Editor,
Chilblains are skin condition frequently seen by physicians worldwide during the COVID‐19 outbreak. 1 , 2 We attended 22 children and adolescents with chilblains during the outbreak peak of COVID‐19 in Madrid. The clinicopathological and laboratory features of these patients have been reported. 1 We describe herein the dermoscopic findings. Approval from the Institutional Ethics Committee and Board was obtained. Standard informed consents were obtained for recording images in all patients.
We analysed 41 dermoscopy pictures obtained from different skin lesions in 12 patients with chilblains. The patients presented erythematous to purpuric macules and violaceous swellings located on the toes and feet. The images corresponded to lesions located on the perionychium (17), tip of toe with or without subungual (13), dorsum or side of toe (seven), dorsum of foot (two), ankle (one) and only subungual (one) (Table 1).
Table 1.
Dermoscopic features of 41 pictures corresponding to 12 children and adolescents with COVID‐19‐related chilblains
| Patient | Lesion | Background area | Globules | Reticule |
|---|---|---|---|---|
| 1 | Perionychium | Red + Brown areas | + | − |
| Tip of toe | Red | + | − | |
| 2 | Perionychium | Purple + Brown areas | ++ | − |
| Perionychium | Brown | ++ | + | |
| Perionychium | Red + Brown areas | ++ | − | |
| Perionychium | Red + Purple areas | ++ | − | |
| 3 | Side of toe | Red | ++ | − |
| Tip of toe | Red + Purple areas | + | − | |
| Tip of toe | Red + Purple areas | + | − | |
| 4 | Dorsum of foot | Red | ++ | − |
| 5 | Dorsum of toe | Brown + Purple areas + Red areas | ++ | + |
| Perionychium | Purple + Brown areas | ++ | + | |
| Tip of toe | Brown | + | − | |
| Tip of toe, subungual | Purple + Brown areas | ++ | − | |
| Tip of toe, subungual | Brown + Purple areas | ++ | − | |
| 6 | Subungual | Brown | − | − |
| Tip of toe | Grey + Purple areas + Brown areas | ++ | − | |
| 7 | Dorsum of toe | Purple + Brown areas + Red areas | ++ | − |
| Ankle | Red + Purple areas + Brown areas | ++ | − | |
| Dorsum of toe | Brown | ++ | + | |
| 8 | Perionychium | Purple + Brown areas | ++ | + |
| Perionychium | Brown + Purple areas | ++ | + | |
| Perionychium | Purple + Brown areas | ++ | + | |
| 9 | Perionychium | Grey + Brown areas | ++ | + |
| Perionychium | Red + Brown areas | ++ | − | |
| Dorsum of toe | Brown + Purple areas + Grey areas | ++ | + | |
| Dorsum of toe | Purple + Brown areas | ++ | + | |
| Dorsum of toe | Brown + Purple areas | ++ | + | |
| 10 | Perionychium | Red + Grey areas + Purple areas + Brown areas | ++ | − |
| Perionychium | Red | + | − | |
| 11 | Perionychium | Red + Purple areas + Brown areas | ++ | + |
| Perionychium | Red + Brown areas | ++ | − | |
| Dorsum of foot | Red + Purple areas | ++ | − | |
| Perionychium | Purple + Brown areas | ++ | − | |
| Perionychium | Purple | ++ | − | |
| Tip of toe | Red + Brown areas | ++ | − | |
| Tip of toe | Red + Purple areas | ++ | − | |
| Tip of toe | Red | − | − | |
| 12 | Tip of toe, subungual | Brown + Red areas | − | − |
| Tip of toe, subungual | Brown + Red areas | ++ | − | |
| Tip of toe, subungual | Purple + Brown areas | ++ | − |
Three main dermoscopic features were observed: a background area, globules and reticule (Fig. 1). The background area is the predominant background colour in the lesion, ranging from red, purple and brown to grey. Globules are round to oval structures of red to purple colour. And the network reticule is a mesh of grey‐brown interconnected lines usually located peripherally within the background macule.
Figure 1.
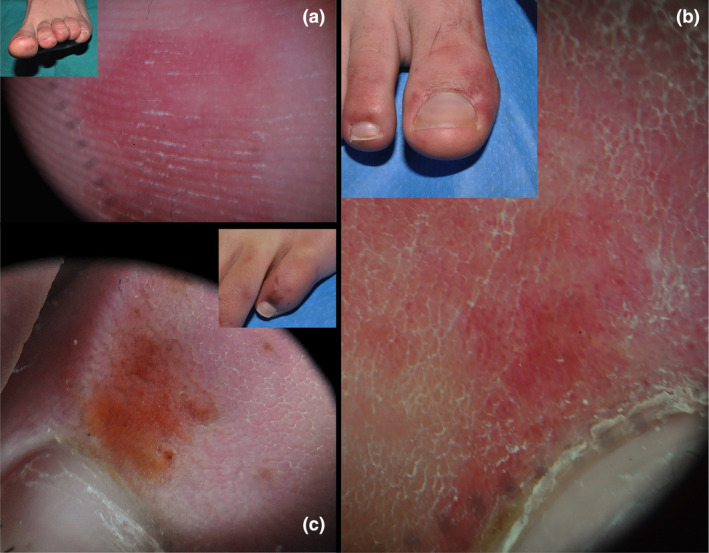
(a) Homogeneous red area on the tip of toe. No globules or reticule are seen. (b) Red background area with purpuric globules on the perionychium. (c) Brown area with reticule and brown globules both within the area and peripherically.
The background area was present in all cases; the predominant colour was red in 18 pictures, brown in 11, purple in 10 and grey in 2. Most pictures (31) contained areas of other colours within the areas whereas in 10 (24.4%) there was only one homogeneous colour present. Globules were seen in 38 images (92.7%) and were prominent in 32 and mild in 6. The globules were included within the background area in most cases, but in some they were seen outside the macules on a background of normal‐looking skin. A reticule was observed in 12 images (29.3%). Other features found were splinter haemorrhages in the nails (three images), dilated capillaries in the nail folds with loss of polarity (two images) and subcorneal haemorrhagic dots (one image).
Dermoscopy mirrors the clinical and histopathologic features of COVID‐19‐related chilblains. 1 The background colour is an indicator of vascular macules, and variations found in the pictures analysed probably reflect the evolution of lesions, being mostly red in early phases from vascular dilatation, purple later from extensive red cell extravasation and finally brown as a consequence of hemosiderin deposition. Grey areas may be indicative of more intense ischaemic phenomena. Globules most likely represent damaged vessels with extravasated red cells. The grey‐brown reticule may be the result of extensive damage to the dermal vascular plexus.
The presence of different colours and features in pictures from different locations in the same patient is most likely due to local factors and to the different state of evolution of different lesions. Patients usually present new lesions throughout the evolution of COVID‐19‐related chilblains.
The specificity of the features found is uncertain because no dermoscopic study of primary chilblains or chilblains secondary to other causes has been published. Dermoscopy studies in purpuric lesions highlight that the background colour is related to the inflammatory infiltrate, hemosiderin deposition and vascular dilatation. 3 , 4 Red globules represent extravasated red cells, and the grey‐brown reticule is possibly due to pigment incontinence and lichenoid infiltrates along with vascular changes. 5
We conclude that dermoscopy may be a useful aid for the diagnosis of chilblains in the setting of COVID‐19 infection.
References
- 1. Andina D, Noguera‐Morel L, Bascuas‐Arribas M et al. Chilblains in children in the setting of COVID‐19 pandemic. Pediatr Dermatol 2020; 37: 406–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. El Hachem M, Diociaiuti A, Concato C et al. A clinical, histopathological and laboratory study of 19 consecutive Italian paediatric patients with chilblain‐like lesions: lights and shadows on the relationship with COVID‐19 infection. J Eur Acad Dermatol Venereol 2020. [Epub ahead of print] 10.1111/jdv.16682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zaballos P, Puig S, Malvehy J. Dermoscopy of pigmented purpuric dermatoses (lichen aureus): a useful tool for clinical diagnosis. Arch Dermatol 2004; 140: 1290–1291. [DOI] [PubMed] [Google Scholar]
- 4. Vazquez‐Lopez F, García‐García B, Sanchez‐Martin J, Argenziano G. Dermoscopic patterns of purpuric lesions. Arch Dermatol 2010; 146: 938. [DOI] [PubMed] [Google Scholar]
- 5. Martín JM, Bella‐Navarro R, Jordá E. Vascular patterns in dermoscopy. Actas Dermosifiliogr 2012; 103: 357–375. [DOI] [PubMed] [Google Scholar]
Acknowledgement
The patients in this manuscript have given written informed consent to the publication of their case details.


