Abstract
The estimation of pleural pressure with esophageal manometry has been used for decades, and it has been a fertile area of physiology research in healthy subject as well as during mechanical ventilation in patients with lung injury. However, its scarce adoption in clinical practice takes its roots from the (false) ideas that it requires expertise with years of training, that the values obtained are not reliable due to technical challenges or discrepant methods of calculation, and that measurement of esophageal pressure has not proved to benefit patient outcomes. Despites these criticisms, esophageal manometry could contribute to better monitoring, optimization, and personalization of mechanical ventilation from the acute initial phase to the weaning period. This review aims to provide a comprehensive but comprehensible guide addressing the technical aspects of esophageal catheter use, its application in different clinical situations and conditions, and an update on the state of the art with recent studies on this topic and on remaining questions and ways for improvement.
Keywords: respiratory mechanics, asynchrony, mechanical ventilation, physiologic monitoring, ARDS, mechanical ventilator weaning
Introduction
More than a century ago, Luigi Luciani1 described the measurement of esophageal pressure (Pes) by means of an esophageal catheter and used it as a surrogate of pleural pressure (Ppl). This technique was later made popular by Buytendijk2 through his dissertation on Pes published in 1949. In the following decades, several renowned researchers such as Meade, Milic-Emili, Fry and their co-workers dedicated a great deal of effort to further develop, improve, and fine-tune the measurement devices and technique.3-9 Since then, Pes monitoring has known periods of enthusiasm and hope (and disappointment), but it has remained primarily a research tool.
Pes is an excellent surrogate for Ppl; therefore, it is extremely useful to understand each patient’s individual respiratory physiology in 3 main scenarios. First, it can be used to characterize the respiratory system mechanics during passive mechanical ventilation. Second, it is useful to monitor patient’s respiratory muscle activity during assisted ventilation. Third, it serves to understand patient–ventilator interaction (ie, synchrony and asynchrony).
Theoretically, the gold standard for Ppl assessment is direct measurement with the insertion of pressure transducers in the pleural space. This can be justified in animal studies, but it is invasive and is not acceptable, practical, or feasible for regular patient monitoring. Thus, esophageal manometry can be a safe alternative.
Esophageal manometry has been used (and is still used) in some expert centers and for research purposes. However, it has never reached a broad audience, and it has not been introduced into routine clinical practice. Despite its potential benefits for better understanding the mechanics of the respiratory system and optimizing mechanical ventilation of hypoxemic patients, the LUNG SAFE study showed that <1% of the subjects with ARDS who were receiving invasive ventilation had an esophageal catheter inserted.10
This review aims to provide a thorough and up-to-date review on esophageal manometry from its theoretical principles to its potential clinical use.
Technical Considerations
Pes is measured via an air-filled balloon catheter inserted in the esophagus. Some catheters are equipped with a second balloon that sits in the stomach and is intended to measure gastric pressure. This allows the assessment of transdiaphragmatic pressure, which is the difference between gastric pressure and Pes. Some gastric feeding tubes include an esophageal balloon that permits both gastric feeding (or suction) and Pes measurement with a single device. However, the use of 2 distinct catheters (ie, one for feeding and one for Pes measurement) is possible and does not affect Pes measurements.11 The quality, accuracy, and reliability of the measurement is affected by the characteristics of the balloon catheter (ie, material, length, diameter), the balloon-filling pressure, and the surrounding pressure, as well as the position of the catheter in the esophagus and the patient’s position. The following section will detail each of these features. As with any therapeutic or monitoring device in the ICU, clinicians must balance the benefits and risks of complication before inserting an esophageal catheter. The contraindications are rare and are basically the same as for a nasogastric tube: risk of bleeding (eg, esophageal varices, severe coagulopathy) and risk of local injury in some specific patients (eg, skull or maxilla-facial fractures).
Catheter Insertion
After unpacking the catheter, an initial inflation and deflation with a few milliliters of air (not exceeding the manufacturer’s recommended volume) loosens the balloon and prevents incorrect measurements due to adhesion of the balloon on the catheter.12 Similar to nasogastric or orogastric tube insertion in a patient who is awake, a local anesthetic spray or gel can be applied in the nose and oropharynx according to the local protocol and in the absence of contraindication. Catheter insertion can be facilitated by placing the patient in a semi-recumbent position with head tilted forward and by lubricating the tip of the tube. The depth at which the catheter should be placed can be estimated by the distance from the nostril to the ear to the xyphoid. The catheter is inserted through the nostril or the mouth and progressively pushed down to the stomach (usually at 50–60 cm, depending on the patient’s height), inflated, and connected to a pressure transducer. The latter is linked to the pressure port of the ventilator or a dedicated monitoring device. At that level, gentle repeated manual pushes below the patient’s xyphoid (epigastric area) are transmitted as simultaneous inflections of the pressure waveform and suggest that the balloon sits in the stomach. Likewise, ventilator insufflation or patient’s inspiratory effort may show a positive swing on the tracing. The catheter is then slowly withdrawn to reach the lower and middle third of the esophagus, at which point cardiac artifacts should appear on the waveform (distance from the teeth is usually 35–45 cm). The middle third of the esophagus is where the pressure measurement is more stable, uniform, and less influenced by external structures.6 However, the catheter should be placed where it better represents Ppl as confirmed by the occlusion test (see Validation of the Measurement). At this location, the appearance of the tracing depends on the patient’s underlying respiratory activity. In a passive patient (eg, comatose, deeply sedated, paralyzed or not), machine insufflation leads to positive deflection due to an increase in Pes (Fig. 1A); in an actively breathing patient, effort leads to a negative swing due to a decrease in Pes (Fig. 1B); when a patient triggers the breath but does not sustain effort (eg, during assisted ventilation), there is an initial negative swing followed by a positive deflection (Fig. 1C). Figure 2 from the review by Akoumianaki et al13 on the same topic shows the pressure waveforms during the insertion of a double-balloon catheter in an intubated patient under pressure support ventilation. Mauri et al14 provided a very useful video showing the insertion and calibration of an esophageal catheter in the online supplement of their recent review.
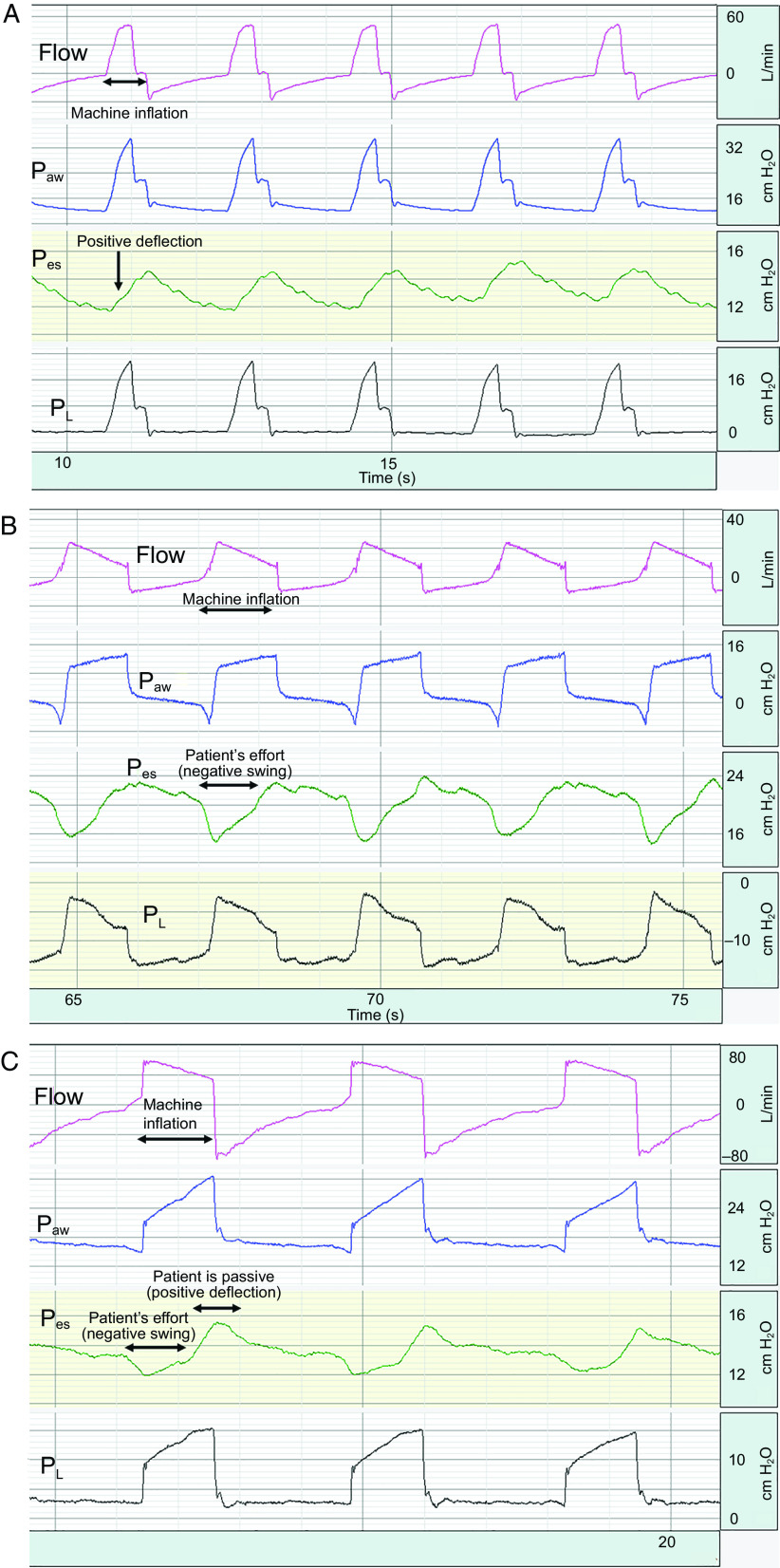
Fig. 1.
Examples of flow (pink), airway pressure (Paw blue), esophageal pressure (Pes, green), transpulmonary pressure (PL, black) in patients with different breathing conditions (passive, active, or partially active). (A) Flow, Paw, Pes, and PL waveforms in a passive patient during volume assist control ventilation. Machine inflation creates a positive deflection on the Pes tracing that comes back to baseline during exhalation. (B) Flow, Paw, Pes, and PL waveforms in a patient breathing actively and triggering all of the breaths during pressure support ventilation. The patient’s effort creates a negative swing in the Pes tracing, triggering machine inflation. (C) Flow, Paw, Pes, and PL waveforms in a patient triggering the machine but not sustaining effort. The patient’s effort creates an initial negative swing in the Pes tracing. When the patient’s effort stops during the second phase of inspiration, the patient is passive and the machine inflation creates a positive pressure transmitted to the Pes, leading to a positive deflection. During exhalation, Pes goes back to baseline.
Fig. 2.
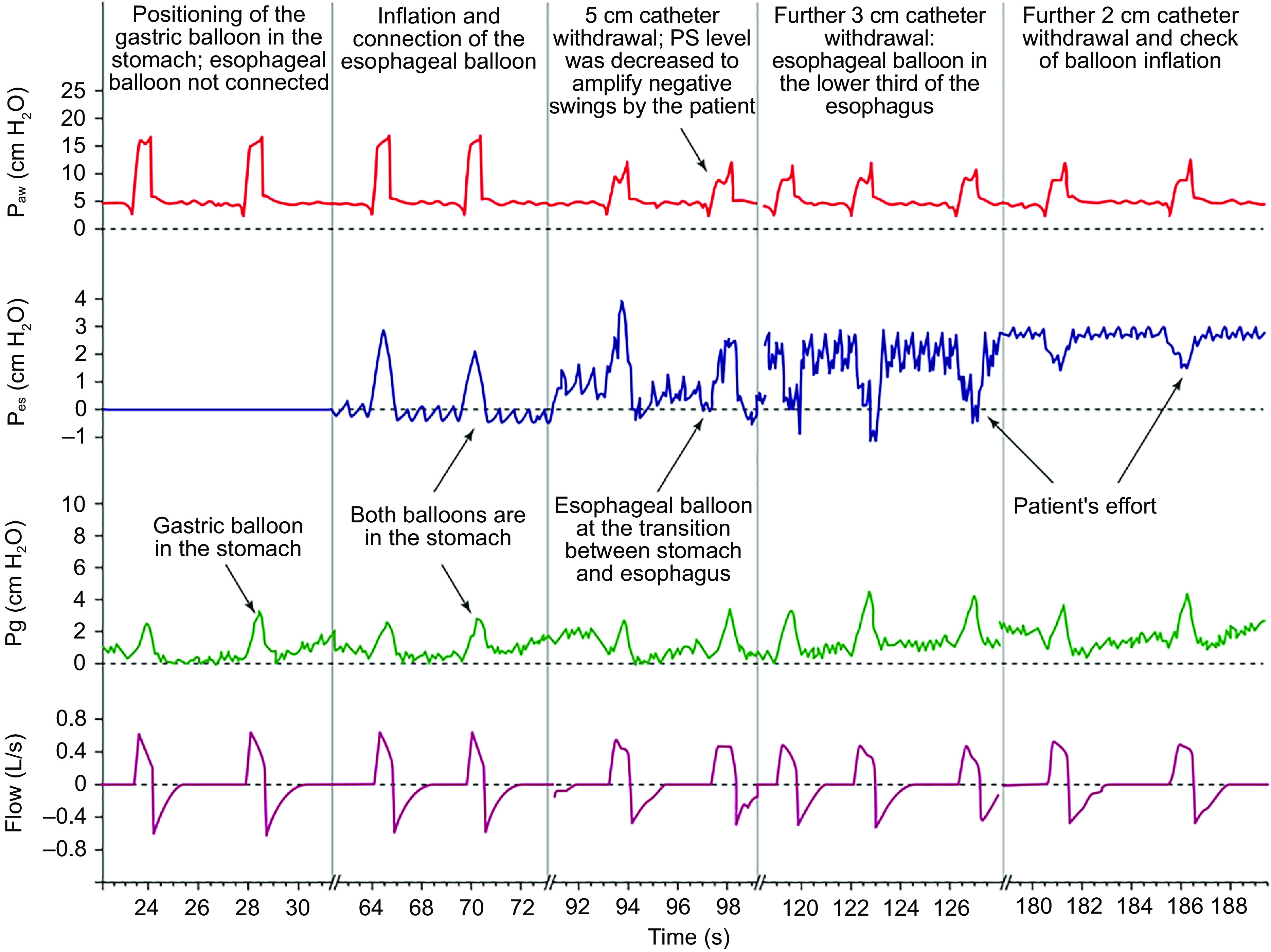
Pressure waveforms during insertion of an esophageal catheter. Paw = airway pressure; Pes = esophageal pressure; Pg = gastric pressure; PS = pressure support. From Reference 13, with permission.
Balloon Inflation Volume
If the filling is optimal, the balloon should fit the esophagus wall but not overstretch it so that it can accurately transmit the surrounding pressure. Similarly, the inflation volume should be small enough to avoid any balloon recoil pressure. If the balloon is underfilled, Pes will be underestimated; if the balloon is overfilled, Pes will be overestimated.
Several teams have performed in vitro studies to assess the mechanical characteristics of different commercially available balloon catheter in various conditions.12,15,16 In these series of experiments to test the reliability of Pes at different filling volumes in static conditions, the authors reported that all catheters could provide an accurate measurement of surrounding pressure ranging from 0 to 30 cm H2O.12,15 However, the range of appropriate filling volumes varied among catheters and were typically higher than those recommended by the manufacturers, especially when surrounding pressure was high.15 Walterspacher et al12 also noted that balloon overinflation led to an overestimation of the actual surrounding pressure; nevertheless, they reported that the mechanical properties of the overinflated balloon changed over time. By repeating their experience after 16 h of overinflation, they could obtain accurate estimates of the surrounding pressure with higher filling volumes than in their initial assessment.12 Still in vitro but in dynamic conditions assessing pressures during end-inspiratory and end-expiratory occlusions, Yang et al16 also reported that there was a range of filling volumes that allowed accurate measurement of the surrounding pressure. The bottom line is that the optimal filling varies with experimental conditions and, in translating these findings to clinical settings, one can hypothesize that optimal volumes vary between patients and for a given patient, with his or her evolution.
Mojoli et al17 proposed a method to optimize the filling volume of the esophageal balloon and calibrate Pes. Briefly, the aim is to determine the optimal volume by computing end-inspiratory and end-expiratory pressure-volume curves at different filling volumes (ranging from 0 to the maximum recommended for a given catheter type) (Fig. 3). Authors defined Vmin and Vmax as the volumes at lower and upper limits of the linear section of the pressure-volume curve, and optimal filling (Vbest) as the volume that maximizes the difference between Pes at end-inspiration and Pes at end-expiration. Elastance of the esophagus (Ees) is calculated based on the slope of the linear section of the end-expiratory pressure-volume curve; the pressure generated by the esophageal wall is ([Vx − Vmin] × Ees), where Vx = a given filling volume. Finally, the calibrated Pes is the difference between the absolute value of Pes and the pressure generated by the esophageal wall. The process is time-consuming but could be an important preliminary step to obtain reliable and accurate estimation of the Ppl in cases where very precise measurements are needed for research purposes. Interestingly, another team confirmed these results, reproducing almost the same experiment with another type of esophageal catheter but limiting the test to only 3 filling volumes.18
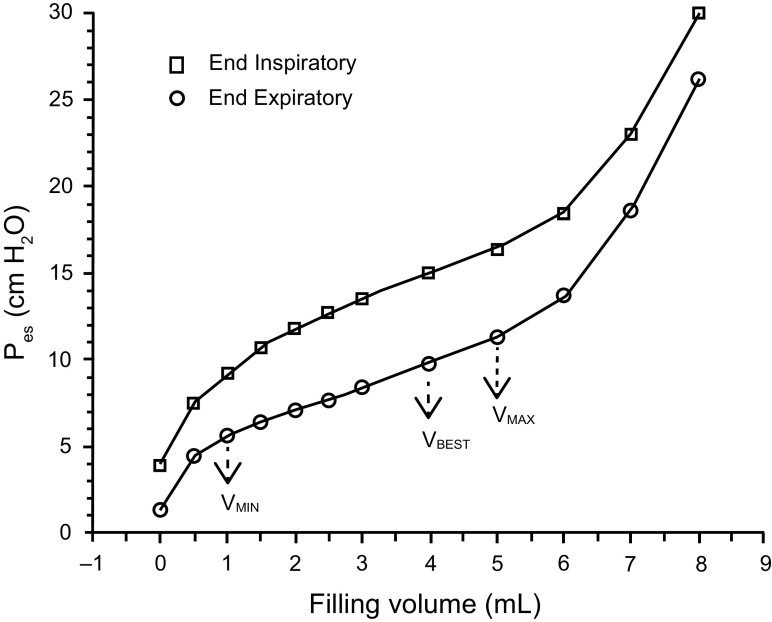
Fig. 3.
Static esophageal balloon pressure-volume curves showing the relationship between balloon filling volume and static values of esophageal pressure (Pes), both at end-expiration (circles) and at end-inspiration (squares). On the end-expiratory pressure-volume curve, the intermediate linear section was graphically detected and analyzed for its lower and upper limits (VMIN and VMAX, respectively). The range between VMIN and VMAX was considered to correspond to appropriate balloon filling, with volumes below VMIN denoting underfilling and volumes above VMAX denoting overdistention. The elastance of the esophagus (cm H2O/mL) was considered equivalent to the slope of this section of the end-expiratory pressure-volume curve. Within the appropriate filling range, we identified VBEST as the filling volume associated with the maximum difference between end-inspiratory Pes and end-expiratory Pes. From Reference 17, with permission.
Validation of the Measurement
To ascertain that the catheter is placed in the appropriate location and provides an acceptable proxy for Ppl, Baydur et al19 proposed an occlusion test in spontaneously breathing subjects. The principle of this test is to occlude the patient’s airway opening so that any change in pressure should be the same in the whole occluded system. In other words, when a patient makes an inspiratory effort during the occlusion, there is no flow in the system and the change in Pes (ΔPes) should be equal to the change in the airway opening pressure (ΔPaw). This means the ratio of ΔPaw to ΔPes should be close to 1. In practice, the Pes measurement is considered a reliable surrogate of Ppl when this ratio is between 0.8 and 1.2. By applying the same concept in passively ventilated patients with lack of inspiratory efforts, a modified occlusion test has been proposed, consisting of an external manual pressure applied to the rib cage during an expiratory pause. This positive pressure occlusion test has been validated in animal studies and more recently in paralyzed subjects.20,21
Artifacts and Troubleshooting
Even when the catheter is in the correct position and the balloon inflation is optimized, artifacts such as transmission of the heart beat or esophageal spasm can impede Pes-based estimation of pleural pressure, particularly when the cardiac oscillations are of the same magnitude as the Pes swings or when the spasms are frequent (Fig. 4). Changing the angle of the bed to have the patient in more of a seated position or withdrawing the catheter a few centimeters can, in some cases, decrease cardiac artifacts. Esophageal spasms are sometimes triggered by patient stimulation or by end-inspiratory or end-expiratory occlusions. In any case, paralysis will not be appropriate to stop esophageal spasms because the lower part of the esophagus, where the catheter is usually placed, consists of smooth, nonstriated muscles, which are insensitive to neuromuscular blocking agents.
Fig. 4.
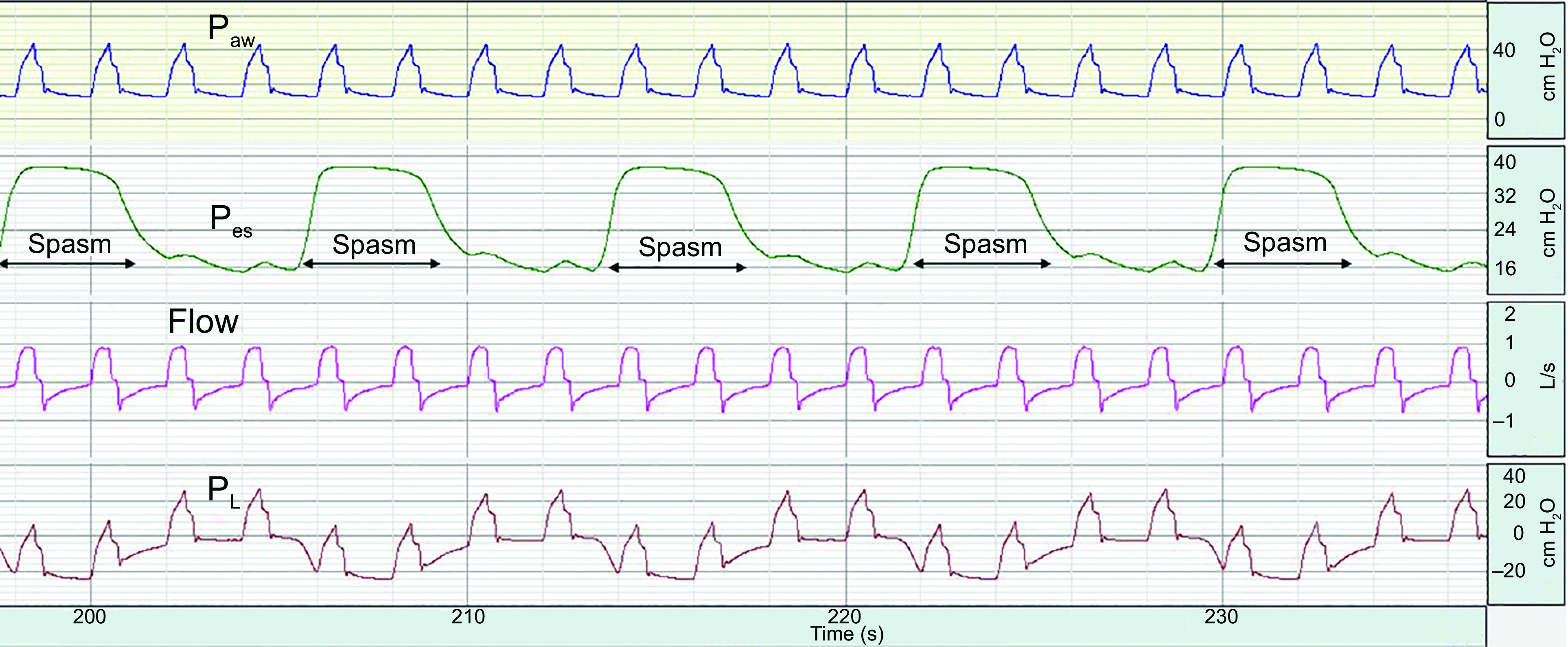
Example of frequent esophageal spasm hampering esophageal pressure (Pes) monitoring. Regular spasm lasting around 4 s occur every 5 s. During spasms, Pes as high as 38 cm H2O is not representative of pleural pressure anymore and end-expiratory transpulmonary pressure (PL) falsely reads -20 cm H2O. Paw = airway pressure.
Position
Since the 1950s, physiologists have known that body position influences Pes and measurement of respiratory system mechanics; specifically, Pes in a supine subject was consistently higher than Pes measured in other conditions.22,23 The main hypothesis was that mediastinal content compressed the esophagus and generated an artifact overestimating Pes.4,6,7,24-26 Most of these studies included healthy subjects who had repeated measurements in different positions, but Mead and Gaensler4 also performed simultaneous assessments in subjects equipped with both an esophageal and a pleural catheter and reported similar results. More recently, Washko et al27 hypothesized that the higher Pes while supine was not only due to a direct compression artifact but also to the change of lung relaxation volume in different positions. They performed an experiment to assess each effect separately, and they reported that part of the increase in Pes is due to the actual pressure difference between upright and supine position caused by relaxation volume reduction. Nevertheless, ∼3 cm H2O is actually a postural artifact and could be corrected by direct subtraction in the measurements. Surprisingly, this correction factor was not used in the subsequent studies from the same group, and it is essential to keep in mind that important interindividual variability exists.28,29 More recently, Yoshida et al30 proved in an animal model and human cadavers that Pes measured in the supine position is a good surrogate of Ppl at the mid-chest. In that study, absolute values of Pes fell between those of the dorsal and ventral Ppl values measured with direct pleural sensors, which minimized the clinical relevance of the so-called postural artifact.30
How Is Esophageal Manometry Interpreted During Passive Ventilation?
Transpulmonary Pressure in the Passive Patient: What It Is and Is Not
During passive ventilation, pressure at the airway opening, referred to as airway pressure (Paw) reflects the total pressure delivered across the entire respiratory system, comprised of both the lungs and chest wall. During air flow, Paw is composed of two components, the flow-resistive pressure (Presistive) and the elastic recoil pressure (Pelastic) of the respiratory system:
| [1] |
where EL and ECW denote lung and chest wall elastance, respectively.
In states of zero flow, such as during a breath-hold, flow-resistive pressure is zero, and Paw then reflects only the recoil pressure of the respiratory system. Perhaps the most common application of esophageal manometry is to isolate lung pressure from chest wall recoil pressure during zero-flow states, such as during a breath-hold. When flow is zero, the transpulmonary pressure (PL) then describes the elastic recoil pressure across the lung, often referred to as lung parenchymal stress:31
| [2] |
It is often reported that PL during zero flow is a measure of transalveolar pressure,13,32 which is incorrect for several reasons.33 Pressure measured at the airway opening (ie, endotracheal tube) may not reflect pressure inside the alveolus when airway closure occurs or when alveoli are fluid-filled.33-35 Additionally, Ppl gradients exist within the chest, and alveolar septal interdependence produces regional mechanical heterogeneity in states of patchy edema.36,37 Thus, although PL during zero flow is, by definition, the pressure difference across the lung, it should not be viewed as equivalent to transalveolar pressure, which varies regionally and is unknowable clinically.
Reconciling the Direct and Elastance-Based Methods of Measuring PL
PL is the pressure difference across the lung (ie, PL = Paw – Ppl).31 While there is broad agreement in this definition, controversy exists around how to use esophageal manometry to estimate Ppl and thus PL. The 2 methods used often in recent literature, the direct and elastance-based methods, yield incongruous results.38
The traditional definition of PL, dating to the mid-20th century, involves substituting Pes directly for Ppl (Ppl = Pes), resulting in PL = Paw – Pes.4,39,40
The alternative elastance-derived method41 estimates Ppl from Paw and the ratio of respiratory system and chest wall elastances obtained during an inspiratory hold:
| [3] |
Therefore:
| [4] |
Although the elastance-derived method has been used in several studies, its assumptions challenge long-established respiratory physiology.33,42 First, elastance of any structure is defined as the change in pressure for a given change in volume (ΔP/ΔV); it is mathematically impossible to infer a static pressure simply from knowing the elastance. Second, the elastance-derived method assumes that Ppl and PL must be 0 cm H2O (atmospheric) when Paw is 0 cm H2O (see Equation 3 and Equation 4). During healthy normal respirations, Paw is 0 cm H2O at both end-inspiration and end-expiration with the airway open and communicating with the ambient (atmospheric) pressure. The elastance-derived method would lead to the invalid conclusion, then, that PL (and lung stress) must be the same (ie, equal to 0 cm H2O) at end-inspiration and end-expiration absent positive-pressure ventilation. However, during critical illness Ppl is often positive at end-expiration and therefore PL negative.
The traditional method, substituting Pes directly for Ppl, also has limitations. Small vertical spatial Ppl gradients exist within the chest.36,43,44 Although these are thought to be less than hydrostatic equilibrium (ie, < 1 cm H2O per cm height), they nevertheless predispose to regional differences in ventilation. Patient position can influence Pes measures due to mediastinal weight.27 Still, several studies have indicated that a correctly placed catheter positioning the balloon in the retrocardiac mid-thoracic esophagus affords a reasonable estimate of average Ppl in the chest.27,30,42,45,46
Despite their conceptual differences, the traditional and elastance-derived methods provide (different but) useful information that are not as incompatible as it may appear at first sight. Yoshida et al30 recently performed a study using both esophageal catheters and sensors inserted directly in the pleural space in cadavers preserved according to the Thiel method47 and in pigs with acute lung injury. One of their most striking findings is that the direct method consistently represents the PL of the dependent lung (anatomically close to the balloon), whereas the elastance-derived method matches inspiratory PL of the nondependent part of the lung. With this elegant demonstration, one can hypothesize that the direct method could be used to optimize collapsed lung recruitment and the elastance-derived method could be helpful to protect nondependent lung areas from overdistention and prevent ventilator-induced lung injury. This approach has not been formally tested yet, and a study aiming at individualizing ventilation based on this concept should start soon (Careful Ventilation in ARDS, NCT03963622). Realistically, it is impossible to reach full recruitment without overdistention, and clinicians have to compromise to optimize PEEP and tidal volume settings.
Pes to Guide PEEP During Passive Ventilation
Esophageal manometry is perhaps best known for its potential role in guiding PEEP titration in ARDS. Small airways and alveoli may be predisposed to closure or collapse when Ppl exceeds Paw.48 Therefore, measuring Pes at end-expiration may be useful to identify the minimum PEEP required to prevent airway closure and alveolar collapse.49 Such a strategy of Pes-guided PEEP was compared to an empiric low PEEP strategy in the EPVent trial, a single-center, randomized trial of 61 subjects with ARDS.28 The Pes-guided PEEP strategy was associated with significantly higher PaO2/FIO2 and respiratory-system compliance. Lower mortality was observed in the Pes-guided group (17% vs 39%), a difference that was statistically significant after adjusting for baseline illness severity.
The follow-up EPVent-2 trial,29 a multi-center trial with 200 subjects, compared Pes-guided PEEP to an empiric high-PEEP strategy and found no significant difference in survival or secondary physiological end points. EPVent-2 was not a validation study of EPVent because the comparator treatment arms were intentionally different.50
In EPVent, an empiric low-PEEP strategy was used in the comparator arm. Thus, in EPVent, end-expiratory Paw was less than Pes on average in the empiric low-PEEP group, potentially predisposing to airways and alveolar collapse, and end-expiratory PL was significantly lower in the empiric low-PEEP group versus the Pes-guided group.
By comparison, EPVent-2 adopted an empiric high-PEEP strategy in the comparator arm, resulting in Paw ≥ Pes in the comparator arm and no significant difference in end-expiratory PL on average over the first few study days. Without a significant difference in PL, which was the hypothesized mechanism of benefit of the Pes-guided intervention, it is unsurprising that no significant differences in key clinical outcomes were observed.
Importantly, there also were no significant differences in barotrauma or adverse hemodynamic effects between groups in EPVent-2. Empiric high PEEP is not routinely used in clinical practice, likely in part due to concerns for barotrauma and hemodynamic compromise.10 Thus, pending more definitive clinical trials data, esophageal manometry still may have an important role in clinical practice by providing additional information about lung and chest wall mechanics when interpreting Paw in consideration of increasing PEEP.
Pes to Guide Tidal Volume During Passive Ventilation
When titrating ventilator settings, especially in ARDS, evidence-based guidelines recommend limiting inspiratory plateau pressure (Pplat) to 30 cm H2O; however, monitoring Paw suffers from the inherent limitation that it has no compelling corollary with normal spontaneous breathing. In contrast, PL has the same meaning during positive-pressure ventilation and spontaneous breathing because it is calculated based on both Paw and Ppl. Studies that measured esophageal manometry in healthy individuals indicate that a PL of approximately 20–25 cm H2O is the upper limit encountered during a breath-hold at total lung capacity, which is considered the upper limit of lung stress that might be encountered by the lungs in normal life.51
Extrapolating this concept to positive-pressure ventilation may be useful for titrating tidal volume by identifying the risk of excess stress. In patients with ARDS, higher end-inspiratory PL correlates with smaller aerated lung volume and has been associated with increased risk of death.52 It is unclear whether this limit is safe in injured lungs, such as in ARDS. Because the ARDS lung is predisposed to injury, a lower threshold than that experienced in healthy breathing may be required. Setting tidal volume to a target value of transpulmonary driving pressure also has been proposed.4 Experts in the field widely recognize the need for an individualized approach to setting tidal volume in ARDS,53,54 but the optimal approach remains to be defined.
How Is Esophageal Manometry Interpreted During Active Breathing?
Estimation of Global Lung Stress
We discussed above that lung stress (ie, the distending pressure of the lung during tidal breathing) is accurately represented by PL. During passive ventilation with no patient activity, when Pes is not monitored, PL is often approximated with Paw, which is available on all ventilators screens and does not require an additional catheter insertion. This is not a perfect substitute, because pleural pressure varies substantially and unpredictably between patients. This issue is compounded further during assisted mechanical ventilation, wherein, the total pressure applied to the respiratory system results from the positive pressure applied by the ventilator (readily available on the ventilator screen), and the negative pressure generated by the respiratory muscles (hidden to the clinician with regular monitoring). Therefore, Paw during assisted ventilation grossly underestimates the distending pressure of the lungs. Measuring Pes as a surrogate of Ppl allows the calculation of lung stress (ie, PL) in this context, unmasking the pressure applied by the respiratory muscles.55 As a proof of concept, Yoshida et al56 used an animal model to show that, despite keeping a constant safe Pplat < 30 cm H2O and a constant tidal volume, strong breathing efforts can result in worsening lung injury consistent with the higher PL.
In this context, the relative risk or benefit of spontaneous breathing depends on the strength of the effort, which determines PL, and the degree and type of lung injury. Specifically, relatively weak breathing efforts and mild lung injury can result in overall benefit, whereas strong efforts in the context of severe injury can result in worsening lung injury, highlighting the importance of measuring Pes to estimate lung stress.57 Of note, PL has a resistive and a elastic component. The resistive component depends on inspiratory flow and resistance, and only the transalveolar component is relevant in terms of lung stress. Transalveolar pressure calculated using Pes has been shown to be negative (ie, lower than PEEP) in some subjects with strong breathing efforts during assisted mechanical ventilation.58 This might have adverse hemodynamic consequences that can lead to increased interstitial and alveolar edema potentially worsening lung injury.
Dynamic changes in PL (ΔPL) are also an important characteristic. Ppl changes during spontaneous breathing are not evenly distributed around the lungs in patients with lung injury. Distribution of negative forces generated by the diaphragm depends on the type of lung injury. In some patients with healthy lungs, change in Ppl is homogeneous around the lung, resulting in homogeneous distribution of PL and lung inflation; this is referred to as fluid-like behavior.55 Other patients with lung injury and a larger amount of nonaerated lung tissue present a solid-like behavior in which distribution of PL and inflation is heterogeneous. More so, the uneven distribution of ΔPL during spontaneous breathing can result in pendelluft flow (ie, distribution of air from one lung region to another), causing regional increases in lung stretch without changing the overall tidal volume.59 Pes is a global estimate of Ppl. Therefore, when calculating PL and ΔPL, this limitation needs to be acknowledged, highlighting the potentially uneven distribution of the distending pressures, which might play a relevant role in lung injury during spontaneous breathing.
Monitoring Inspiratory Effort
Activation of respiratory muscles generates a negative change in Ppl; given that Pes is a surrogate of Ppl, several parameters can be calculated using Pes to quantify the magnitude of breathing effort. The simplest and most readily available is the change in Pes (ΔPes) during tidal breathing. However, muscular pressure (Pmus), which is the force generated by the respiratory muscles and is calculated as the difference between Pes and the chest wall recoil pressure (Pcw) at the given tidal volume, is slightly higher than ΔPes. Pcw is the static pressure generated by the chest wall when displaced from its resting position at a certain tidal volume. During passive conditions, Pes represents Pcw or trans-chest wall pressure (ie, Ppl – Patm). However, during spontaneous breathing, Ppl (Pes) no longer represents the passive mechanical characteristics of the chest wall, but the negative deflection in Ppl during spontaneous breathing is the result of the negative pressure generated by the respiratory muscles: Ppl = Pcw – Pmus. Therefore, as explained before, Pmus = Pcw – Ppl.
Chest wall recoil pressure cannot be measured during spontaneous breathing; therefore, it is calculated as the product of tidal volume and chest wall elastance (Ecw):
| [5] |
| [6] |
Ecw can also only be measured in passive conditions; however, it is relatively stable in a patient for a short period of time. Therefore, if passive respiratory mechanics were measured early during mechanical ventilation in a patient, this information might be used for calculating Pmus when actively breathing. Alternatively, if a patient is breathing spontaneously, transient complete relaxation can be achieved by hyperventilation. Hyperventilation using high tidal volumes decreases respiratory drive and results in relaxation of respiratory muscles, which allows the measurement of Ecw. Otherwise, chest wall compliance can be estimated as 4% of predicted vital capacity per cm H2O.14,60,61 Predicted vital capacity is based on sex, height, and weight, and it can be calculated using several online calculators; Ecw is the inverse of chest wall compliance, measured in L/cm H2O.
However, inspiratory effort is not an instantaneous event; timing of breathing effort is relevant in terms of energy expenditure of the respiratory muscles, risk of injury, and fatigue. Therefore, the reference method to measure inspiratory effort resulting from activation of all respiratory muscles is the pressure-time product of the esophagus (PTPes). It is calculated as the integral of Pmus over time from the beginning of inspiratory effort until the end of inspiration62 and correlates with energy expenditure of the respiratory muscles (Fig. 5A). Work of breathing is calculated as the area enclosed in the Pes – volume loop using the Campbell diagram (Fig. 5B).63 It is closely related to the concept of work in physics that refers to the force generated to move an object over a certain distance. The main limitation relies on the fact that it only quantifies inspiratory effort during volume displacement, ignoring activation of respiratory muscles during isometric contraction. Both the pressure-time product of the esophagus and work of breathing can be partitioned into the inspiratory effort exerted to overcome the elastic (due to intrinsic PEEP and mechanical characteristics of the respiratory system) and resistive load. The Campbell diagram can also be used to assess activation of expiratory muscles.62,63
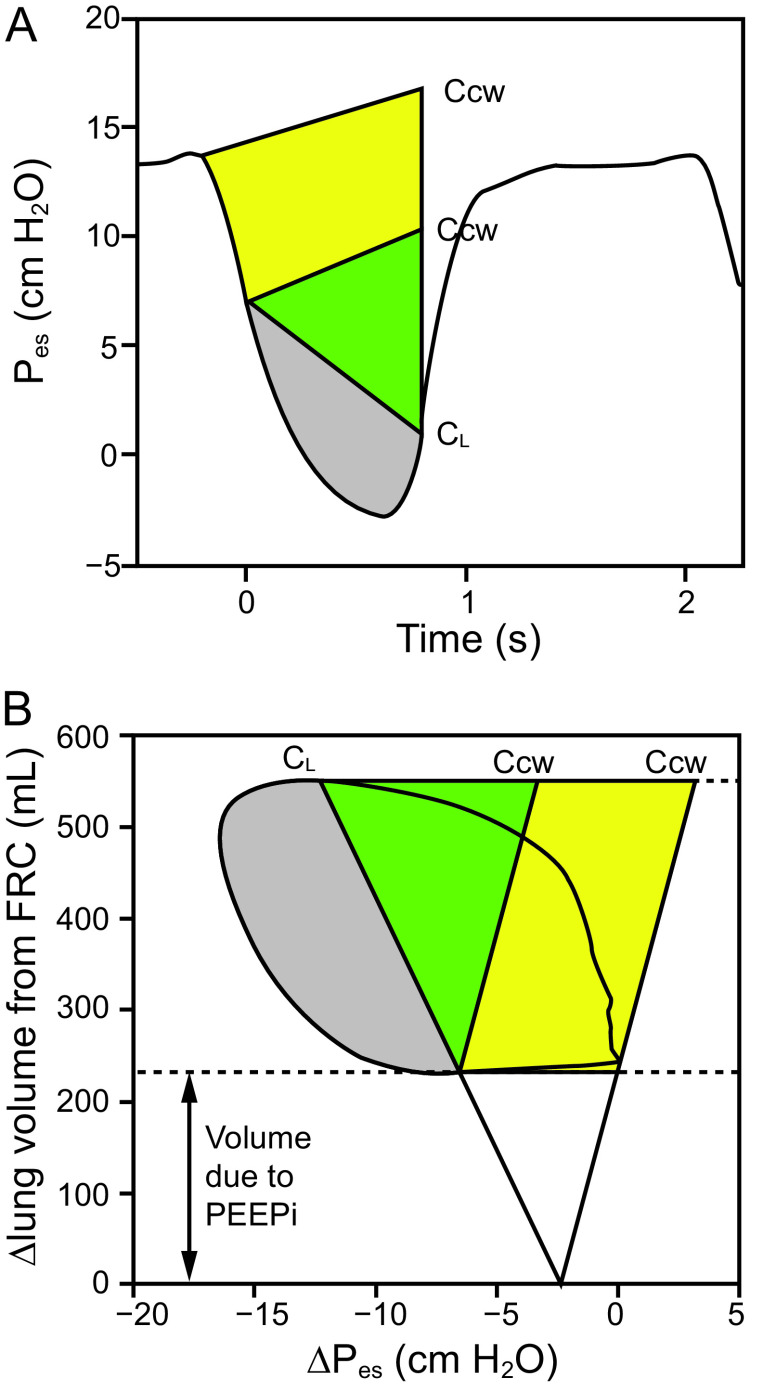
Fig. 5.
Examples of ways to assess patient effort with esophageal pressure. (A) Esophageal pressure (Pes) tracings. Ccw, estimated at 4% of vital capacity, has been superimposed on Pes at the onset of the fall in Pes and at the onset of inspiratory flow generation (ie, the first vertical line), together with dynamic CL. The colored area comprises the total pressure-time product (PTP) of respiratory muscle pressure. The yellow area is the PTP attributed to intrinsic PEEP, the green area represents elastic PTP, and the gray area represents resistive PTP. (B) Pressure-volume curve of Pes and lung volume. The Ccw and CL intersect at FRC. The yellow area represents work of breathing (WOB) attributed to intrinsic PEEP, the green area represents elastic WOB, and the gray area represents resistive WOB. Ccw = compliance of the chest wall; CL = compliance of the lung; FRC = functional residual capacity; PEEP = positive end-expiratory pressure; FRC = functional residual capacity; VC = vital capacity; PEEPi = intrinsic PEEP. Redrawn from data in reference 61.
When gastric pressure is available, transdiaphragmatic pressure (Pdi) can be calculated as the difference between gastric pressure and Pes and allows the estimation of the pressure specifically generated by the diaphragm, which is the main inspiratory muscle. Positive deflection in Pdi can be calculated (ΔPdi) or the pressure-time product of the diaphragm as the integral of Pdi over the duration of inspiration, which also correlates with energy expenditure of the diaphragm.64
Monitoring Patient–Ventilator Interactions (Diagnosis of Dyssynchronies)
Asynchrony, usually defined as a discrepancy between a patient’s neural times and need and the ventilator-delivered breath, could have an impact on patient outcomes.65-69 Asynchrony regularly happens when a patient is overassisted (eg, ineffective effort, delayed cycling) or underassisted (eg, premature cycling, flow starvation). Asynchrony can be challenging to detect only with Paw and flow waveforms, therefore esophageal manometry might assist in the diagnosis. In this section, we summarize common dyssynchronies and how they can be diagnosed on tracings displaying Pes.
Delayed cycling occurs when ventilator insufflation is longer than the patient’s inspiratory effort. This can occur during continuous mandatory ventilation when the inspiration time is too long or during pressure support due to either excessive support or inadequate cycling criteria resulting in long insufflation times. An example of delayed cycling is shown in Figure 6A: diagnosis is facilitated by the Pes tracing, in which the patient’s effort (Pes negative swing) has ended but machine insufflation continues (Pes passively increases).
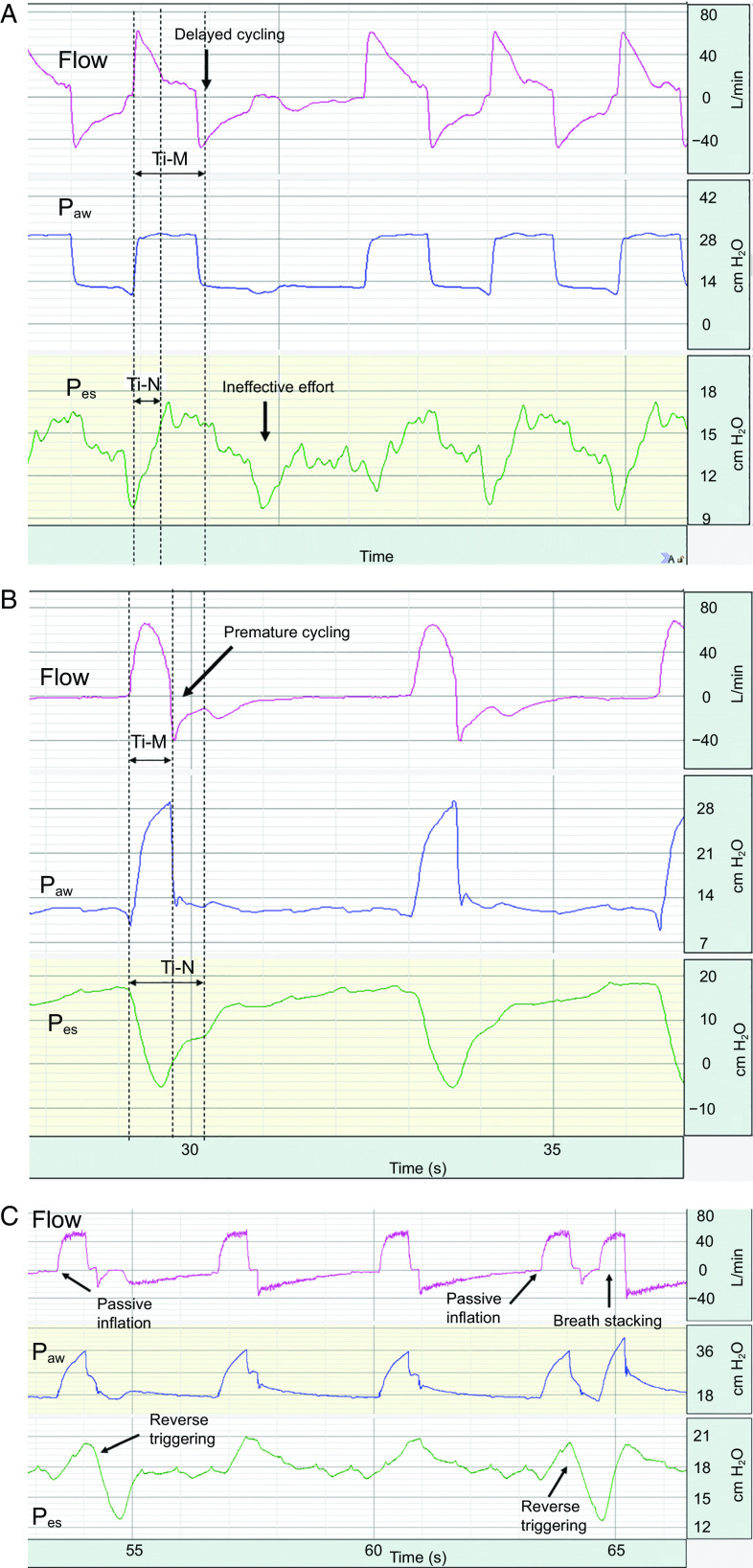
Fig. 6.
Flow (pink), airway pressure (Paw, blue), and esophageal pressure (Pes, green) waveforms showing patient-ventilator dyssynchronies. (A) In pressure assist controlled mode, the machine inflation time (Ti-M) lasts longer than the patient’s neural inspiration (Ti-N), creating delayed cycling. This excess assistance causes ineffective effort in the following breath because the patient’s respiratory muscle contraction is not strong enough to trigger an inflation (ie, wasted effort). This is clearly seen on the Pes tracing, which shows a negative deflection failing to trigger a machine inflation. This can also be suggested by the concomitant bump seen on the flow tracing during the expiration phase. (B) In pressure controlled continuous mandatory ventilation mode, the Ti-M is shorter than the patient’s Ti-N, creating premature cycling. The patient’s inspiratory effort continues beyond machine inspiration and prevents the peak expiration flow usually seen when the expiration valve opens and the exhalation is passive (ie, the patient tries to get flow in while the circuit is supposed to let the flow go out). The bump in the early phase of the exhalation is also suggestive of the patient effort continuing during expiration. (C) In volume controlled continuous ventilation mode, the initial inflation is passive in all breaths, and the machine starts the inspiration phase on a time command. At the end of the inspiration phase, the patient’s effort occurs (ie, the negative swing seen on the first breath), and there is a muscle contraction continuing during the expiration. As during ineffective effort or short cycling, this can be suggested by the bump on the flow seen during expiration. This likely creates an eccentric diaphragm contraction that could be injurious. This sequence of passive inflation followed by a muscle contraction is defined as reverse triggering. Of note, the fourth breath shows the same type of asynchrony, but this reverse triggering is strong enough to trigger a second inflation and breath stacking. This type of reverse triggering with breath stacking can injure the lung by providing tidal volume as high as twice the value set on the machine.
Ineffective efforts, also known as failed triggering, are patient inspiratory efforts that fail to result in triggering a ventilator inspiratory cycle. Insofar as they lead to eccentric diaphragm contractions, they may contribute to ventilation-induced diaphragm dysfunction.70 Ineffective efforts can be especially difficult to detect clinically when they occur early during the expiratory phase or in patients with auto-PEEP because either case will result in only subtle changes in flow and Paw.71 By contrast, ineffective efforts are readily detectable with esophageal manometry by observing negative deflections in Pes without the corresponding initiation of the machine’s inspiratory cycle (Fig. 6A). This can be caused by overassistance leading to weak efforts, typically in patients with delayed cycling or dynamic hyperinflation.
Premature cycling, on the other hand, is a case of underassistance and is defined by the mechanical ventilator expiration starting before the patient’s inspiratory effort is over. Again, this phenomenon is easily diagnosed with a Pes tracing in which the negative swing continues during the exhalation phase (Fig. 6B). When the patient’s effort remains strong during the exhalation phase, a second insufflation can be triggered, leading to an increase in the global tidal volume (ie, breath-stacking).
The term reverse-triggering was recently defined as a patient’s muscle contraction following a passive insufflation.67 Usually, a patient’s effort triggers a breath, but in reverse-triggering the machine insufflation triggers a patient’s effort. Because the Pes tracing provides clear identification of patient effort (ie, negative swing), it helps diagnose reverse-triggering; a machine insufflation (with no patient effort) comes first (ie, Pes passively rises), then the start of muscle contraction creates a negative swing (Fig. 6C). Respiratory entrainment is defined as phase-locking of the patient neural respiratory rhythm (and effort) to an extrinsic rhythm, such as the pre-set rate or rhythm of the ventilator.72-75 Respiratory entrainment can result in ineffective efforts, eccentric diaphragm contraction, and breath-stacking. When reverse-triggering happens in the context of entrainment, the rhythmic, stereotyped pattern of patient effort that is the hallmark feature of entrainment is readily identified with esophageal manometry.
Flow starvation is a form of asynchrony when insufflation flow does not match patient demand. It typically occurs during continuous mandatory ventilation when the peak flow is not set high enough. It could be diagnosed when a concavity that corresponds to a patient’s strong inspiratory effort is present on the Paw waveform. However, Pes tracing facilitates the interpretation by actually displaying the negative swings in Pes proportional to patient’s effort.
What Could Be the Best Indications?
Lung- and Diaphragm-Protective Ventilation
The use of Pes can help clinicians individualize mechanical ventilation and sedation practices based on concrete physiological variables. As with any monitoring techniques, esophageal manometry does not describe the patient’s unique physiological characteristics only at baseline but must also assess the response to specific interventions. Conducting randomized controlled clinical trials to test interventions related to mechanical ventilation is challenging. Therefore, understanding each patient’s individual physiology allows clinicians to adjust the available evidence to unique patients and guide mechanical ventilation when there is no conclusive evidence emerging from the trials.
Specifically in this context, the use of Pes might help in the design and implementation of a lung- and diaphragm-protective ventilation strategy.76 There is an urgent need for such strategies because interventions that aim to protect the lung might harm the diaphragm and vice versa. Precise monitoring techniques, individualized treatment, and personalized ventilation settings could prevent or balance lung and diaphragm injury. For example, the use of heavy sedation or paralysis during early acute hypoxemic respiratory failure that completely inhibits inspiratory effort to obtain low tidal volume ventilation can result in rapid disuse myotrauma of the diaphragm.70 Instead, precise measurements of the magnitude of inspiratory effort and understanding its potential impact on lung and diaphragm injury in each patient might allow the clinician to maintain a safe amount of breathing effort that might avoid muscle disuse atrophy while still protecting the lung. Clinical evidence on the safety and efficacy of such strategies are not available yet despite growing physiological and epidemiological data indicating that some injurious clinical presentations should be avoided (eg, excessive inspiratory efforts in patients with severe lung injury or prolonged absence of inspiratory efforts).57,77,78 Clinical evidence on the practical use of Pes for this purpose will probably become available in the next few years, but for now, we share our personal perspective on the practical use of Pes during the course of mechanical ventilation for all critically ill patients. In the next section, we will focus on specific conditions.
During early mechanical ventilation, especially when there is significant lung injury with altered respiratory mechanics, Pes might serve to determine the relative weight of abnormalities in lung and chest wall mechanics and estimate global lung stress and strain. It can then serve to monitor the effect of changes in ventilator parameters such as changes in tidal volume, PEEP, or prone position on a patient’s respiratory mechanics. In fact, implementing a program for systematic assessment of respiratory mechanics using Pes in all patients with moderate and severe acute respiratory distress syndrome (ARDS) was shown to be feasible, resulted in changes in ventilator settings, and was associated with an improvement of several physiological variables such as oxygenation index and driving pressure.79 Concurrently, Pes in the early phase permits the titration of sedation or neuromuscular blocking agents to the minimum dose that still controls or eliminates inspiratory efforts. Finally, Pes during that early period could potentially help in achieving a minimum safe amount of effort that allows the patient to breathe spontaneously by measuring global lung stress and strain. Recent recommendations and trends in clinical practice suggest minimizing the use of sedative drugs, and after partial recovery with improvement in oxygenation, respiratory mechanics, and hemodynamics, continuous sedation should be stopped.80 Pes in this context can be extremely helpful in detecting overassistance with very low breathing effort (ie, when the patient only triggers the ventilator and then relaxes), injurious breathing effort (underassistance), and dyssynchronies.65,81 Moreover, Pes can assist in monitoring any intervention that aims to control drive and effort, including changes in sedation and ventilator parameters.
Specific Conditions and Subpopulations
Data are still limited with regard to the advantages of using an esophageal catheter to set and monitor mechanical ventilation in clinical practice. Two randomized controlled trials28,29 in which end-expiratory PL was used to set PEEP reported conflicting results, and only a few observational studies focused on this topic. However, some specific populations of patients (such as those with hypoxemia/ARDS, obesity, chest wall abnormalities, intra-abdominal hypertension) might benefit from personalized ventilation based on PL.
Patients with ARDS.
Absolute values of Pes vary widely, and its value is unpredictable.40,82 Therefore, a Pplat that is considered safe can mean different things in terms of risk of lung overdistention depending on the mechanical characteristics of the chest wall. High Pplat in the context of high chest wall elastance might still be safe in terms of lung overdistention, and a safe Pplat might represent a potentially injurious condition for the lung if the chest wall elastance is low. Likewise, high PEEP can be insufficient when end-expiratory Pes is high, leading to end-expiratory lung collapse and atelectrauma through the closing and reopening phenomenon. The one size fits all protective ventilation approach of setting tidal volume to 6 mL/kg predicted body weight and PEEP to obtain Pplat of 27–30 cm H2O might not be adequate or appropriate to limit ventilator-induced lung injury in all patients.83,84 In the era of precision medicine, Pes could be one of the important tools to initially optimize and then adapt settings during the course of mechanical ventilation by considering the many changes that occur during an ICU stay. Translating into practice the observation that direct measurement and elastance-derived calculation of PL represent different areas of the lung could be an interesting way to control ventilator-induced lung injury.30 However, it seems virtually impossible to completely recruit the lung (ie, maximize end-expiratory lung volume) without any overdistention, and the optimal ventilation will remain a trade-off.85
Lung injury alters respiratory mechanics and drive, possibly making dyssynchronous efforts more harmful. As discussed in the previous section, Pes monitoring in these patients is an interesting tool to monitor asynchrony, the amount of muscle activity after the acute phase of the disease, or to guide the weaning period.
Prone Position.
It is commonly accepted that one of the beneficial effects of prone positioning in patients with ARDS stems from the increase of chest-wall elastance, which renders the lung more homogeneous.86,87 A recent study comparing lung mechanics in prone versus supine position did not report any change in chest-wall elastance, and its authors hypothesized that their use of an inclination >0° during prone position could explain this discrepancy.88 Interestingly, this study reported improvement of lung mechanics during prone position with, again, unpredictable individual variations of the effect of proning on end-expiratory Pes and PL.88 Therefore, measurement of advanced respiratory mechanics (discriminating lung and chest wall mechanics) might be warranted to understand the unique response to prone positioning in different patients.
Obesity.
Compared to lean patients, overweight and obese patients have increased end-expiratory Pes, thus esophageal manometry might be of special interest in obese patients on ventilation.89 This population often exhibits reduced lung volume and atelectasis due to increased thoracoabdominal pressure, especially when lying supine in the ICU, and is at risk of airway closure.34,35,48,49,90,91 Though it has been reported that chest-wall elastance was normal and lung elastance reduced in obese subjects, the chest-wall pressure-volume curve is shifted to the right due to the mass loading.48,92-95 In other words, compared to nonobese patients, at a given Paw, PL and lung volume are lower, increasing the risks of atelectasis. In such patients, ventilation without esophageal manometry blinds the clinician to important information, and setting ventilation only with Paw and PEEP tables seems insufficient. Interestingly, a recent study testing 3 PEEP-titration strategies in obese subjects challenges this assertion, reporting that setting ventilation to optimize respiratory system elastance without chest-wall elastance measurement could be efficient.96 In this crossover study, Fumagalli et al96 showed that setting PEEP to obtain the lowest respiratory system elastance (after a recruitment maneuver) led to more similar PEEP than the study group set to obtain a 0–2 cm H2O end-expiratory PL. Compared to the low PEEP- ARDSnet table,83 both strategies led to significantly increased PEEP and improved oxygenation, recruitment, and respiratory mechanics. The optimized respiratory system elastance strategy was even more beneficial in that it further increased recruitment and reduced overdistention of the nondependent part of the lung.
Weaning.
The use of Pes has contributed substantially to understanding the underlying respiratory physiology pertaining to the weaning process in general and weaning failure in particular.62 Specifically, by quantifying the work of breathing and inspiratory effort using Pes together with other physiological parameters, several features are better understood.97 First, successful weaning results from an adequate balance between the load imposed to the respiratory muscles (ie, altered mechanics and gas exchange) and their capacity (ie, respiratory muscle function). Second, work of breathing immediately after extubation is often increased.98 Third, the load imposed to the respiratory muscles after extubation (ie, work of breathing) can be predicted by performing a spontaneous breathing trial without assistance (ie, T-piece or CPAP 0 cm H2O), and therefore the risk of weaning failure can be predicted using various monitoring parameters during these tests.99
However, implementation of Pes in clinical practice to assist clinicians in the decision to extubate a patient was rarely tested. In a study of subjects with prolonged ventilation (mean 20 d of mechanical ventilation), Jubran et al100 reported that a progressive increase in inspiratory effort quantified by the change in Pes swings (ΔPes) between the first and the ninth minute of a spontaneous breathing trial using a T-piece had an excellent diagnostic accuracy to predict failure of the weaning test (area under receiver operating characteristic = 0.94). This index performed better than measuring the ΔPes or rapid shallow breathing index during the first minute. For this purpose, Jubran et al100 developed an algorithm to quantify the progressive change in ΔPes, which they named the trend index. This index may be applicable in monitoring devices to follow patients in real time; however, it has not been implemented yet. Nevertheless, the rationale and results of this study provide some insights on the pathophysiology of weaning failure and how to use this information during weaning. First, a progressive increase in inspiratory effort measured during a spontaneous breathing trial without assistance is highly suggestive of possible failure. Second, if this is encountered, clinicians might consider evaluating the potential trigger (eg, weaning-induced pulmonary edema or bronchospasm) and treat accordingly to avoid failure by using diuretics, afterload reduction agents, inotropes, or bronchodilators.
Limits of the Technique and Barriers to Its Widespread Use
While we advocated throughout this review for a broader but sensible use of Pes measurement, several barriers to its adoption in clinical settings remain, which could explain the small number of patients with Pes monitoring in the LUNG SAFE study.10 It is not necessary to obtain dedicated monitoring devices because most newer ventilators and the usual monitors can display Pes and PL. However, catheters are disposables, and individual cost is not negligible. This price must be considered in the care strategy and can be dissuasive in settings with limited resources. A common criticism is that the technique is complicated and requires expertise at each step: choice of the type of catheter, catheter insertion, balloon filling, validation maneuver, pressure collection, number interpretation, and repeated measurements in evolving conditions and after position changes. As with the implementation of any new device, protocol, or procedure, initiating Pes measurement in the clinical setting necessitates a motivated and proactive team that is convinced of the enhancement this could bring to patient care. The team at St Michael’s hospital in Toronto, Ontario, Canada, educated their clinical fellows and respiratory therapists on the topic by way of a quality-improvement program. Since then, most of the respiratory therapists working in this hospital have the technical skills to independently insert a catheter, measure respiratory mechanics, and optimize ventilation based on interpretation of the values.79 Expertise in esophageal manometry increases with exposure to the technique, and new devices such as high-resolution manometry might solve some technical issues in the near future.26
Some clinicians are reluctant to use Pes because they remain skeptical about the reliability of the values measured and are concerned by the discrepancy between direct and elastance-derived methods to calculate PL. We hope we clarified in this review that measurement accuracy depends on the careful step-by-step process from catheter insertion to the actual assessment. As detailed above, the direct and elastance-derived methods are not incompatible but are complementary and represent different parts of the lung.30
Finally, the current absence of evidence of clinical benefit should not lead to the absolute rejection of this technique; instead it should be an incentive to better understand the underlying physiology, to better select patients who might benefit from Pes monitoring, and to propose other ways to optimize and personalize ventilation.
Summary
Esophageal manometry as a surrogate of Ppl allows us to separate lung from chest wall mechanics assessment and provides useful information to monitor and potentially optimize mechanical ventilation. Careful step-by-step catheter insertion and pressure transduction verification ensures the quality of the signal acquired, as well as the accuracy and reliability of the data obtained. During passive ventilation, esophageal manometry could help prevent ventilator-induced lung injury by optimizing recruitment of the dependent lung while avoiding overdistention of the nondependent lung. When patients have active muscle contraction, Pes tracings are a handy tool to diagnose all types of asynchrony and to measure PL and breathing effort. Later in the course of ventilation, for patients with challenging weaning, quantification of effort and changes in the amount of effort during a spontaneous breathing test can help clinicians better understand the patient’s condition and potential treatment. Despite these potential benefits, no trials have definitively demonstrated the positive impact of esophageal manometry on patient outcomes. This might explain its scarce use in clinical practice and the reluctance of non-experts to start using it despite being available for decades. Some specific subpopulations of patients with chest-wall abnormalities, such as those with abdominal hypertension or obesity, could benefit from this monitoring and should be targeted in future studies. Future research might use esophageal manometry to find the right amount of patient effort to provide both lung- and diaphragm-protective ventilation. This technique may be essential to the personalization and optimization of ventilation in the context of precision medicine.
Footnotes
A version of this paper at the 58th Respiratory Care Journal Conference, held June 10–11, 2019, in St Petersburg, Florida.
Dr Pham has disclosed a relationship with BetterCare. Dr Telias has disclosed relationships with the Canadian Institutes for Health Research, Covidien, and MbMed SA. Dr Beitler has disclosed no conflicts of interest.
Discussion
Schmidt:
I want to come back to the question of setting of PEEP in ARDS patients. I wonder if we should set PEEP the same in active and passive patients? When we think about the balance of recruitment or over-distension we’re largely thinking about the passive setting. The active patient might be different because of the issue of pendelluft, and because pendelluft seems to be PEEP-dependent maybe PEEP should be different in an active and a passive patient. Maybe we should be studying PEEP settings differently in passive patients than we do in active patients. Do you think esophageal pressure measurements could be a way to pick a patient population?
Pham:
I totally agree with your comments. One of the things esophageal pressure cannot assess is pendelluft; we could do it using, for instance, a combination of EIT and esophageal pressure, which can be interesting. Regarding active ventilation, I think it depends on the period when you’re studying and assessing the patient. Up to now most trials have focusing on the initial period, where most severe ARDS patients with a PaO2/FIO2 ratio lower than 150 are sedated, likely paralyzed, and sometimes prone. We also know it’s not the practice worldwide, as in the LUNG SAFE study1 less than 40% of the patients with severe ARDS were paralyzed. You already have severe ARDS patients who are actively breathing so, how do you use esophageal pressure to measure respiratory system mechanics in this setting? I agree with you that pendelluft is important in these patients and if it occurs, likely having a higher PEEP is protective.2 So it might be different to set PEEP in a patient with active breathing as compared to passive patients. Also, some patients have intermittent active breathing and you are able to do a proper assessment and set PEEP based on the passive breaths. Most of the time, the PEEP you use when you have any assessment of respiratory mechanics is higher than what you use if you didn’t have esophageal pressure. You also might need more protective ventilation even if the patient is actively breathing, but this is only a hypothesis. I have no data to show you.
Piraino:
For setting of PEEP with an actively breathing patient using esophageal pressure, it may be better to use something like the swing rather than the absolute value. This concept in patients with severe intrinsic PEEP where you can see the change in esophageal pressure that occurs prior to the triggering of the activation of a mandatory breath. Again if you adjust PEEP and you see a reduction of the swing and better timing, then it may be important to understand the drive. I can tell you from experience that it’s very difficult to get a nice baseline absolute value of esophageal pressure in an actively breathing patient. When you do an expiratory occlusion, they’re trying to trigger, and there may be expiratory activity that can cause the baseline to never be flat – so I think the swing would be more important here. The swing would be an optimal setting for somebody with active breathing to determine the effect of PEEP or perhaps the course of pressure support. The amount of support will impact the swing, but PEEP may also impact it. Ewan [Goligher], do you want to comment on that?
Goligher:
I completely agree with your point that the mechanisms driving injury may be very different between active and passive patients, and I think it just highlights the broader issue that we should know whether our patients are actively or passively breathing and make decisions accordingly. Maybe this will come up again, but to me, the major deficit that occurs in practice, aside from a relative inability to interpret waveforms properly, is not having a waveform that tells us how much effort the patient is actually doing, which is very difficult to infer from flow and airway pressure and so on. The future of esophageal pressure is ensuring safe spontaneous breathing and knowing if patients are breathing or not and knowing if they’re breathing way too much, which is really what drives our concerns about pendelluft and patient self-inflicted lung injury as well as under-assistance myotrauma and so forth. The exciting thing about esophageal pressure is the potential to more reliably monitor when the patient is passive or active and make good decisions accordingly.
Scott:
I like what you’re saying about the future of esophageal manometry, but I think we need to recognize the fact that it’s been around for a long time. I’m asking the folks in the room, why has esophageal manometry really never been a more mainstream approach? Why does it seem to be reemerging now, although we have papers that date back to the 1980s on the same exact concept? Is it that the technology just wasn’t there? An added point to that is that I still don’t find the equipment to be user-friendly.
Goligher:
I think that’s a huge issue. There are a number of ventilators with the ability to monitor esophageal pressure. In our ICU, for example, all of the ECMO patients have esophageal balloons placed. We use a ventilator that allows us to monitor the waveform directly on the screen, which I think facilitates things. More and more companies are catching on that it’s useful. But I agree, the actual mechanics of acquiring the signal have been challenging for a long time.
Scott:
So going forward, what will prevent us, 20 years from now, from talking about esophageal manometry and how it never really caught on in 2019? How do we get past this? What’s really the issue now? Is it the lack of available monitors in each facility? Is it the lack of training or understanding? What I don’t want is 20 years from now for us to be talking about esophageal manometry again like it’s something new or fresh. Why can’t we move forward?
MacIntyre:
Somebody made the point earlier today. Clinicians want things that they can act upon and I think that’s true here. We’ve been looking at the esophageal balloon and fascinated with the physiology, but it has rarely changed clinical decisions. Going back to Talmor’s study,3 the biggest problem to me was that they ended up with the same PEEP level in both arms of the study. I think where you’re going to see an esophageal balloon helping is where you’re going to have a different PEEP being driven by that. I was very disappointed in that second study because it seems to me that they did not focus on a population where a high esophageal pressure would drive the PEEP higher than a conventional PEEP-FIO2 table (e.g., the obese population). In going back to Fumagalli et al4 looking at adding PEEP according to esophageal pressure in obese subjects, the average PEEP level when they optimized it was 8 to 9 cm H2O higher, and yet the Pplat didn’t go up very much at all.
Scott:
Is what I’m hearing you say is that we can get the information but everybody will stand at the bedside and say, what now?
MacIntyre:
We say this all the time on rounds. One of the most common questions when somebody reports a value or wants to do a test should be: ‘is this going to change what you’re doing?’ And more often than not, the answer is ‘no’. So under those conditions why bother to go through the expense, time, hassle and so on. But now I’ll defend the esophageal balloon because I think there are places where it could be extraordinarily helpful and change decisions. We’ve been talking about obese patients. They say that Iowa is corn-fed but in North Carolina it’s pork – we’ve got obesity issues across the country. That’s at least one population where I think the esophageal balloon may be helpful.
*Hess:
I’ve put in hundreds of esophageal balloons, and I don’t think we can minimize the technical challenges of getting the balloon in, having it correctly positioned, and then knowing what to do with the information. I think it is clinically challenging to get these in and get them positioned correctly and then using the information appropriately.
Branson:
I agree with Dean [Hess], I’ve done hundreds of these over my career and esophageal manometry is incredibly instructive for bedside clinicians to see the physiology; there is a lack of understanding and interest. The clinicians want to know what does the evidence say on where I should set the tidal volume or the PEEP? All the guidelines they are bombarded with are probably overwhelming and trying to keep up with the current state of the art, but I think some of it is lack of understanding of physiology by the people at the bedside - whether they’re physicians, therapists, or nurses. This change to evidence-based practice, which emphasizes following guidelines and not necessarily understanding physiology, presents some challenges. If you look back there was a medical device, the Bicore monitor, that was created just to do esophageal manometry and it made it very easy, gave us the displays, gave us the calculations, but it failed commercially because not enough people saw it as valuable so it turned out not to be a viable product. That kind of tells you the status.
MacIntyre:
I’m almost reluctant to say what I’m about to say because I believe in physiology, but I remember Art Slutsky had a paper called the seduction of physiology.5 Basically, the point was that physiology is fascinating, can be very instructive, and should lead us down investigative pathways but should be used with caution as a major study endpoint. Going back to the ARDSnet trial in 2000,6 which I’m sure everyone here is familiar with, the physiology got a lot better in the people with larger tidal volumes and that’s because for at least a day or two the big tidal volumes probably did do some additional recruitment and the PO2 and compliance got better. But lo and behold, lurking in the background, was developing ventilator-induced lung injury that was going to kill those people. A great example of a fundamental disconnect between short-term physiology and outcome. Again, I really think physiology is important for understanding disease processes and guiding how we write guidelines, but I want to throw out that word of caution to be careful. Sometimes the price you pay for a small physiological benefit short over a short period of time turns out to be a lot more than you realize.
Walsh:
One of the things I think we’ve always tried to do is to look for a silver bullet, we look for one measurement to tell us the answer to PEEP titration. To Brady’s [Scott] point, we’ve done the same thing with CO2 elimination, we’ve used that to titrate PEEP (best CO2 elimination), that measurement is readily available on lots of ventilators and you don’t have to place a catheter, but it (CO2 elimination) also died over time and I don’t know why.
Blanch:
This is a clear example that, if we want to go to precise and personalized medicine, esophageal manometry will help some patients but not all. Then, the problem is to translate all this physiology at the bedside. Like you said Neil [MacIntyre], what does it mean a small improvement in oxygenation? Likely is physiologically more important an improvement in ventilatory efficiency. Bedsides, we need to evaluate the effect on these two measurements.
Goligher:
I was meeting with Art last week because we’re working on a trial design using physiology to select subjects, so I think he’s still being seduced by it despite that paper.5 He said to say hello, by the way.
MacIntyre:
It seduces all of us.
Goligher:
Yes, that’s why we’re here I guess. To build on your point, I believe the physiology is relevant where it’s mechanistically linked to the pathway that drives outcome. So with respect to lower tidal volume ventilation, oxygenation is not particularly relevant to the mechanism by which lowering tidal volume impacts outcome. On the other hand, oxygenation might be on the pathway that determines whether higher PEEP recruits the lung and relieves lung stress to improve outcome. The important thing is for us to understand what’s actually driving the outcome and then what markers physiologically will reflect that pathway. For example, the reason I’m excited about esophageal manometry in spontaneous breathing is because I really believe that insufficient or excessive expiratory effort drives diaphragm injury and that, in turn, drives clinically important outcomes. So potentially using the balloon or any other technique to monitor inspiratory effort could be a way of avoiding that problem and then improving outcome. We need to draw really clear line between what we’re monitoring and the mechanism that drives outcome. If you can connect those 2 dots you’ll get massive buy-in. But for esophageal manometry, to this point, we really haven’t been able to connect those 2 dots.
Branson:
Realizing there are a lot of differing practice around the table, in the ICU you last worked in for a year and were clinically active how many people had one patient in the ICU that had an esophageal monitor every day?
MacIntyre:
In the ICU, did you use it at least once?
Branson:
No, however many patients you have in your ICU, how many times did you have an esophageal catheter in a patient every day? Three, the guys from Toronto.
Scott:
We use it but we don’t use it every day.
Branson:
How many of you used it at least once a week in your ICU? Nobody. How about once a month? Five. How about less than once a month but still used it at all? Three. How about never? One. It’s just interesting in a group of experts to see who does and who doesn’t use it. I’m with Dean, I don’t think you can underestimate regardless of his experience or my experience, the average RT is very intimidated about placing these catheters.
Goligher:
I’m curious, with that experience you’re speaking to, in what percentage of patients would you say you couldn’t get measurements or couldn’t trust them?
*Hess:
I’d say very few, but there have been patients where I have spent an hour getting it in and positioned correctly.
Branson:
I think the technical challenge goes beyond that because it’s not just placing it but making sure it stays in position. You gave an excellent presentation, but how many average clinicians understand how much air has to go in the balloon? That was one of the advantages to the Bicore, that it maintained balloon volume. But all the ventilators do is display esophageal pressure, there’s no maintenance of the volume of the balloon. It’s more technically complex than we, in general, give it credence.
Smallwood:
Although I raised my hand at only using the esophageal balloon a handful of times, I must admit it was mostly an excuse to use higher PEEP. It was a larger kid coming into the ICU and we said, ‘hey let’s do something that can assuage our concerns about blowing this kid up’. So you put in an esophageal balloon and crank the PEEP up. I’m making light of my experience, but I think you see the point. Often we start with a piece of technology and then try to figure out how best to use it to improve mechanical ventilation. Has this been the case for esophageal manometry? I don’t know. But on the other hand, we can start with a problem and then work backward to find the optimal technology. In the context of asynchrony, we have a lot of options to detect what’s happening with our patients, and you spoke to a handful of them: electrical activity of the diaphragm, waveform analyses, whether automated or not, and esophageal balloon manometry. All of these offer a mechanism to assess asynchrony. Of these three options though, which one is the most attractive? One could make the case that it should be simply waveform analysis since this option requires no additional technology, or lines, or tubes. All you need is some software and the ventilator that your patient is already connected to. With all that said, I don’t want to throw away the esophageal manometer just yet. In history we see that whenever a technology becomes available to help us get a new view of our patient’s physiology it can take a lot of time before it’s use comes to the surface. Esophageal manometry has been around for at least 20 years, and that sounds like forever. But the time period between when the electrocardiogram was first discovered and when it was actually used in clinical practice was over 100 years. I just want to maintain some optimism for the technology as we diligently work towards understanding where this fits in, perhaps a more precise definition of the patient cohort who gets it is a start. That would be nice since then we hopefully don’t have these trials designed where everybody who’s ever seen a ventilator gets a probe when maybe only 5% of mechanically ventilated patients will turn out to have a benefit.
Pham:
I think one of the major challenges that could help esophageal manometry to progress would be to select proper conditions and patients that might benefit from it. Likely obese patients; I suppose any patients who have chest wall issues, those with abdominal hypertension, and maybe the most severe ARDS patients. Regarding technical challenges, when I arrived in Toronto in 2016 I had never seen an esophageal manometer or placed one; I was completely naïve. I saw they actually used it on a daily basis and was amazed that after some teaching all of the RTs were familiar with the technique: they insert the balloons, they don’t even ask, when the patient meets the criteria in the ICU they insert the balloon, do all the measurements and send them to us. Of course I helped with some insertions and did some myself and it was actually easier than I thought. I was kind of afraid of using it at first, but I think when everybody is trained, optimistic and wants to move the technique forward it creates this nice atmosphere to use it. And as with any technique the more you use it, the more you understand, the more you want to use it, and it creates a virtuous cycle.
Piraino:
One last comment, now that we have EIT in the ICU and RTs are putting that on, they’re realizing it’s a lot simpler than placing an esophageal balloon and now all of a sudden they’re asking, ‘can we put EIT on?’ and we should probably put the balloon in, we have a form that we fill out for all of our hypoxemic patients, but now they’re starting to ask for EIT before esophageal manometry. So although they’ve become very comfortable and competent at putting in the balloon they still, when they see something that’s slightly easier that gives them valuable information, they’re already gravitating towards it.
Pham:
We have an ARDS registry in Toronto which is filled in by the RTs. It looks like a lot, but a lot of the measurements are automated on a PDF document. You input the ventilator settings, then you insert the balloon, then they do the measurements at different levels of PEEP.
Dean R Hess PhD RRT FAARC is Managing Editor of Respiratory Care.
References
- 1.Luciani L. Esame comparativo dei metodi per registrare la pressione toracica e addominale. In: Delle oscillazioni della pressione intratoracica e intraddominale. Torino, Italy: Vicenzo Bona; 1877:2-18. [Google Scholar]
- 2.Buytendijk HJ. Oesophagusdruk en longelasticiteit. Dissertation, University of Groningen 1949.
- 3.Mead J, McIlroy MB, Selverstone NJ, Kriete BC. Measurement of intraesophageal pressure. J Appl Physiol 1955;7(5):491-495. [DOI] [PubMed] [Google Scholar]
- 4.Mead J, Gaensler EA. Esophageal and pleural pressures in man, upright and supine. J Appl Physiol 1959;14(1):81-83. [DOI] [PubMed] [Google Scholar]
- 5.Milic-Emili G, Petit JM. Relationship between endoesophageal and intrathoracic pressure variations in dog. J Appl Physiol 1959;14(4):535-537. [Google Scholar]
- 6.Milic-Emili J, Mead J, Turner JM. Topography of esophageal pressure as a function of posture in man. J Appl Physiol 1964;19(2):212-216. [DOI] [PubMed] [Google Scholar]
- 7.Milic-Emili J, Mead J, Turner JM, Glauser EM. Improved technique for estimating pleural pressure from esophageal balloons. J Appl Physiol 1964;19(2):207-211. [DOI] [PubMed] [Google Scholar]
- 8.Fry DL, Stead WW, Ebert RV, Lubin RI, Wells HS. The measurement of intraesophageal pressure and its relationship to intrathoracic pressure. J Lab Clin Med 1952;40(5):664-673. [PubMed] [Google Scholar]
- 9.Schilder DP, Hyatt RE, Fry DL. An improved balloon system for measuring intraesophageal pressure. J Appl Physiol 1959;14(6):1057-1058. [DOI] [PubMed] [Google Scholar]
- 10.Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA 2016;315(8):788-800. [DOI] [PubMed] [Google Scholar]
- 11.Niknam J, Chandra A, Adams AB, Nahum A, Ravenscraft SA, Marini JJ. Effect of a nasogastric tube on esophageal pressure measurement in normal adults. Chest 1994;106(1):137-141. [DOI] [PubMed] [Google Scholar]
- 12.Walterspacher S, Isaak L, Guttmann J, Kabitz H-J, Schumann S. Assessing respiratory function depends on mechanical characteristics of balloon catheters. Respir Care 2014;59(9):1345-1352. [DOI] [PubMed] [Google Scholar]
- 13.Akoumianaki E, Maggiore SM, Valenza F, Bellani G, Jubran A, Loring SH, et al. The application of esophageal pressure measurement in patients with respiratory failure. Am J Respir Crit Care Med 2014;189(5):520-531. [DOI] [PubMed] [Google Scholar]
- 14.Mauri T, Yoshida T, Bellani G, Goligher EC, Carteaux G, Rittayamai N, et al. Esophageal and transpulmonary pressure in the clinical setting: meaning, usefulness and perspectives. Intensive Care Med 2016;42(9):1360-1373. [DOI] [PubMed] [Google Scholar]
- 15.Mojoli F, Chiumello D, Pozzi M, Algieri I, Bianzina S, Luoni S, et al. Esophageal pressure measurements under different conditions of intrathoracic pressure: an in vitro study of second generation balloon catheters. Minerva Anestesiol 2015;81(8):855-864. [PubMed] [Google Scholar]
- 16.Yang Y-L, He X, Sun X-M, Chen H, Shi Z-H, Xu M, et al. Optimal esophageal balloon volume for accurate estimation of pleural pressure at end-expiration and end-inspiration: an in vitro bench experiment. Intensive Care Med Exp 2017;5(1):35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mojoli F, Iotti GA, Torriglia F, Pozzi M, Volta CA, Bianzina S, et al. In vivo calibration of esophageal pressure in the mechanically ventilated patient makes measurements reliable. Crit Care 2016;20(1):98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sun X-M, Chen G-Q, Huang H-W, He X, Yang Y-L, Shi Z-H, et al. Use of esophageal balloon pressure-volume curve analysis to determine esophageal wall elastance and calibrate raw esophageal pressure: a bench experiment and clinical study. BMC Anesthesiol 2018;18(1):21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baydur A, Behrakis PK, Zin WA, Jaeger M, Milic-Emili J. A simple method for assessing the validity of the esophageal balloon technique. Am Rev Respir Dis 1982;126(5):788-791. [DOI] [PubMed] [Google Scholar]
- 20.Lanteri CJ, Kano S, Sly PD. Validation of esophageal pressure occlusion test after paralysis. Pediatr Pulmonol 1994;17(1):56-62. [DOI] [PubMed] [Google Scholar]
- 21.Chiumello D, Consonni D, Coppola S, Froio S, Crimella F, Colombo A. The occlusion tests and end-expiratory esophageal pressure: measurements and comparison in controlled and assisted ventilation. Ann Intensive Care 2016;6(1):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Attinger EO, Monroe RG, Segal MS. The mechanics of breathing in different body positions. I. In normal subjects. J Clin Invest 1956;35(8):904-911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Attinger EO, Herschfus JA, Segal MS. The mechanics of breathing in different body positions. II. In cardiopulmonary disease. J Clin Invest 1956;35(8):912-920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Knowles JH, Hong SK, Rahn H. Possible errors using esophageal balloon in determination of pressure-volume characteristics of the lung and thoracic cage. J Appl Physiol 1959;14(4):525-530. [Google Scholar]
- 25.Ferris BG, Mead J, Frank NR. Effect of body position on esophageal pressure and measurement of pulmonary compliance. J Appl Physiol 1959;14(4):521-524. [Google Scholar]
- 26.Persson P, Ahlstrand R, Gudmundsson M, A de L, Lundin S. Detailed measurements of oesophageal pressure during mechanical ventilation with an advanced high-resolution manometry catheter. Crit Care 2019;23(1):217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Washko GR, O'Donnell CR, Loring SH. Volume-related and volume-independent effects of posture on esophageal and transpulmonary pressures in healthy subjects. J Appl Physiol (1985) 2006;100(3):753-758. [DOI] [PubMed] [Google Scholar]
- 28.Talmor D, Sarge T, Malhotra A, O’Donnell CR, Ritz R, Lisbon A, et al. Mechanical ventilation guided by esophageal pressure in acute lung injury. N Engl J Med 2008;359(20):2095-2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Beitler JR, Sarge T, Banner-Goodspeed VM, Gong MN, Cook D, Novack V, et al. Effect of titrating positive end-expiratory pressure (PEEP) With an esophageal pressure-guided strategy vs an empirical high PEEP-FiO2 strategy on death and days free from mechanical ventilation among patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA 2019;321(9):846-857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yoshida T, Amato MBP, Grieco DL, Chen L, Lima CAS, Roldan R, et al. Esophageal manometry and regional transpulmonary pressure in lung injury. Am J Respir Crit Care Med 2018;197(8):1018-1026. [DOI] [PubMed] [Google Scholar]
- 31.Mead J, Takishima T, Leith D. Stress distribution in lungs: a model of pulmonary elasticity. J Appl Physiol 1970;28(5):596-608. [DOI] [PubMed] [Google Scholar]
- 32.Slutsky AS, Ranieri VM. Ventilator-induced lung injury. N Engl J Med 2013;369(22):2126-2136. [DOI] [PubMed] [Google Scholar]
- 33.Loring SH, Topulos GP, Hubmayr RD. Transpulmonary pressure: the importance of precise definitions and limiting assumptions. Am J Respir Crit Care Med 2016;194(12):1452-1457. [DOI] [PubMed] [Google Scholar]
- 34.Grieco DL, Anzellotti GM, Russo A, Bongiovanni F, Costantini B, D’Indinosante M, et al. Airway closure during surgical pneumoperitoneum in obese patients. Anesthesiology 2019;131(1):58-73. [DOI] [PubMed] [Google Scholar]
- 35.Chen L, Del Sorbo L, Grieco DL, Shklar O, Junhasavasdikul D, Telias I, et al. Airway closure in acute respiratory distress syndrome: an underestimated and misinterpreted phenomenon. Am J Respir Crit Care Med 2018;197(1):132-136. [DOI] [PubMed] [Google Scholar]
- 36.Lai-Fook SJ, Rodarte JR. Pleural pressure distribution and its relationship to lung volume and interstitial pressure. J Appl Physiol (1985) 1991;70(3):967-978. [DOI] [PubMed] [Google Scholar]
- 37.Perlman CE, Lederer DJ, Bhattacharya J. Micromechanics of alveolar edema. Am J Respir Cell Mol Biol 2011;44(1):34-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gulati G, Novero A, Loring SH, Talmor D. Pleural pressure and optimal positive end-expiratory pressure based on esophageal pressure versus chest wall elastance: incompatible results. Crit Care Med 2013;41(8):1951-1957. [DOI] [PubMed] [Google Scholar]
- 39.Dornhorst AC, Leathart GL. A method of assessing the mechanical properties of lungs and air-passages. Lancet 1952;260(6725):109-111. [DOI] [PubMed] [Google Scholar]
- 40.Talmor D, Sarge T, O’Donnell CR, Ritz R, Malhotra A, Lisbon A, Loring SH. Esophageal and transpulmonary pressures in acute respiratory failure. Crit Care Med 2006;34(5):1389-1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gattinoni L, Chiumello D, Carlesso E, Valenza F. Bench-to-bedside review: chest wall elastance in acute lung injury/acute respiratory distress syndrome patients. Crit Care 2004;8(5):350-355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Loring SH, O’Donnell CR, Behazin N, Malhotra A, Sarge T, Ritz R, et al. Esophageal pressures in acute lung injury: do they represent artifact or useful information about transpulmonary pressure, chest wall mechanics, and lung stress? J Appl Physiol (1985) 2010;108(3):515-522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mutoh T, Guest RJ, Lamm WJ, Albert RK. Prone position alters the effect of volume overload on regional pleural pressures and improves hypoxemia in pigs in vivo. Am Rev Respir Dis 1992;146(2):300-306. [DOI] [PubMed] [Google Scholar]
- 44.Wiener-Kronish JP, Gropper MA, Lai-Fook SJ. Pleural liquid pressure in dogs measured using a rib capsule. J Appl Physiol (1985) 1985;59(2):597-602. [DOI] [PubMed] [Google Scholar]
- 45.Terragni P, Mascia L, Fanelli V, Biondi-Zoccai G, Ranieri VM. Accuracy of esophageal pressure to assess transpulmonary pressure during mechanical ventilation. Intensive Care Med 2017;43(1):142-143. [DOI] [PubMed] [Google Scholar]
- 46.Pelosi P, Goldner M, McKibben A, Adams A, Eccher G, Caironi P, et al. Recruitment and derecruitment during acute respiratory failure: an experimental study. Am J Respir Crit Care Med 2001;164(1):122-130. [DOI] [PubMed] [Google Scholar]
- 47.Hunter A, Eisma R, Lamb C. Thiel embalming fluid: a new way to revive formalin-fixed cadaveric specimens. Clin Anat N Anat 2014;27(6):853-855. [DOI] [PubMed] [Google Scholar]
- 48.Behazin N, Jones SB, Cohen RI, Loring SH. Respiratory restriction and elevated pleural and esophageal pressures in morbid obesity. J Appl Physiol (1985) 2010;108(1):212-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fumagalli J, Berra L, Zhang C, Pirrone M, Santiago R, Gomes S, et al. Transpulmonary pressure describes lung morphology during decremental positive end-expiratory pressure trials in obesity. Crit Care Med 2017;45(8):1374-1381. [DOI] [PubMed] [Google Scholar]
- 50.Beitler JR, Talmor D. Strategies to adjust positive end-expiratory pressure in patients with ARDS-reply. JAMA 2019;322(6):580-582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Loring SH, O’Donnell CR, Butler JP, Lindholm P, Jacobson F, Ferrigno M. Transpulmonary pressures and lung mechanics with glossopharyngeal insufflation and exsufflation beyond normal lung volumes in competitive breath-hold divers. J Appl Physiol (1985) 2007;102(3):841-846. [DOI] [PubMed] [Google Scholar]
- 52.Beitler JR, Majumdar R, Hubmayr RD, Malhotra A, Thompson BT, Owens RL. Volume delivered during recruitment maneuver predicts lung stress in acute respiratory distress syndrome. Crit Care Med 2016;44(1):91-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.MacIntyre NR. Lung protective ventilator strategies: beyond scaling tidal volumes to ideal lung size. Crit Care Med 2016;44(1):244-245. [DOI] [PubMed] [Google Scholar]
- 54.Amato MBP, Meade MO, Slutsky AS, Brochard L, Costa ELV, Schoenfeld DA, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med 2015;372(8):747-755. [DOI] [PubMed] [Google Scholar]
- 55.Yoshida T, Fujino Y, Amato MBP, Kavanagh BP. Fifty years of research in ARDS. Spontaneous breathing during mechanical ventilation. risks, mechanisms, and management. Am J Respir Crit Care Med 2017;195(8):985-992. [DOI] [PubMed] [Google Scholar]
- 56.Yoshida T, Uchiyama A, Matsuura N, Mashimo T, Fujino Y. Spontaneous breathing during lung-protective ventilation in an experimental acute lung injury model: high transpulmonary pressure associated with strong spontaneous breathing effort may worsen lung injury. Crit Care Med 2012;40(5):1578-1585. [DOI] [PubMed] [Google Scholar]
- 57.Yoshida T, Uchiyama A, Matsuura N, Mashimo T, Fujino Y. The comparison of spontaneous breathing and muscle paralysis in two different severities of experimental lung injury. Crit Care Med 2013;41(2):536-545. [DOI] [PubMed] [Google Scholar]
- 58.Bellani G, Grasselli G, Teggia-Droghi M, Mauri T, Coppadoro A, Brochard L, Pesenti A. Do spontaneous and mechanical breathing have similar effects on average transpulmonary and alveolar pressure? A clinical crossover study. Crit Care 2016;20(1):142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yoshida T, Torsani V, Gomes S, Santis RRD, Beraldo MA, Costa ELV, et al. Spontaneous effort causes occult pendelluft during mechanical ventilation. Am J Respir Crit Care Med 2013;188(12):1420-1427. [DOI] [PubMed] [Google Scholar]
- 60.Agostoni E, Mead J. Statics of the respiratory system [Internet]. In: Handbook of Physiology. Section 3: Respiration. Washington, DC: American Physiological Society; 1964:387-409. [Google Scholar]
- 61.Vries H. D, Jonkman A, Shi Z-H, Spoelstra-de Man A, Heunks L. Assessing breathing effort in mechanical ventilation: physiology and clinical implications. Ann Transl Med 2018;6(19):387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Jubran A, Tobin MJ. Pathophysiologic basis of acute respiratory distress in patients who fail a trial of weaning from mechanical ventilation. Am J Respir Crit Care Med 1997;155(3):906-915. [DOI] [PubMed] [Google Scholar]
- 63.Cabello B, Mancebo J. Work of breathing. Intensive Care Med 2006;32(9):1311-1314. [DOI] [PubMed] [Google Scholar]
- 64.Field S, Sanci S, Grassino A. Respiratory muscle oxygen consumption estimated by the diaphragm pressure-time index. J Appl Physiol 1984;57(1):44-51. [DOI] [PubMed] [Google Scholar]
- 65.Pham T, Telias I, Piraino T, Yoshida T, Brochard LJ. Asynchrony consequences and management. Crit Care Clin 2018;34(3):325-341. [DOI] [PubMed] [Google Scholar]
- 66.Vaporidi K, Babalis D, Chytas A, Lilitsis E, Kondili E, Amargianitakis V, et al. Clusters of ineffective efforts during mechanical ventilation: impact on outcome. Intensive Care Med 2017;43(2):184-191. [DOI] [PubMed] [Google Scholar]
- 67.Akoumianaki E, Lyazidi A, Rey N, Matamis D, Perez-Martinez N, Giraud R, et al. Mechanical ventilation-induced reverse-triggered breaths: a frequently unrecognized form of neuromechanical coupling. Chest 2013;143(4):927-938. [DOI] [PubMed] [Google Scholar]
- 68.Beitler JR, Sands SA, Loring SH, Owens RL, Malhotra A, Spragg RG, et al. Quantifying unintended exposure to high tidal volumes from breath stacking dyssynchrony in ARDS: the BREATHE criteria. Intensive Care Med 2016;42(9):1427-1436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Blanch L, Villagra A, Sales B, Montanya J, Lucangelo U, Luján M, et al. Asynchronies during mechanical ventilation are associated with mortality. Intensive Care Med 2015;41(4):633-641. [DOI] [PubMed] [Google Scholar]
- 70.Goligher EC, Brochard LJ, Reid WD, Fan E, Saarela O, Slutsky AS, et al. Diaphragmatic myotrauma: a mediator of prolonged ventilation and poor patient outcomes in acute respiratory failure. Lancet Respir Med 2019;7(1):90-98. [DOI] [PubMed] [Google Scholar]
- 71.Georgopoulos D, Prinianakis G, Kondili E. Bedside waveforms interpretation as a tool to identify patient-ventilator asynchronies. Intensive Care Med 2006;32(1):34-47. [DOI] [PubMed] [Google Scholar]
- 72.Graves C, Glass L, Laporta D, Meloche R, Grassino A. Respiratory phase locking during mechanical ventilation in anesthetized human subjects. Am J Physiol 1986;250(5):R902-R909. [DOI] [PubMed] [Google Scholar]
- 73.Petrillo GA, Glass L. A theory for phase locking of respiration in cats to a mechanical ventilator. Am J Physiol 1984;246(3):R311-R320. [DOI] [PubMed] [Google Scholar]
- 74.Simon PM, Habel AM, Daubenspeck JA, Leiter JC. Vagal feedback in the entrainment of respiration to mechanical ventilation in sleeping humans. J Appl Physiol (1985) 2000;89(2):760-769. [DOI] [PubMed] [Google Scholar]
- 75.Simon PM, Zurob AS, Wies WM, Leiter JC, Hubmayr RD, Jensen ML, Stroetz RW. Entrainment of respiration in humans by periodic lung inflations. Effect of state and CO(2). Am J Respir Crit Care Med 1999;160(3):950-960. [DOI] [PubMed] [Google Scholar]
- 76.Schepens T, Goligher EC. Lung- and diaphragm-protective ventilation in acute respiratory distress syndrome: rationale and challenges. Anesthesiology 2019;130(4):620-633. [DOI] [PubMed] [Google Scholar]
- 77.Goligher EC, Fan E, Herridge MS, Murray A, Vorona S, Brace D, et al. Evolution of diaphragm thickness during mechanical ventilation: Impact of inspiratory effort. Am J Respir Crit Care Med 2015;192(9):1080-1088. [DOI] [PubMed] [Google Scholar]
- 78.Goligher EC, Dres M, Fan E, Rubenfeld GD, Scales DC, Herridge MS, et al. Mechanical ventilation-induced diaphragm atrophy strongly impacts clinical outcomes. Am J Respir Crit Care Med 2018;197(2):204-213. [DOI] [PubMed] [Google Scholar]
- 79.Chen L, Chen G-Q, Shore K, Shklar O, Martins C, Devenyi B, et al. Implementing a bedside assessment of respiratory mechanics in patients with acute respiratory distress syndrome. Crit Care 2017;21(1):84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Devlin JW, Skrobik Y, Gélinas C, Needham DM, Slooter AJC, Pandharipande PP, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med 2018;46(9):e825-e873. [DOI] [PubMed] [Google Scholar]
- 81.Pletsch-Assuncao R, Caleffi Pereira M, Ferreira JG, Cardenas LZ, Albuquerque AD, Carvalho C. D, Caruso P. Accuracy of invasive and noninvasive parameters for diagnosing ventilatory overassistance during pressure support ventilation. Crit Care Med 2017;46(6):1. [DOI] [PubMed] [Google Scholar]
- 82.Chiumello D, Carlesso E, Cadringher P, Caironi P, Valenza F, Polli F, et al. Lung stress and strain during mechanical ventilation for acute respiratory distress syndrome. Am J Respir Crit Care Med 2008;178(4):346-355. [DOI] [PubMed] [Google Scholar]
- 83.The Acute Respiratory Distress Syndrome Network, Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, Wheeler A. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 2000;342(18):1301-1308. [DOI] [PubMed] [Google Scholar]
- 84.Mercat A, Richard J-C, Vielle B, Jaber S, Osman D, Diehl J-L, et al. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA 2008;299(6):646-655. [DOI] [PubMed] [Google Scholar]
- 85.Bergez M, Fritsch N, Tran-Van D, Saghi T, Bounkim T, Gentile A, et al. PEEP titration in moderate to severe ARDS: plateau versus transpulmonary pressure. Ann Intensive Care 2019;9(1):81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mentzelopoulos SD, Roussos C, Zakynthinos SG. Prone position reduces lung stress and strain in severe acute respiratory distress syndrome. Eur Respir J 2005;25(3):534-544. [DOI] [PubMed] [Google Scholar]
- 87.Riad Z, Mezidi M, Subtil F, Louis B, Guérin C. Short-term effects of the prone positioning maneuver on lung and chest wall mechanics in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med 2018;197(10):1355-1358. [DOI] [PubMed] [Google Scholar]
- 88.Mezidi M, Parrilla FJ, Yonis H, Riad Z, Böhm SH, Waldmann AD, et al. Effects of positive end-expiratory pressure strategy in supine and prone position on lung and chest wall mechanics in acute respiratory distress syndrome. Ann Intensive Care 2018;8(1):86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Owens RL, Campana LM, Hess L, Eckert DJ, Loring SH, Malhotra A. Sitting and supine esophageal pressures in overweight and obese subjects. Obesity (Silver Spring) 2012;20(12):2354-2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Jones RL, Nzekwu M-M. The effects of body mass index on lung volumes. Chest 2006;130(3):827-833. [DOI] [PubMed] [Google Scholar]
- 91.Yap JC, Watson RA, Gilbey S, Pride NB. Effects of posture on respiratory mechanics in obesity. J Appl Physiol 1995;79(4):1199-1205. [DOI] [PubMed] [Google Scholar]
- 92.Suratt PM, Wilhoit SC, Hsiao HS, Atkinson RL, Rochester DF. Compliance of chest wall in obese subjects. J Appl Physiol 1984;57(2):403-407. [DOI] [PubMed] [Google Scholar]
- 93.Hedenstierna G, Santesson J. Breathing mechanics, dead space and gas exchange in the extremely obese, breathing spontaneously and during anaesthesia with intermittent positive pressure ventilation. Acta Anaesthesiol Scand 1976;20(3):248-254. [DOI] [PubMed] [Google Scholar]
- 94.Pirrone M, Fisher D, Chipman D, Imber DA, Corona J, Mietto C, et al. Recruitment maneuvers and positive end-expiratory pressure titration in morbidly obese ICU patients. Crit Care Med 2016;44(2):300-307. [DOI] [PubMed] [Google Scholar]
- 95.Sharp JT, Henry JP, Sweany SK, Meadows WR, Pietras RJ. Effects of mass loading the respiratory system in man. J Appl Physiol 1964;19(5):959-966. [DOI] [PubMed] [Google Scholar]
- 96.Fumagalli J, Santiago RRS, Teggia Droghi M, Zhang C, Fintelmann FJ, Troschel FM, et al. Lung recruitment in obese patients with acute respiratory distress syndrome. Anesthesiology 2019;130(5):791-803. [DOI] [PubMed] [Google Scholar]
- 97.Tobin MJ. Remembrance of weaning past: the seminal papers. Intensive Care Med 2006;32(10):1485-1493. [DOI] [PubMed] [Google Scholar]
- 98.Ishaaya AM, Nathan SD, Belman MJ. Work of breathing after extubation. Chest 1995;107(1):204-209. [DOI] [PubMed] [Google Scholar]
- 99.Sklar MC, Burns K, Rittayamai N, Lanys A, Rauseo M, Chen L, et al. Effort to breathe with various spontaneous breathing trial techniques: a physiologic meta-analysis. Am J Respir Crit Care Med 2017;195(11):1477-1485. [DOI] [PubMed] [Google Scholar]
- 100.Jubran A, Grant BJB, Laghi F, Parthasarathy S, Tobin MJ. Weaning prediction esophageal pressure monitoring complements readiness testing. Am J Respir Crit Care Med 2005;171(11):1252-1259. [DOI] [PubMed] [Google Scholar]
References
- 1.Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA 2016;315(8):788-800. [DOI] [PubMed] [Google Scholar]
- 2.Morais CCA, Koyama Y, Yoshida T, Plens GM, Gomes S, Lima CAS, et al. High positive end-expiratory pressure renders spontaneous effort noninjurious. Am J Respir Crit Care Med 2018;197(10):1285-1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beitler JR, Sarge T, Banner-Goodspeed VM, Gong MN, Cook D, Novack V, et al. Effect of titrating positive end-expiratory pressure (peep) with an esophageal pressure-guided strategy vs an empirical high PEEP-FIO2 strategy on death and days free from mechanical ventilation among patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA 2019;321(9):846-857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fumagalli J1, Santiago RRS, Teggia Droghi M, Zhang C, Fintelmann FJ, et al. Lung recruitment in obese patients with acute respiratory distress syndrome. Anesthesiology 2019;130(5):791-803. [DOI] [PubMed] [Google Scholar]
- 5.Slutsky AS. Improving outcomes in critically ill patients: the seduction of physiology. JAMA 2009;302(18):2030-2032. [DOI] [PubMed] [Google Scholar]
- 6.Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, Wheeler A. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 2000;342(18):1301-1308. [DOI] [PubMed] [Google Scholar]