Abstract
Background
To investigate the 3-month postoperative performance and safety after implantation of a trifocal intraocular lens (IOL) in a Korean population.
Methods
This was a clinical, prospective, multicenter, single-arm study. Forty-four subjects (88 eyes) with bilateral cataract with expected postoperative corneal astigmatism of < 1.00 diopter (D) and no ocular disease or eye condition underwent bilateral implantation of the AcrySof IQ® PanOptix IOL (TFNT00). Postoperative examination at 3 months included binocular defocus curve; binocular best corrected distance visual acuity (BCDVA); monocular/binocular uncorrected VA (UCVA) at distance (4 m), intermediate (60 cm), and near (40 cm); contrast sensitivity under photopic conditions with/without glare; and subjective outcomes, including satisfaction and spectacle independence.
Results
Binocular defocus curve at 3 months after bilateral implantation showed VA of 0.1 logMAR or better from + 0.5 D through − 2.5 D. Binocular BCDVA mean ± SD at 4 m was − 0.05 ± 0.07 logMAR. Binocular and monocular UCVA was 0.03 ± 0.1 and 0.08 ± 0.12 logMAR (4 m), − 0.00 ± 0.11 and 0.05 ± 0.13 logMAR (60 cm), and 0.03 ± 0.12 and 0.09 ± 0.13 logMAR (40 cm), respectively. Contrast sensitivity with glare was 1.67 ± 0.13, 1.91 ± 0.17, 1.54 ± 0.21, and 1.14 ± 0.20 log units at 3, 6, 12, and 18 cycles/degree, respectively. At near and intermediate distances, 84 and 77% of subjects reported good/excellent satisfaction, and 84 and 91% of subjects reported spectacle independence, respectively.
Conclusions
In a Korean population, visual performance of the trifocal TFNT00 IOL 3 months postoperatively was < 0.1 logMAR for binocular UCVA at all distances, with high subject satisfaction and spectacle independence.
Trial registration
www.ClinicalTrials.gov (NCT03268746). Registered August 31, 2017.
Keywords: Intraocular lens, Satisfaction, Spectacle independence, Trifocal, Visual acuity
Background
Many subjects who receive monofocal intraocular lenses (IOLs) ultimately require corrective glasses after cataract surgery to improve their intermediate or near distance vision [1]. Most multifocal IOLs can produce 2 foci for distance and near vision, providing a more complete range of vision compared with monofocal IOLs [2, 3]; however, glasses may be needed for intermediate vision [3, 4]. Because many daily activities, such as viewing computer or smartphone screens, are performed at intermediate distances [5, 6], trifocal IOLs with 3 focal points have been developed to address the need for improved intermediate vision after cataract surgery [7].
The first generation of trifocal IOLs, including AT LISA® tri 839MP (Carl Zeiss Meditec, Jena, Germany) and FineVision® Micro F (PhysIOL, Liège, Belgium), has an intermediate focal point at 80 cm [8, 9]. However, for many people, the optimal distance for daily intermediate vision tasks is at arm’s length, approximately 60 to 70 cm for populations of average height [6, 10]. The AcrySof® IQ PanOptix® IOL model TFNT00 (Alcon Vision LLC, Fort Worth, TX, USA) has near and distance focal points similar to a conventional multifocal IOL and an intermediate focal point at 60 cm [11, 12]. In an optical bench study, TFNT00 provided better image quality at intermediate distance compared with either AT LISA tri 839MP or FineVision Micro F because of improved light utilization [13]. Clinical studies of TFNT00 have shown that subjects achieved visual acuity (VA) of 20/25 or better from near (40 cm) through intermediate distance (60 cm) 6 to 12 months after IOL implantation [14–16]. The results of these studies indicate that the 60-cm focal point may provide optimal intermediate vision compared with the 80-cm focal point of earlier-generation trifocal IOLs.
The popularity of cataract surgery and IOL implantation has increased in Korea over the past decade, and multifocal IOLs are the most frequently selected lenses [17]. The TFNT00 IOL may provide good VA at intermediate distance for Korean subjects, for whom average arm length is between 53 and 59 cm [18, 19]; however, no clinical studies have been conducted in this population.
The purpose of this study was to evaluate the safety and effectiveness of TFNT00 in a Korean population 3 months after implantation, including visual performance, quality of vision, and subject satisfaction of postoperative vision.
Methods
Intraocular Lens
The TFNT00 IOL is intended for implantation in the capsular bag to correct presbyopia after cataract surgery [12]. TFNT00 is a single-piece, ultraviolet-absorbing, and blue-light-filtering IOL with a 13.0-mm overall diameter and a 6.0-mm biconvex optic. The anterior surface of the IOL has 0.1-μm negative spherical aberration to compensate for the positive spherical aberration of an average cornea. The multifocal diffractive structure in the central 4.5-mm portion of the anterior surface of the optical zone divides incoming light to create + 2.17 diopter (D) (intermediate) and + 3.25 D (near) add powers. Cataract surgery was performed following surgeons’ routine procedures. Clear corneal incisions (1.8 to 2.75 mm) were made either on temporal or on steep axis. After phacoemulsification, implantation of the TFNT00 IOL was carried out according to the local guidelines and product information provided by Alcon Vision LLC [12].
Study design and population
This prospective, single-arm, unmasked, nonrandomized, multicenter study enrolled subjects aged > 20 years requiring bilateral cataract surgery. The study was conducted at 4 sites in Korea: Samsung Medical Center (n = 15), Asan Medical Center (n = 12), and Severance Hospital (n = 15) in Seoul and Seoul National University Bundang Hospital (n = 10) in Seongnam-si. Eligible subjects were those without ocular disease that could confound study outcomes who wanted an IOL that provided near, intermediate, and distance vision. Inclusion criteria were clear intraocular media other than cataract in both eyes, calculated lens power between + 16.0 D and + 24.0 D, and preoperative or expected postoperative regular corneal astigmatism of < 1.00 D. Exclusion criteria were clinically significant corneal abnormalities; previous corneal transplantation; ocular trauma; previous refractive surgery or refractive procedures throughout the study duration; history of concurrent retinal conditions; anterior chamber ≤2.5 mm not caused by swollen cataract; concurrent anterior or posterior segment inflammation; and expectation of ocular surgical treatment, large capsulotomy, or retinal laser treatment during the study (excluding neodymium-doped yttrium aluminum garnet [Nd:YAG] capsulotomy).
Study visits included a screening visit, an operative visit for each eye, and postoperative visits at week 1 and months 1 and 3. At the screening visit, the eye with worse best corrected distance VA (BCDVA) was selected as the first operative eye; if BCDVA was the same in both eyes, the right eye was selected as the first operative eye. Implantation of the IOL in the second eye occurred within 30 days of the first eye, and according to the standard visit schedule at each participating site.
Effectiveness endpoints
The primary endpoint was the binocular defocus curve measured 3 months after implantation. Best distance correction was varied from − 5.00 to + 2.00 D in steps of 0.50 D under photopic conditions (approximately 85 cd/m2), and VA was recorded at each refractive correction.
Secondary endpoints were the binocular defocus curve measured 1 month after implantation, VA at 1 and 3 months after implantation, contrast sensitivity 3 months after implantation, and responses to the subject satisfaction questionnaire at the preoperative visit and 3 months after implantation. BCDVA and mean monocular and binocular uncorrected distance VA (UCDVA, 4 m), uncorrected intermediate VA (UCIVA, 60 cm), and uncorrected near VA (UCNVA, 40 cm) were measured under photopic conditions with ambient lighting lower than chart luminance using CSV-1000 charts (distance) and Early Treatment Diabetic Retinopathy Study charts (distance, intermediate, and near). Photopic best corrected binocular contrast sensitivity was measured at 3, 6, 12, and 18 cycles per degree (cpd) using CSV-1000E charts at a distance of 2.45 m, without glare and with glare (approximately 2.5 cd/m2).
Subjects completed a 12-item questionnaire to determine satisfaction levels and spectacle independence. Other exploratory endpoints were photopic and mesopic pupil size 3 months after implantation, measured with a pupilometer to the nearest 0.5 mm at distance, and manifest refraction spherical equivalent (MRSE) at week 1, month 1, and month 3 after implantation, measured under photopic conditions at 2.45 m in steps of 0.25 D.
Safety analyses
Ocular nonserious and serious adverse events (AEs), including secondary surgical interventions related to the optical properties of the IOL, were assessed for ≤3 months after implantation and coded using the Medical Dictionary for Regulatory Activities Version 21.0. Additional safety endpoints included IOL tilt/decentration, intraocular pressure, surgical problems, and device deficiencies.
Statistical analyses
Binocular effectiveness was evaluated for all subjects with successful bilateral IOL implantation (full analysis set), monocular effectiveness was evaluated for all eyes with successful IOL implantation (all-implanted analysis set), and safety data were collected for all subjects with attempted IOL implantation (safety set).
Subject demographics were summarized using descriptive statistics. Effectiveness endpoints were evaluated using a 2-sided 90% CI of the mean for VA data (logarithm of the minimum angle of resolution [logMAR]). BCDVA and monocular/binocular UCDVA, UCIVA, and UCNVA were also summarized as categorical variables by visit as percentage of subjects with 20/20, 20/25, 20/32, or 20/40 vision or better. Subjective symptom questions were summarized by visit per question as total number of observations and counts and percentages in each category. AEs were summarized as counts and percentages of eyes with ocular AEs for first and second operative eyes.
Ethics
This clinical study was conducted under an approved Institutional Review Board protocol in accordance with the ethical principles of the Declaration of Helsinki, ISO14155:2011 Clinical Investigation of Medical Devices for Human Subjects – Good Clinical Practice, and Standards for Medical Devices for Good Clinical Practice. All subjects provided voluntary informed consent before initiation of any study procedures.
Results
Subject disposition
Of 52 enrolled subjects, 7 discontinued the study before IOL implantation because of screen failure. Most subjects (84%) were aged < 65 years and female (Table 1). Of the 45 subjects who received TFNT00, 1 subject withdrew from the study after the first eye implantation and did not receive an IOL in the second eye. The implanted eye was included in the all-implanted and safety analysis sets; the subject was excluded from the full analysis set.
Table 1.
Demographics and Baseline Characteristics (Full Analysis Set)
| Characteristic | TFNT00 (n = 44) |
|---|---|
| Age, mean (SD), y | 60 (8) |
| Sex, n (%) | |
| Female | 33 (75) |
| Race, n (%) | |
| Asian | 44 (100) |
| Height, mean (SD), cm | 159.9 (8.3) |
| Arm length, mean (SD), cm | 54.2 (6.3) |
| Axial length, mean (SD), mm | |
| First eye | 23.6 (0.67) |
| Second eye | 23.6 (0.67) |
| Corneal astigmatism, mean (SD), D | |
| First eye | 0.62 (0.32) |
| Second eye | 0.57 (0.25) |
| Monocular BCDVA, mean (SD), logMAR | |
| First eye | 0.26 (0.29) |
| Second eye | 0.10 (0.18) |
| MRSE, mean (SD), D | |
| First eye | 0.36 (1.48) |
| Second eye | 0.30 (1.57) |
BCDVA Best corrected distance visual acuity, D Diopter, logMAR Logarithm of the minimum angle of resolution, MRSE Manifest refraction spherical equivalent
Effectiveness
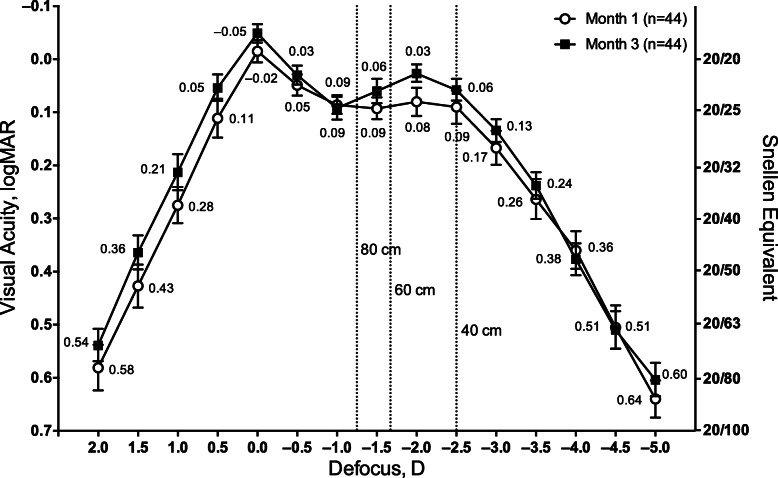
At month 3 after implantation, the binocular defocus curve showed mean VA of 0.1 logMAR (20/25 Snellen) or better between + 0.50 and − 2.50 D defocus (Fig. 1). Overall, the binocular defocus curve showed that TFNT00 provided functional VA across a full range of distances, with most refractive steps showing better VA at month 3 compared with month 1.
Fig. 1.
Binocular defocus curves 1 and 3 months after implantation of TFNT00. Error bars represent 90% CI. D = diopter; logMAR = logarithm of the minimum angle of resolution
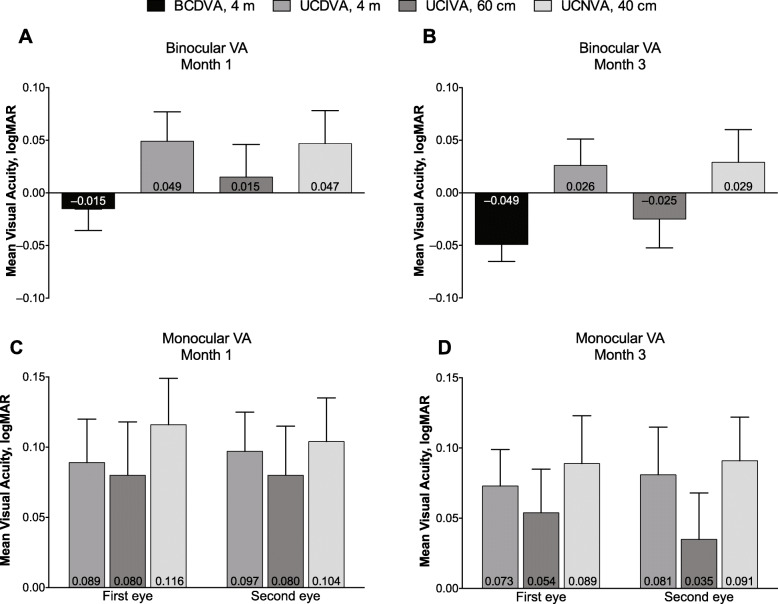
Binocular and monocular visual acuity are summarized in Table 2. Mean binocular BCDVA decreased from approximately 0.1 logMAR before implantation to 0.0 logMAR (20/20 Snellen) at month 1 (Fig. 2a) and month 3 (Fig. 2b) after implantation. By month 3, binocular UCVA was 0.3 logMAR or better at distance (4 m), intermediate (60 cm), and near (40 cm). Similarly, monocular UCVA improved from month 1 (Fig. 2c) to month 3 (Fig. 2d). All subjects had BCDVA 20/40 or better at month 3 compared with the preoperative visit (Fig. 3a). Most subjects had 20/40 vision or better at month 3 for binocular UCDVA (100%), UCIVA (100%), and UCNVA (96%) (Fig. 3b). Mean photopic best corrected contrast sensitivity was similar for conditions without glare (Fig. 4a) or with glare (Fig. 4b) and was highest for 6 cpd.
Table 2.
Mean Binocular and Monocular Visual Acuity. (All-Implanted Analysis Set)
| Mean binocular visual acuity, logMAR | Month 1 | Month 3 | ||
| BCDVA, 4 m | − 0.02 | −0.05 | ||
| UCDVA, 4 m | 0.05 | 0.03 | ||
| UCIVA, 60 cm | 0.02 | −0.03 | ||
| UCNVA, 40 cm | 0.05 | 0.03 | ||
| Mean monocular visual acuity, logMAR | Month 1 | Month 3 | ||
| First eye | Second eye | First eye | Second eye | |
| UCDVA, 4 m | 0.09 | 0.10 | 0.07 | 0.08 |
| UCIVA, 60 cm | 0.08 | 0.08 | 0.05 | 0.04 |
| UCNVA, 40 cm | 0.12 | 0.10 | 0.09 | 0.09 |
BCDVA Best corrected distance visual acuity, logMAR Logarithm of the minimum angle of resolution, UCDVA Uncorrected distance visual acuity, UCIVA Uncorrected intermediate visual acuity, UCNVA Uncorrected near visual acuity
Fig. 2.
Binocular visual acuity (a) 1 month and (b) 3 months and monocular visual acuity at (c) 1 month and (d) 3 months after implantation of TFNT00 (full analysis set). Error bars represent 90% CI. BCDVA = best corrected distance visual acuity; logMAR = logarithm of the minimum angle of resolution; UCDVA = uncorrected distance VA; UCIVA = uncorrected intermediate VA; UCNVA = uncorrected near VA; VA = visual acuity
Fig. 3.
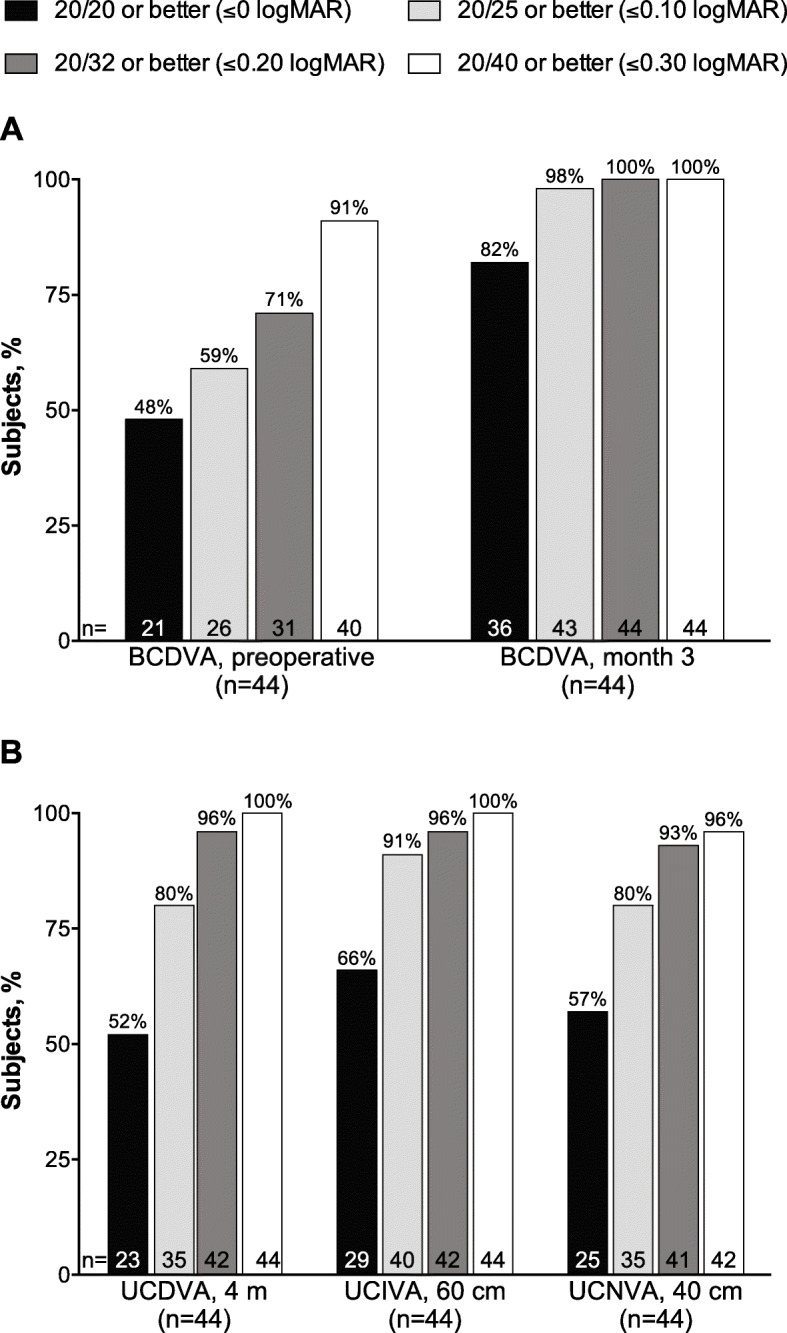
Percentages of subjects with 20/40 vision or better for (a) BCDVA before implantation and 3 months after implantation of TFNT00 and (b) UCDVA, UCIVA, and UCNVA 3 months after implantation of TFNT00 (full analysis set). BCDVA = best corrected distance visual acuity; logMAR = logarithm of the minimum angle of resolution; UCDVA = uncorrected distance VA; UCIVA = uncorrected intermediate VA; UCNVA = uncorrected near VA
Fig. 4.
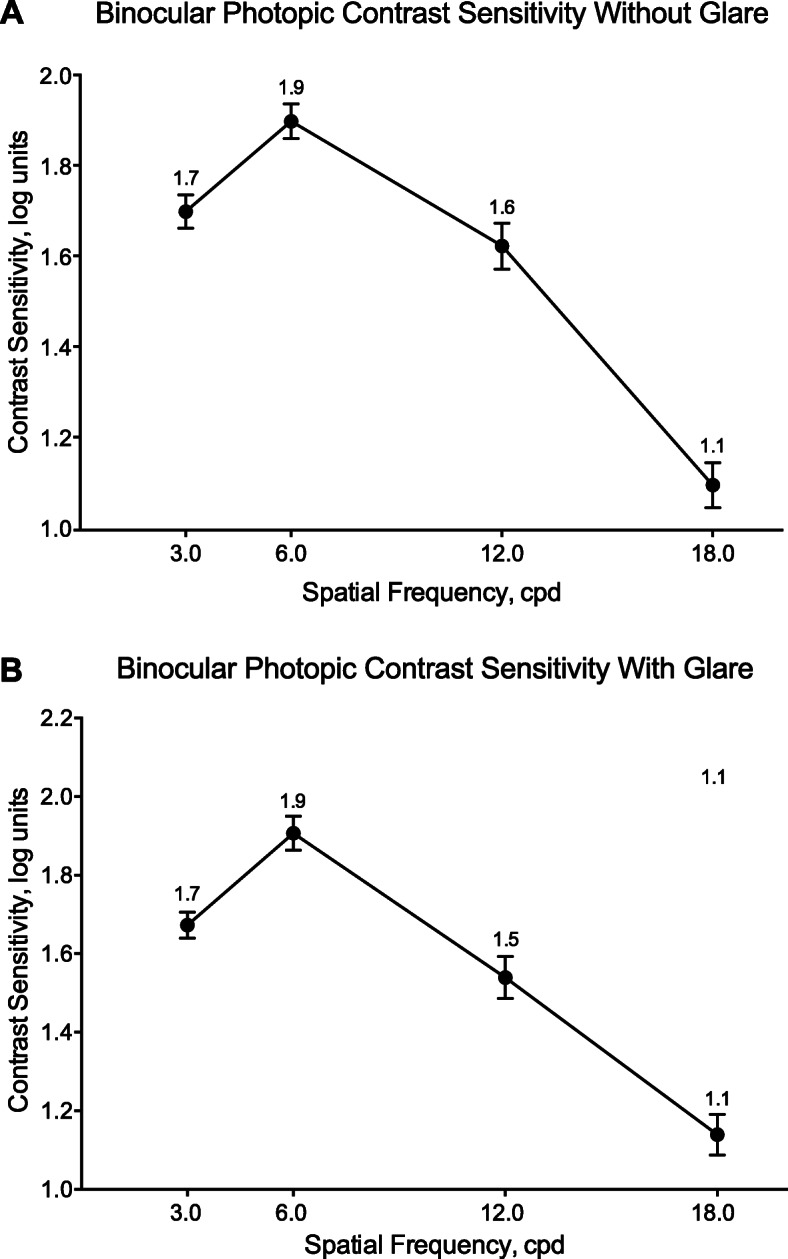
Photopic best corrected binocular contrast sensitivity at 3 months after implantation of TFNT00 (a) without glare and (b) with glare (full analysis set). Error bars represent 90% CI. cpd = cycles per degree
Overall, after implantation of TFNT00, subject satisfaction was higher for near and intermediate vision compared with distance vision (Table 3). Before surgery, 89 and 86% of subjects were dissatisfied with their near and intermediate vision, respectively. At month 3 after IOL implantation, 84 and 77% of subjects were satisfied with their near and intermediate vision, respectively. Spectacle independence for distance, intermediate, and near vision increased by > 60% after IOL implantation. Of the 2 subjects who reported being “very dissatisfied” with surgery results at month 3, 1 experienced mild posterior capsule opacification that was not resolved and the other experienced visual impairment, conjunctivitis, corneal edema, and dry eye.
Table 3.
Responses to Subject Satisfaction Questions (Full Analysis Set)
| TFNT00 (n = 44) | |||
|---|---|---|---|
| Question | Response | Preoperative n (%) |
Month 3 n (%) |
| How satisfied are you with your vision for seeing objects at near distance? | Dissatisfied/very dissatisfied | 39 (89) | 3 (7) |
| Neither satisfied nor dissatisfied | 3 (7) | 4 (9) | |
| Satisfied/very satisfied | 2 (5) | 37 (84) | |
| How often do you wear eyeglasses or contact lenses for seeing objects at near distance? | None of the time | 7 (16) | 37 (84) |
| Some of the time | 7 (16) | 6 (14) | |
| Most of the time | 11 (25) | 0 | |
| All of the time | 19 (43) | 1 (2) | |
| How satisfied are you with your vision for seeing objects at intermediate distance? | Dissatisfied/very dissatisfied | 38 (86) | 5 (11) |
| Neither satisfied nor dissatisfied | 3 (7) | 5 (11) | |
| Satisfied/very satisfied | 3 (7) | 34 (77) | |
| How often do you wear eyeglasses or contact lenses for seeing objects at intermediate distance? | None of the time | 9 (21) | 40 (91) |
| Some of the time | 12 (27) | 3 (7) | |
| Most of the time | 11 (25) | 0 | |
| All of the time | 12 (27) | 1 (2) | |
| How satisfied are you with your vision for seeing objects at distance? | Dissatisfied/very dissatisfied | 28 (64) | 4 (9) |
| Neither satisfied nor dissatisfied | 11 (25) | 9 (21) | |
| Satisfied/very satisfied | 5 (11) | 31 (70) | |
| How often do you wear eyeglasses or contact lenses for seeing objects at distance? | None of the time | 14 (32) | 42 (96) |
| Some of the time | 9 (21) | 1 (2) | |
| Most of the time | 5 (11) | 0 | |
| All of the time | 16 (36) | 1 (2) | |
| How often do you experience halos? | None of the time | 10 (23) | 3 (7) |
| Some of the time | 20 (46) | 11 (25) | |
| Most of the time | 10 (23) | 15 (34) | |
| All of the time | 4 (9) | 15 (34) | |
| How severe were these halos? | None | 9 (21) | 3 (7) |
| Mild | 13 (30) | 5 (11) | |
| Moderate | 15 (34) | 22 (50) | |
| Severe | 7 (16) | 14 (32) | |
| If you currently drive, how much difficulty do you have driving at night? | No difficulty at all | 5 (11) | 4 (9) |
| A little difficulty | 5 (11) | 5 (11) | |
| Moderate difficulty | 13 (30) | 11 (25) | |
| Extreme difficulty | 11 (25) | 10 (23) | |
| I do not drive at night | 10 (23) | 14 (32) | |
| If you do not drive at night, what is the reason? | Because of your current eyesight | 12 (27) | 11 (25) |
| Because you are not interested in driving | 5 (11) | 5 (11) | |
| Because you have other reasons | 10 (23) | 12 (27) | |
| I drive at night | 17 (39) | 16 (36) | |
| How satisfied are you with your cataract surgery result? | Dissatisfied/very dissatisfied | N/A | 3 (7) |
| Neither satisfied nor dissatisfied | 8 (18) | ||
| Satisfied/very satisfied | 33 (75) | ||
| Would you recommend the cataract surgery and the new lenses that were put into your eyes to other people? | No | N/A | 16 (36) |
| Yes | 28 (64) | ||
N/A Not applicable
Although the study sample size was relatively small, a range of pupil sizes were observed in the all-implanted analysis set (Table 4). Subgroup analysis of the defocus curve by pupil size at month 3 did not show an effect of photopic pupil size on visual performance at any range of defocus.
Table 4.
Photopic and Mesopic Pupil Size 3 Months Post-Implantation (All-Implanted Analysis Set)
| TFNT00 | ||
|---|---|---|
| First Eye (n = 45) |
Second Eye (n = 44) |
|
| Photopic pupil size, mean (SD), mm | 3.84 (0.71) | 3.82 (0.84) |
| Photopic pupil size category, n (%) | ||
| Small (≤2.5 mm) | 0 | 2 (5) |
| Medium (2.5–4 mm) | 27 (61) | 25 (57) |
| Large (≥4 mm) | 17 (39) | 17 (39) |
| Mesopic pupil size, mean (SD), mm | 5.31 (0.95) | 5.26 (1.01) |
| Mesopic pupil size category, n (%) | ||
| Small (≤2.5 mm) | 0 | 0 |
| Medium (2.5–4 mm) | 4 (9) | 3 (7) |
| Large (≥4 mm) | 40 (91) | 41 (93) |
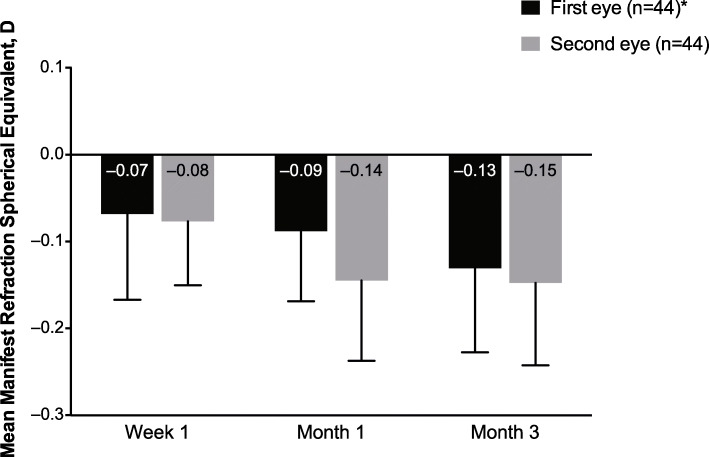
After IOL implantation, mean MRSE was approximately − 0.1 D throughout the study period (Fig. 5). By month 3, absolute residual refraction was within 0.3 D of the target MRSE, indicating good refractive predictability of TFNT00.
Fig. 5.
Mean manifest refraction spherical equivalent over time after implantation of TFNT00 (all-implanted analysis set). Error bars represent 90% CI. D = diopter. *At week 1, n = 45 for the first eye.
Safety
The most common AEs were dry eye (24%) and glare (22%). All other AEs occurred in < 10% of subjects (Table 5), and no subjects discontinued the study because of an AE. Although halo vision occurred in 7% of eyes, no subjects required secondary surgical intervention because of halos. Two serious ocular AEs were reported in 1 subject who experienced mild decentration (2 mm) of the IOL due to capsular contraction and subsequently underwent secondary surgical intervention for repositioning of the IOL.
Table 5.
Adverse Eventsa (Safety Set)
| Preferred Term | TFNT00 | |||
|---|---|---|---|---|
| First Eye (n = 45) |
Second Eye (n = 44) |
|||
| n (%) | E | n (%) | E | |
| Dry eye | 11 (24) | 11 | 10 (23) | 10 |
| Glare | 10 (22) | 10 | 9 (21) | 9 |
| Visual impairment | 3 (7) | 4 | 3 (7) | 3 |
| Halo vision | 3 (7) | 3 | 3 (7) | 3 |
| Foreign body sensation in eyes | 3 (7) | 3 | 2 (5) | 2 |
| Vitreous floaters | 2 (4) | 2 | 3 (7) | 3 |
| Posterior capsule opacification | 1 (2) | 1 | 2 (5) | 2 |
| Vision blurred | 1 (2) | 1 | 2 (5) | 2 |
| Conjunctivitis allergic | 1 (2) | 1 | 1 (2) | 1 |
| Corneal abrasion | 1 (2) | 1 | 1 (2) | 1 |
| Corneal edema | 1 (2) | 1 | 1 (2) | 1 |
| Meibomian gland dysfunction | 1 (2) | 1 | 1 (2) | 1 |
| Conjunctivitis | 1 (2) | 1 | 0 | 0 |
| Corneal opacity | 1 (2) | 1 | 0 | 0 |
| Device dislocation | 0 | 0 | 1 (2) | 1 |
| Myopia | 0 | 0 | 1 (2) | 1 |
| Optic disc hemorrhage | 1 (2) | 1 | 0 | 0 |
| Photopsia | 1 (2) | 1 | 0 | 0 |
| Surgery | 0 | 0 | 1 (2) | 1 |
AE Adverse event, E Event, n Number of eyes with an event. a If an eye had multiple occurrences of an AE, the eye was presented only once in the respective eye count column for the corresponding AE. Events were counted each time in the event column. AEs were coded using the Medical Dictionary for Regulatory Activities Version 21.0
Clinically significant subjective posterior capsule opacification was reported in 3 eyes of 2 subjects and was assessed by the investigator as mild and not related to the IOL. One eye required an Nd:YAG laser treatment of 2-mm-diameter posterior capsulotomy. Two nonserious ocular device AEs were reported by 2 subjects: 1 subject reported mild halo vision in both eyes that resolved at month 3, and 1 subject reported mild visual impairment in both eyes that resolved without sequelae.
Discussion
Subjects who receive IOLs increasingly expect to achieve an extended range of vision after cataract surgery [20]. Compared with a standard monofocal IOL, the trifocal TFNT00 IOL had better corrected and uncorrected near and intermediate VA [21] and may be a suitable choice for subjects who want to achieve spectacle independence after cataract surgery. In 2 large multicenter clinical trials of TFNT00 with study sites located in Australia, Europe, South America, and the United Kingdom, subjects reported high levels of satisfaction with TFNT00 in addition to improved visual outcomes for near, intermediate, and distance vision [16]. Although TFNT00 has been studied in western populations, it has not been evaluated in the Korean population. Recently, the prevalence of myopia in Korea has increased [22], and ophthalmic evaluation surveys from 2008 to 2014 showed that 71% of Korean subjects aged < 50 years and 65% of children had myopia [23, 24]. In some regions, the prevalence of myopia has been reported to be > 80% [25], which may result from increased time spent performing near-distance work [23]. Consequently, many people in Korea have worn glasses since childhood, leading to high expectations for spectacle independence after cataract surgery. In addition, approximately 33% of Korean subjects undergoing cataract surgery are aged < 65 years [19], and this relatively young population wants to achieve spectacle independence after surgery for daily intermediate-distance activities such as computer work.
In this study, visual outcomes and safety were evaluated 3 months after implantation of the TFNT00 IOL in a Korean population. The intermediate focal point at 60 cm was expected to provide optimal intermediate vision for most subjects in the study, because average arm length is 54 cm. At month 3, the binocular defocus curve showed that TFNT00 provided vision of approximately 0.1 logMAR or better over a full range of defocus, and between defocus corresponding to distances of 80 to 40 cm, subjects achieved 0.06 logMAR or better. Study results showed that the Korean population had similar visual outcomes compared with those of western populations who received TFNT00. In a 12-month single-arm trial of 145 subjects in western countries, the mean ± SD best corrected intermediate VA was 0.04 ± 0.12 and 0.08 ± 0.14 logMAR at 60 cm and 80 cm, respectively, and VA of 20/25 or better was achieved across a range of distances from 4 m to 40 cm [15]. In the current study, binocular UCIVA measured at 60 cm was 0.02 logMAR 1 month after IOL implantation and improved to − 0.03 logMAR by month 3, indicating that TFNT00 provided excellent intermediate vision. Overall, 90% of Korean subjects achieved 20/25 vision or better at intermediate distance. Approximately 80% of subjects were satisfied with their postoperative vision, and spectacle independence for intermediate vision increased from 21% before IOL implantation to 91% after implantation. This finding suggests that overall subject satisfaction was improved by better intermediate vision.
In previous comparative clinical trials of TFNT00 with other trifocal IOLs, TFNT00 showed improved visual outcomes at 60 cm. A study of TFNT00 compared with the visual performance of Micro F, an earlier-generation trifocal IOL, showed better VA at 60 cm for subjects who received TFNT00 (P < 0.05) [14]. Furthermore, VA at preferred reading distance (approximately 42 cm) was 0.07 ± 0.07 and 0.11 ± 0.08 logMAR for TFNT00 and Micro F, respectively (P = 0.04) [14]. Similarly, TFNT00 showed improved performance at near distance and at preferred reading distance compared with the Tecnis Symfony (Johnson & Johnson) IOL, an extended depth-of-focus lens [26]. At 40 cm, mean VA was 0.04 ± 0.06 and 0.20 ± 0.06 logMAR for TFNT00 and Symfony, respectively (P < 0.001), and the VA at 60 cm for TFNT00 was 0.06 ± 0.10 logMAR [26], the results of which are comparable with those reported in the current study. The results of these studies suggest that TFNT00 may be a good choice for subjects who want to achieve spectacle independence at both intermediate and near distances.
In a large multicenter trial conducted in western countries, binocular UCIVA and UCNVA was better for subjects who received TFNT00 compared with those who received AT LISA tri 839MP (P = 0.002 and P = 0.003, respectively) 6 months after IOL implantation [16]. Recent trials of the AT LISA tri 839MP IOL, which has an intermediate focal point at 80 cm, in Korean subjects showed that AT LISA tri 839MP provided better VA at intermediate distances compared with a conventional multifocal IOL [27]; however, UCIVA was 0.13 logMAR 6 months after implantation of AT LISA tri 839MP [28]. Although future comparative studies should be conducted for Asian populations, the results of the current study indicate that visual outcomes may be improved with TFNT00 compared with AT LISA tri 839MP for subjects in Korea.
Some subjects who receive multifocal IOLs may have increased visual disturbances and reduced contrast sensitivity compared with those who receive monofocal lenses [29]. Overall, the rates of visual disturbances reported after implantation of TFNT00 in this study were consistent with those in previous studies [29]. Contrast sensitivity results showed a curve similar to that reported for healthy young subjects (mean age 21 y) with normal VA [30], indicating that TFNT00 did not cause a meaningful reduction in contrast sensitivity. Additionally, glare did not affect contrast sensitivity results, and no secondary surgical interventions were required because of visual disturbances of halo or glare.
Limitations of the present study were the relatively short follow-up period and lack of a comparison group. Future trials should evaluate the long-term outcomes, including subject satisfaction, of TFNT00 in the Korean population compared with other multifocal lens options for the correction of presbyopia. Another caveat is that in this study, we used a standard 60-cm distance to assess intermediate vision, although the average arm length in this population is 53–59 cm. Additionally, this study did not include visual quality measurements such as mesopic and scotopic contrast sensitivity, halometry, and ocular aberration; these outcomes should be evaluated in future trials.
Conclusions
In conclusion, this study showed that Korean subjects who received TFNT00 had functional results across the full range of distance, particularly from near to intermediate, had good quality of vision at all distances, and high satisfaction. Overall, the TFNT00 IOL may provide this population with the best intermediate distance results compared with other available trifocal IOLs.
Acknowledgements
Medical writing assistance was provided by Catherine DeBrosse, PhD, of ICON (North Wales, PA), and was funded by Alcon.
Abbreviations
- AEs
Adverse events
- BCDVA
Best corrected distance visual acuity
- cpd
Cycles per degree
- D
Diopter
- IOLs
Intraocular lenses
- logMAR
Logarithm of the minimum angle of resolution
- MRSE
Manifest refraction spherical equivalent
- Nd:YAG
Neodymium-doped yttrium aluminum garnet
- UCDVA
Uncorrected distance visual acuity
- UCIVA
Uncorrected intermediate visual acuity
- UCNVA
Uncorrected near visual acuity
- VA
Visual acuity
Authors’ contributions
TIK, TYC, MJK, KHL, and JYH contributed to the concept and design of the study, acquisition, analysis and interpretation of the data, drafting and revising of the manuscript, administrative and technical support, and final approval of the manuscript. KHL’s contributions also included statistical analysis and securing funding for this study.
Funding
This study was funded by Alcon Research LLC, Fort Worth, TX, USA, and Alcon Korea Ltd., Seoul, South Korea. The sponsor participated in study design; data management, analysis, and interpretation; and funding for the manuscript preparation.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This clinical study was conducted under an approved Institutional Review Board protocol in accordance with the ethical principles of the Declaration of Helsinki, ISO14155:2011 Clinical Investigation of Medical Devices for Human Subjects – Good Clinical Practice, and Standards for Medical Devices for Good Clinical Practice. All subjects provided voluntary written informed consent before initiation of any study procedures.
Consent for publication
Not applicable.
Competing interests
TIK is an advisory board member of and has received personal fees from Hoya Surgical Optics. TYC has nothing to disclose. MJK received grants from Alcon during the study, and has received personal and consultancy fees from Alcon unrelated to the present work. KHL was an employee of Alcon Korea Ltd. during the study. JYH received grants from Alcon Korea Ltd. during the study.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Javitt J, Brauweiler HP, Jacobi KW, Klemen U, Kohnen S, Quentin CD, et al. Cataract extraction with multifocal intraocular lens implantation: clinical, functional, and quality-of-life outcomes. Multicenter clinical trial in Germany and Austria. J Cataract Refract Surg. 2000;26:1356–1366. doi: 10.1016/S0886-3350(00)00636-2. [DOI] [PubMed] [Google Scholar]
- 2.Vingolo EM, Grenga P, Iacobelli L, Grenga R. Visual acuity and contrast sensitivity: AcrySof ReSTOR apodized diffractive versus AcrySof SA60AT monofocal intraocular lenses. J Cataract Refract Surg. 2007;33:1244–1247. doi: 10.1016/j.jcrs.2007.03.052. [DOI] [PubMed] [Google Scholar]
- 3.Kohnen T, Allen D, Boureau C, Dublineau P, Hartmann C, Mehdorn E, et al. European multicenter study of the AcrySof ReSTOR apodized diffractive intraocular lens. Ophthalmology. 2006;113:578–584. doi: 10.1016/j.ophtha.2005.11.020. [DOI] [PubMed] [Google Scholar]
- 4.Alfonso JF, Fernandez-Vega L, Baamonde MB, Montes-Mico R. Prospective visual evaluation of apodized diffractive intraocular lenses. J Cataract Refract Surg. 2007;33:1235–1243. doi: 10.1016/j.jcrs.2007.03.034. [DOI] [PubMed] [Google Scholar]
- 5.Bababekova Y, Rosenfield M, Hue JE, Huang RR. Font size and viewing distance of handheld smart phones. Optom Vis Sci. 2011;88:795–797. doi: 10.1097/OPX.0b013e3182198792. [DOI] [PubMed] [Google Scholar]
- 6.Occupational Safety and Health Administration. Working Safely With Video Display Terminals. OSHA 3092. US Department of Labor; 1997.
- 7.Gatinel D, Pagnoulle C, Houbrechts Y, Gobin L. Design and qualification of a diffractive trifocal optical profile for intraocular lenses. J Cataract Refract Surg. 2011;37:2060–2067. doi: 10.1016/j.jcrs.2011.05.047. [DOI] [PubMed] [Google Scholar]
- 8.Carson D, Hill WE, Hong X, Karakelle M. Optical bench performance of AcrySof® IQ ReSTOR®, AT LISA® tri, and FineVision® intraocular lenses. Clin Ophthalmol. 2014;8:2105–2113. doi: 10.2147/OPTH.S66760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kohnen T, Titke C, Bohm M. Trifocal intraocular lens implantation to treat visual demands in various distances following lens removal. Am J Ophthalmol. 2016;161:71–77. doi: 10.1016/j.ajo.2015.09.030. [DOI] [PubMed] [Google Scholar]
- 10.Charness N, Dijkstra K, Jastrzembski T, Weaver S, Champion M. Monitor viewing distance for younger and older workers. Proc Hum Factors Ergon Soc Annu Meet. 2008;52:1614–1617. doi: 10.1177/154193120805201965. [DOI] [Google Scholar]
- 11.Kohnen T. First implantation of a diffractive quadrafocal (trifocal) intraocular lens. J Cataract Refract Surg. 2015;41:2330–2332. doi: 10.1016/j.jcrs.2015.11.012. [DOI] [PubMed] [Google Scholar]
- 12.AcrySof IQ PanOptix Presbyopia-Correcting IOL. Product Information. Forth Worth: Alcon Laboratories, Inc.; 2015.
- 13.Carson D, Xu Z, Alexander E, Choi M, Zhao Z, Hong X. Optical bench performance of 3 trifocal intraocular lenses. J Cataract Refract Surg. 2016;42:1361–1367. doi: 10.1016/j.jcrs.2016.06.036. [DOI] [PubMed] [Google Scholar]
- 14.Gundersen KG, Potvin R. Trifocal intraocular lenses: a comparison of the visual performance and quality of vision provided by two different lens designs. Clin Ophthalmol. 2017;11:1081–1087. doi: 10.2147/OPTH.S136164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bala C, Martinez AA, Kohnen T. Multicenter visual outcomes evaluation of a new trifocal presbyopia correcting IOL – 12 month results. Presented at: American Society of Cataract and Refractive Surgery, April 13-17, 2018.. Washington, DC.
- 16.Lapid-Gortzak R, Martinez A. Multicenter clinical investigation of visual function after bilateral implantation of two presbyopia-correcting trifocal IOLs [abstract]. Presented at: European Society of Cataract and Refractive Surgeons, September 22-26, 2018. Vienna; 2018.
- 17.Ahn JH, Kim DH, Shyn KH. Investigation of the changes in refractive surgery trends in Korea. Korean J Ophthalmol. 2018;32:8–15. doi: 10.3341/kjo.2017.0010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee Y. Estimation of body size and growth patterns in Korean boys. J Physiol Anthropol. 2015;34:20. doi: 10.1186/s40101-015-0058-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Korean Statistical Information Service. Available at: http://kosis.kr/eng/index/index.do. Accessed 21 June 2019.
- 20.Pager CK. Expectations and outcomes in cataract surgery: a prospective test of 2 models of satisfaction. Arch Ophthalmol. 2004;122:1788–1792. doi: 10.1001/archopht.122.12.1788. [DOI] [PubMed] [Google Scholar]
- 21.Monaco G, Gari M, Di Censo F, Poscia A, Ruggi G, Scialdone A. Visual performance after bilateral implantation of 2 new presbyopia-correcting intraocular lenses: trifocal versus extended range of vision. J Cataract Refract Surg. 2017;43:737–747. doi: 10.1016/j.jcrs.2017.03.037. [DOI] [PubMed] [Google Scholar]
- 22.Lee DC, Lee SY, Kim YC. An epidemiological study of the risk factors associated with myopia in young adult men in Korea. Sci Rep. 2018;8:511. doi: 10.1038/s41598-017-18926-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Han SB, Jang J, Yang HK, Hwang JM, Park SK. Prevalence and risk factors of myopia in adult Korean population: Korea national health and nutrition examination survey 2013-2014 (KNHANES VI) PLoS One. 2019;14:e0211204. doi: 10.1371/journal.pone.0211204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lim DH, Han J, Chung TY, Kang S, Yim HW. Epidemiologic survey Committee of the Korean Ophthalmologic Society. The high prevalence of myopia in Korean children with influence of parental refractive errors: the 2008-2012 Korean National Health and nutrition examination survey. PLoS One. 2018;13:e0207690. doi: 10.1371/journal.pone.0207690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee JH, Jee D, Kwon JW, Lee WK. Prevalence and risk factors for myopia in a rural Korean population. Invest Ophthalmol Vis Sci. 2013;54:5466–5471. doi: 10.1167/iovs.13-12478. [DOI] [PubMed] [Google Scholar]
- 26.Ruiz-Mesa R, Abengozar-Vela A, Ruiz-Santos M. A comparative study of the visual outcomes between a new trifocal and an extended depth of focus intraocular lens. Eur J Ophthalmol. 2018;28:182–187. doi: 10.5301/ejo.5001029. [DOI] [PubMed] [Google Scholar]
- 27.Yu S, Kim YI, Ha SW, Lee GJ, Lee KW, Park YJ. Comparison of the visual outcomes after cataract surgery with implantation of a bifocal and trifocal diffractive intraocular lens. J Korean Ophthalmol Soc. 2016;57:405–412. doi: 10.3341/jkos.2016.57.3.405. [DOI] [Google Scholar]
- 28.Kwon YK, Kim HK, Lee JH. Clinical outcomes of diffractive trifocal intraocular lens in both eyes: a 6-month follow-up. J Korean Ophthalmol Soc. 2015;56:1331–1337. doi: 10.3341/jkos.2015.56.9.1331. [DOI] [Google Scholar]
- 29.de Silva SR, Evans JR, Kirthi V, Ziaei M, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2016;12:CD003169. doi: 10.1002/14651858.CD003169.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Koefoed VF, Baste V, Roumes C, Hovding G. Contrast sensitivity measured by two different test methods in healthy, young adults with normal visual acuity. Acta Ophthalmol. 2015;93:154–161. doi: 10.1111/aos.12487. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.