TO THE EDITOR:
Despite unprecedented efficacy,1 the use of axicabtagene ciloleucel (axi-cel) for the treatment of patients with relapsed or refractory large B-cell lymphoma (LBCL) remains associated with acute toxicity, such as grade ≥3 cytokine release syndrome (CRS) and immune effector cell–associated neurotoxicity syndrome (ICANS), occurring in 11% and 32% of patients, respectively.2 Analysis of 44 different analytes in the serum of patients with relapsed or refractory LBCL treated with axi-cel showed that an increase in IL-6 or IL-1 may be associated with such toxicity.3 However, in 2 murine models, whereas IL-6 blockade (typically achieved in clinical practice with the use of tocilizumab) prevented CRS only, only IL-1 blockade prevented both CRS and/or ICANS.4,5 IL-1 blockade can be clinically achieved with the use of anakinra, an IL-1 receptor antagonist, currently approved by the US Food and Drug Administration for the treatment of patients with rheumatoid arthritis and neonatal-onset multisystem inflammatory disease.6,7 Anakinra is also used off label for the treatment of secondary hemophagocytic lymphohistiocytosis (HLH), a condition in the spectrum of CRS potentially associated with chimeric antigen receptor (CAR) T-cell therapy.8,9 Data regarding the clinical use of anakinra for the mitigation of axi-cel–associated toxicity have not been published.
Patients with relapsed or refractory LBCL treated with standard axi-cel therapy, who received anakinra for mitigation of CAR T-cell therapy–associated toxicity at The University of Texas MD Anderson Cancer Center from September 2018 through September 2019, were eligible for this study. During this time, 100 patients with relapsed or refractory LBCL were treated with standard-of-care axi-cel, 41 developed grade ≥3 ICANS, 9 had grade ≥3 CRS, and 5 had HLH. Among these, 8 patients with LBCL (6 with diffuse LBCL and 2 with transformed follicular lymphoma) were treated with anakinra. CRS and ICANS were prospectively graded according to the CAR toxicity (CARTOX) grading system.10 An unpaired Student t test was used for area-under-the-curve comparisons.
Baseline characteristics are shown in Table 1. The indication for use of anakinra was high-grade ICANS in 6 patients and HLH in 2 patients. At the time of initiation of anakinra, the median cumulative dexamethasone equivalent dose was 273 mg (range, 0-1344), and the median cumulative tocilizumab dose was 1080 mg (range, 0-1480; with a median of 2 doses of 8 mg/kg each). Anakinra was started at a median of 12 days (range, 6-41) after axi-cel infusion, with a median daily dose of 100 mg (range, 50-200 mg) subcutaneously (SC), for a median of 7 days (range, 1-7) and a median cumulative dose of 700 mg (range, 200-700 mg). Although none of the patients continued to receive tocilizumab after initiation of anakinra, all continued to receive corticosteroids, for a cumulative dexamethasone equivalent dose of 722 mg (range, 10-1545 mg).
Table 1.
Baseline characteristics at day −5 before initiation of conditioning
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 | Patient 7 | Patient 8 | |
|---|---|---|---|---|---|---|---|---|
| Age, y | 46 | 72 | 60 | 83 | 59 | 76 | 24 | 38 |
| Sex | Female | Male | Male | Male | Male | Female | Male | Female |
| ECOG PS | 1 | 2 | 0 | 2 | 0 | 1 | 1 | 3 |
| Histology | DLBCL | DLBCL | tFL | DLBCL | DLBCL | tFL | DLBCL | DLBCL |
| Ann Arbor stage | IV | III | IV | IV | IV | III | IV | IV |
| IPI score | 3 | 4 | 3 | 4 | 3 | 3 | 3 | 4 |
| Prior CNS lymphoma | No | No | No | Yes | No | No | No | No |
| Previous treatment | ||||||||
| Previous therapies, n | 2 | 2 | 6 | 3 | 3 | 3 | 3 | 4 |
| Refractory disease | No | No | Yes | Yes | No | Yes | Yes | Yes |
| Previous ASCT | Yes | Yes | Yes | No | Yes | No | No | No |
| Inflammatory and disease burden markers | ||||||||
| CRP, mg/L | 2 | 13 | 51 | 4 | 232 | 35 | 191 | 214 |
| Ferritin, mg/L | 1554 | 1135 | 3332 | 628 | 14 240 | 190 | 8718 | 6183 |
| LDH > ULN | No | No | No | No | Yes | No | Yes | Yes |
| Toxicity management | ||||||||
| Treated toxicity | ICANS G4 | ICANS G3 | ICANS G4 | ICANS G4 | ICANS G4 | ICANS G4 | HLH | HLH |
| Tocilizumab start | Day 4 | Day 5 | — | Day 4 | Day 4 | — | Day 3 | Day 11 |
| Tocilizumab dose | 8 mg/kg IV ×2 | 8 mg/kg IV ×2 | 0 | 8 mg/kg IV ×2 | 8 mg/kg IV ×2 | 0 | 8 mg/kg IV ×1 | 8 mg/kg IV ×2 |
| Corticosteroid start | Day 4 | Day 5 | Day 34 | Day 5 | Day 6 | Day 7 | Day 3 | Day 7 |
| Dexamethasone dose | 8-186 mg ×24 d | 1-186 mg ×57 d | 10 mg ×1 d | 40-186 mg ×13 d | 40-80 mg ×19 d | 4-186 mg ×35 d | 12-186 mg ×14 d | 40-80 mg ×9 d |
| Anakinra start | Day 6 | Day 41 | Day 31 | Day 7 | Day 10 | Day 31 | Day 7 | Day 14 |
| Anakinra dose | 100 mg SC daily ×7 | 100 mg SC daily ×7 | 100 mg SC daily ×7 | 100 mg SC daily ×7 | 100 mg SC every other day ×5 | 100 mg SC daily ×7 | 100 mg SC daily ×7 | 200 mg SC daily ×1 |
| Response to anakinra | ||||||||
| Toxicity response | Yes (G0) | Yes (G1) | Yes (G0) | Yes (G2) | No | No | No | No |
| Toxicity recurrence | No | No | No | Yes | Yes | Yes | Yes | Yes |
| Day of death (cause) | — | Day 80 (pneumonia) | Day 71 (HLH) | Day 18 (PD) | Day 31 (ICH) | Day 51 (ICANS) | Day 17 (PD) | Day 15 (HLH) |
No patient had received previous CAR T-cell therapy or ASCT. Seven of 8 patients were admitted to an intensive care unit. One patient had not received corticosteroids, and 2 had not received tocilizumab before initiation of anakinra.
ASCT, autologous stem cell transplantation; CNS, central nervous system; DLBCL, diffuse LBCL; ECOG PS, European Cooperative Oncology Group performance status; G, grade; ICH, intracranial hemorrhage; IPI, International Prognostic Index; PD, progressive disease; tFL, transformed follicular lymphoma; ULN, upper limit of normal.
Overall, 4 patients had a clinical response after initiation of anakinra, and 4 were refractory (Figure 1A).
Figure 1.
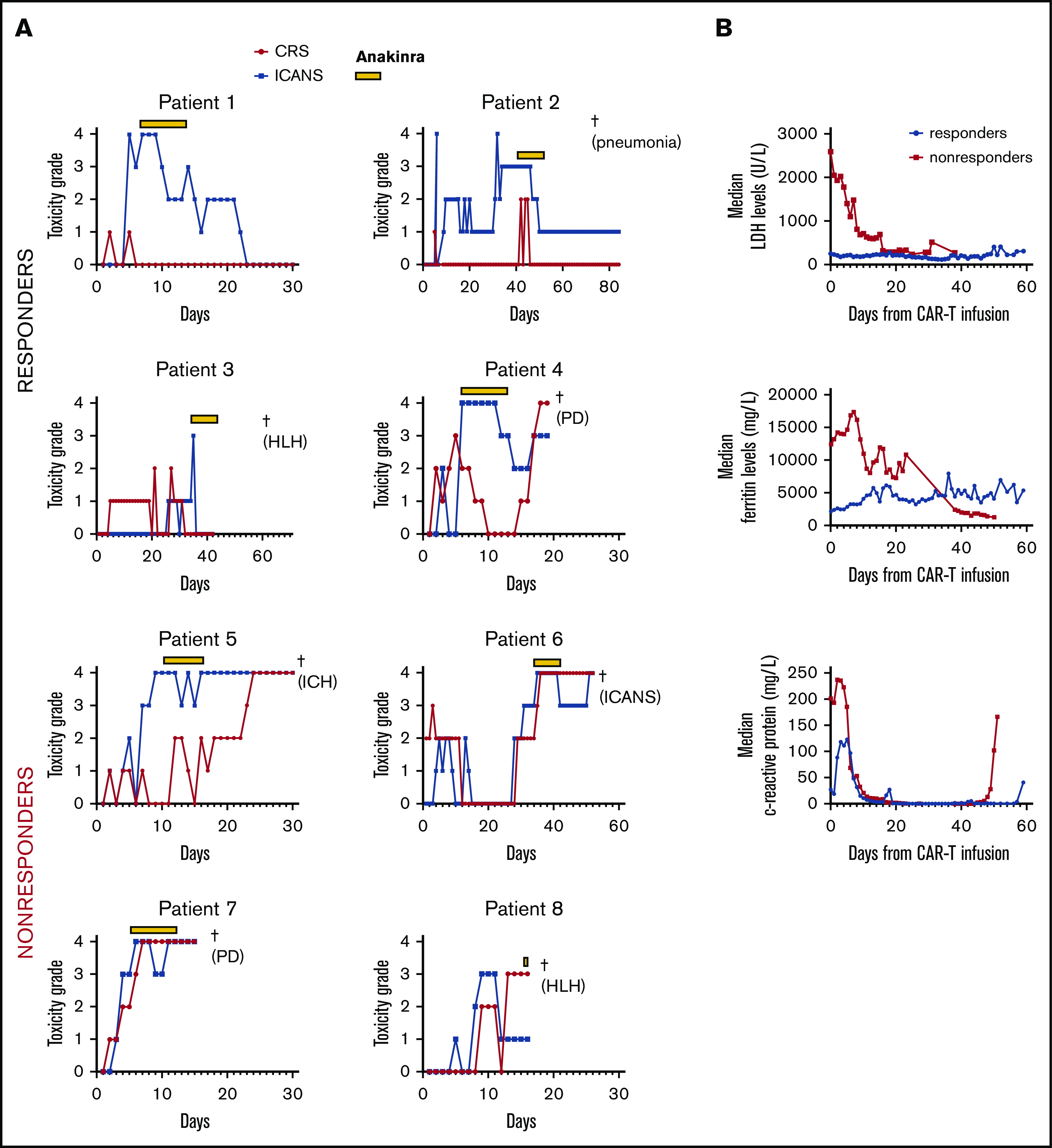
Trend of toxicity and inflammatory markers. (A) The toxicity grade trend for each patient, including responders and nonresponders to anakinra. (B) LDH, ferritin, and CRP trends and associations with response to anakinra. †Fatal event (cause). In patient 5, ICH was present before anakinra initiation. In both patients treated for HLH, the latter was characterized by pancytopenia, elevated serum ferritin and triglyceride levels, decreased fibrinogen levels, and bone marrow evidence of hemophagocytosis. None of the 4 patients who responded to anakinra had LDH >500 U/L, ferritin >10 000 mg/L, or CRP >300 mg/L. Because of the small sample size, differences did not reach statistical significance (P = .55 [ferritin]; P = .77 [CRP]; P = .26 [LDH]). ICH, intracranial hemorrhage; PD, progressive disease.
In all 4 responders, the indication for use of anakinra was high-grade ICANS, and all received 100 mg SC daily for 7 days. Patient 1 started anakinra on day 6 for grade 4 ICANS (after a cumulative dexamethasone dose of 336 mg and a cumulative tocilizumab dose of 1480 mg), with durable conversion to low-grade ICANS on day 10 and a decrease to grade 0 on day 22 (a cumulative dexamethasone dose of 1081 mg was provided during treatment with anakinra). The patient achieved complete response (CR) on day 30 and was in remission 9 months after axi-cel infusion. Patient 2 started anakinra on day 41 for grade 3 ICANS (after a cumulative dexamethasone dose of 1344 mg and a cumulative tocilizumab dose of 1180 mg), with durable conversion to low-grade ICANS on day 46 (a cumulative dexamethasone dose of 333 mg was provided during treatment with anakinra). The patient died of severe pneumonia on day 80, while in CR and with persistent grade 1 ICANS (represented by mild cognitive impairment). Patient 3 started anakinra on day 31 for grade 3 ICANS (with no previous exposure to corticosteroids and/or tocilizumab), with a decrease to grade 0 on day 35 (a single dose of dexamethasone 10 mg was provided during treatment with anakinra), but died of HLH on day 71, while in CR. Patient 4 started anakinra on day 7 for grade 4 ICANS (after a cumulative dexamethasone dose of 140 mg and a cumulative tocilizumab dose of 1400 mg), with temporary conversion to low-grade ICANS on day 13 (a cumulative dexamethasone dose of 1336 mg was provided during treatment with anakinra). After the patient completed 7 days of anakinra, high-grade (grade ≥3) ICANS recurred on day 16, and he died of progressive LBCL on day 18. Response to anakinra was associated with lower area-under-the-curve lactate dehydrogenase (LDH), serum ferritin, and c-reactive protein (CRP) levels (Figure 1B).
Among the 4 nonresponders, the indication for use of anakinra was high-grade ICANS in 2 patients and HLH in 2. Patient 5 started anakinra for grade 4 ICANS, at a dose of 100 mg every other day (because of renal dysfunction), on day 10 (after a cumulative dexamethasone dose of 210 mg and a cumulative tocilizumab dose of 1360 mg), for 10 days (a cumulative dexamethasone dose of 735 mg was provided during treatment with anakinra). No change in ICANS grade was observed, and the patient died of intracranial hemorrhage on day 31. Patient 6 started anakinra for grade 4 ICANS (after a cumulative dexamethasone dose of 166 mg and no previous exposure to tocilizumab), at a dose of 100 mg SC daily, on day 31, for 7 days (a cumulative dexamethasone dose of 1545 mg was provided during treatment with anakinra). No change in ICANS grade was observed, and the patient died of severe ICANS on day 51. Patient 7 started anakinra for steroid-refractory HLH on day 7 (after a cumulative dexamethasone dose of 465 mg and a cumulative tocilizumab dose of 800 mg), at a dose of 100 mg SC daily for 7 days, along with etoposide (a cumulative dexamethasone dose of 708 mg was provided during treatment with anakinra). No improvement was observed, and the patient died of progressive lymphoma on day 17. Patient 8 started anakinra for steroid- and etoposide-refractory HLH on day 14 (after a cumulative dexamethasone dose of 450 mg and a cumulative tocilizumab dose of 980 mg), at a dose of 200 mg SC. The patient died of HLH on day 15, after only 1 dose of anakinra.
In our series, 4 of 6 patients who received anakinra for the management of high-grade ICANS experienced clinical benefit. Although the onset of high-grade (grade ≥3) CRS has been associated with higher response rates and longer survival,11 the onset of high-grade ICANS has been associated with worse outcomes.12 Because tocilizumab is not effective for the treatment of ICANS without CRS, corticosteroids remain the cornerstone of its management. Their use, however, may hamper the activity of CAR T cells, thus explaining the prognostic impact of severe CRS in contrast with ICANS. This finding further supports the need to develop steroid-sparing agents for the treatment or prevention of ICANS, such as anakinra.
One of 4 responders had only a transient benefit, and eventually succumbed to progressive LBCL. In a mouse model of CAR T-cell therapy–associated toxicity, IL-1 blockade did not affect CAR T-cell expansion or disease clearance.4,5 Despite encouraging data, the potential effects of anakinra on CAR T-cell amplification and function remain to be fully investigated in humans.
In 2 of the 6 patients with high-grade ICANS, no clinical activity of anakinra was appreciated, despite similar doses and schedules, as compared with those of the 4 responders. IL-1 has been shown to peak in the serum of patients with relapsed or refractory LBCL within the first 7 days after axi-cel infusion.3 In this series, median time to initiation of anakinra was 12 days, a potential explanation of its limited activity. This result is further supported by the association between early elevated serum ferritin and CRP levels and lack of clinical efficacy of anakinra. Resistance to anakinra may also have been caused by pharmacokinetic problems, including route of administration and schedule, which may have limited achievement of adequate concentrations in the blood and cerebral spinal fluid.13
Neither of the 2 patients in whom anakinra was used for management of HLH experienced any clinical benefit. This result is in contrast with recently published data showing clinical efficacy of anakinra for the treatment of HLH associated with the use of anti-CD22 CAR T-cell therapy.14 The biological mechanisms of HLH in patients treated with anti-CD22 CAR T cells may differ from those treated with anti-CD19 CAR T cells, and an interstudy comparison is not possible. In addition, in the former study, the use of anakinra was early and systematic and at a higher dose, whereas in this series, treatment began late and was guided by the treating physician’s preference at a lower dose. It is interesting to note that ICANS response to anakinra mirrored CRS response, as expected based on the above outlined preclinical data.4,5 Systematic measurement of IL-1 not only in blood, but also in the cerebral spinal fluid, will help to shed light on the pathophysiology of these toxicities and their response to IL-1 blockade.
Finally, the association between early elevated levels of serum LDH and lack of clinical efficacy of anakinra suggests that high disease burden and early progression limit its activity.
We acknowledge some major limitations of our observations, including their retrospective and single-center nature, the small sample size, and the lack of serial IL-1 serum measurements in these patients.
In summary, anakinra represents a potential steroid-sparing strategy for the treatment of CAR T-cell therapy–associated toxicities, mainly ICANS. Although overall outcomes were dismal when anakinra was used as a last resource, clinical trials investigating its early and/or prophylactic use are ongoing (registered at clinicaltrials.gov #NCT04432506, #NCT04359784, #NCT04148430, and #NCT04205838) and upcoming (from this institution) and may bear more favorable results.
Acknowledgments:
This work was supported by National Institutes of Health, National Cancer Institute grant P30 CA016672 (MD Anderson Cancer Center). P.S. is supported by a Lymphoma Research Foundation Career Development Award, and M.R.G. by a Leukemia and Lymphoma Society Scholar Award.
Contribution: P.S. and S.S.N. designed the study and analyzed the data; P.S. wrote the paper; P.K., L.J.N., J.R.W., M.A.R., R.N., S.A., and E.J.S. provided clinical care to the patients; M.R.G., C.M.C., G.W., S.H., A.R.T.B., M.A.R., R.N., and D.O. coauthored the manuscript; C.M.C., G.W., S.H., A.R.T.B., B.D., and D.O. collected the clinical data; M.R.G. critically analyzed the data and cases; S.S.N. wrote the manuscript; and all authors reviewed and approved the manuscript.
Conflict-of-interest disclosure: S.S.N. has received honoraria and research support from Kite, a Gilead company, Merck, and Celgene; research support from Bristol-Myers Squibb, Poseida, Cellectis, Karus, and Acerta Pharma; and honoraria from Novartis, Pfizer, and Unum Therapeutics. L.J.N. has received honoraria from Celgene, Genentech, Gilead, Janssen, Juno, Novartis, and Spectrum; and research support from Celgene, Genentech, Janssen, and Merck. J.R.W. has received honoraria and research support from Kite, Bristol-Myers Squibb, Novartis, and Unum Therapeutics. The remaining authors declare no competing financial interests.
Correspondence: Paolo Strati, Department of Lymphoma and Myeloma, The University of Texas MD Anderson Cancer Center, 1515 Holcombe Blvd, Unit 428, Houston, TX 77030; e-mail: pstrati@mdanderson.org.
References
- 1.Yoder AK, Gunther JR, Milgrom SA, et al. Hitting a moving target: successful management of diffuse large B-cell lymphoma involving the mesentery with volumetric image-guided intensity modulated radiation therapy. Clin Lymphoma Myeloma Leuk. 2019;19(1):e51-e61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holscher CM, Haugen CE, Jackson KR, et al. Self-reported incident hypertension and long-term kidney function in living kidney donors compared with healthy nondonors. Clin J Am Soc Nephrol. 2019;14(10):1493-1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Locke FL, Rossi J, Xue X, et al. Immune signatures of cytokine release syndrome and neurologic events in a multicenter registrational trial (ZUMA-1) in subjects with refractory diffuse large B cell lymphoma treated with axicabtagene ciloleucel (KTE-C19) [abstract]. Cancer Res 2017;77(suppl 13). Abstract CT020.
- 4.Norelli M, Camisa B, Barbiera G, et al. Monocyte-derived IL-1 and IL-6 are differentially required for cytokine-release syndrome and neurotoxicity due to CAR T cells. Nat Med. 2018;24(6):739-748. [DOI] [PubMed] [Google Scholar]
- 5.Giavridis T, van der Stegen SJC, Eyquem J, Hamieh M, Piersigilli A, Sadelain M. CAR T cell-induced cytokine release syndrome is mediated by macrophages and abated by IL-1 blockade. Nat Med. 2018;24(6):731-738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Genovese MC, Cohen S, Moreland L, et al. ; 20000223 Study Group . Combination therapy with etanercept and anakinra in the treatment of patients with rheumatoid arthritis who have been treated unsuccessfully with methotrexate. Arthritis Rheum. 2004;50(5):1412-1419. [DOI] [PubMed] [Google Scholar]
- 7.Goldbach-Mansky R, Dailey NJ, Canna SW, et al. Neonatal-onset multisystem inflammatory disease responsive to interleukin-1beta inhibition. N Engl J Med. 2006;355(6):581-592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rajasekaran S, Kruse K, Kovey K, et al. Therapeutic role of anakinra, an interleukin-1 receptor antagonist, in the management of secondary hemophagocytic lymphohistiocytosis/sepsis/multiple organ dysfunction/macrophage activating syndrome in critically ill children. Pediatr Crit Care Med. 2014;15(5):401-408. [DOI] [PubMed] [Google Scholar]
- 9.Shakoory B, Carcillo JA, Chatham WW, et al. Interleukin-1 receptor blockade Is associated with reduced mortality in sepsis patients with features of macrophage activation syndrome: reanalysis of a prior phase III trial. Crit Care Med. 2016;44(2):275-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Neelapu SS, Tummala S, Kebriaei P, et al. Chimeric antigen receptor T-cell therapy - assessment and management of toxicities. Nat Rev Clin Oncol. 2018;15(1):47-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jacobs MT, Jain MD, Spiegel JY, et al. Characteristics and outcomes of patients who did not develop CRS after axicabtagene ciloleucel for relapsed/refractory large B-Cell lymphoma: results from the US Lymphoma CAR-T Consortium [abstract]. Blood. 2019;134(suppl 1). Abstract 1583. [Google Scholar]
- 12.Strati P, Tummala S, Nastoupil LJ, et al. Clinical and radiological correlates of neurotoxicity after standard of care axicabtagene ciloleucel in patients with relapsed/refractory large B-cell lymphoma [abstract]. Blood. 2019;134(suppl 1). Abstract 765. [Google Scholar]
- 13.Mehta P, Cron RQ, Hartwell J, Manson JJ, Tattersall RS. Silencing the cytokine storm: the use of intravenous anakinra in haemophagocytic lymphohistiocytosis or macrophage activation syndrome Lancet Rheumatol. 2020;2(6):e358-e367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shah NN, Highfill SL, Shalabi H, et al. CD4/CD8 T-cell selection affects chimeric antigen receptor (CAR) T-cell potency and toxicity: updated results from a phase I anti-CD22 CAR T-cell trial. J Clin Oncol. 2020;38(17):1938-1950. [DOI] [PMC free article] [PubMed] [Google Scholar]


