Key Points
Non–ANT-based regimen chemotherapy was associated with a survival improvement in the entire cohort and risk subgroups.
Abstract
The present study investigated the survival benefit of non–anthracycline (ANT)-based vs ANT-based regimens in a large-scale, real-world cohort of patients with extranodal natural killer (NK)/T-cell lymphoma, nasal type (ENKTCL). Within the China Lymphoma Collaborative Group (CLCG) database (2000-2015), we identified 2560 newly diagnosed patients who received chemotherapy with or without radiotherapy. Propensity score matching (PSM) and multivariable analyses were used to compare overall survival (OS) and progression-free survival (PFS) between the 2 chemotherapy regimens. We explored the survival benefit of non–ANT-based regimens in patients with different treatments in early-stage disease and in risk-stratified subgroups. Non–ANT-based regimens significantly improved survivals compared with ANT-based regimens. The 5-year OS and PFS were 68.9% and 59.5% for non–ANT-based regimens compared with 57.5% and 44.5% for ANT-based regimens in the entire cohort. The clinical advantage of non–ANT-based regimens was substantial across the subgroups examined, regardless of stage and risk-stratified subgroup, and remained significant in early-stage patients who received radiotherapy. The survival benefits of non–ANT-based regimens were consistent after adjustment using multivariable and PSM analyses. These findings provide additional evidence supporting non–ANT-based regimens as a first-line treatment of patients with ENKTCL.
Visual Abstract
Introduction
Extranodal natural killer/T-cell lymphoma, nasal type (ENKTCL) is rare in Western populations but more frequent in East Asia.1-3 The disease is unique among aggressive lymphomas in terms of its clinical features and treatment principle. ENKTCL is resistant to anthracycline (ANT)-based regimens but sensitive to radiation.2,4-6 Radiotherapy plays an important role in both locoregional disease control and maintaining long-term survival in early-stage patients.2-6 In a recent registry study from the National Cancer Database,2 the omission or inadequate dose (<50 Gy) of radiotherapy is negatively associated with overall survival (OS). Furthermore, in a previous study from the China Lymphoma Collaborative Group (CLCG),6 improved locoregional control using appropriate radiotherapy is associated with prolonged OS and progression-free survival (PFS). Primary radiotherapy achieves a favorable prognosis in patients with early-stage ENKTCL,4-6 whereas adding ANT-based chemotherapy into radiotherapy significantly improves survival in high-risk early-stage patients.5 However, the prognosis of patients with localized or disseminated diseases is poor using ANT-based chemotherapy alone.2,5
Prospective phase 1/2 trials and retrospective studies demonstrated that non–ANT-based regimens provided survival benefits compared with ANT-based regimens in newly diagnosed or relapsed/refractory ENKTCL.7-18 A variety of non–ANT-based regimens, mainly asparaginase (ASP)-based regimens, have been recommended as first-line treatments for ENKTCL. However, evidence supporting the clinical use of non–ANT-based regimens is limited to single-arm phase 1/2 trials or retrospective studies with small cohorts of patients. The restrictive recruitment criteria in prospective uncontrolled trials might select out suitable young patients with preserved organ function, leading to favorable treatment outcomes. Therefore, the beneficial effect of non–ANT-based regimens needs to be validated in a large comparative study.
Given the rarity of ENKTCL and the difficulty in conducting randomized controlled trials, we designed a large-scale retrospective study to compare the survival benefit of non–ANT-based over ANT-based regimens.
Methods
Patient inclusion
The renewed ENKTCL database from the CLCG included 3046 patients between 2000 and 2015 from 20 institutions. The eligibility criteria for this study included: (1) a newly diagnosed ENKTCL with the typical histological and immunophenotypic evaluations that included CD20/CD79α, CD3ε, CD3s, CD56, cytotoxic molecules (TIA-1, Gram-B, perforin), and Epstein-Barr virus–encoded RNA in situ hybridization, according to the World Health Organization classification of lymphomas; (2) patients received chemotherapy with or without radiotherapy; and (3) complete clinicopathologic and follow-up information. Patients receiving radiotherapy alone (n = 389) or unknown regimens (n = 97) were excluded. Finally, 2560 patients formed the study population. The institutional review boards approved the project and waived the need for informed consent because of the deidentification of patient data.
Evaluation, definition, and treatment
Clinical staging evaluation and the definition of primary tumor invasion (PTI) have been described previously.18 Briefly, clinical evaluation included history and physical examination; endoscopy of the upper-aerodigestive tract (UADT); blood biochemistry; computed tomography (CT) scans of the head and neck, chest, abdomen, and pelvis; magnetic resonance imaging of the head and neck; and bone marrow examination. Positron emission tomography (PET) CT has been recommended for all patients since 2010, particularly for those with locally advanced-stage or disseminated diseases. Patients were staged using the Ann Arbor staging system and stratified using 3 ENKTCL-specific models: the nomogram-revised risk index,3,19 the Korea prognostic index,20 and the prognostic index of natural killer lymphoma.21 Quantitative measurement of circulating Epstein-Barr virus DNA was not performed in this study.
Chemotherapy was dichotomized into non–ANT-based (n = 1351, 52.8%) and ANT-based regimens (n = 1209, 47.2%). ANT-based regimens included CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone; n = 919) or CHOP-like (CHOP plus etoposide; n = 290), whereas the most commonly used non–ANT-based regimens were ASP (l-ASP or pegaspargase)–containing regimens (n = 1054), followed by platinum-containing (n = 166) and gemcitabine (GEM)–containing (n = 131) regimens. Based on previous systematic review and meta-analysis studies on efficacy and toxicity,22,23 we further subclassified non–ANT-based regimens into 5 categories (supplemental Table 1): ASP/ANT based (30.3%), ASP/GEM based (25.5%), ASP/methotrexate based (8.8%), ASP/not otherwise specified based (13.4%), and platinum/other regimens (18.9%, usually with GEM). The median number of chemotherapy cycles was 4. Extended involved-site radiotherapy was delivered, with a median dose of 50 Gy.
End point and statistics
Primary end points were OS and PFS. OS was calculated from the date of first treatment until the time of death or last follow-up and PFS from the date of first treatment until the date of disease progression, relapse, death, or time of last follow-up. Survival was estimated using the Kaplan-Meier method and compared using a log-rank test. Propensity score matching (PSM) analysis was applied to adjust confounding variables and generate comparable study arms; 1:1 patient matching without replacement was used to pair each patient receiving non–ANT-based regimens with another patient receiving ANT-based regimens whose propensity score was within the designated caliper size. After PSM, baseline covariates and survival rates were compared between chemotherapy groups. Standardized mean difference is used to examine the balance of covariate distribution between treatment groups. Covariates were considered well balanced when the standardized mean difference was <0.10. The measured covariate balances were assessed both graphically and analytically. Cox proportional hazards regression was performed for multivariable analysis in entire group and prespecified subgroups based on ENKTCL-specific models. The interactions between covariates and treatment in Cox model were checked.
Results
Patient characteristics
The patient characteristics are summarized (Table 1). The median age was 43 years (range, 6-84 years), and the male-to-female ratio was 2.42:1. Most patients had good performance status and primary UADT site (93.8%). Elevated LDH was present in 31.5% of patients, PTI was present in 57.3%, and the majority had early-stage disease (87.0%).
Table 1.
Patient characteristics stratified by chemotherapy regimens before and after PSM for patients with all stages, early-stage, and advanced-stage disease
| Characteristic | Total | Before PSM | After PSM | ||||
|---|---|---|---|---|---|---|---|
| Non–ANT based | ANT based | P | Non–ANT based | ANT based | P | ||
| All stages (n = 2560) | 2560 | 1351 | 1209 | 1114 | 1114 | ||
| Male sex | 1811 (70.7) | 956 (70.8) | 855 (70.7) | .981 | 731 (65.6) | 766 (68.8) | .114 |
| Age >60 y | 309 (12.1) | 165(12.2) | 144 (11.9) | .815 | 129 (11.6) | 128 (11.5) | .947 |
| B symptoms | 1106 (43.2) | 575 (42.6) | 531 (43.9) | .488 | 560 (50.3) | 525 (47.1) | .138 |
| ECOG score ≥2 | 198 (7.7) | 89 (6.6) | 109 (9.0) | .022 | 72 (6.5) | 72 (6.5) | 1.000 |
| Stage I-II | 2226 (87.0) | 1156 (85.6) | 1070 (88.5) | .028 | 979 (87.9) | 979 (87.9) | 1.000 |
| PTI | 1466 (57.3) | 777 (57.5) | 689 (57.0) | .789 | 635 (57.0) | 638 (57.3) | .898 |
| Elevated LDH | 807 (31.5) | 392 (29.0) | 415 (34.3) | .004 | 346 (31.1) | 346 (31.1) | 1.000 |
| UADT site | 2400 (93.8) | 1248 (92.4) | 1152 (95.3) | .002 | 1060 (95.2) | 1060 (95.2) | 1.000 |
| Regional LN involvement | 984 (38.4) | 564 (41.7) | 420 (34.7) | <.001 | 410 (36.8) | 410 (36.8) | 1.000 |
| Distant LN involvement | 160 (6.2) | 88 (6.5) | 72 (6.0) | .560 | 61 (5.5) | 70 (6.3) | .418 |
| Stage I-II (n = 2226) | 2226 | 1156 | 1070 | 968 | 968 | ||
| Male sex | 1576 (70.8) | 812 (70.2) | 764 (71.4) | .548 | 625 (64.6) | 664 (68.6) | .060 |
| Age >60 y | 271 (12.2) | 145 (12.5) | 126 (11.8) | .580 | 116 (12.0) | 112 (11.6) | .778 |
| B symptoms | 929 (41.7) | 469 (40.6) | 460 (43.0) | .247 | 405 (41.8) | 405 (41.8) | 1.000 |
| ECOG score ≥2 | 126 (5.7) | 46 (4.0) | 80 (7.5) | <.001 | 37 (3.8) | 37 (3.8) | 1.000 |
| Stage II | 788 (35.4) | 447 (38.7) | 341 (31.9) | .001 | 330 (34.1) | 330 (34.1) | 1.000 |
| Elevated LDH | 634 (28.5) | 293 (25.3) | 341 (31.9) | .001 | 272 (28.1) | 272 (28.1) | 1.000 |
| PTI | 1269 (57.0) | 647 (56.0) | 622 (58.1) | .303 | 552 (57.0) | 552 (57.0) | 1.000 |
| UADT site | 2152 (96.7) | 1119 (96.8) | 1033 (96.5) | .216 | 933 (96.4) | 943 (97.4) | .190 |
| Stage III-IV (n = 334) | 334 | 195 | 139 | 101 | 101 | ||
| Male sex | 235 (70.4) | 144 (73.8) | 91 (65.5) | .098 | 65 (64.4) | 60 (59.4) | .469 |
| Age >60 y | 38 (11.4) | 20 (10.3) | 18 (12.9) | .445 | 10 (9.9) | 10 (9.9) | 1.000 |
| B symptoms | 177 (53.0) | 106 (54.4) | 71 (51.1) | .554 | 52 (51.5) | 52 (51.5) | 1.000 |
| ECOG score ≥2 | 72 (21.6) | 43 (22.1) | 29 (20.9) | .795 | 34 (33.7) | 26 (25.7) | .218 |
| Elevated LDH | 173 (51.8) | 99 (50.8) | 74 (53.2) | .565 | 49 (48.5) | 49 (48.5) | 1.000 |
| PTI | 197 (59.0) | 130 (66.7) | 67 (48.2) | .001 | 64 (63.4) | 64 (63.4) | 1.000 |
| UADT site | 236 (70.7) | 129 (66.2) | 107 (77.0) | .032 | 77 (76.2) | 77 (76.2) | 1.000 |
| Distant LN involvement | 160 (47.9) | 130 (66.7) | 67 (48.2) | .001 | 45 (44.6) | 45 (44.6) | 1.000 |
Data are presented as n (%) of patients.
ECOG, Eastern Cooperative Oncology Group; LDH, lactate dehydrogenase; LN, lymph node.
Benefit of non–ANT-based regimens in the entire cohort
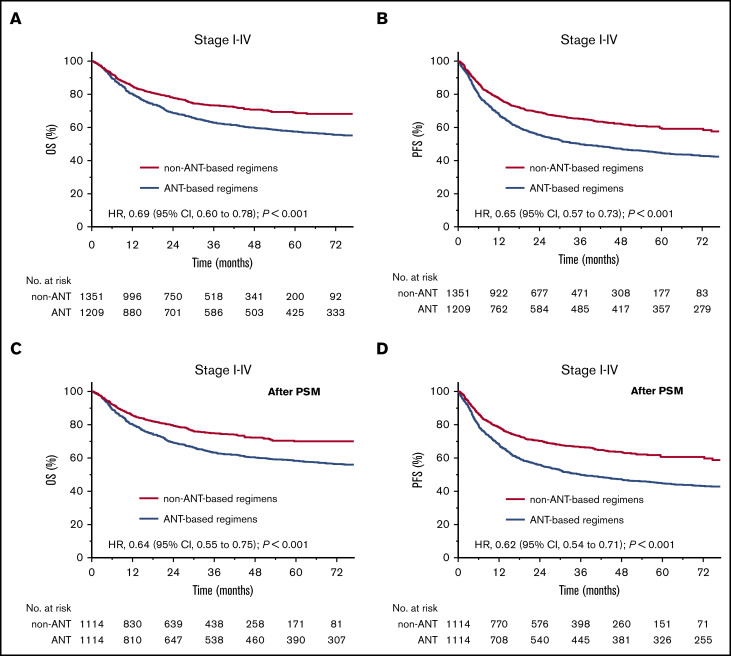
We investigated the survival benefit of non–ANT-based regimens in the entire cohort. With a median follow-up time of 48 months for surviving patients, the 5-year OS and PFS rates were 68.9% (95% confidence interval [CI], 65.9-72.1) and 59.5% (95% CI, 56.3-62.9) for non–ANT-based regimens compared with 57.5% (95% CI, 54.5-60.6; hazard ratio [HR], 0.69; 95% CI, 0.60–0.78; P < .001; Figure 1A) and 44.5% (95% CI, 41.6-47.6; HR, 0.65; 95% CI, 0.57-0.73; P < .001; Figure 1B) for ANT-based regimens.
Figure 1.
OS and PFS stratified by chemotherapy regimens in the entire cohort. OS (A) and PFS (B) of non–ANT-based regimens vs ANT-based regimens before PSM. OS (C) and PFS (D) of non–ANT-based regimens vs ANT-based regimens after PSM.
After adjustment using PSM, the clinical variables were comparable between the 2 groups (Table 1; supplemental Table 2). Non–ANT-based regimens resulted in significantly better OS (HR, 0.64; 95% CI, 0.55-0.75; P < .001; Figure 1C) and PFS (HR, 0.62; 95% CI, 0.54-0.71; P < .001; Figure 1D) than ANT-based regimens. After adjusting for confounding variables, treatments, and time periods via multivariable analysis, in addition to other clinical factors (age, performance status, stage, LDH, regional and distant lymph node involvement, and PTI), both non–ANT-based regimens and radiotherapy were independent prognostic factors for survival (Table 2). The HRs for OS and PFS of radiotherapy vs no radiotherapy were 0.42 (95% CI, 0.35-0.49; P < .001) and 0.38 (95% CI, 0.33-0.44; P < .001). The HRs for OS and PFS of non–ANT-based regimens vs ANT-based regimens were 0.72 (95% CI, 0.60-0.85; P < .001) and 0.63 (95% CI, 0.54-0.73; P < .001). Thus, non–ANT-based regimens are associated with ∼30% improvement in OS and PFS in the entire cohort. Since 26.5% of the patients in the non–ANT-based regimens were treated with CHOP plus ASP (CHOP-ASP), a crude comparison with CHOP and CHOP-ASP was made to address the role of ASP in ENKTCL. The addition of ASP to CHOP was associated with significantly better OS and PFS in the entire cohort (supplemental Figure 1). Explorative analysis of survival outcomes with other non–ANT-based regimens was not performed.
Table 2.
Multivariable analysis of OS and PFS for patients with all stages, early-stage, and advanced-stage disease
| Variables | OS | PFS | ||
|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | |
| All stages (n = 2560) | ||||
| Year of treatment | ||||
| 2000-2004 | Reference | Reference | ||
| 2005-2009 | 0.99 (0.81-1.21) | .889 | 1.09 (0.91-1.30) | .343 |
| 2010-2015 | 0.87 (0.70-1.09) | .220 | 0.97 (0.80-1.18) | .763 |
| Sex (female vs male) | 0.91 (0.78-1.06) | .216 | 0.93 (0.80-1.06) | .287 |
| Age (>60 y vs ≤60 y) | 1.61 (1.33-1.95) | <.001 | 1.34 (1.13-1.59) | .001 |
| B symptoms (yes vs no) | 1.01 (0.88-1.17) | .873 | 1.06 (0.94-1.20) | .365 |
| ECOG score (≥2 vs 0-1) | 2.15 (1.76-2.62) | <.001 | 1.80 (1.50-2.17) | <.001 |
| Ann Arbor stage (III-IV vs I-II) | 2.26 (1.77-2.89) | <.001 | 1.96 (1.57-2.45) | <.001 |
| Elevated LDH (yes vs no) | 1.39 (1.20-1.60) | <.001 | 1.17 (1.03-1.32) | .017 |
| PTI (yes vs no) | 1.58 (1.37-1.83) | <.001 | 1.50 (1.33-1.70) | <.001 |
| UADT site (yes vs no) | 1.00 (0.76-1.31) | .987 | 0.90 (0.71-1.14) | .386 |
| Regional LN involvement (yes vs no) | 1.40 (1.21-1.62) | <.001 | 1.25 (1.10-1.42) | <.001 |
| Distant LN involvement (yes vs no) | 1.77 (1.30-2.39) | <.001 | 1.78 (1.35-2.35) | <.001 |
| Radiotherapy (yes vs no) | 0.42 (0.35-0.49) | <.001 | 0.38 (0.33-0.44) | <.001 |
| Regimen (non-ANT vs ANT based) | 0.72 (0.60-0.85) | <.001 | 0.63 (0.54-0.73) | <.001 |
| Stage I-II (n = 2226) | ||||
| Year of treatment | ||||
| 2000-2004 | Reference | Reference | ||
| 2005-2009 | 0.93 (0.75-1.16) | .517 | 1.06 (0.88-1.29) | .519 |
| 2010-2015 | 0.76 (0.59-0.97) | .027 | 0.91 (0.74-1.13) | .401 |
| Sex (female vs male) | 0.85 (0.71-1.02) | .073 | 0.92 (0.79-1.06) | .252 |
| Age (>60 y vs ≤60 y) | 1.54 (1.25-1.91) | <.001 | 1.32 (1.10-1.59) | .004 |
| B symptoms (yes vs no) | 0.99 (0.85-1.16) | .918 | 1.09 (0.95-1.25) | .213 |
| ECOG score (≥2 vs 0-1) | 2.27 (1.77-2.91) | <.001 | 1.97 (1.57-2.47) | <.001 |
| Ann Arbor stage (II vs I) | 1.44 (1.23-1.70) | <.001 | 1.29 (1.13-1.49) | <.001 |
| Elevated LDH (yes vs no) | 1.25 (1.06-1.48) | .008 | 1.08 (0.93-1.24) | .315 |
| PTI (yes vs no) | 1.63 (1.37-1.93) | <.001 | 1.55 (1.35-1.79) | <.001 |
| UADT site (yes vs no) | 0.95 (0.59-1.55) | .843 | 1.24 (0.87-1.78) | .237 |
| Radiotherapy (yes vs no) | 0.43 (0.35-0.51) | <.001 | 0.37 (0.32-0.43) | <.001 |
| Regimen (non-ANT vs ANT based) | 0.79 (0.64-0.97) | .021 | 0.67 (0.56-0.79) | <.001 |
| Stage III-IV (n = 334) | ||||
| Year of treatment | ||||
| 2000-2004 | Reference | Reference | ||
| 2005-2009 | 1.44 (0.83-2.48) | .192 | 1.30 (0.78-2.14) | .312 |
| 2010-2015 | 1.67 (0.96-2.89) | .070 | 1.26 (0.76-2.09) | .371 |
| Sex (female vs male) | 1.02 (0.73-1.41) | .934 | 0.93 (0.69-1.25) | .619 |
| Age (>60 y vs ≤60 y) | 2.24 (1.44-3.48) | <.001 | 1.47 (0.96-2.27) | .079 |
| B symptoms (yes vs no) | 1.16 (0.86-1.58) | .334 | 0.98 (0.74-1.30) | .888 |
| ECOG score (≥2 vs 0-1) | 1.76 (1.26-2.47) | .001 | 1.53 (1.12-2.08) | .008 |
| Elevated LDH (yes vs no) | 1.97 (1.44-2.69) | <.001 | 1.59 (1.20-2.10) | .001 |
| PTI (yes vs no) | 1.42 (1.04-1.93) | .028 | 1.36 (1.02-1.80) | .036 |
| Distant LN involvement (yes vs no) | 0.69 (0.53-0.94) | .020 | 0.61 (0.46-0.82) | .001 |
| Radiotherapy (yes vs no) | 0.38 (0.26-0.54) | <.001 | 0.44 (0.32-0.60) | <.001 |
| Regimen (non-ANT vs ANT based) | 0.55 (0.38-0.78) | .001 | 0.54 (0.-0.75) | <.001 |
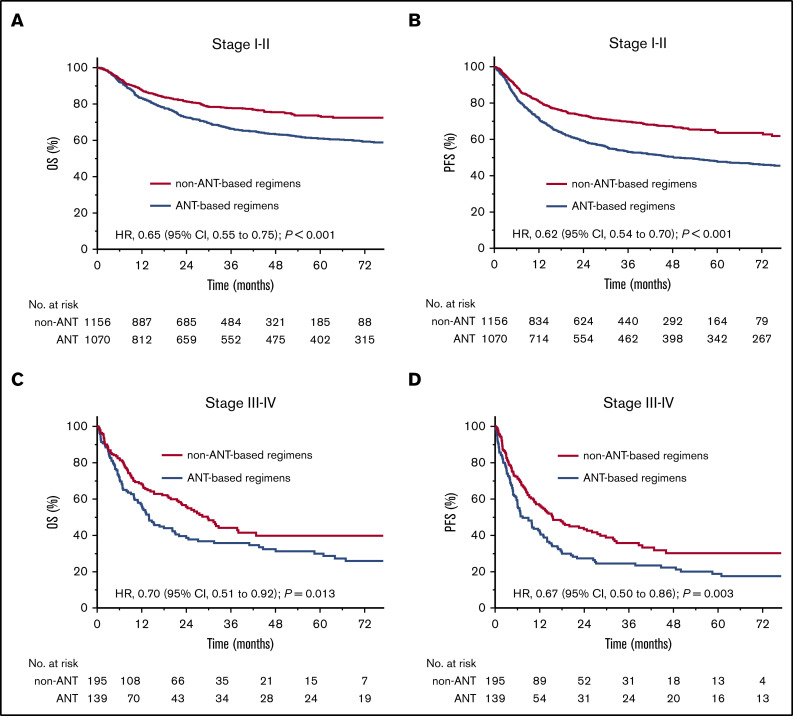
Benefit of non–ANT-based regimens in different stages
We evaluated the survival benefit of non–ANT-based regimens in different stages, because treatment strategies and prognosis varied between early-stage and advanced-stage diseases. In early-stage disease, the 5-year OS and PFS rates were 73.3% (95% CI, 70.2-76.6) and 64.0% (95% CI, 60.6-67.5) for non–ANT-based regimens compared with 61.0% (95% CI, 57.8-64.2; HR 0.65, 95% CI, 0.55–0.75; P < .001; Figure 2A) and 47.8% (95% CI, 44.7-51.1; HR 0.62, 95% CI, 0.54-0.70; P < .001; Figure 2B) for ANT-based regimens. In advanced-stage disease, the 5-year OS and PFS rates were 39.8% (95% CI, 31.7-49.9) and 30.1% (95% CI, 22.8-39.9) for non–ANT-based regimens compared with 29.9% (95% CI, 22.5-39.8; HR 0.70, 95% CI, 0.51-0.92; P = .013; Figure 2C) and 18.8% (95% CI, 12.8-27.7; HR 0.67; 95% CI, 0.50-0.86; P = .003; Figure 2D) for ANT-based regimens.
Figure 2.
OS and PFS stratified by chemotherapy regimens in early-stage and advanced-stage diseases. OS (A) and PFS (B) of non–ANT-based regimens vs ANT-based regimens in early-stage patients before PSM. OS (C) and PFS (D) of non–ANT-based regimens vs ANT-based regimens in advanced-stage patients before PSM.
PSM adequately balanced the clinical variables between the chemotherapy groups (Table 1; supplemental Table 2). The adjusted HRs for OS and PFS of non–ANT-based regimens vs ANT-based regimens were 0.65 (95% CI, 0.55-0.77; P < .001) and 0.61 (95% CI, 0.53-0.70; P < .001) for early-stage patients and 0.63 (95% CI, 0.44-0.89; P = .009) and 0.58 (95% CI, 0.42-0.80; P = .001) for advanced-stage patients. In multivariable analysis (Table 2), the HRs for OS and PFS were 0.79 (95% CI, 0.64-0.97; P = .021) and 0.67 (95% CI, 0.56-0.79; P < .001) for early-stage patients and 0.55 (95% CI, 0.38-0.78; P = .001) and 0.54 (95% CI, 0.39-0.75; P < .001) for advanced-stage patients. Thus, non–ANT-based regimens provided significantly better survival than ANT-based regimens, independent of stages.
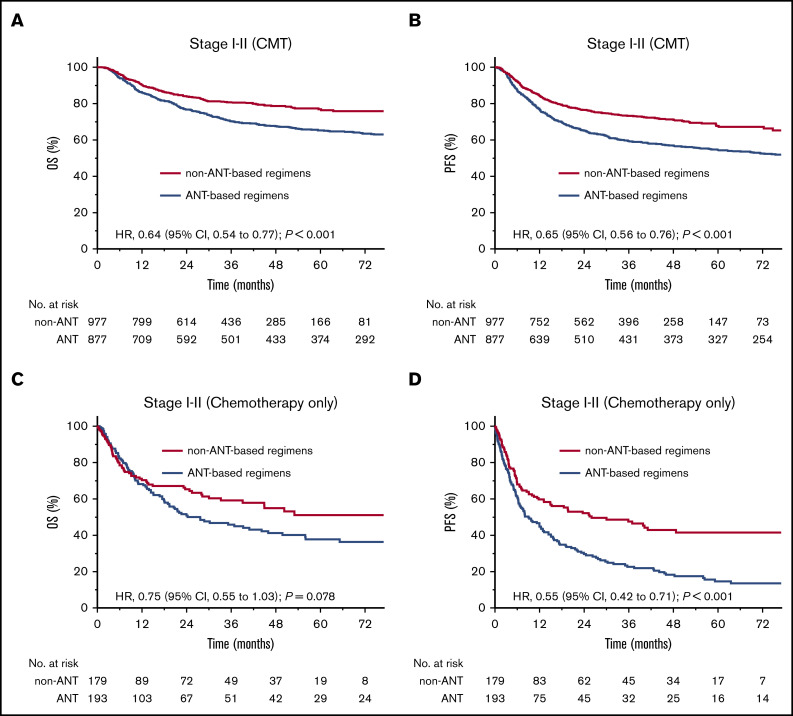
Benefit of non–ANT-based regimens with or without radiotherapy for early-stage disease
We determined whether the benefit of non–ANT-based regimens existed in early-stage patients receiving radiotherapy. For patients receiving combined modality therapy (CMT), the 5-year OS and PFS rates were 77.0% (95% CI, 73.6-80.2) and 67.7% (95% CI, 64.0-71.5) for the non–ANT-based regimens compared with 65.3% (95% CI, 61.9-68.7; HR; 0.64, 95% CI, 0.54-0.77; P < .001; Figure 3A) and 54.4% (95% CI, 51.0-58.0; HR, 0.65; 95% CI, 0.56-0.76; P < .001; Figure 3B) for ANT-based regimens. For patients receiving chemotherapy only, the 5-year OS and PFS rates were 50.1% (95% CI, 42.0-62.1) and 39.7% (95% CI, 33.5-51.3) for non–ANT-based regimens compared with 36.7% (95% CI, 30.2-47.2; HR, 0.75; 95% CI, 0.55-1.03; P = .078; Figure 3C) and 14.1% (95% CI, 9.7-21.8; HR, 0.55; 95% CI, 0.42-0.71; P < .001; Figure 3D) for ANT-based regimens.
Figure 3.
OS and PFS stratified by chemotherapy regimens in early-stage patients receiving CMT or chemotherapy only. OS (A) and PFS (B) of non–ANT-based regimens vs ANT-based regimens in early-stage patients receiving CMT before PSM. OS (C) and PFS (D) of non–ANT-based regimens vs ANT-based regimens in early-stage patients receiving chemotherapy only before PSM.
After adjustment with PSM, matched cohorts were well balanced in early-stage disease (supplemental Tables 2 and 3). The adjusted HRs for OS and PFS (non–ANT-based vs ANT-based regimens) were 0.60 (95% CI, 0.49-0.74; P < .001) and 0.59 (95% CI, 0.50-0.71; P < .001) for CMT, and 0.78 (95% CI, 0.55-1.10; P = 0.161) and 0.57 (95% CI, 0.43-0.76; P < .001) for chemotherapy only. In multivariable analysis (supplemental Table 4), the HRs for OS and PFS were 0.64 (95% CI, 0.50-0.83; P = .001) and 0.60 (95% CI, 0.48-0.74; P < .001) for CMT, and 1.11 (95% CI, 0.73-1.69; P = 0.633) and 0.69 (95% CI, 0.48-0.98; P = .037) for chemotherapy only. Thus, non–ANT-based regimens significantly improved the PFS for early-stage ENKTCL, independent of radiotherapy.
In early-stage patients who received either non–ANT-based regimens or ANT-based regimens, chemotherapy alone was associated with significantly inferior survivals compared with CMT (Figure 4). The HRs of CMT vs chemotherapy alone were 0.36 (95% CI, 0.24-0.54; P < .001; Figure 4A) for OS and 0.38 (95% CI, 0.27-0.54; P < .001; Figure 4B) for PFS in the non–ANT-based regimens group; and 0.43 (95% CI, 0.32-0.59; P < .001; Figure 4C) for OS and 0.33 (95% CI, 0.25-0.43; P < .001; Figure 4D) for PFS in the ANT-based regimens group.
Figure 4.
OS and PFS stratified by treatment options in early-stage patients receiving non–ANT-based or ANT-based regimens. OS (A) and PFS (B) of CMT vs CT alone in early-stage patients receiving non–ANT-based regimens before PSM. OS (C) and PFS (D) of CMT vs CT alone in early-stage patients receiving ANT-based regimens before PSM.
The sequences of treatment with radiotherapy and chemotherapy were evaluated in early-stage patients who received either non–ANT-based or ANT-based regimens. The baseline characteristics in each group are listed in supplemental Table 5. In either group, radiotherapy followed by chemotherapy was associated with a better survival than chemotherapy followed by radiotherapy (supplemental Figure 2).
Benefit of non–ANT-based regimens in risk-stratified groups
We evaluated the benefit of non–ANT-based regimens in the risk-stratified patients according to 3 ENKTCL-specific models. Figure 5 shows the 5-year OS and PFS rates and HRs of the non–ANT-based regimens vs the ANT-based regimens in each risk subgroup. Non–ANT-based regimens were associated with a significant PFS benefit across all risk subgroups within each model. The HRs for PFS ranged from 0.47 to 0.75 (all P < .05), whereas the HRs for OS varied from 0.47 to 0.80 across these risk subgroups. Thus, non–ANT-based regimens appear to be beneficial in risk-stratified patients.
Figure 5.
Forest plot depicting the HRs of non–ANT-based regimens vs ANT-based regimens in different risk subgroups according to the 3 risk models. KPI, Korea prognostic index; NRI, nomogram-revised risk index; PINK, prognostic index of natural killer lymphoma.
Discussion
This is a large-scale, real-world multicenter comparison of non–ANT-based regimens with ANT-based regimens to treat ENKTCL. Non–ANT-based regimens provided OS and PFS benefits over ANT-based regimens, even after adjusting for prognostic confounders and time periods via PSM and multivariable analyses. The clinical advantage of non–ANT-based regimens was consistent across all subgroups examined, regardless of stage and risk subgroup, and was retained for early-stage patients receiving radiotherapy.
Treatment of ENKTCL has evolved, with the introduction of up-front modern radiotherapy and non–ANT-based chemotherapy that have improved survival outcomes.2,4-18,24-28 However, there are no published data describing the benefit of non–ANT-based regimens in a randomized controlled trial or a large multicenter comparative study. The present comprehensive study from real-world data represents a critical step toward understanding the effect of non–ANT-based regimens on long-term survival. Our study provided direct comparison information with abundant sample size, which allowed statistical adjustments for potentially confounding factors, and showed a decreased mortality risk of ∼30% using non–ANT-based regimens in the entire cohort. Non–ANT-based regimens significantly improved PFS and OS for ENKTCL. The beneficial effect of non–ANT-based regimens remained consistent after adjustments using PSM and multivariable analyses and persisted within different stages and individual risk groups. The survival benefit profiles of non–ANT-based regimens after risk stratification could be used for risk-adapted therapy deintensification or intensification in ENKTCL. The survival gain in this large cohort of patients across a substantial number of institutions demonstrated the efficacy and feasibility of non–ANT-based chemotherapy for ENKTCL.
Improvements in long-term survival have been reported in the first-line treatment of early-stage patients over the last decade, mainly as a result of adding radiotherapy into the less effective ANT-based regimens.2-5 In the modern chemotherapy era, radiotherapy remained an essential component of first-line therapy for early-stage ENKTCL,24-27 even after a complete response to ASP-based regimens.27 Here, we further demonstrated that non–ANT-based chemotherapy (mostly with radiotherapy) significantly improved survival outcomes for stage I–II patients. The 5-year OS rate was 73.3% in this study, comparable to the recent large multicenter studies from Japan (72%)29 and Asian joint data (∼74% to 79%),30 but higher than the International T-cell Project registry data (median OS, 59 months),31 probably because of more heterogeneous treatments in the latter study. Interestingly, survival outcomes in these large series were similar to that of prospective phase 1/2 trials (3-year OS, 66%-87.5%; 5-year OS, 60%-82.1%) and retrospective studies (∼75%; Table 3).7-10,12-14,26,29-40 Furthermore, the survival benefits of non–ANT-based regimens in this study were prominent in early-stage patients who underwent CMT vs chemotherapy only. In our previous study,24 non–ANT-based regimens and radiotherapy were associated with higher conditional survival and lower annual failure hazard in early-stage patients. Consistent with the International T-cell Project registry study,31 even with more effective non–ANT-based regimens, chemotherapy alone still resulted in inferior outcomes in early-stage patients, with both 5-year OS and PFS rates of only 50.1% and 39.7% in the present CLCG study. In our previous study, up to 46.9% of early-stage patients who achieved a complete response with ASP-based chemotherapy developed disease relapse.27 The current study also demonstrated that radiotherapy followed by chemotherapy provided survival benefit over chemotherapy followed by radiotherapy for early-stage ENKTCL in the CMT setting with ANT-based or non–ANT-based regimens. These results emphasize the important role of radiotherapy for early-stage patients in the modern chemotherapy era. On the other hand, patients with advanced-stage disease had extremely poor prognoses after non–ANT-based regimen chemotherapy (Table 3), with a median OS of 5.4 to 36.6 months and a 5-year OS of <40% in these prospective and retrospective studies.29,31,41-46 Furthermore, the risk of death or progression is variable due to the interactions between clinical stages and treatments in patients with relapsed/refractory ENKTCL.7,15,16,47-49 As indicated in Table 3, the favorable outcomes of non–ANT-based regimen chemotherapy (5-year OS, 55%-66.9%) reported in these patients are partly attributable to the inclusion of those with localized-relapsed/refractory7,15,16,47-49 or newly diagnosed early-stage ENKTCL21,29,31,50-52 treated with effective radiotherapy. These findings support further consideration of more effective systematic therapy or innovative treatment strategy for patients with advanced-stage or disseminated diseases and the use of risk-adapted therapy involving radiotherapy and better-tolerated non–ANT-based chemotherapy for patients with early-stage or localized diseases.
Table 3.
Treatment outcomes of non–ANT-based or ASP-based chemotherapy with or without radiotherapy in patients with ENKTCL
| Author | Total no. | Eligibility and stage | Study type | Chemotherapy regimen | RT no. (%) | OS % (y) | PFS % (y) |
|---|---|---|---|---|---|---|---|
| Early stage (newly diagnosed, n ≥ 30) | |||||||
| Yamaguchi et al7,8 | 33 | Newly, I: 22, II: 11 | Phase 1/2 | Concurrent DeVIC/RT | 33 (100) | 73 (5) | 67 (5) |
| Kim et al9 | 30 | Newly, I: 15, II: 15 | Phase 2 | Concurrent VIDP/RT | 30 (100) | 86.3 (3) | 85.2 (3) |
| Ke et al32 | 32 | Newly, I: 17, II: 15 | Phase 2 | Concurrent GDP/RT | 32 (100) | 87.5 (3) | 84.4 (3) |
| Kim et al12 | 30 | Newly, I: 21, II: 9 | Phase 2 | Concurrent VIDL/RT | 30 (100) | 60 (5) | 73 (5) |
| Kim et al13 | 44 | Newly, stage I-II | Phase 2 | Sequential IMEP/RT | 44 (100) | 66 (3) | 65 (3) |
| Tsai et al10 | 33 | Newly, I: 21, II: 12 | Phase 2 | Concurrent VIDP/RT | 33 (100) | 66 (5) | 60 (5) |
| Xu et al33 | 40 | Newly, stage I-II | Phase 2 | Sequential MESA/RT | 36 (90) | 92 (2) | 89.1 (2) |
| Qi et al14 | 40 | Newly, I: 27, II: 13, high-risk | Phase 2 | Sequential RT/GDP | 40 (100) | 82.1 (5) | 79.4 (5) |
| Oh et al34 | 62 | Newly, I: 46, II: 16 | Retrospective | Concurrent VIDP/MIDLE/RT | 13 (100) | 83.1 (3) | 77.1 (3) |
| Wang et al35 | 93 | Newly, stage I-II | Retrospective | Sequential GELOX/RT | 40 (100) | 78.9 (5) | 79 (5) |
| Sequential EPOCH/RT | 53 (100) | 50.4 (5) | 46.5 (5) | ||||
| Zang et al36 | 64 | Newly, I: 53, II: 11 | Retrospective | Sequential CHOP-L/SMILE/RT | Early (100) | 84.2 (3) | 74.3 (3) |
| Late (100) | 57.6 (3) | 55.9 (3) | |||||
| Tian et al37 | 72 | Newly, I: 54, II: 18 | Retrospective | Sequential GDP/RT | 72 (100) | 72 (5) | NR |
| Qi et al26 | 75 | Newly, I: 44, II: 31 | Retrospective | Sequential RT/GDP | 75 (100) | 79.4 (5) | NR |
| Hu et al38 | 94 | Newly, I: 19, II: 75 | Retrospective | Sequential LVD/RT | 94 (100) | 74.3 (5) | NR |
| Wei et al39 | 71 | Newly, stage I-II | Retrospective | Sequential EPOCHL/RT | 68 (96) | 65.3 (5) | NR |
| Kim et al21 | 344 | Newly, I: 228, II: 11, training cohort | Large multicenter | Non-ANT-based ± RT | NR | 75 (3) | 63 (3) |
| Li et al40 | 167 | Newly, stage I-II | Large multicenter | Sequential GELOXD/P-GEMOXD±RT | 142 (85) | 73 (3) | 72.8 (3) |
| Yamaguchi et al29 | 257 | Newly, stage I-II | Large multicenter | Concurrent DeVIC/RT: 150 | 150 (100) | 72 (5) | 61 (5) |
| Kwong et al30 | 244 | Newly, I: 170, II: 74 | Large multicenter | Concurrent non-ANT/RT Sequential non-ANT/RT | 54 (100) | 79.8 (5)* | 68.5 (5)* |
| 190 (100) | 74.4 (5)* | 52.2 (5)* | |||||
| Fox et al31 | 104 | Newly, I: 74, II: 30 | Large multicenter | Sequential non-ANT (62%) ±RT | 48/59 (81) | 59 m† | 46 m† |
| Present study | 1156 | Newly, I: 1438, II: 788 | Large multicenter | Sequential non-ANT ±RT | 977 (85) | 73.3 (5) | 64.0 (5) |
| Advanced stage (newly, relapsed or refractory) | |||||||
| Kim et al41 | 27 | Newly, IV: 27 | Phase 2 | SMILE (HSCT: 11) | 0 | 10.6 m† | 5.1 m† |
| Wang et al42 | 18 | Newly, III: 3, IV: 15 | Phase 2 | LVDP | 18 (100) | 23.0 m† | 10.5 m† |
| Ji et al43 | 21 | Newly, II: 1, III-IV: 20 | Retrospective | GLIDE (HSCT: 4) | 0 | 56 (3) | 35.8 (3) |
| Bi et al44 | 73 | Newly, III: 11, IV: 62 | Retrospective | L-ASP-based: 23 | 17 (27) | 38.3 (2) | 25.4 (2) |
| L-ASP absent: 46 | 22.7 (2) | 14.9 (2) | |||||
| Ding et al45 | 13 | R/R, III: 8, IV: 5 | Retrospective | MEDA | 8 (62) | 69.2 (1) | 61.5 (1) |
| Kim et al46 | 70 | Newly, III: 4, IV: 66 | Multicenter | L-IMEP: 22 | 0 | 36.6 m† | 10.1 m† |
| IMEP: 48 | 5.4 m† | 3.2 m† | |||||
| Yamaguchi et al29 | 101 | Newly, stage III-IV | Large multicenter | ASP based (70%) | 69 (68) | 24 (5) | NR |
| Fox et al31 | 49 | Newly, stage III-IV | Large multicenter | Non–ANT based | NR | 19 m† | 15 m† |
| Present study | 195 | Newly, III: 48, IV: 147 | Large multicenter | Non–ANT based | 74 (38) | 39.8 (5) | 30.1 (5) |
| Early and advanced stage (newly, relapsed or refractory) | |||||||
| Yamaguchi et al7 | 38 | R/R or newly, I-II: 11, III-IV: 27 | Phase 2 | SMILE (HSCT: 21) | NR | 55 (1) | 53 (1) |
| Jaccard et al15 | 19 | R/R, I-II: 12, III-IV: 7 | Phase 2 | AspaMetDex (ASCT: 5) | 1 (5) | 12.2 m† | 12.2 m† |
| Kwong et al16 | 87 | R/R 44, Newly, 43. I-II: 38, III-IV: 49 | Phase 2 | SMILE (HSCT: 24) | 19 (22) | 50 (5) | 64 (4) |
| Yong et al47 | 18 | Refractory, I-II2: 7, III-IV: 11 | Retrospective | L-ASP based | 18 (100) | 55.6 (5) | NR |
| Yong et al48 | 45 | R/R, I-II: 33, III-IV: 12 | Retrospective | LVD | 41 (91) | 66.9 (5) | NR |
| Zhou et al49 | 17 | R/R, I-II: 8, III-IV: 9 | Retrospective | DDGP | 4 (24) | 82.4 (1) | 64.7 (1) |
| Lin et al50 | 38 | Newly, I-II: 31, III-IV: 7 | Phase 2 | CHOP-L | 31 (82) | 80.1 (2) | 81 (2) |
| Guo et al51 | 55 | Newly, I-II: 45, III-IV: 10 | Retrospective | GOLD | 45 (82) | 74 (3) | 57 (3) |
| Wang et al52 | 98 | Newly, I-II: 77, III-IV: 21 | Retrospective | GELOX, P-Gemox | 77 (79) | 65.2 (3) | 57.0 (3) |
| Kim et al21 | 527 | Newly, I-II: 344, III-IV: 183 | Large multicenter | Non–ANT based (HSCT: 49) | 325 (62) | 59 (3) | 48 (3) |
| Yahaguchi et al29 | 358 | Newly, I-II: 257, III-IV: 101 | Large multicenter | Non–ANT based | 278 (78) | 56 (5) | 45 (5) |
| Fox et al31 | 166 | Newly, I-II: 104, III-IV: 49 | Large multicenter | Non–ANT based | 87/130 (67) | 59 m† | 20† |
| Present study | 1351 | Newly, I-II: 1156, III-IV: 195 | Large multicenter | Non–ANT based | 1051 (78) | 68.9 (5) | 59.5 (5) |
Estimated from the figures.
Median survival time (months).
ASCT, allogeneic stem cell transplant; AspaMetDex, l-ASP, methotrexate, and dexamethasone; CHOP-L, cyclophosphamide, doxorubicin, vincristine, prednisolone, and l-ASP; CT, chemotherapy; DDGP, GEM, pegaspargase, cisplatin, and dexamethasone; DeVIC, carboplatin, etoposide, ifosfamide, and dexamethasone; EPOCH, etoposide, vincristine, cyclophosphamide, doxorubicin, and prednisone; ESHAP, etoposide, steroid, high-dose Ara-C, and platinum; GDP, GEM, dexamethasone, and cisplatin; GELOX, GEM, oxaliplatin, and l-ASP; GLIDE, GEM, l-ASP, ifosfamide, dexamethasone, and etoposide; GOLD, GEM oxaliplatin, l-ASP, and dexamethasone; HSCT, hematopoietic stem cell transplant; IMEP, ifosfamide, methotrexate, etoposide, and prednisolone; L-ASP, l-ASP; L-IMEP, l-ASP, ifosfamide, methotrexate, etoposide, and prednisolone; LVD, l-ASP, vincristine, and dexamethasone; LVDP, l-ASP, etoposide, dexamethasone, and cisplatin; LVP, l-ASP, vincristine, and prednisolone; MEDA/MESA, methotrexate, etoposide, dexamethasone, and pegaspargase; MIDLE, methotrexate, etoposide, ifosfamide, mesna, and l-ASP; NR, not reported; P-Gemox, pegaspargase, GEM, and oxaliplatin; R/R, relapsed/refractory; RT, radiotherapy; SMILE, dexamethasone, methotrexate, ifosfamide, l-ASP, and etoposide; VIDL, etoposide, ifosfamide, cisplatin, and l-ASP; VIDP, etoposide, ifosfamide, cisplatin, and dexamethasone.
The rarity of the disease and lack of randomized controlled trial data have resulted in a variety of non–ANT-based regimens for ENKTCL being developed and recommended by guidelines and adopted in clinical practice among the CLCG institutions. Although treatment options and non–ANT-based regimens varied across countries and even within institutions, consistent with other studies,29-31 ASP-based regimens have formed the mainstay of chemotherapy across China over the past decade. The wide utility of ASP-based regimens in the world indicated its feasibility in clinical practice and prompted their further validation and optimization. Interestingly, the addition of ASP to CHOP was associated with significantly improved survival compared with CHOP, indicating the important role of ASP in ENKTCL. However, only a small proportion of patients received first-line ASP/methotrexate–based regimens such as SMILE (l-ASP, ifosfamide, methotrexate, etoposide, and dexamethasone) in this study, probably because of its highly severe toxicities.7,15,16 The heterogeneity of ASP-based regimens reflects the evolving practice pattern of chemotherapy regimens, associated with a lack of a general consensus on the standard regimens for ENKTCL. Further work is needed to determine the optimal non–ANT-based regimens.
This retrospective study had several limitations. First, the chemotherapy regimens were not randomly assigned; therefore, the results may be affected by selection bias. However, given the recognition of ENKTCL resistant to ANT-based regimens, a further prospective study designed as a direct randomized comparison of ANT-based and non–ANT-based regimens may raise ethical concerns. Second, non–ANT-based regimens were applied in more recent years, accompanied with more accurate imaging such as PET/CT or magnetic resonance imaging and advanced radiotherapy techniques.28 As PET/CT scan was routinely used for staging of patients after 2010, the majority of patients recruited from 2000 to 2009 were therefore not staged properly according to the current standard. This would result in misleading conclusion on the effect of disease stage. We attempted to circumvent these limitations using PSM and multivariable analyses involving time period (2000-2004 vs 2005-2009 vs 2010-2015) and prognostic variables. However, even with PSM analysis, there remains a chance that the underlying confounding factors may have influenced the results. Some other factors, such as treatment toxicity and patient or physician preference, were not completely evaluated. Third, we only focused on effectiveness; however, the toxicity profiles of non–ANT-based regimens could be considered when dealing with different-stage patients or elderly patients. Finally, histologic results were not centrally reviewed in the CLCG; this may lead to misdiagnosis in few cases. However, with distinctive clinicopathological and immunophenotypic findings defined in the World Health Organization classification, ENKTCL is easily distinguished from other cytotoxic T-cell lymphomas.53 We believe this is not likely to significantly affect our conclusions.
In summary, we demonstrated that non–ANT-based regimens significantly improved survival compared with ANT-based regimens, regardless of stage, risk subgroup, or radiotherapy. These findings provide additional evidence supporting non–ANT-based regimens as first-line treatments for ENKTCL.
Supplementary Material
The full-text version of this article contains a data supplement.
Acknowledgments
The authors thank Ying Huang (Center of Cancer Research, National Cancer Institute, Bethesda, MD) for her critical review of the manuscript.
This work was supported by grants from the Chinese Academy of Medical Science Innovation Fund for Medical Sciences (CIFMS; 2016-I2M-1-001), the National Key Projects of Research and Development of China (2016YFC0904600), Capital’s Funds for Health Improvement and Research (grant 2018-1-2151), and the National Natural Science Foundation of China (grants 81670185 and 81870154).
Footnotes
Portions of our work were presented orally at the 15th International Conference on Malignant Lymphoma, Lugano, Switzerland, 20 June 2019.
For data sharing, contact Ye-Xiong Li (e-mail: yexiong@yahoo.com or yexiong12@163.com).
Authorship
Contribution: S.-N.Q., Y.Y., Y.-Q.S., J.Z., and Y.-X.L. designed the study, analyzed the data, and wrote the manuscript; S.-N.Q., Y.Y., Y.-Q.S., C.H., J.Z., and Y.-X.L. contributed to the study concept; Y.-X.L., J.Z., Y.-Q.S., S.-N.Q., and Y.Y. contributed to the study coordination; S.-N.Q., Y.Y., C.H., and Y.-X.L. performed the statistical analysis; and all authors contributed to data collection and interpretation, and finally approved the manuscript.
Conflict-of-interest disclosure: C.H. has received grants from the National Institutes of Health/National Cancer Institute and personal fees from Varian Medical Systems outside the submitted work. The remaining authors declare no competing financial interests. A complete list of the members of the China Lymphoma Collaborative Group appears in “Appendix.”
Correspondence: Ye-Xiong Li, State Key Laboratory of Molecular Oncology, Department of Radiation Oncology, National Cancer Center/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, PanJiaYuan NanLi #17, ChaoYang District, Beijing 100021, People’s Republic of China; e-mail: yexiong12@163.com or yexiong@yahoo.com; and Jun Zhu, Key Laboratory of Carcinogenesis and Translational Research, Ministry of Education, Peking University Cancer Hospital & Institute, FuCheng Rd #52, HaiDian District, Beijing 100142, People’s Republic of China, e-mail: zhu-jun2017@outlook.com.
Appendix
The members of the China Lymphoma Collaborative Group are: Y.-J.Z., Y.-X.L., J.Z., T.W., J.-Z.C., Y.Z., X.-Y.Q., M.S., H.S., Y.W., S.-Y.Z., Z.-Y.Y., X.H., G.W., H.W., B.-L.Q., J.-X.W., F.-Q.Z., L.-T.Q., and G.-F.L.
References
- 1.Vose J, Armitage J, Weisenburger D; International T-Cell Lymphoma Project . International peripheral T-cell and natural killer/T-cell lymphoma study: pathology findings and clinical outcomes. J Clin Oncol. 2008;26(25):4124-4130. [DOI] [PubMed] [Google Scholar]
- 2.Vargo JA, Patel A, Glaser SM, et al. The impact of the omission or inadequate dosing of radiotherapy in extranodal natural killer T-cell lymphoma, nasal type, in the United States. Cancer. 2017;123(16):3176-3185. [DOI] [PubMed] [Google Scholar]
- 3.Yang Y, Zhang YJ, Zhu Y, et al. Prognostic nomogram for overall survival in previously untreated patients with extranodal NK/T-cell lymphoma, nasal-type: a multicenter study. Leukemia. 2015;29(7):1571-1577. [DOI] [PubMed] [Google Scholar]
- 4.Li YX, Yao B, Jin J, et al. Radiotherapy as primary treatment for stage IE and IIE nasal natural killer/T-cell lymphoma. J Clin Oncol. 2006;24(1):181-189. [DOI] [PubMed] [Google Scholar]
- 5.Yang Y, Zhu Y, Cao JZ, et al. Risk-adapted therapy for early-stage extranodal nasal-type NK/T-cell lymphoma: analysis from a multicenter study. Blood. 2015;126(12):1424-1432, quiz 1517. [DOI] [PubMed] [Google Scholar]
- 6.Yang Y, Cao JZ, Lan SM, et al. Association of improved locoregional control with prolonged survival in early-stage extranodal nasal-type natural killer/T-cell lymphoma. JAMA Oncol. 2017;3(1):83-91. [DOI] [PubMed] [Google Scholar]
- 7.Yamaguchi M, Kwong YL, Kim WS, et al. Phase II study of SMILE chemotherapy for newly diagnosed stage IV, relapsed, or refractory extranodal natural killer (NK)/T-cell lymphoma, nasal type: the NK-Cell Tumor Study Group study. J Clin Oncol. 2011;29(33):4410-4416. [DOI] [PubMed] [Google Scholar]
- 8.Yamaguchi M, Tobinai K, Oguchi M, et al. Concurrent chemoradiotherapy for localized nasal natural killer/T-cell lymphoma: an updated analysis of the Japan clinical oncology group study JCOG0211. J Clin Oncol. 2012;30(32):4044-4046. [DOI] [PubMed] [Google Scholar]
- 9.Kim SJ, Kim K, Kim BS, et al. Phase II trial of concurrent radiation and weekly cisplatin followed by VIPD chemotherapy in newly diagnosed, stage IE to IIE, nasal, extranodal NK/T-Cell Lymphoma: Consortium for Improving Survival of Lymphoma study. J Clin Oncol. 2009;27(35):6027-6032. [DOI] [PubMed] [Google Scholar]
- 10.Tsai HJ, Lin SF, Chen CC, et al. Long-term results of a phase II trial with frontline concurrent chemoradiotherapy followed by consolidation chemotherapy for localized nasal natural killer/T-cell lymphoma. Eur J Haematol. 2015;94(2):130-137. [DOI] [PubMed] [Google Scholar]
- 11.Wang L, Wang ZH, Chen XQ, et al. First-line combination of gemcitabine, oxaliplatin, and L-asparaginase (GELOX) followed by involved-field radiation therapy for patients with stage IE/IIE extranodal natural killer/T-cell lymphoma. Cancer. 2013;119(2):348-355. [DOI] [PubMed] [Google Scholar]
- 12.Kim SJ, Yang DH, Kim JS, et al. Concurrent chemoradiotherapy followed by L-asparaginase-containing chemotherapy, VIDL, for localized nasal extranodal NK/T cell lymphoma: CISL08-01 phase II study. Ann Hematol. 2014;93(11):1895-1901. [DOI] [PubMed] [Google Scholar]
- 13.Kim TM, Kim DW, Kang YK, et al. A phase II study of ifosfamide, methotrexate, etoposide, and prednisolone for previously untreated stage I/II extranodal natural killer/T-cell lymphoma, nasal type: a multicenter trial of the Korean Cancer Study Group. Oncologist. 2014;19(11):1129-1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Qi F, Wang WH, He XH, et al. Phase 2 study of first-line intensity modulated radiation therapy followed by gemcitabine, dexamethasone, and cisplatin for high-risk, early stage extranodal nasal-type NK/T-cell lymphoma: the GREEN study. Int J Radiat Oncol Biol Phys. 2018;102(1):61-70. [DOI] [PubMed] [Google Scholar]
- 15.Jaccard A, Gachard N, Marin B, et al. ; GELA and GOELAMS Intergroup . Efficacy of L-asparaginase with methotrexate and dexamethasone (AspaMetDex regimen) in patients with refractory or relapsing extranodal NK/T-cell lymphoma, a phase 2 study. Blood. 2011;117(6):1834-1839. [DOI] [PubMed] [Google Scholar]
- 16.Kwong YL, Kim WS, Lim ST, et al. SMILE for natural killer/T-cell lymphoma: analysis of safety and efficacy from the Asia Lymphoma Study Group. Blood. 2012;120(15):2973-2980. [DOI] [PubMed] [Google Scholar]
- 17.Wang L, Wang WD, Xia ZJ, Zhang YJ, Xiang J, Lu Y. Combination of gemcitabine, L-asparaginase, and oxaliplatin (GELOX) is superior to EPOCH or CHOP in the treatment of patients with stage IE/IIE extranodal natural killer/T cell lymphoma: a retrospective study in a cohort of 227 patients with long-term follow-up. Med Oncol. 2014;31(3):860. [DOI] [PubMed] [Google Scholar]
- 18.Qi SN, Xu LM, Yuan ZY, et al. Effect of primary tumor invasion on treatment and survival in extranodal nasal-type NK/T-cell lymphoma in the modern chemotherapy era: a multicenter study from the China Lymphoma Collaborative Group (CLCG). Leuk Lymphoma. 2019;60(11):2669-2678. [DOI] [PubMed] [Google Scholar]
- 19.Chen SY, Yang Y, Qi SN, et al. Validation of nomogram-revised risk index and comparison with other models for extranodal nasal-type NK/T-cell lymphoma in the modern chemotherapy era: indication for prognostication and clinical decision-making. Leukemia. 2020; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee J, Suh C, Park YH, et al. Extranodal natural killer T-cell lymphoma, nasal-type: a prognostic model from a retrospective multicenter study. J Clin Oncol. 2006;24(4):612-618. [DOI] [PubMed] [Google Scholar]
- 21.Kim SJ, Yoon DH, Jaccard A, et al. A prognostic index for natural killer cell lymphoma after non-anthracycline-based treatment: a multicentre, retrospective analysis. Lancet Oncol. 2016;17(3):389-400. [DOI] [PubMed] [Google Scholar]
- 22.Pokrovsky VS, Vinnikov D. L-Asparaginase for newly diagnosed extra-nodal NK/T-cell lymphoma: systematic review and meta-analysis. Expert Rev Anticancer Ther. 2017;17(8):759-768. [DOI] [PubMed] [Google Scholar]
- 23.Pokrovsky VS, Vinnikov D. Defining the toxicity of current regimens for extranodal NK/T cell lymphoma: a systematic review and metaproportion. Expert Rev Anticancer Ther. 2019;19(1):93-104. [DOI] [PubMed] [Google Scholar]
- 24.Liu X, Wu T, Zhu SY, et al. Risk-dependent conditional survival and failure hazard after radiotherapy for early-stage extranodal natural killer/T-cell lymphoma. JAMA Netw Open. 2019;2(3):e190194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu WX, Shi M, Su H, et al. Effect of age as a continuous variable on survival outcomes and treatment selection in patients with extranodal nasal-type NK/T-cell lymphoma from the China Lymphoma Collaborative Group (CLCG). Aging (Albany NY). 2019;11(19):8463-8473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Qi F, Chen B, Wang J, et al. Upfront radiation is essential for high-risk early-stage extranodal NK/T-cell lymphoma, nasal type: comparison of two sequential treatment modalities combining radiotherapy and GDP (gemcitabine, dexamethasone, and cisplatin) in the modern era. Leuk Lymphoma. 2019;60(11):2679-2688. [DOI] [PubMed] [Google Scholar]
- 27.Deng XW, Wu JX, Wu T, et al. Radiotherapy is essential after complete response to asparaginase-containing chemotherapy in early-stage extranodal nasal-type NK/T-cell lymphoma: a multicenter study from the China Lymphoma Collaborative Group (CLCG). Radiother Oncol. 2018;129(1):3-9. [DOI] [PubMed] [Google Scholar]
- 28.Wu T, Yang Y, Zhu SY, et al. Risk-adapted survival benefit of IMRT in early-stage NKTCL: a multicenter study from the China Lymphoma Collaborative Group. Blood Adv. 2018;2(18):2369-2377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yamaguchi M, Suzuki R, Oguchi M, et al. Treatments and outcomes of patients with extranodal natural killer/T-cell lymphoma diagnosed between 2000 and 2013: a cooperative study in Japan. J Clin Oncol. 2017;35(1):32-39. [DOI] [PubMed] [Google Scholar]
- 30.Kwong YL, Kim SJ, Tse E, et al. Sequential chemotherapy/radiotherapy was comparable with concurrent chemoradiotherapy for stage I/II NK/T-cell lymphoma. Ann Oncol. 2018;29(1):256-263. [DOI] [PubMed] [Google Scholar]
- 31.Fox CP, Civallero M, Ko YH, et al. Survival outcomes of patients with extranodal natural-killer T-cell lymphoma: a prospective cohort study from the international T-cell project. Lancet Haematol. 2020;7(4):e284-e294. [DOI] [PubMed] [Google Scholar]
- 32.Ke QH, Zhou SQ, Du W, Liang G, Lei Y, Luo F. Concurrent IMRT and weekly cisplatin followed by GDP chemotherapy in newly diagnosed, stage IE to IIE, nasal, extranodal NK/T-Cell lymphoma. Blood Cancer J. 2014;4(12):e267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xu PP, Xiong J, Cheng S, et al. A phase II study of methotrexate, etoposide, dexamethasone and pegaspargase sandwiched with radiotherapy in the treatment of newly diagnosed, stage IE to IIE extranodal natural-killer/T-cell lymphoma, nasal-type. EBioMedicine. 2017;25:41-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Oh D, Ahn YC, Kim SJ, Kim WS, Ko YH. Concurrent chemoradiation therapy followed by consolidation chemotherapy for localized extranodal natural killer/T-cell lymphoma, nasal type. Int J Radiat Oncol Biol Phys. 2015;93(3):677-683. [DOI] [PubMed] [Google Scholar]
- 35.Wang H, Wuxiao ZJ, Zhu J, et al. Comparison of gemcitabine, oxaliplatin and L-asparaginase and etoposide, vincristine, doxorubicin, cyclophosphamide and prednisone as first-line chemotherapy in patients with stage IE to IIE extranodal natural killer/T-cell lymphoma: a multicenter retrospective study. Leuk Lymphoma. 2015;56(4):971-977. [DOI] [PubMed] [Google Scholar]
- 36.Zang J, Li C, Luo SQ, et al. Early radiotherapy has an essential role for improving survival in patients with stage I-II nasal-type of NK/T cell lymphoma treated with L-asparaginase-containing chemotherapy–a single institution experience. Ann Hematol. 2015;94(4):583-591. [DOI] [PubMed] [Google Scholar]
- 37.Tian S, Li R, Wang T, et al. Gemcitabine, dexamethasone, and cisplatin (GDP) chemotherapy with sandwiched radiotherapy in the treatment of newly diagnosed stage IE/IIE extranodal natural killer/T-cell lymphoma, nasal type. Cancer Med. 2019;8(7):3349-3358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hu Y, Chen M, Song Y, et al. Study of L-asparaginase, vincristine, and dexamethasone combined with intensity-modulated radiation therapy in early-stage nasal NK/T-cell Lymphoma. Am J Clin Oncol. 2020;43(4):257-262. [DOI] [PubMed] [Google Scholar]
- 39.Wei L, Wang J, Ye J, et al. Long-term outcomes of patients treated with an EPOCHL regimen as first-line chemotherapy for newly diagnosed extranodal natural killer/T-cell lymphoma: a retrospective single-center study. Leuk Lymphoma. 2020;61(2):337-343. [DOI] [PubMed] [Google Scholar]
- 40.Li JW, Li YJ, Zhong MZ, et al. Efficacy and tolerance of GELOXD/P-GEMOXD in newly diagnosed nasal-type extranodal NK/T-cell lymphoma: a multicenter retrospective study. Eur J Haematol. 2018;100(3):247-256. [DOI] [PubMed] [Google Scholar]
- 41.Kim SJ, Park S, Kang ES, et al. Induction treatment with SMILE and consolidation with autologous stem cell transplantation for newly diagnosed stage IV extranodal natural killer/T-cell lymphoma patients. Ann Hematol. 2015;94(1):71-78. [DOI] [PubMed] [Google Scholar]
- 42.Wang YQ, Yang Y, Zhuo HY, Zou LQ, Jiang Y, Jiang M. Trial of LVDP regimen (L-asparaginase, etoposide, dexamethasone, and cisplatin, followed by radiotherapy) as first-line treatment for newly diagnosed, stage III/IV extranodal natural killer/T cell lymphoma. Med Oncol. 2015;32(2):435. [DOI] [PubMed] [Google Scholar]
- 43.Ji J, Liu T, Xiang B, et al. A study of gemcitabine, l-asparaginase, ifosfamide, dexamethasone and etoposide chemotherapy for newly diagnosed stage IV, relapsed or refractory extranodal natural killer/T-cell lymphoma, nasal type. Leuk Lymphoma. 2014;55(12):2955-2957. [DOI] [PubMed] [Google Scholar]
- 44.Bi XW, Jiang WQ, Zhang WW, et al. Treatment outcome of patients with advanced stage natural killer/T-cell lymphoma: elucidating the effects of asparaginase and postchemotherapeutic radiotherapy. Ann Hematol. 2015;94(7):1175-1184. [DOI] [PubMed] [Google Scholar]
- 45.Ding H, Chang J, Liu LG, et al. High-dose methotrexate, etoposide, dexamethasone and pegaspargase (MEDA) combination chemotherapy is effective for advanced and relapsed/refractory extranodal natural killer/T cell lymphoma: a retrospective study. Int J Hematol. 2015;102(2):181-187. [DOI] [PubMed] [Google Scholar]
- 46.Kim M, Kim TM, Kim KH, et al. Ifosfamide, methotrexate, etoposide, and prednisolone (IMEP) plus L-asparaginase as a first-line therapy improves outcomes in stage III/IV NK/T cell-lymphoma, nasal type (NTCL). Ann Hematol. 2015;94(3):437-444. [DOI] [PubMed] [Google Scholar]
- 47.Yong W, Zheng W, Zhang Y, et al. L-asparaginase-based regimen in the treatment of refractory midline nasal/nasal-type T/NK-cell lymphoma. Int J Hematol. 2003;78(2):163-167. [DOI] [PubMed] [Google Scholar]
- 48.Yong W, Zheng W, Zhu J, et al. L-asparaginase in the treatment of refractory and relapsed extranodal NK/T-cell lymphoma, nasal type. Ann Hematol. 2009;88(7):647-652. [DOI] [PubMed] [Google Scholar]
- 49.Zhou Z, Li X, Chen C, et al. Effectiveness of gemcitabine, pegaspargase, cisplatin, and dexamethasone (DDGP) combination chemotherapy in the treatment of relapsed/refractory extranodal NK/T cell lymphoma: a retrospective study of 17 patients. Ann Hematol. 2014;93(11):1889-1894. [DOI] [PubMed] [Google Scholar]
- 50.Lin N, Song Y, Zheng W, et al. A prospective phase II study of L-asparaginase- CHOP plus radiation in newly diagnosed extranodal NK/T-cell lymphoma, nasal type. J Hematol Oncol. 2013;6(1):44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Guo HQ, Liu L, Wang XF, et al. Efficacy of gemcitabine combined with oxaliplatin, L-asparaginase and dexamethasone in patients with newly-diagnosed extranodal NK/T-cell lymphoma. Mol Clin Oncol. 2014;2(6):1172-1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wang H, Wang L, Wuxiao Z, et al. Increased serum levels of interleukin-10 predict poor prognosis in extranodal natural killer/T-cell lymphoma patients receiving asparaginase-based chemotherapy. OncoTargets Ther. 2015;8:2589-2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ko YH, Cho EY, Kim JE, et al. NK and NK-like T-cell lymphoma in extranasal sites: a comparative clinicopathological study according to site and EBV status. Histopathology. 2004;44(5):480-489. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.