c4b6f4d1f2136.shtml]. Accessed 12 February 2020 (in Chinese).
- 12. Yan W, Wang X, Kuang H, Chen Y, Baktash MB, Eskenazi B, et al. Physical activity and blood pressure during pregnancy: mediation by anxiety symptoms. J Affect Disord 2020;264:376–82. [DOI] [PubMed] [Google Scholar]
- 13. National Health Commission of the People's Republic of China . Notice on strengthening maternal disease treatment and safe midwifery during the prevention and control of new coronavirus pneumonia [www.nhc.gov.cn/xcs/zhengcwj/202002/4f80657b346e4d6ba76e2cfc3888c630.shtml]. Accessed 8 February 2020 (in Chinese).
- 14. Qiao J. What are the risks of COVID‐19 infection in pregnant women? Lancet 2020;395:760–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID‐19 infection in nine pregnant women: a retrospective review of medical records. Lancet 2020;395:809–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dowswell T, Carroli G, Duley L, Gates S, Gulmezoglu AM, Khan‐Neelofur D, et al. Alternative versus standard packages of antenatal care for low‐risk pregnancy. Cochrane Database Syst Rev 2015;(7):CD000934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cheng BH, Chen JH, Wang GH. Psychological factors influencing choice of prenatal diagnosis in Chinese multiparous women with advanced maternal age. J Matern Fetal Neonatal Med 2019;32:2295–301. [DOI] [PubMed] [Google Scholar]
- 18. Chou D, Daelmans B, Jolivet RR, Kinney M, Say L, Every Newborn Action Plan Ending Preventable Maternal Mortality Working Groups . Ending preventable maternal and newborn mortality and stillbirths. BMJ 2015;351:h4255. [DOI] [PubMed] [Google Scholar]
- 19. Obstetrics Subgroup, Chinese Society of Obstetrics and Gynecology, Chinese Medical Association . Guideline of preconception and prenatal care (2018). Chin J Obstet Gynecol 2018;53:7–13 (in Chinese). [Google Scholar]
- 20. Brown MA, Magee LA, Kenny LC, Karumanchi SA, McCarthy FP, Saito S, et al. The hypertensive disorders of pregnancy: ISSHP classification, diagnosis & management recommendations for international practice. Pregnancy Hypertens 2018;13:291–310. [DOI] [PubMed] [Google Scholar]
- 21. Dunkel Schetter C, Tanner L. Anxiety, depression and stress in pregnancy: implications for mothers, children, research, and practice. Curr Opin Psychiatry 2012;25:141–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rose MS, Pana G, Premji S. Prenatal maternal anxiety as a risk factor for preterm birth and the effects of heterogeneity on this relationship: a systematic review and meta‐analysis. Biomed Res Int 2016;2016:8312158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Faherty LJ, Rasmussen SA, Lurie N. A call for science preparedness for pregnant women during public health emergencies. Am J Obstet Gynecol 2017;216:34 e1–5. [DOI] [PubMed] [Google Scholar]
- 24. Zung WW. A rating instrument for anxiety disorders. Psychosomatics 1971;12:371–9. [DOI] [PubMed] [Google Scholar]
- 25. Wang ZY. Chinese version of Zung's self‐rating anxiety scale. J Shanghai Psychiatry 1984;2:73–4 (in Chinese). [Google Scholar]
- 26. Ma X, Wang Y, Hu H, Tao XG, Zhang Y, Shi H. The impact of resilience on prenatal anxiety and depression among pregnant women in Shanghai. J Affect Disord 2019;250:57–64. [DOI] [PubMed] [Google Scholar]
- 27. Glynn LM, Schetter CD, Hobel CJ, Sandman CA. Pattern of perceived stress and anxiety in pregnancy predicts preterm birth. Health Psychol 2008;27:43–51. [DOI] [PubMed] [Google Scholar]
- 28. YunYiTong. Version 1.0 [www.cqyyt.net/]. Accessed 2 February 2020 (in Chinese).
- 29. World Health Organization (WHO) . Maternal Mental Health and Child Health and Development in Resource‐Constrained Settings: Report of a UNFPA/WHO International Expert Meeting: The Interface between Reproductive Health and Mental Health. Geneva: World Health Organization Press; 2009. [Google Scholar]
- 30. Bennett HA, Einarson A, Taddio A, Koren G, Einarson TR. Prevalence of depression during pregnancy: systematic review. Obstet Gynecol 2004;103:698–709. [DOI] [PubMed] [Google Scholar]
- 31. Tang X, Lu Z, Hu D, Zhong X. Influencing factors for prenatal stress, anxiety and depression in early pregnancy among women in Chongqing, China. J Affect Disord 2019;253:292–302. [DOI] [PubMed] [Google Scholar]
- 32. Kang YT, Yao Y, Dou J, Guo X, Li SY, Zhao CN, et al. Prevalence and risk factors of maternal anxiety in late pregnancy in China. Int J Environ Res Public Health 2016;13:468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Zhang Y, Muyiduli X, Wang S, Jiang W, Wu J, Li M, et al. Prevalence and relevant factors of anxiety and depression among pregnant women in a cohort study from south‐east China. J Reprod Infant Psychol 2018;36:519–29. [DOI] [PubMed] [Google Scholar]
- 34. Sahin NH, Gungor I. Congenital anomalies: parents' anxiety and women's concerns before prenatal testing and women's opinions towards the risk factors. J Clin Nurs 2008;17:827–36. [DOI] [PubMed] [Google Scholar]
- 35. Nasreen HE, Kabir ZN, Forsell Y, Edhborg M. Low birth weight in offspring of women with depressive and anxiety symptoms during pregnancy: results from a population based study in Bangladesh. BMC Public Health 2010;10:515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kogan MD, Alexander GR, Kotelchuck M, Nagey DA. Relation of the content of prenatal care to the risk of low birth weight. Maternal reports of health behavior advice and initial prenatal care procedures. JAMA 1994;271:1340–5. [PubMed] [Google Scholar]
- 37. Liu XY, Shi Y, Chen M, Zhang J, Wang JH, Baker PN, et al. Obstetrical view of COVID‐19: a call for appropriate prenatal care during public health emergencies. Authorea 2020. 10.22541/au.158575936.68181007 [DOI] [Google Scholar]
- 38. Zheng QL, Duan T, Jin LP. Single‐cell RNA expression profiling of ACE2 and AXL in the human maternal–fetal interface. Reprod Dev Med 2020;4:7–10 [Google Scholar]
- 39. Alfaraj SH, Al‐Tawfiq JA, Memish ZA. Middle East Respiratory Syndrome Coronavirus (MERS‐CoV) infection during pregnancy: report of two cases & review of the literature. J Microbiol Immunol Infect 2019;52:501–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Wong SF, Chow KM, Leung TN, Ng WF, Ng TK, Shek CC, et al. Pregnancy and perinatal outcomes of women with severe acute respiratory syndrome. Am J Obstet Gynecol 2004;191:292–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Maxwell C, McGeer A, Tai KFY, Sermer MN. 225‐Management guidelines for obstetric patients and neonates born to mothers with suspected or probable severe acute respiratory syndrome (SARS). J Obstet Gynaecol Can 2017;39:e130–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Qi H, Luo X, Zheng Y, Zhang H, Li J, Zou L, et al. Safe delivery for COVID‐19 infected pregnancies. BJOG 2020;127:927–29. [DOI] [PubMed] [Google Scholar]
- 43. Rubin GJ, Wessely S. The psychological effects of quarantining a city. BMJ 2020;368:m313. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Self‐Rating Anxiety Scale (SAS).
Figure S2. The stage of the epidemic in each of the two cities.
Table S1. Participants' background of demographic, pregnancy and COVID‐19 epidemic.
Table S2. Comorbidity and complication of participants.
Table S3. Univariable analysis of background factors associated with anxiety.
Table S4. Participants' obstetric decisions (on the third trimester only).
Table S5. Current obstetric situations in two hospitals.
Appendix S1. The questionnaire.
Video S1. Author insights.
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material


