Abstract
Importance
The COVID‐19 pandemic is changing how health care providers practice. As some telemedicine and telecommunication support tools have been incorporated into the otolaryngology practice in response to safety and access demands, it is essential to review how these tools and services can help facilitate facial trauma evaluation during a time when clinical resources are limited.
Objective
To review applications of telemedicine for the evaluation of facial trauma to better direct utilization of these methods and technologies during times of limited access to clinical resources such as the COVID‐19 pandemic.
Methods
A systematic review was conducted using PubMed, Embase, and Web of Science.
Results
After screening 158 titles and abstracts, we identified 16 eligible studies involving facial trauma evaluation using telemedicine. Telemedicine opportunities for facial trauma evaluation have the potential to be developed in the areas of multidisciplinary remote consultations, facial trauma triage, patient engagement, and postoperative follow‐up.
Conclusion
The COVID‐19 pandemic is posing obstacles for both providers and patients in the delivery of health care at a time of limited clinical resources. Telemedicine may provide a potential useful tool in the evaluation and triage of facial injuries and patient engagement.
Keywords: COVID‐19, facial trauma, telemedicine
The COVID‐19 pandemic is posing obstacles for both providers and patients in the delivery of health care at a time of limited clinical resources. Telemedicine may provide a potential tool in the evaluation and triage of facial trauma.

1. INTRODUCTION
With the rapid, worldwide spread of the 2019 novel coronavirus disease (COVID‐19) caused by SARS‐CoV‐2, practicing clinicians and health care workers at the front lines of essential care are impacted by concerns of exposure, infection, and the allocation of critical resources to patients in need. During this pandemic, personal protective equipment (PPE) can be in short supply, and the potential aerosolization of respiratory droplets from the upper aerodigestive tract have put otolaryngologists and other providers at higher risk for contracting COVID‐19 while examining patients or performing procedures. 1 , 2 , 3 , 4 , 5 To maintain patient safety and limit viral transmission at all health care facilities, a tiered framework focused on maintaining critical care has been enacted while reducing nonemergent, elective medical services.
Facial trauma remains a significant morbidity of concern as patients continue to enter the emergency room from falls, assaults, or accidents. 6 , 7 , 8 Evaluation of acute facial injuries requires considerable provider‐patient interaction as the thorough examination process guides successful treatment. Risk of cross infection increases during patient evaluations and head/neck surgeries, especially when clinicians come in close contact with the anatomical nasal and oral mucosa areas where the virus can thrive. 6 Opportunities for technology‐based clinical evaluations are much needed.
Telemedicine, according to the Institute of Medicine (IOM), is the “use of electronic information and communications technologies to provide and support health care when distance separates participants.” 9 Often used interchangeably with the broader Medicare term, telehealth, telemedicine has the potential to improve communication in otolaryngology, save time, and aid in diagnosis. 10 With the recent change in Centers for Medicare & Medicaid (CMS) reimbursements, and establishment of social distancing practices from shelter‐in‐place orders around the nation, telehealth visits and synchronous virtual services offered by health care institutions have ramped up significantly in a matter of weeks. 4 , 10
Other than routine telephone follow‐up calls, few otolaryngologists utilized telemedicine in their practice 20 years ago. 11 As technologies developed and internet access improved over the years, however, some physicians envisioned telemedicine's practical potential for facilitating medical care, such as implementing tele‐tools for consultation to the underserved, proctored surgery, treatment, education, and research. 11 , 12 Early adoption in telemedicine for otolaryngology began in rural areas alongside the improvement of otologic image quality. 13
Today, in light of this unprecedented time during the COVID‐19 pandemic, telemedicine has become more relevant to give patients the supportive care they need and at the same time reduce exposure risks to other patients and clinicians. With the increased adoption of telemedicine in otolaryngology practice and growing concern for subsequent “waves” of infection, we review the literature in regard to the applications of telemedicine in the evaluation of facial trauma.
2. METHODS
A systematic review was conducted in PubMed, Embase, and Web of Science using the search terms: “telemedicine,” “telehealth,” “remote monitoring,” “virtual visit,” “virtual consultation,” “facial trauma,” “facial,” “facial injury,” “face trauma,” and “face injury.” Supplementary Appendix A: Search Strings. The search was limited by dates between June 1, 1997 and April 30, 2020. This review followed the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) guidelines. 14
Titles, abstracts, and selected articles were independently assessed by three authors (M.S., J.H., and V.N.). The population of interest was patients who experienced facial trauma and received a clinical evaluation. We took into consideration all modalities of telemedicine or telehealth application, in addition to any medical tool that may potentially serve as a telemedicine application. We read original peer‐reviewed research studies on the population of interest. Included were randomized controlled trials (RCT), non‐RCTs, case‐control studies, cohort studies, cross‐sectional studies, case series, case reports, and qualitative research studies. We also added additional sources through reference review. Excluded were narrative reviews, articles without full‐text access, and non‐English language articles. We also excluded intervention studies that did not have a telemedicine approach. Disagreements and discrepancies between reviewers were discussed and resolved through consensus.
3. RESULTS
A total of 257 references were identified in the database search, of which 158 were considered eligible for inclusion based on the assessment of title and abstract. Upon full article review, 16 original peer reviewed research articles were selected for final inclusion (Figure 1).
FIGURE 1.
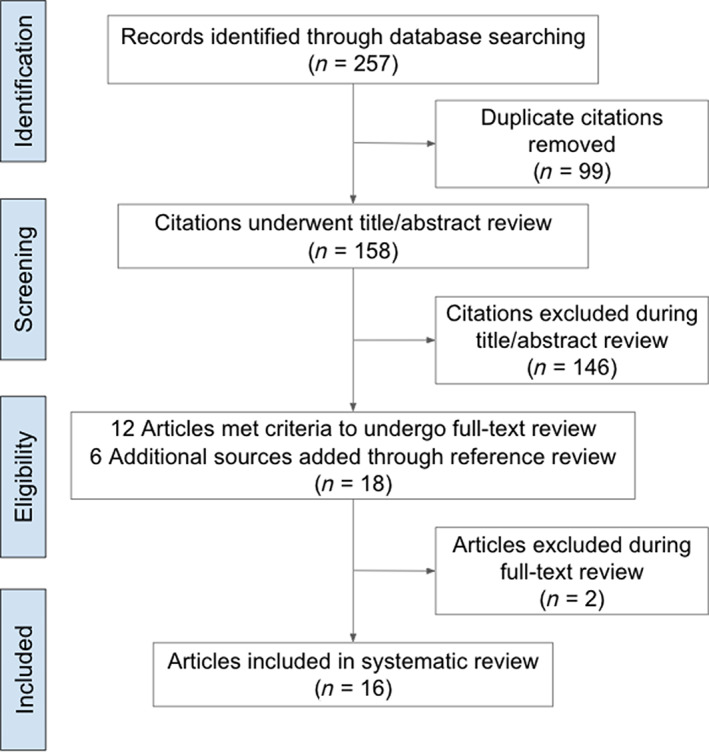
PRISMA flow diagram of systematic review
Due to the heterogeneity in research methodology and populations studied, formal meta‐analysis was not conducted. Instead, we present a narrative synthesis of the results for the key domains of facial trauma evaluation using telemedicine. Table 1 shows the distribution of included articles across different domains of telemedicine.
TABLE 1.
Distribution of included studies across different domains of telemedicine
| Domain | Study count a | References |
|---|---|---|
| Function | ||
| Functional trauma assessment | 13 | Millesi et al. (1997), Jacobs et al. (2002), Pap et al. (2002), Moumoulidis et al. (2007), Walker et al. (2011), Hutchison et al. (2012), Farook et al. (2013), Van Dillen et al. (2013), Fonseca et al. (2016), Paik et al. (2017), Ambroise et al. (2019), Brucoli et al. (2019), Tan et al. (2019) |
| Evaluation/diagnosis | ||
| Accuracy or concordance of diagnosis | 5 | Jacobs et al. (2002), Pap et al. (2002), Moumoulidis et al. (2007), Paik et al. (2017), Tan et al. (2019) |
| Teleradiology | 5 | Millesi et al. (1997), Jacobs et al. (2002), Chiao et al. (2005), Brucoli et al. (2019), Mitsuno et al. (2019) |
| Traumatic facial skin injuries | 3 | Walker et al. (2011), Van Dillen et al. (2013), Farook et al. (2013) |
| Triage | 5 | Hutchison et al. (2012), Farook et al. (2013), Fonseca et al. (2016), Ambroise et al. (2019), Brucoli et al. (2019) |
| Referral | 5 | Pap et al. (2002), Hutchison et al. (2012), Farook et al. (2013), Paik et al. (2017), Ambroise et al. (2019) |
| Facial trauma monitoring | 2 | Chiao et al. (2005), Walker et al. (2011) |
| Facial trauma treatment advice | 3 | Millesi et al. (1997), Van Dillen et al. (2013), Mitsuno et al. (2019) |
| Facial trauma follow‐up | ||
| Patient engagement | 2 | Moumoulidis et al. (2007), Walker et al. (2011) |
| Telemedicine technology | ||
| Store‐and‐forward | 5 | Jacobs et al. (2002), Pap et al. (2002), Farook et al. (2013), Brucoli et al. (2019), Tan et al. (2019) |
| Live interactive | 8 | Millesi et al. (1997), Jacobs et al. (2002), Chiao et al. (2005), Hutchison et al. (2012), Van Dillen et al. (2013), Fonseca et al. (2016), Ambroise et al. (2019), Mitsuno et al. (2019) |
| Remote monitoring | 1 | Chiao et al. (2005) |
| Mobile health application/device | 7 | Jacobs et al. (2002), Chiao et al. (2005), Moumoulidis et al. (2007), Walker et al. (2011), Fonseca et al. (2016), Paik et al. (2017), Ambroise et al. (2019) |
There may be overlap the studies for the different domains.
This review found telemedicine technologies functioning as facilitators to facial trauma assessment, monitoring, treatment, and/or follow‐up. The majority of articles (88%; 14/16) mentioned some form of assessment, which included using telemedicine tools to aid in diagnosis, triage, and referrals. Telemedicine technologies were described to be either store‐and‐forward, live interactive, remote monitoring, and/or mobile health application/device (Table 1).
3.1. Teleradiology
Teleradiology was utilized in the evaluation of patients with facial trauma. 15 , 16 , 17 , 18 , 19 Brucoli et al 15 retrospectively investigated the efficacy of teleradiology in triaging 605 traumatic facial fractures in 467 patients treated across 6 peripheral hospitals and a central maxillofacial surgery center. A teleradiology system was used between emergency medicine physicians and maxillofacial surgeons to share radiographic and clinical information to determine indication for surgery. Patients were reassessed at the central referral center to confirm the telemedicine decisions. Preliminary indications were correct based on teleradiology for all (68 surgical candidates; 223 nonsurgical candidates). Out of 176 patients with “possible” surgical indications, 27 were offered surgery. Of note, the indication for surgical intervention for naso‐orbital‐ethmoid fractures was underestimated using teleradiology. Teleradiology allowed for accurate triaging of patients with orbitozygomatic maxillary complex, orbital wall, mandibular, maxillary, nasal, Le Fort, frontal sinus, and dentoalveolar fractures. 15
Jacobs et al. 16 highlighted the value of image quality through a prospective study comparing radiographic findings, diagnosis, confidence of read, and assessment of image quality of 20 facial plain radiographs. These preselected, plain radiographs, with and without mandibular and zygomatic fractures, were presented to eight oral maxillofacial surgery (OMFS) and eight emergency medicine (EM) physicians to interpret. OMFS physicians using plain radiographs had the highest sensitivity (100%) and specificity (84%) for diagnosis of fractures, followed by the EM physicians using plain radiographs (90% sensitivity, 77% specificity, respectively), then OMFS with telemedicine images (86% sensitivity, 80% specificity, respectively). Rates of diagnosis were similar between OMFS utilizing telemedicine and EM physicians utilizing plain radiographs. Telemedicine images were associated with lower image quality ratings, lower sensitivity, and lower confidence of diagnosis. Although a powerful adjunctive tool for the diagnosis of facial fractures, teleradiology must be used in conjunction with clinical information and with a strong emphasis on image quality. 16
In a case report, Millesi et al. 17 first described the use of real‐time teleradiology and telemedicine in the intraoperative setting. For a patient requiring repair of the zygomatico‐orbital, central midface, and comminuted maxillary fractures, the authors used the Virtual Patient System remotely. This real‐time fusion of radiologic, video, photographic, and 3D modeling data, guided position, symmetry, planning, and evaluation. Additional advantages of this technology mentioned in the article included education and training of surgeons. 17
Mitsuno et al. 18 noted that telemedicine may have an expanding role in training and mentoring of surgeons treating facial trauma. Surgical models of the face were used in conjunction with shared real‐time video communication (Skype) and virtual surgical field marking through the head‐mounted, mixed reality device (Microsoft HoloLens). It was demonstrated that surgeons could have a resource to guide trainees through incisions, dissections, osteotomies, reductions, and suturing of facial models with complex facial fractures or cleft lip. This case series demonstration showed fast response with no voice delay and video latency of less than 0.5 seconds, with overall consistent image quality permitting landmark identification and comprehension of the surgical situation.
Telementoring shown with the Mitsuno et al. 18 study, was also highlighted in the Chiao et al. 19 case report describing a telemedicine demonstration where a comprehensive examination of the eye with ultrasound was conducted by minimally‐trained crew members in space using reference cards, and real‐time guidance from a remote radiologist. This remote guidance yielded ocular images of diagnostic quality that could guide remote decision‐making—suggesting possible applications in craniofacial trauma patients with a remote expert guiding a responder in image acquisition. 19
3.2. Traumatic facial skin injuries
The evaluation of traumatic facial skin wounds was explored with telemedicine tools. 20 , 21 , 22 Van Dillen et al. 20 compared bedside videoconference evaluations with in‐person assessments of acute traumatic wounds of patients presenting in the emergency room (n = 173). They observed correlation coefficients of .96 and .85 for the primary outcomes of wound length and depth, respectively, and agreement on wound characteristics ranged from 84% to 100%. 20 Management choices were concordant in 94% of cases. Video evaluations showed high sensitivities and specificities in determining wound severity and need for hospitalization. The findings in this study supported the use of mobile video conferencing in the work‐up and treatment of traumatic skin wounds. 20
In a retrospective single center study, Farook et al. 21 compared the utility and efficacy of photographs via telemedicine in the evaluation of pediatric facial lacerations (n = 143). There was no significant difference in surgical intervention rates between the pediatric patients with facial lacerations in the telemedicine group and the control group. The most common site of injury was the lip. None of the patients who underwent conservative treatment in the telemedicine group required a second evaluation. Telemedicine photographs, together with clinical history, can be effective in managing children with facial lacerations. 21 Walker et al. 22 studied the feasibility of mobile phone pictures as a follow‐up tool to track the healing progress of facial laceration repairs (see patient engagement section).
3.3. Telemedicine via mobile device applications
The utility of specialized mobile device applications in the management of patients with facial trauma has been advocated to improve security of medical data, traceability of patient information sharing, improve communication between providers, and also facilitate epidemiological data collection. 23 , 24 , 25 Paik et al. 24 assessed a remote consulting software in the emergency department (n = 42). Software utilization demonstrated a 5‐fold quicker response time when compared to in‐person consultations. There was an overall congruence of treatment recommendation (90.5%) between in‐hospital and remote consultations compared to previous studies noting general agreement rates of 70% to 80% between physicians. 24 The software offered an accurate and efficient consulting service for emergency department (ED) clinicians and a method for reducing ED wait time and improving patient satisfaction. 24
A prospective study by Fonseca et al. 26 compared the independent evaluation of patients with traumatic facial injuries in the ED by an in‐person surgery team vs a remote telemedicine team using videoconferencing by smartphone and tablet (n = 50). There was substantial concordance of physical exam findings (κ = 0.720), and almost perfect concordance of facial CT scan findings (κ = 0.899) and treatment recommendations (κ = 0.891) as assessed by a standardized questionnaire. Telemedicine was shown to be feasible and accurate in the evaluation of facial trauma, with the potential to optimize triage, length of stay, transfers, and patient cost in part by extending the possible area covered by a single surgeon compared to face‐to‐face evaluations. 26
A repeated measures study by Tan et al. 27 compared the reliability of telemedicine video evaluation of facial nerve paralysis (FNP) in 28 patients using the House‐Brackmann, Sydney, and Sunnybrook facial grading systems evaluated by 7 clinicians. All three scoring systems demonstrated strong reliability in both mediums, with weak reliability in assessment of synkinesis. The significant variation in agreement between the assessments done by video recording vs face to face evaluation may have been attributed to the 2D nature of the video recording. This study suggested that there is promise in utilizing video recordings for the assessment of FNP, but there is need for improvement and further testing using more real time images. 27
3.4. Follow up by activating patient engagement
Two studies explored the potential for using telemedicine tools to engage the patient in participating in their own facial trauma evaluation and follow up. 22 , 28 Moumoulidis et al. 28 conducted a prospective single center study (n = 25) to assess the use of mobile phone photographs in diagnosing nasal fractures. Patients were asked in a questionnaire to judge their own perceived nasal shape change. They were also asked to take photographs of their nose and face with a mobile phone, to be reviewed by a clinician, to determine the presence of a fracture and indication for surgery. The same clinician then conducted an in‐person clinical assessment to compare results. The camera assessment failed to identify 62% of nasal bone deviation cases determined by clinical examination. The patients' self‐assessments were 100% sensitive whereas the image assessment had only a 38% sensitivity for detecting a deviated nose. It was determined that the use of photographs alone, without a telephone consultation or high resolution image, was considered unfeasible for diagnosis of nasal fractures. 28
The patients who refused to participate in the Moumoulidis et al. 28 study cited reasons of feeling embarrassed and not wanting to have their picture taken. The participants of the Walker et al. 22 cohort study (n = 50), on the other hand, all agreed to send mobile phone pictures of their facial lacerations to their clinician to show progress after repair in the emergency room, but none of the patients complied. Despite being reminded with a 6‐ and 12‐month automated call, and reporting high satisfaction with their scar at those time intervals, no patients sent follow‐up pictures—leaving the research team to suspect that some patients may be unable to use the mobile phone features despite owning a device, and some patients may perceive a lack of benefit from follow‐up because the scar revision healed as expected. 22
3.5. Practice patterns
Hutchinson et al. 12 conducted a retrospective study assessing telemedicine practice patterns for the referral of facial trauma patients to a trauma center (n = 137). Only one patient underwent an interfacility telemedicine evaluation during this study. A third of the patients were discharged by the trauma clinic after one appointment, and 22.2% of patients failed to attend follow‐up appointments. Telemedicine resources were highly underutilized in their region, showing poor use of medical resources and diminished quality of care, particularly for the patients in rural locations with telehealth systems in place. 12
Medford‐Davis et al. 29 advocated for the use of telemedicine consultation with sub‐specialists. The retrospective study analyzed ED‐to‐ED trauma transfers between two EDs in six states in the United States (n = 48 160). About 50% of 2088 of transferred patients with facial trauma were discharged without procedures. Additionally, in a multivariate analysis controlling for patient demographics and clinical characteristics, transferred patients with facial trauma were more likely to be discharged without procedures. An additional estimated $2859 per patient is associated with transfer for trauma care, not including cost of interfacility transportation. 29 Telemedicine may play a role in mitigating unnecessary health care spending. 29 Furthermore, minimizing unnecessary ED‐to‐ED transfers may decrease cross contamination and disease transmission such as the COVID‐19.
4. DISCUSSION
The COVID‐19 pandemic has forced health care systems across the globe to quickly rise to the challenge to protect their patients, staff, and community. Otolaryngologists and other front‐line health workers are leveraging telemedicine and telehealth tools to support their efforts in this time of resource scarcity. Virtual care programs in almost all specialties are sprouting seemingly overnight in response to the demand from this and future widespread emergencies. New methods of health systems operation and care delivery have inevitably changed how health care providers plan, prepare, and practice while ensuring access and safety. In this time of uncertainty, where some have estimated that the virus may infect up to 60% of the population in the next year, 30 , 31 the growth of telemedicine offers a number of anticipated advantages for clinicians, which include workforce sustainability, decreased provider burnout, exposure control, reduction of PPE waste, and the ability to diagnose, treat, or monitor patients.
With facial trauma evaluations, the ability to quickly review imaging information helps clinicians locate fractures and identify soft tissue injuries that may compromise airway, vision, mastication, lacrimal and sinus function. For this study, we reviewed the literature in its current state describing the application of telemedicine in the evaluation and treatment of facial trauma. The majority of the research conducted in the past two decades associated with the evaluation of facial trauma and telemedicine has been focused on assessment. Face‐to‐face evaluation of facial trauma patients is invaluable. However in the setting of limited resources, telemedicine is a potentially useful tool for triaging patients with facial fractures to improve access to subspecialty care, reduce costs and save time for patients. Even more, telemedicine may be used in the COVID‐19 pandemic or during anticipated second waves to minimize the risk of virus transmission between providers and patients. Telemedicine appears to show promise for use in evaluation of facial trauma, including craniofacial fractures, 15 , 17 , 28 facial cutaneous lacerations, 21 , 22 and operative planning. 17
The potential benefits of telemedicine includes possible facilitation of appropriate triage for facial trauma injuries, improvement in speed of care and time of consultation, continuity of care with follow‐up of patients, anticipated reduction in health care costs, and expansion of the geographic area covered by a single facial trauma surgeon. Expanded use of telemedicine for facial trauma, may reduce unnecessary exposure to patients and health care providers in the current COVID‐19 pandemic and in anticipated future waves. The continued improvement of telemedicine technology itself suggests continued expansion in the scope and level of care it can facilitate. Telemedicine must be used in conjunction with the patient history for the most effective assessment. 21 For obvious reasons of any surgical subspecialty, a recognized barrier in the use of telemedicine is the accurate diagnostic and procedural aspects. 32 Currently, the technology cannot fully replace in‐person physical examinations (ie, palpation, auscultation, touch and smell) in assessing patients, or substitute the in‐person patient‐physician communication.
Due to the severe consequences of postponing some facial trauma treatments, otolaryngologists, oral maxillofacial surgeons, and facial plastic surgeons are all taking special considerations regarding the triage protocol during this COVID‐19 pandemic, which includes being aware of indications, paying attention to timing, and taking precaution during evaluation. 33 This systematic review highlights the gap in knowledge of telehealth‐supported facial trauma evaluation. Technological innovations have opened some opportunities for integration of telemedicine into practice, however, little is known about the potential benefits and detriments of these interventions. More evidence is needed to determine how clinicians may integrate telemedicine in ways that improve diagnosis, treatment, monitoring, and care. Although this systematic review suggests favorable outcomes for specific telehealth interventions, especially in consultation and remote monitoring, more studies should be designed to examine interventions for virtual visits to include the larger integration of telemedicine in head and neck surgery.
Future research directions include further exploring economic benefits of utilizing telemedicine to triage and transfer facial trauma patients appropriately to enhance resource allocation. 29 More well‐designed studies are needed to assess the patient’s comfort with and perception of telemedicine as well as each stakeholder’s willingness to adopt to new technology and share information, particularly in regarding to follow up and utilization of patient provided images, since Walker et al. 22 noted difficulties with patient compliance in this regard.
Current limitations with full adoption of telemedicine for facial trauma evaluation are the 2D video nature of the image and the variable lighting available on physical exam. Thus, evaluating for clinical evidence of septal hematoma, intraoral malocclusion, and facial contour asymmetries are difficult. In addition, since one cannot palpate the face, one cannot evaluate for facial fracture mobility and stability; differentiate between edema vs hematoma; and assess degree of tenderness. With the inability to smell during the physical exam, one cannot identify odors that would indicate an infection. However, by performing a telemedicine visit with good resolution CT scan images, the facial surgeon can usually quickly assess if surgery is acutely needed in many instances while discussing with the patient. While telemedicine may increase access to medical care, lack of access to the internet and telehealth devices limits the application of telemedicine in communities without such technology.
This study had limited high‐level evidence supporting the efficacy and concordance of telemedicine despite many lower level studies supporting it. The technology behind telemedicine itself has rapidly progressed in the last decade, meaning older studies utilize technologies with lower resolutions, possibly weakening concordance between in person and telemedicine assessments and allowing for more misdiagnoses. Although we retrieved articles from three databases (PubMed, Embase, and Web of Science), and believe that the important scientific literature on the topic of interest was covered, this systematic review includes only articles on patients afflicted by facial trauma. We recognize the limited data on the use of telemedicine approaches in other patient populations (with or without facial trauma) can be informative. However, we believe that facial trauma is a unique injury with its own physical and psychological characteristics that require a specific focus on this topic of interest for providers.
5. CONCLUSION
During the COVID‐19 pandemic, patients and health care providers alike will continue to face more safety and logistical obstacles during this time of uncertainty and limited clinical resources. Telemedicine in regards to facial injuries holds future potential for improved patient and provider safety, triage, speed of consultation, costs of care, follow‐up, and extended geographic access to care. One must also realize the current limitations of telemedicine in regards to sensitivity and specificity in evaluating facial trauma as discussed in this article. With expected future disruptions from anticipated second waves of COVID‐19, telemedicine will likely be a useful complementary tool in the clinical management of facial trauma.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
Supporting information
Appendix S1: Supplementary Information
Said M, Ngo V, Hwang J, Hom DB. Navigating telemedicine for facial trauma during the COVID‐19 pandemic. Laryngoscope Investigative Otolaryngology. 2020;5:649–656. 10.1002/lio2.428
Mena Said and Victoria Ngo are co‐first authors.
REFERENCES
- 1. Edwards SP, Kasten S, Nelson C, Elner V, McKean E. Maxillofacial trauma management during COVID‐19: multidisciplinary recommendations. Facial Plast Surg Aesthet Med. 2020;22(3):157‐159. 10.1089/fpsam.2020.0158 [DOI] [PubMed] [Google Scholar]
- 2. Kowalski LP, Sanabria A, Ridge JA, et al. COVID‐19 pandemic: effects and evidence‐based recommendations for otolaryngology and head and neck surgery practice. Head Neck. 2020;42:1259–1267. 10.1002/hed.26164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Meng L, Hua F, Bian Z. Coronavirus disease 2019 (COVID‐19): emerging and future challenges for dental and Oral medicine. J Dent Res. 2020;99(5):481‐487. 10.1177/0022034520914246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Setzen M, Svider PF, Pollock K. COVID‐19 and rhinology: a look at the future. Am J Otolaryngol. 2020;41:102491 10.1016/j.amjoto.2020.102491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019‐nCoV) patients. Can J Anaesth J Can Anesth. 2020;67(5):568‐576. 10.1007/s12630-020-01591-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Holmes S, Bhatti N, Bhandari R, Chatzopoulou D. Toward a consensus view in the management of acute facial injuries during the COVID‐19 pandemic. Br J Oral Maxillofac Surg. 2020;58:571‐576. 10.1016/j.bjoms.2020.03.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lalloo R, Lucchesi LR, Bisignano C, et al. Epidemiology of facial fractures: incidence, prevalence and years lived with disability estimates from the Global Burden of Disease 2017 study. Inj Prev. 2020. https://doi.org.10.1136/injuryprev-2019-043297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. VandeGriend ZP, Hashemi A, Shkoukani M. Changing trends in adult facial trauma epidemiology. J Craniofac Surg. 2015;26(1):108‐112. 10.1097/SCS.0000000000001299 [DOI] [PubMed] [Google Scholar]
- 9. Institute of Medicine (US) Committee on Evaluating Clinical Applications of Telemedicine . Telemedicine: A Guide to Assessing Telecommunications in Health Care In Field MJ, ed. National Academies Press; 1996. http://www.ncbi.nlm.nih.gov/books/NBK45448/. Accessed May 4, 2020. [PubMed]
- 10. Pollock K, Setzen M, Svider PF. Embracing telemedicine into your otolaryngology practice amid the COVID‐19 crisis: an invited commentary. Am J Otolaryngol. 2020;41:102490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Syms MJ, Syms CA III. The regular practice of telemedicine: telemedicine in otolaryngology. Arch Otolaryngol Neck Surg. 2001;127(3):333‐336. 10.1001/archotol.127.3.333 [DOI] [PubMed] [Google Scholar]
- 12. Hutchinson JRB. Telemedicine in otolaryngology. Otolaryngol Clin North Am. 1998;31(2):319‐329. 10.1016/S0030-6665(05)70051-7 [DOI] [PubMed] [Google Scholar]
- 13. Kokesh J, Ferguson AS, Patricoski C, LeMaster B. Traveling an audiologist to provide otolaryngology care using store‐and‐forward telemedicine. Telemed E‐Health. 2009;15(8):758‐763. 10.1089/tmj.2009.0046 [DOI] [PubMed] [Google Scholar]
- 14. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264‐269. [DOI] [PubMed] [Google Scholar]
- 15. Brucoli M, Boffano P, Franchi S, Pezzana A, Baragiotta N, Benech A. The use of teleradiology for triaging of maxillofacial trauma. J Craniomaxillofac Surg. 2019;47(10):1535‐1541. 10.1016/j.jcms.2019.07.007 [DOI] [PubMed] [Google Scholar]
- 16. Jacobs MJ, Edmondson MJ, Lowry JC. Accuracy of diagnosis of fractures by maxillofacial and accident and emergency doctors using plain radiography compared with a telemedicine system: a prospective study. Br J Oral Maxillofac Surg. 2002;40(2):156‐162. 10.1054/bjom.2001.0751 [DOI] [PubMed] [Google Scholar]
- 17. Millesi W, Truppe M, Watzinger F, et al. Remote stereotactic visualization for image‐guided surgery: technical innovation. J Cranio‐Maxillo‐Fac Surg Off Publ Eur Assoc Cranio‐Maxillo‐Fac Surg. 1997;25(3):136‐138. 10.1016/s1010-5182(97)80004-2 [DOI] [PubMed] [Google Scholar]
- 18. Mitsuno D, Hirota Y, Akamatsu J, Kino H, Okamoto T, Ueda K. Telementoring demonstration in craniofacial surgery with HoloLens, Skype, and three‐layer facial models. J Craniofac Surg. 2019;30(1):28‐32. 10.1097/scs.0000000000004899 [DOI] [PubMed] [Google Scholar]
- 19. Chiao L, Sharipov S, Sargsyan AE, et al. Ocular examination for trauma; clinical ultrasound aboard the International Space Station. J Trauma. 2005;58(5):885‐889. 10.1097/01.ta.0000162456.37962.01 [DOI] [PubMed] [Google Scholar]
- 20. Van Dillen C, Silvestri S, Haney M, et al. Evaluation of an off‐the‐shelf mobile telemedicine model in emergency department wound assessment and management. J Telemed Telecare. 2013;19(2):84‐88. 10.1177/1357633x13476231 [DOI] [PubMed] [Google Scholar]
- 21. Farook SA, Davis AK, Sadiq Z, Dua R, Newman L. A retrospective study of the influence of telemedicine in the management of pediatric facial lacerations. Pediatr Emerg Care. 2013;29(8):912‐915. 10.1097/PEC.0b013e31829ec25c [DOI] [PubMed] [Google Scholar]
- 22. Walker TWM, O'Connor N, Byrne S, McCann PJ, Kerin MJ. Electronic follow‐up of facial lacerations in the emergency department. J Telemed Telecare. 2011;17(3):133‐136. 10.1258/jtt.2010.100307 [DOI] [PubMed] [Google Scholar]
- 23. Ambroise B, Benateau H, Garmi R, Hauchard K, Prevost R, Veyssiere A. The role of telemedicine in the management of maxillofacial trauma in emergency departments – preliminary results. J Stomatol Oral Maxillofac Surg. 2019;120(2):95‐98. 10.1016/j.jormas.2018.11.015 [DOI] [PubMed] [Google Scholar]
- 24. Paik AM, Granick MS, Scott S. Plastic surgery telehealth consultation expedites Emergency Department treatment. J Telemed Telecare. 2017;23(2):321‐327. 10.1177/1357633x16639459 [DOI] [PubMed] [Google Scholar]
- 25. Pap SA, Lach E, Upton J. Telemedicine in plastic surgery: E‐consult the attending surgeon. Plast Reconstr Surg. 2002;110(2):452‐456. 10.1097/00006534-200208000-00012 [DOI] [PubMed] [Google Scholar]
- 26. Fonseca AS, Goldenberg DC, Stocchero GF, Luiz AV, Gemperli R. Validation of videoconference with smartphones in telemedicine facial trauma care: analysis of concordance to on‐site evaluation. Ann Plast Surg. 2016;77(4):433‐437. 10.1097/sap.0000000000000623 [DOI] [PubMed] [Google Scholar]
- 27. Tan JR, Coulson S, Keep M. Face‐to‐face versus video assessment of facial paralysis: implications for telemedicine. J Med Internet Res. 2019;21(4):e11109 10.2196/11109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Moumoulidis I, Mani N, Patel H, Leong P. A novel use of photo messaging in the assessment of nasal fractures. J Telemed Telecare. 2007;13(8):387‐390. 10.1258/135763307783064412 [DOI] [PubMed] [Google Scholar]
- 29. Medford‐Davis LN, Holena DN, Karp D, Kallan MJ, Delgado MK. Which transfers can we avoid: multi‐state analysis of factors associated with discharge home without procedure after ED to ED transfer for traumatic injury. Am J Emerg Med. 2018;36(5):797‐803. 10.1016/j.ajem.2017.10.024 [DOI] [PubMed] [Google Scholar]
- 30. Powell A. Hundreds of U.S. coronavirus cases may have slipped through screenings Harvard Gazette. https://news.harvard.edu/gazette/story/2020/03/hundreds-of-u-s-coronavirus-cases-may-have-slipped-through-screenings/. Accessed May 11, 2020.
- 31. Doshi A, Platt Y, Dressen JR, Mathews BK, Siy JC. Keep calm and log on: telemedicine for COVID‐19 pandemic response. J Hosp Med. 2020;15(5):302‐304. 10.12788/jhm.3419 [DOI] [PubMed] [Google Scholar]
- 32. McCool RR, Davies L. Where does telemedicine fit into otolaryngology? An assessment of telemedicine eligibility among otolaryngology diagnoses. Otolaryngol—Head Neck Surg Off J Am Acad Otolaryngol‐Head Neck Surg. 2018;158(4):641‐644. 10.1177/0194599818757724 [DOI] [PubMed] [Google Scholar]
- 33. Hsieh T‐Y, Dedhia RD, Chiao W, et al. A guide to facial trauma triage and precautions in the COVID‐19 pandemic. Facial Plast Surg Aesthet Med. 2020;22:164‐169. 10.1089/fpsam.2020.0185 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1: Supplementary Information


