Abstract
Purpose
The purpose of this study was to identify leading sources of stress, describe rates of mental health outcomes, and examine their associations among U.S. adults during the first months of the COVID‐19 pandemic.
Method
In a cross‐sectional, general population survey conducted from March 18 to April 4, 2020, U.S. adults (n = 10,625) were recruited through Qualtrics Panels using quota sampling methods.
Results
Life stressors, probable depression, past‐month suicide ideation, and past‐month suicide attempts were not elevated among participants subject to state‐level stay‐at‐home orders and/or large gathering bans. Multiple life stressors were associated with increased rates of probable depression. Past‐month suicide ideation was significantly higher among participants reporting ongoing arguments with a partner and serious legal problems. Past‐month suicide attempt was significantly higher among participants reporting concerns about a life‐threatening illness or injury, but was significantly lower among participants reporting an unexpected bill or expense.
Conclusions
Results failed to support the conclusion that physical distancing measures are correlated with worse mental health outcomes. Concerns about life‐threatening illness or injury were uniquely associated with increased risk of suicide attempt.
1. INTRODUCTION
The first report of a novel coronavirus disease 2019 (COVID‐19) in the United States came on January 20, 2020. Since then, confirmed cases of COVID‐19 have rapidly increased. Efforts to slow the spread of the virus have emphasized physical distancing strategies such as bans on large public events, partial or complete closure of businesses and educational institutions, and stay‐at‐home orders. These measures could increase exposure to situations and circumstances associated with poor mental health outcomes, including economic and financial strain, reduced social contact, and limited access to medical and mental health care services (Reger, Stanley, & Joiner, 2020). Supporting these concerns are early reports from China indicating increased rates of anxiety and emotional distress (Qiu et al., 2020) and recent polls (Kirzinger et al., 2020) conducted during the first month of the U.S. pandemic finding that over 40% of U.S. adults reported a negative impact of the pandemic on their mental health, with 19% describing this impact as “major.” In that same poll, respondents who were sheltering‐in‐place were significantly more likely to report pandemic‐related worry or stress having a major negative impact on their mental health than respondents who were not sheltering‐in‐place (21% vs. 13%), raising concerns that public health efforts such as physical distancing measures could increase rates of suicide mortality through increased mental illness and loneliness (Reger et al., 2020). Data specific to mental health outcomes during the COVID‐19 pandemic are therefore needed to guide decisions about how to most effectively and efficiently allocate mental health resources.
The primary aims of the present study were to describe rates of life stressor exposure and mental health outcomes among U.S. adults during the early stages of the COVID‐19 pandemic, and to examine their associations. To achieve these aims, we analyzed data collected as part of a cross‐sectional survey fielded during the first months of the U.S. pandemic.
2. METHODS
2.1. Study design and setting
We performed an online cross‐sectional study focused on recent life stressors, emotional distress, and suicidal thoughts and behaviors using Qualtrics Panels, an online survey platform that maintains a database of several million U.S. residents who have volunteered to participate in periodic survey‐based research. Because of their efficiency, online survey panels have been used with increased frequency to obtain general population samples for health‐related and social research (Cheng, 2015; DeVylder et al., 2018; Jensen et al., 2016; Johnson, Harkins, Cary, Sankar, & Karlawish, 2015; Tinghög et al., 2013). Qualtrics Panels uses quota sampling methods to identify participants meeting each study’s eligibility criteria, with a target to recruit a sample that was demographically similar to 2010 U.S. census distributions for age, sex, and race/ethnicity (±10%). Panel members received an email invitation with an embedded hyperlink that redirected the individual to our survey landing page, which contained an informed consent form explaining study purpose, procedures, and risks and benefits. Consent to participate in the study was implied by selecting a box indicating their understanding of this information, which enabled them to proceed to the survey. Participants who completed the survey were financially compensated in the amount that was agreed upon when they initially agreed to join a panel. The only inclusion criterion was to be 18 years or older; no exclusion criteria were employed. Participants who did not complete the survey in full were excluded from subgroup quotas. Of 65,079 panel members who accessed the survey landing page and reviewed the informed consent form, 10,625 (16.3%) subsequently completed the survey. This survey study was reviewed and approved by the University of Utah Institutional Review Board. Data were collected between March 18, 2020, and April 2, 2020.
2.2. Measures
Stressor exposure was assessed with a researcher‐developed checklist of 13 potential stressors involving health, relationships, financial strain, legal issues, and work‐related concerns, plus one additional option for “other” unspecified stressors. Participants were directed to check all of the stressors that “caused you to experience more stress than usual during the past month.”
Probable depression was assessed using the 9‐item Patient Health Questionnaire depression subscale (PHQ‐9), (Kroenke, Spitzer, & Williams, 2001) which assesses the frequency of each DSM‐defined symptom of major depressive disorder during the past 2 weeks. The internal consistency of the PHQ‐9 in this sample was excellent (α = 0.92). A total score of 14 or higher, which indicates at least moderately severe depression, was used to identify cases with probable depression.
Suicide ideation and attempts were assessed using the Self‐Injurious Thoughts and Behaviors Interview (SITBI) (Nock, Holmberg, Photos, & Michel, 2007). Suicide ideation was assessed with the following item: “Have you ever had thoughts of killing yourself?” Suicide attempt was assessed with the following item: “Have you ever made an actual attempt to kill yourself in which you had at least some intent to die?” To determine whether these thoughts or behaviors had occurred within the preceding month, participants who positively endorsed each item were subsequently asked when they most recently had these thoughts or made a suicide attempt: within the past month, within the past year, or more than a year ago.
Physical distancing measures were assessed using data drawn from the Kaiser Family Foundation’s (KFF) website (https://www.kff.org/report‐section/state‐data‐and‐policy‐actions‐to‐address‐coronavirus‐sources/). We extracted the dates on which each U.S. state implemented two physical distancing measures that could influence mental health outcomes through increased loneliness: stay‐at‐home orders and large gathering bans. Implementation dates by state were matched to each participant’s state of residence, which was assessed during the survey.
2.3. Statistical analysis
All analyses were conducted using SPSS software, version 25. Data were missing from fewer than 0.4% of participants. To test associations among predictors and criterion variables, we constructed a series of logistic regression models with household income, gender, race, and age included as covariates in all analyses. For models examining correlates of past‐month suicide attempts, we conducted sensitivity analyses wherein we repeated the analysis in the subset of participants reporting past‐month suicide ideation, thereby enabling us to determine whether predictor variables distinguished participants with a recent suicide attempt from those with recent ideation. In terms of power, our sample size (N = 10,625) provides 80% power to detect a minimum odds ratio of 1.6, assuming a two‐tailed alpha of .05, an outcome rate of 1%, and a binary predictor occurring in 40% of the sample. If a binary predictor occurred in only 10% of the sample, however, there was 80% power to detect a minimum odds ratio of 2.1.
3. RESULTS
The sample’s demographic profile is summarized in Table 1. The percentage of participants self‐identifying as white was lower than U.S. census estimates due to a higher than expected percentage of participants self‐identifying as “other.” Most participants (86.4%) choosing the “other” option also self‐identified as Hispanic, Latino, or Spanish origin, suggesting the “other” racial identity and Hispanic, Latino, and Spanish origin ethnicity options overlapped to a large degree. The mean PHQ‐9 score was 7.3 (SD = 6.7), reflecting a mild level of depressive symptoms during the previous 2 weeks. 19.5% of participants had probable depression, 4.6% reported past‐month suicide ideation, and 1.2% reported past‐month suicide attempts. The majority of participants were subject to at least one physical distancing measure (Table 2).
Table 1.
Sample demographics
| Variable | (N = 10,625) |
|---|---|
| Age, mean (SD), year | 45.2 (17.0) |
| Gender, n (%) | |
| Male | 5,181 (48.8) |
| Female | 5,389 (50.7) |
| Transgender | 32 (0.3) |
| Other | 23 (0.2) |
| Race, n (%) | |
| White | 6,577 (61.9) |
| Black | 1,307 (12.3) |
| Asian | 703 (6.6) |
| American Indian | 398 (3.7) |
| Pacific Islander | 89 (0.8) |
| Other | 1,551 (14.6) |
| Hispanic ethnicity, n (%) | |
| Yes | 3,715 (35.0) |
| No | 6,910 (65.0) |
| Annual household income, n (%) | |
| <$25,000 | 1,994 (18.8) |
| $25,000–34,999 | 1,145 (10.8) |
| $35,000–49,999 | 1,111 (10.5) |
| $50,000–74,999 | 2,086 (19.6) |
| $75,000–99,999 | 1,421 (13.4) |
| $100,000–149,999 | 1,675 (15.8) |
| $150,000–199,999 | 642 (6.0) |
| >$200,000 | 551 (5.2) |
Table 2.
Number of participants who completed the survey when statewide stay‐at‐home orders and large gathering bans were or were not in effect
| Stay‐at‐home order | Total | Large gathering ban | |
|---|---|---|---|
| Not in effect | In effect | ||
| Not in effect | 4,268 (40.2%) | 1,962 (18.5%) | 2,306 (21.7%) |
| In effect | 6,344 (59.8%) | 529 (5.0%) | 5,815 (54.8%) |
| Total | 10,612 (100.0%) | 2,491 (23.5%) | 8,121 (76.5%) |
3.1. Rates of life stressors and associations with physical distancing measures
Figure 1 shows the percentage of participants reporting each type of life stressor within the past month. The most common stressors within the preceding month included unexpected bills or expenses (28.2%), the death of a close friend or family member (22.2%), and a life‐threatening illness or injury for a close friend or family member (17.3%). Rates of life stressors were unrelated to physical distancing measures, with one exception (see Table 3): participants subject to large gathering bans were significantly more likely to report increased stress related to being disciplined or punished at work (OR = 1.56, 95% CI = 1.17–2.07, p = .002).
Figure 1.
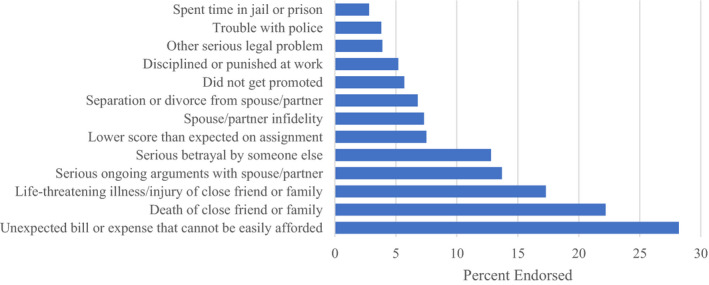
Percentage of sample endorsing each of 13 possible stressors causing more than usual stress within the past month
Table 3.
Percentage of participants endorsing each life stressor within the past month, by state‐level physical distancing measures in effect at the time of survey completion
| Past‐month stressor | None | SAH only | LGB only | Both | Stay‐at‐home order | Large gathering ban | Both | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | % | % | % | OR | (95% CI) | p | OR | (95% CI) | p | OR | (95% CI) | p | |
| Life‐threatening illness/injury of friend/family | 17.8 | 16.1 | 16.2 | 17.6 | 0.94 | (0.73–1.23) | .658 | 0.91 | (0.77–1.07) | .257 | 1.15 | (0.85–1.54) | .363 |
| Death of close friend or family | 22.5 | 20.2 | 23.5 | 21.7 | 0.93 | (0.74–1.19) | .579 | 1.09 | (0.94–1.26) | .256 | 0.97 | (0.74–1.27) | .817 |
| Separation or divorce from spouse/partner | 8.0 | 6.0 | 6.8 | 6.5 | 0.85 | (0.57–1.27) | .435 | 0.87 | (0.69–1.10) | .250 | 1.11 | (0.71–1.74) | .634 |
| Serious arguments with spouse/partner | 16.0 | 11.9 | 12.6 | 13.4 | 0.84 | (0.63–1.13) | .258 | 0.86 | (0.72–1.02) | .086 | 1.24 | (0.89–1.72) | .207 |
| Spouse/partner infidelity | 9.0 | 5.3 | 7.3 | 6.9 | 0.75 | (0.49–1.13) | .168 | 0.93 | (0.74–1.17) | .541 | 1.24 | (0.79–1.96) | .353 |
| Serious betrayal by someone else | 15.7 | 10.4 | 11.8 | 12.4 | 0.86 | (0.63–1.17) | .329 | 0.87 | (0.72–1.04) | .122 | 1.21 | (0.85–1.71) | .285 |
| Unexpected bill or expense | 28.3 | 29.9 | 28.1 | 28.0 | 1.23 | (0.99–1.53) | .057 | 1.11 | (0.97–1.27) | .149 | 0.82 | (0.64–1.04) | .103 |
| Did not get promoted | 6.2 | 5.1 | 5.6 | 5.7 | 0.95 | (0.62–1.47) | .815 | 0.98 | (0.76–1.27) | .885 | 1.01 | (0.62–1.63) | .985 |
| Lower score than expected on assignment | 9.3 | 6.4 | 6.7 | 7.4 | 1.08 | (0.73–1.60) | .711 | 0.93 | (0.74–1.17) | .525 | 0.95 | (0.61–1.48) | .835 |
| Disciplined or punished at work | 4.2 | 4.7 | 5.8 | 5.4 | 1.34 | (0.84–2.14) | .215 | 1.56 | (1.17–2.07) | .002 | 0.64 | (0.38–1.06) | .083 |
| Trouble with police | 3.9 | 2.3 | 4.3 | 3.6 | 0.74 | (0.40–1.37) | .336 | 1.22 | (0.89–1.66) | .210 | 1.13 | (0.58–2.21) | .722 |
| Spent time in jail or prison | 3.4 | 1.9 | 2.7 | 2.8 | 0.69 | (0.35–1.36) | .282 | 0.85 | (0.59–1.21) | .358 | 1.53 | (0.73–3.23) | .261 |
| Other serious legal problem | 4.0 | 3.9 | 3.4 | 3.9 | 1.04 | (0.62–1.77) | .874 | 1.11 | (0.81–1.52) | .517 | 0.93 | (0.52–1.68) | .819 |
3.2. Rates of poor mental health outcomes and associations with physical distancing measures
Rates of poor mental health outcomes were generally unrelated to physical distancing measures, with two exceptions (see Table 4): Participants subject to stay‐at‐home orders were significantly less likely to report probable depression (OR = 0.75, 95% CI = 0.57–0.99, p = .044), and participants with past‐month suicide ideation who were subject to large gathering bans were significantly less likely to report a suicide attempt in the prior month (OR = 0.39, 95% CI = 0.17–0.88, p = .024).
Table 4.
Percentage of participants with probable depression, past‐month suicide ideation, and past‐month suicide attempt, by state‐level physical distancing measures in effect at the time of survey completion
| Mental health outcome | None | SAH Only | LGB Only | Both | Stay‐at‐home order | Large gathering ban | Both both | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | % | % | % | OR | (95% CI) | p | OR | (95% CI) | p | OR | (95% CI) | p | |
| Probable depression | 23.4 | 14.4 | 18.6 | 19.2 | 0.75 | (0.57–0.99) | .044 | 0.91 | (0.78–1.06) | .211 | 1.32 | (0.98–1.79) | .071 |
| Past‐month suicide ideation | 5.9 | 3.0 | 4.2 | 4.5 | 0.70 | (0.41–1.21) | .201 | 0.86 | (0.64–1.14) | .279 | 1.50 | (0.83–2.71) | .180 |
| Past‐month suicide attempt | 1.5 | 0.4 | 1.1 | 1.2 | 0.35 | (0.08–1.49) | .155 | 0.85 | (0.49–1.45) | .547 | 2.70 | (0.59–12.30) | .201 |
| Among those with past‐month ideation | 22.6 | 6.3 | 11.5 | 15.3 | 0.29 | (0.03–2.49) | .258 | 0.39 | (0.17–0.88) | .024 | 4.59 | (0.47–44.75) | .190 |
3.3. Association of past‐month stressors with suicide ideation and suicide attempt
The likelihood of probable depression was significantly increased among participants endorsing stress about life‐threatening illness or injury of friends or family (OR = 1.81, 95% CI = 1.59–2.05, p < .001), separation or divorce from a spouse or partner (OR = 1.81, 95% CI = 1.51–2.17, p < .001), serious arguments with a spouse or partner (OR = 1.83, 95% CI = 1.59–2.09, p < .001), infidelity by a spouse or partner (OR = 1.43, 95% CI = 1.19–1.71, p < .001), serious betrayal by someone else (OR = 1.52, 95% CI = 1.32–1.76, p < .001), an unexpected bill or expense (OR = 1.15, 95% CI = 1.03–1.29, p = .018), and other serious legal problems (OR = 1.88, 95% CI = 1.49–2.36, p < .001). The likelihood of past‐month suicide ideation was significantly increased among participants endorsing serious ongoing arguments with a spouse or partner (OR = 1.46, 95% CI = 1.16–1.83, p = .001) and other serious legal problems (OR = 1.85, 95% CI = 1.31–2.62, p < .001). The likelihood of past‐month suicide attempt was significantly increased among those endorsing stress about a life‐threatening illness or injury of a close friend or family member (OR = 2.26, 95% CI = 1.48‐3.46, p < .001) but was decreased among those endorsing an unexpected bill or expense that cannot be easily afforded (OR = 0.41, 95% CI = 0.24–0.70, p = .001). In the subset of participants reporting past‐month suicide ideation (n = 489), only stress about a life‐threatening illness or injury of a close friend or family member was associated with significantly increased likelihood of past‐month suicide attempt (OR = 3.87, 95% CI = 2.14–6.99, p < .001). Results are summarized in Table 5.
Table 5.
Association of past‐month stressors with probable depression, past‐month suicide ideation, and past‐month suicide attempt
| Past‐month stressors | Probable depression | Past‐month suicide ideation | Past‐month suicide attempt | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Full sample | Among those with past‐month ideation | |||||||||||
| OR | (95% CI) | p | OR | (95% CI) | p | OR | (95% CI) | p | OR | (95% CI) | p | |
| Life‐threatening illness/injury of friend/family | 1.81 | (1.59–2.05) | <.001 | 0.96 | (0.75–1.22) | .740 | 2.26 | (1.48–3.46) | <.001 | 3.87 | (2.14–6.99) | <.001 |
| Death of close friend or family | 1.12 | (0.99–1.27) | .073 | 0.88 | (0.70–1.11) | .278 | 0.89 | (0.58–1.39) | .616 | 1.07 | (0.58–1.99) | .830 |
| Separation or divorce from spouse/partner | 1.81 | (1.51–2.17) | <.001 | 1.36 | (1.00–1.84) | .049 | 1.45 | (0.91–2.33) | .120 | 1.18 | (0.57–2.44) | .659 |
| Serious arguments with spouse/partner | 1.83 | (1.59–2.09) | <.001 | 1.46 | (1.16–1.83) | .001 | 1.64 | (1.08–2.48) | .020 | 1.06 | (0.56–2.03) | .855 |
| Spouse/partner infidelity | 1.43 | (1.19–1.71) | <.001 | 0.95 | (0.70–1.29) | .725 | 1.83 | (1.10–3.04) | .020 | 1.57 | (0.74–3.35) | .244 |
| Serious betrayal by someone else | 1.52 | (1.32–1.76) | <.001 | 1.25 | (0.97–1.60) | .086 | 1.18 | (0.74–1.89) | .495 | 0.91 | (0.45–1.84) | .801 |
| Unexpected bill or expense | 1.15 | (1.03–1.29) | .018 | 1.05 | (0.84–1.32) | .657 | 0.41 | (0.24–0.70) | .001 | 0.38 | (0.17–0.85) | .019 |
| Did not get promoted | 1.12 | (0.91–1.38) | .273 | 0.96 | (0.67–1.39) | .843 | 0.93 | (0.49–1.78) | .825 | 1.16 | (0.46–2.94) | .750 |
| Lower score than expected on assignment | 0.85 | (0.71–1.02) | .086 | 1.27 | (0.95–1.72) | .112 | 1.30 | (0.76–2.22) | .335 | 1.19 | (0.56–2.50) | .656 |
| Disciplined or punished at work | 1.07 | (0.86–1.32) | .555 | 1.28 | (0.89–1.83) | .183 | 0.87 | (0.47–1.60) | .648 | 0.56 | (0.18–1.820 | .337 |
| Trouble with police | 1.17 | (0.91–1.52) | .220 | 0.63 | (0.39–1.01) | .053 | 1.45 | (0.72–2.94) | .297 | 1.08 | (0.38–3.09) | .888 |
| Spent time in jail or prison | 1.01 | (0.75–1.35) | .959 | 1.15 | (0.70–1.91) | .577 | 1.07 | (0.50–2.27) | .865 | 1.46 | (0.52–4.07) | .474 |
| Other serious legal problem | 1.88 | (1.49–2.36) | <.001 | 1.85 | (1.31–2.62) | <.001 | 1.29 | (0.65–2.55) | .462 | 0.78 | (0.35–1.77) | .559 |
4. DISCUSSION
The rapid spread of COVID‐19 globally has contributed to increased anxiety and a range of social consequences that are known to be associated with increased risk for poor mental health outcomes and suicide mortality: economic and financial strain, social isolation, decreased social activities and engagement, and reduced access to health care services (Kirzinger, Kearney, Hamel, & Brodie, 2020; Qiu et al., 2020). The present study entailed a national cross‐sectional survey conducted during the first months of the COVID‐19 pandemic in the United States. Our results indicate the leading sources of stress among respondents were financial strain, the death of a very close friend or family member, and the life‐threatening illness or injury of a very close friend or family member. Because our survey was created and prepared for distribution before the first confirmed case of COVID‐19 in the United States, we did not design items that could more precisely measure pandemic‐specific sources of stress and variables. We therefore recommend caution when interpreting these findings, as we cannot know for sure if the financial strain reported by participants was directly related to the pandemic (e.g., reduced work hours, layoffs or furloughs, increased medical expenses). Similarly, we are unable to determine whether participants’ reported anxieties about the death, illness, and/or injury of loved ones are specifically attributable to COVID‐19. Additional research designed to specifically assess these relationships is needed to draw these conclusions with greater certainty.
Our results failed to support our hypothesis that physical distancing measures were associated with increased life stress, depression, and suicide risk in our sample. On the contrary, several findings were more supportive of the opposite conclusion, which is that mental health outcomes were somewhat better among participants subject to physical distancing measures. Here again, we recommend caution when drawing conclusions based on these findings until they can be replicated in other studies, however, especially when considering the relatively narrow range of mental health outcomes assessed in our survey: general distress, depression, and suicidal thoughts and behaviors. It is possible that other, unassessed mental health outcomes (e.g., anxiety, sleep disturbance) would yield different patterns of results. Furthermore, because our survey was fielded during the first few months of the U.S. pandemic, it is possible that the deleterious effects of physical distancing on mental health outcomes had not yet emerged. To this end, our results may serve as a useful benchmark or reference point for future studies that will be conducted later in the pandemic.
In the present study, multiple life stressors were associated with increased risk for probable depression, but a relatively smaller subset of these stressors was associated with increased risk for suicide ideation and attempts. Of note, stress related to a life‐threatening illness or injury of a close friend or family member was the only life stressor that significantly distinguished participants who had attempted suicide in the past month from those who had thought about suicide. Although these patterns generally align with previous risk factor research, (Franklin et al., 2017; Kroenke et al., 2001) we again emphasize that caution is warranted in drawing the conclusion that respondents were thinking specifically of COVID‐19 when endorsing concerns about a “life‐threatening illness.” Additional research that specifically asks about worry, anxiety, and/or other emotional distress specific to friends and families who have been diagnosed with COVID‐19 is needed to confirm this possible interpretation and conclusion.
Our results revealed an unexpected finding involving financial strain and suicide risk. Specifically, in contrast to previous research finding increased risk for suicidal behaviors among those experiencing financial strain, (Bryan & Bryan, 2019; Franklin et al., 2017) participants in the present study who reported feeling stressed about an unexpected bill or expense that could not be easily afforded were significantly less likely to have made a suicide attempt during the previous month. One potential explanation for this finding is that the risk of a suicide attempt initially declines in the immediate aftermath of acute financial strain, but increases over time as the financial strain persists. Another possibility is that the typically positive association of financial strain with suicidal behavior depends in part (or in whole) on the social context. From this perspective, the COVID‐19 pandemic may function as a moderator variable that affects the strength (and direction) of the relationship between financial strain and suicide attempts. A third possibility is that the deleterious effect of financial strain was offset by news of the U.S. economic stimulus package, which was passed on March 28, 2020, approximately halfway through the data collection period. A final possibility is that this finding is spurious. Conclusions based on this specific finding should therefore be made cautiously until it can be replicated or further examined in future studies.
In addition to the limitations mentioned above, our study was also limited by our cross‐sectional design and absence of prepandemic data, which limit our ability to determine whether participants experienced the onset of the life stressors assessed in our study before or after the first confirmed COVID‐19 case in the United States. Despite the study’s limitations, our findings suggest that increased stress stemming from health‐related concerns may be associated with increased risk for suicidal behaviors during the pandemic. Additional research, especially those utilizing probabilistic sampling methods that can clarify the generalizability of the present results, is needed to confirm these initial findings and to further assess mental health outcomes within the context of the COVID‐19 pandemic. Such research could inform optimal resource allocation during the current pandemic and improve national and global readiness for future public health crises.
Bryan CJ, Bryan AO, & Baker JC. Associations among state‐level physical distancing measures and suicidal thoughts and behaviors among U.S. adults during the early COVID‐19 pandemic. Suicide Life Threat Behav. 2020;50:1223–1229. 10.1111/sltb.12653
REFERENCES
- Bryan, C. J. , & Bryan, A. O. (2019). Financial strain, suicidal thoughts, and suicidal behavior among US military personnel in the National Guard. Crisis, 40, 437–445. [DOI] [PubMed] [Google Scholar]
- Cheng, Z. H. (2015). Asian Americans and European Americans’ stigma levels in response to biological and social explanations of depression. Social Psychiatry and Psychiatric Epidemiology, 50, 767–776. 10.1007/s00127-014-0999-5 [DOI] [PubMed] [Google Scholar]
- DeVylder, J. E. , Jun, H. , Fedina, L. , Coleman, D. , Anglin, D. , Cogburn, C. , … Barth, R. P. (2018). Association of exposure to police violence with prevalence of mental health symptoms among urban residents in the United States. JAMA Network Open, 1, e184945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franklin, J. C. , Ribeiro, J. D. , Fox, K. R. , Bentley, K. H. , Kleiman, E. M. , Huang, X. , … Nock, M. K. (2017). Risk factors for suicidal thoughts and behaviors: A meta‐analysis of 50 years of research. Psychological Bulletin, 143, 187–232. 10.1037/bul0000084 [DOI] [PubMed] [Google Scholar]
- Jensen, J. D. , Holton, A. E. , Krakow, M. , Weaver, J. , Donovan, E. , & Tavtigian, S. (2016). Colorectal cancer prevention and intentions to use low‐dose aspirin: A survey of 1000 US adults aged 40–65. Cancer Epidemiology, 41, 99–105. 10.1016/j.canep.2016.02.003 [DOI] [PubMed] [Google Scholar]
- Johnson, R. , Harkins, K. , Cary, M. , Sankar, P. , & Karlawish, J. (2015). The relative contributions of disease label and disease prognosis to Alzheimer’s stigma: A vignette‐based experiment. Social Science and Medicine, 143, 117–127. [DOI] [PubMed] [Google Scholar]
- Kirzinger, A. , Kearney, A. , Hamel, L. , & Brodie, M. (2020). KFF health tracking poll—Early April 2020: The impact of coronavirus on life in America. Retrieved from https://www.kff.org/health‐reform/report/kff‐health‐tracking‐poll‐early‐april‐2020/ [Google Scholar]
- Kroenke, K. , Spitzer, R. L. , & Williams, J. B. (2001). The PHQ‐9: validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock, M. K. , Holmberg, E. B. , Photos, V. I. , & Michel, B. D. (2007). Self‐injurious thoughts and behaviors interview: Development, reliability, and validity in an adolescent sample. Psychological Assessment, 19, 309–317. [DOI] [PubMed] [Google Scholar]
- Qiu, J. , Shen, B. , Zhao, M. , Wang, Z. , Xie, B. , & Xu, Y. (2020). A nationwide survey of psychological distress among Chinese people in the COVID‐19 epidemic: Implications and policy recommendations. General Psychiatry, 33, e100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reger, M. A. , Stanley, I. H. , & Joiner, T. E. (2020). Suicide mortality and coronavirus disease 2019—A perfect storm? JAMA Psychiatry. 10.1001/jamapsychiatry.2020.1060. [DOI] [PubMed] [Google Scholar]
- Stone, D. M. , Simon, T. R. , Fowler, K. A. , Kegler, S. R. , Yuan, K. , Holland, K. M. , … Crosby, A. E. (2018). Vital signs: Trends in state suicide rates—United States, 1999–2016 and circumstances contributing to suicide—27 states, 2015. MMWR, 67, 617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinghög, G. , Andersson, D. , Bonn, C. , Böttiger, H. , Josephson, C. , Lundgren, G. , … Johannesson, M. (2013). Intuition and cooperation reconsidered. Nature, 498(7452), E1–E2. 10.1038/nature12194. [DOI] [PubMed] [Google Scholar]


