Abstract
Background
Immunization to prevent infectious diseases is a core strategy to improve childhood health as well as survival. It remains a challenge for some African countries to attain the required childhood immunization coverage. We aim at identifying individual barriers confronting parents/caretakers, providers, and health systems that hinder childhood immunization coverage in Sub-Saharan Africa.
Method
This systematic review searched PubMed/MEDLINE, Web of Science and EMBASE. We restricted to published articles in English that focused on childhood immunization barriers in sub-Saharan Africa from January 1988 to December 2019. We excluded studies if: focused on barriers to immunization for children in other regions of the world, studied adult immunization barriers; studies not available on the university library, they were editorial, reports, reviews, supplement, and bulletins. Study designs included were cross-sectional, second-hand data analysis; and case control.
Results
Of the 2652 items identified, 48 met inclusion criteria. Parents/caretakers were the most common subjects. Nine articles were of moderate and 39 were of high methodological quality. Nine studies analyzed secondary data; 36 used cross-sectional designs and three employed case control method. Thirty studies reported national immunization coverage of key vaccines for children under one, eighteen did not. When reported, national immunization coverage of childhood vaccines is reported to be low. Parents/caretaker’ barriers included lack of knowledge of immunization, distance to access point, financial deprivation, lack of partners support, and distrust in vaccines and immunization programs. Other associated factors for low vaccine rates included the number of off-springs, lifestyle, migration, occupation and parent’s forgetfulness, inconvenient time and language barrier. Barriers at health system level cited by healthcare providers included limited human resources and inadequate infrastructures to maintain the cold chain and adequate supply of vaccines.
Conclusion
In this review we identified more thoroughly the parents/caretakers’ barriers than those of providers and health systems. Factors that influenced decisions to get children vaccinated were mainly their gender, beliefs, socio-culture factors in the communities in which they live. Thus it is vital that immunization programs consider these barriers and address the people and societies in their communities across sub-Saharan Africa.
Keywords: Barriers, Childhood, Immunization, Sub-Saharan Africa
Background
Immunization is a protective measure against infectious diseases [1]. Childhood immunization remains one of the highest impact public health interventions, reducing infectious diseases-related morbidly and mortality of children at a low cost [2]. It is a core child survival strategy and is demonstrated to avert more than 1·2 million child deaths each year [3, 4]. It is a key strategy towards attaining Sustainable Development Goal (SDG) number 3, namely the reduction of under-five mortality to less than 25/1000 live births by 2013 [5]. Despite these gains, vaccine-preventable diseases remain a major cause of child illnesses and deaths, particularly in low-income countries [6].
Africa has the highest under-five mortality rate of the entire world and accounts for 40% of the total deaths in this age group. This is mainly due to vaccine-preventable diseases [7]. Over the past few decades, African immunization programs have made progress, yet coverages remains low for some recommended childhood vaccines. In 2014, it was reported that only Zimbabwe among the Sub-Saharan region was estimated to have met the Global Vaccine Action Plan threshold of 80% or higher coverage of diphtheria–tetanus-pertussis vaccine (DTP3), a benchmark used to measure performance of routine vaccine delivery system [8]. In 2016, one in five African children goes without lifesaving vaccines [9]. Most African countries are unable to reach the most vulnerable children populations in remote and rural communities [5, 10]. Studies [1–3, 7, 11–54] conducted in Africa have attempted to elucidate potential barriers that lead to low uptake and none-completion of immunization series. Previous review [55] exploring reasons related to non-vaccination and under-vaccination of children in low- and middle-income countries categorized factors into major themes: Immunization systems; communication and information; family characteristics and parental attitudes/knowledge. However, it noted the lack of peer reviewed literature in Central Africa. Another review [56] investigated factors associated with incomplete or delayed vaccination across countries. Despite its potential importance, it did not categorize findings into major domains, as policy implication for each might be different.
This systematic review aims at identifying relevant studies and summarizing major barriers confronting health systems, providers, and caregivers that hinder immunization coverage in sub-Saharan Africa. The results of this review will add to existing knowledge of the problem, and guide policy makers to improve immunization programs in sub-Saharan Africa, especially in those countries where the included studies had been conducted; and also to provide useful information for further research on these problems.
Methods
Search strategy and study selection
The study employed Preferred Reporting Items for Systematic Reviews and Meta- Analysis (PRSMA) guidelines [57]. We performed electronic searches of articles included in this systematic review from the Web of Science, PubMed/Medline and EMBASE from January, 1988 to December, 2019. We combined the following terms: (child or children or childhood or infant or baby or newborn), and (immunization or immunisation or vaccination or vaccine or immunity), and (barrier or hesitant or refuse or refusal or delay or denial or denier or denied or concern or reason or doubt “non-acceptance” or incomplete or obstacle or constraint), and (“Sub Saharan Africa” or Angola or Benin or Botswana or “Burkina Faso” or Burundi or “Cabo Verde” or Cameroon or “Central African Republic” or Chad or Comoros or Congo or “Cote d’Ivoire” or “Equatorial Guinea” or Eritrea or Ethiopia or Gabon or Gambia or Ghana or Guinea or “Guinea- Bissau” or Kenya or Lesotho or Liberia or Madagascar or Malawi or Mali or Mauritania or Mauritius or Mozambique or Namibia or Niger or Nigeria or Rwanda or Senegal or Sierra Leone or Somalia or “South Africa” or “South Sudan” or Sudan or Tanzania or Togo or Uganda or Zambia or Zimbabwe) [See supplementary materials 1].
We restricted to published articles in English that focused on childhood immunization barriers, conducted in Sub-Saharan Africa from January 1988 to December 2019. Articles were excluded if: (i) focused on barriers to immunization for children in other regions of the world, (ii) studied adult immunization barriers (iii) published before December, 1988 and beyond December, 2019; (iv) they were editorials, (v) reports, (vi) review articles, (vii) supplement articles, (vii) bulletins and (ix) studies not available on the university library. We included only observational studies in this systematic review.
Data analysis
Search result items were uploaded into EndNote X7 library. Duplicates were removed. JBB and DQ did the initial screening (title and abstract) and full texts of articles based on the inclusion and exclusion criteria. We resolved disagreements with third review (FO). The study employed narrative synthesis. The author uses the following approaches: tabulation and thematic analysis. The analysis focus on thematically grouping the barriers identified in the included studies. Researchers formulated table to capture descriptive information and data for each include study. This includes author, year, geographical location and number of countries included in a study; participants and demographic; study design; reported national immunization coverage, data source, date; study quality; and key reported barriers. JBB synthesized data and created table with input from LC and SX. JBB and LC classified reported barriers into three major categories: barriers confronting the parents/caretakers, those specific to the health system, and those linked to the providers. Discrepancies were resolved by consensus after discussions.
Study methodological quality
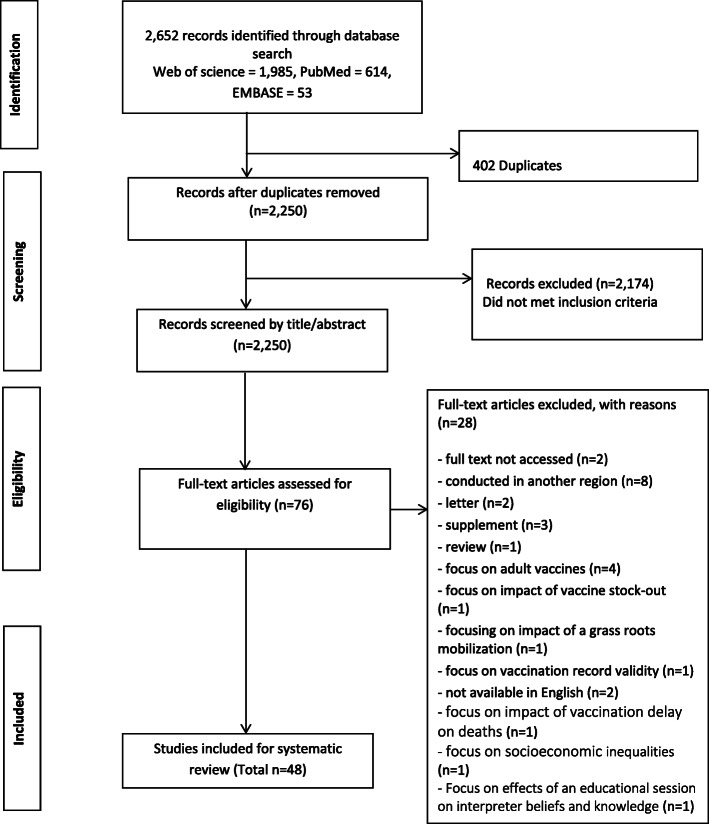
JBB and DQ assessed articles for methodological quality independently based on modified tool designed to assess quantitative and qualitative studies used in a similar study published elsewhere [58]. [See supplementary materials 2] It included a range of items from 1 to 14. Each item scores one point. Based on the scores, we grouped articles into three: low, moderate and high; articles scored 12 points and above were considered high methodological quality, moderate 8 to11 points,7 points and below were low. If ratings differed, we discussed the article in an effort to arrive at a consensus (Fig. 1).
Fig. 1.
Study selection
Results
Our database searches yielded 2652 records. 2250 records were screened by title and abstract after duplicates removed; 76 full-text articles assessed for eligibility. Forty-eight articles met all inclusion criteria for this study; 28 articles were excluded for various reasons. [See supplementary materials 3] Nine articles employed second-hand data analysis [7, 12, 18, 27, 37, 40–42, 47]; thirty-six used cross-sectional design [1–3, 11, 13–17, 19, 21–26, 28–36, 38, 39, 42, 45, 46, 48–51, 53, 54] and three used case-control study [20, 43, 44]. All described studies were conducted on Africa populations (103,655 adults and 76,327 children). Forty-seven articles focus on identifying barriers to general childhood vaccination 0–59 months [1–3, 7, 11–17, 19–54] in the following countries: Uganda, Ethiopia, Kenya, Sudan, Nigeria, Gabon, Cameroon, South Africa, Tanzania, Burkina Faso, Togo, Ghana, Malawi and few unspecified countries in Sub-Saharan. One critically examined barriers specific to vaccination doses at birth 0 – 1 day [18] in the Gambia. Thirty articles reported national immunization coverage [1, 2, 7, 11–16, 20–25, 28, 29, 32, 34, 35, 38–40, 43–46, 49, 50, 52–54], eighteen did not [3, 17–19, 22, 24, 26, 27, 30, 31, 33, 36, 37, 41, 42, 47, 48, 51]. 39 articles were classed as high and 9 were moderate methodological quality. We split results into three sections – parental barriers, health system barriers, and providers’ barriers. 8 studies examined all – parental/caretakers, health systems and providers’ barriers [3, 11, 13, 16, 43, 45, 48, 52]; 21 studies examined parental/caretakers and health system barriers [1, 2, 14, 15, 18, 19, 22, 23, 25, 29, 31–33, 35, 38, 44, 47, 49–51, 53]; 18 studies only looked at parental//caretakers barriers [7, 12, 17, 20, 21, 24, 26–28, 34, 36, 37, 39, 42, 46, 54] and one study examined parental and providers’ barriers. Several Sub-Saharan countries were reported to have low childhood immunization coverage with variations across the region. Nigeria reported lowest with 12·7% in 2013 and Ethiopia highest with 88% in 2013. See summary table for studies’ characteristics and key findings (Table 1).
Table 1.
Summary of studies’ characteristics and key findings
| Author, year, geographical location and number of countries included in the study | Participants and demographic | Study design | Reported national immunization coverage, Data source, Date | Quality | Key childhood immunization reported barriers | ||
|---|---|---|---|---|---|---|---|
| Parental/caretakers barriers | Health systems barriers | Providers barriers | |||||
| Tadesse et al. [1], 2009 Ethiopia East Africa, 1 | 126 adults | Cross-sectional | 38·5% National health survey of Ethiopia, 2006 | Moderate | Misunderstanding of side effects, busy with seasonal farm work | Absence of electricity to maintain the cold chain | |
| Obasoha et al. [2], 2018 Nigeria West Africa, 1 | 215 mothers | Cross-sectional | 25%, World Health Organization, Global Immunization Vision and Strategies, 2013 | High | Unaware of the need of immunization, lack of information, fear of side effect | Vaccines not available, vaccinators absence, long distance to cover | |
| Malande et al. [3], 2014 Uganda East Africa, 1 | 311 caretakers/child pairs | Cross -sectional | Not reported | High | Language barrier, less support from husband | Vaccine stock outs, difficult terrain and poor road network, inadequate transportation means, poor working condition of vaccine fridges, inadequate staff, long distance, transportation difficulties | Lack of knowledge of vaccines adverse effects |
| Wiysonge et al. [7], 2012 Sub-Saharan Africa countries, 24 | 27,094 children aged 12–23 month | Second-hand data Analysis | 71%, WHO (2010); vaccine preventable diseases: monitoring syatem-2010 | High | poor households, high illiteracy rates, lack of vaccines information, poor health seeking behaviors (Not going for ANC visit) | ||
| Tefera et al. [11], 2018 Ethiopia East Africa, 1 | 540 mothers with children aged between 12 and 23 months | Cross -sectional | 86%,WHO/UNICEF Immunization coverage,2015 | High | fear of side reactions, lack of information, being too busy, place/time being unknown, long waiting time, | vaccinators were absent, vaccines were not available, limited health facilities, vaccine site being too far | |
| Porth et al. [12], 2019 Ethiopia East Africa, 1 | 2722 children | Second-hand data Analysis | 39%, Ethiopia Demographic and health survey, 2016 | High | Negative perception of vaccines, religion, waiting too long | limited operating hours, clinic distance | |
| Kiptoo et al. [13], 2015 Kenya East Africa, 1 | 298 mothers/guardians | Cross - sectional | 86%, Kenya Expanded program on immunization, 2009 | High | lack of knowledge, earning less, many siblings | Inadequate health facilities, long distance for out-reach service | |
| Cockcroft et al. [14], 2014 Nigeria West Africa, 1 | 2836 children | Cross-sectional | 42%, Nigeria Demographic and Health Survey, 2013 | High | Misconception about vaccines, fear of side effect, negligence, being busy with other household work | Lack of vaccines | |
| Nolna et al. [15], 2018 ameroonWest Africa, 1 | 1134 caretakers | Cross-sectional | 82%, WHO-UNICEF estimates of DPT3 coverage, 2017 | High | Lack of money, lack of knowledge of vaccines importance, busy with other seasonal work | Shortage of health personnel, inadequate means of transportation | |
| Zewdie et al. [16], 2016 Ethiopia East Africa, 1 | 28 mothers | Cross-sectional | 88%, Ethiopia National immunization survey, 2013 | Moderate | Lack of information, lack of support from male partners, high workload, fear of mistreatment and lack of cooperation from service providers | Poor arrangement and coordination of immunization services, vaccines stock out, lack of viable defaulter tracking system | Inadequate home visit, lack of commitment, poor counseling skills |
| Babirye et al. [17], 2011 Uganda East Africa, 1 | 1000 adults | Cross-sectional | Not reported | High | male partner non-supportive, Lack of clothing, lack of money for vaccine related cost, lack of trust in immunization, fear of associated side effects, less education | ||
| Miyahara et al. [18], 2016 Gambia West Africa, 1 | 50,455 residents including children | Second-hand data Analysis | Not reported | High | living in urban and peri-urban settings, ethnicity, low maternal education, life style | use of multi-dose vails with limited time, long distance | Use of multi-dose vails with limited time |
| Pertet et al. [19], 2018 Kenya East Africa, 1 | 515 mothers | Cross-sectional | Not reported | High | Movement of the whole family (migration) | Lack of vaccines, difficult to access the health facility due to bad terrines | |
| Yenit et al. [20], 2018 Ethiopia East Africa, 1 | 308 mothers | Case-control study | 39%, Ethiopian Demographic and Health Survey, 2016 | High | Delivery at home, lack of antenatal and postnatal care visit, miss conception about vaccines, | ||
| Tugumisirize et al. [21], 2002 Uganda East Africa, 1 | 408 caretakers | Cross-sectional | 29%, Uganda Demographic and Health Survey, 1995 | High | Fear of rude health workers, being busy, low level of formal education, fear of side effects, perceived contradictions, | Long distance | |
| Babalola S [22]., 2011 Nigeria West Africa, 1 | 882 women | Cross-sectional | Not reported | High | Lack of knowledge about immunization schedule and sources, spouses disapproval of immunization, myth and rumors about side effects, mothers too busy, religious and cultural beliefs, home delivery | Vaccines unavailability, Long distance | |
| Oladokun et al. [23], 2010 Nigeria West Africa, 1 | 248 mothers | Cross-sectional | 12·7% National immunization survey, 2003 | High | Religion, low mother’s education, mothers not being aware of additional doses | Non-availability of vaccines, | |
| Schwarz et al. [24], 2009 Gabon West Africa, 1 | 262 mothers | Cross-sectional | Not reported | Moderate | feeling ashamed of poverty-associated reasons such as poorly cloth child or dirty, lack of knowledge, | Transportation cost, long distance | |
| Ismail et al. [25], 2014 Sudan East Africa, 1 | 213 children | Cross-sectional | 60%, Federal Ministry of Health, 2005 | High | lack of knowledge,, mothers too busy, many siblings, fear of side effect | Vaccinators absence, vaccine stock out, long distance | |
| Rees et al. [26], 1991 South Africa South Africa, 1 | 315 women | Cross-sectional | Not reported | High | low literacy level of mothers | Long distance to reach facility | |
| Nadella et al. [27], 2019 Tanzania East Africa, 1 | 31,999 children | Secondary data analysis | Not reported | High | Parents not educated, mothers not attending ANC, delivery at home, poor household | ||
| Meleko et al. [28], 2017 Ethiopia East Africa, 1 | 322 mothers/caretakers | cross-sectional | 24.3% Ethiopia Demographic Health Survey (EDHS), 2011 | High | Low parental educational level, delivery at home, parents not utilizing maternal health care services. Lack of knowledge | ||
| Itimi et al. [29], 2012 Nigeria west Africa, 1 | 558 women | cross-sectional | 23% Nigeria Demographic and Health Survey, 2008 | High | Adverse rumor about childhood immunization | Inadequate health personnel (Vaccinators) | |
| Kagoné et al. [30], 2018 Burkina Faso West Africa, 1 | Not stated | cross-sectional | Not reported | Moderate | Migration, mothers being busy, poor interaction between women and health workers, potential adverse events, and lack of information. | Geographic (hard to reach arears) | Not open multi-dose vails unless a critical number of children are present |
| Tobin-West et al. [31], 2012 Nigeria West Africa, 1 | 1560 mothers/caregivers | cross-sectional | Not reported | High | Long waiting time, belief in the efficacy of traditional medicines as an alternative to immunization, poor rapport with health workers, | Frequent shortage of vaccine | |
| Braka et al. [32], 2011 Uganda East Africa, 1 | 136 caretakers | cross-sectional | 80% W H O Immunization profile—Uganda 1980–2008, 2010 | High | Misconceptions, adverse effects experience, providers’ bad attitudes | Inadequate staff at health center level, poor storage facilities for vaccines, | |
| Ambe et al. [33], 2001 Nigeria West Africa, 1 | 500 mothers | cross-sectional | Not reported | High | Parents don’t have trust in vaccines, parents are abused in hospitals, husband refused/not supportive | Vaccines not available | |
| Tadesse et al. [34], 2009 Ethiopia East Africa, 1 | 226 children | cross-sectional | 49.9% Federal Ministry of Health Ethiopia, 2006 | High | Poor knowledge about immunization, mother’s negative perceptions, low monthly income of parents | ||
| Jani et al. [35], 2008 Mozambique South Africa, 1 | 668 mothers | cross-sectional | 80% Expanded program on immunization, 1998 | High | Low education level of mothers, long waiting time for vaccination, parent’s forgetfulness, migration, concomitant treatment by traditional healers | Vaccines shortage, Inadequate health workers (Vaccinators) | |
| Eng et al. [36], 1991 Togo West Africa, 1 | 110 mothers/caretakers | cross-sectional | Not reported | Moderate | Lack of knowledge, parent’s forgetfulness, health workers being aggressive, long waiting time, laziness, lack of information about vaccines, low income of parents | Long distance to health facilities | |
| Landoh et al. [37], 2016 Togo West Africa, 1 | 2067 children (12 to 59 months) | Secondary data analysis | Not reported | High | Residence of mother (Muslims dominated), non-schooled mothers, being a single mother, negative cultural beliefs | ||
| Legesse et al. [38], 2015 Ethiopia East Africa, 1 | 591 children 12 to 23 months and their mothers | cross-sectional | 36.5% Ethiopia Demographic Health Survey (EDHS), 2011 | High | Lack of knowledge, lack of information, low family income, low education level of parents, low maternal health care utilization, fear of adverse reactions, lack of trust on immunization, male partners non supportive | Poor quality of health information regarding immunization, Long distance to health facilities | |
| Wemakor et al. [39], 2018 Ghana West Africa, 1 | 322 children and their mothers | cross-sectional | 77% Ghana Demographic and Health Survey 2014 | Community of residence of mothers, lack of knowledge, | |||
| Adedokun1et al [40], 2017 Nigeria West Africa, 1 | 5754 children aged 12–23 months | Secondary data analysis | 81.5% Federal Ministry of Health Nigeria, 2011 | Moderate | Mothers being illiterate, lack of information about immunization, mothers not attending ANC, delivery at home, economically dis advantage mothers, difficulty getting to health facility due to bad terrines | ||
| Chidiebere et al. [41], 2014 Nigeria West Africa, 1 | 34,596 women | Secondary data analysis | Not reported | High | Lack of information about immunization, fear of side-effects, delivery at home, place of residence | Immunization centers too far | |
| Ekouevi et al. [42], 2018 Togo West Africa, 1 | 1128 children aged 12–23 months | cross-sectional | Not reported | High | Mothers not educated, low income, poor road conditions,, | Lack of means of transportation, Long distance to health center | |
| Tadess et al. [43], 2017 Ethiopia East Africa, 1 | 630 mothers/caretakers | Case control | 79% Ethiopian Health Sector Transformation Plan (HSTP), 2009 | High | Inaccessible health facility, poor motivation, unfavorable attitude and bad treatment of health workers, lack of logistics, inconvenient immunization time, inadequate information about immunization | Vaccines shortages | Inadequate communication skills, lack of willingness and restricted vaccine open policy, |
| Negussie et al. [44], 2016 Ethiopia East Africa, 1 | 548 children aged 12 to 23 months | Case control | 24% Ethiopia Demographic and Health Survey, 2011 | High | Lack of knowledge about immunization benefits, mother’s negative perception of vaccine side effects, migration of mothers | Unavailability of vaccines | |
| Bosu et al. [45], 1997 Ghana West Africa, 1 | 469 mothers | Cross sectional | 43% Ministry of Health Ghana Maternal and Child Health and Family Planning. Annual Report, 1992 | High | Poor knowledge about immunization, financial difficulties, long waiting times,, attitude of service providers and fear of side-effects | Lack of suitable venues and furniture at outreach clinics, and weak inter-sectoral collaboration, transport difficulties | Poorly motivated service providers |
| Desgrées du Loû et al. [46], 1994 Senegal West Africa, 1 | 6078 Mothers/caretakers | Cross sectional | 51% WHO/EPI/CEIS/93.1 (summary for the WHO African Region) 1990 | Moderate | children in large compound with large number of children. | Distance between the child and the health center, difficult geographical terrain | |
| Sato R [47]., 2019 Nigeria West Africa, 1 | 28,085 children | Secondary data analysis | Not reported | Moderate | Have no faith in immunization, lack of awareness of the need for immunization, poor household | Shortage of vaccine, limited health centers immunization point is too far/inconvenient | |
| Akwataghibe, N. N. et al. [48], 2019 Nigeria West Africa, 1 | 215 children, | Cross sectional | Not reported | High | Ethnicity, culture, household decision making, and gender relations; lack of knowledge and awareness of the value of immunization, negative beliefs and attitudes toward immunization; past experiences with immunization, migration | shortage of health workers, unavailability of vaccines at scheduled times; Inadequate electrical power supply to keep the vaccine cold chain at facilities, long distances for mothers in hard-to-reach areas | Reminders not sent on time about routine immunization or outreach days |
| Yismaw, A. E. et al. [49], 2019 Ethiopia East Africa, 1 | 301 mothers/caretakers | cross-sectional | 86% Federal Ministry of Health (2010) | High | Lack of Knowledge of next visit; and lack of knowledge about the benefits of vaccination | long distances to reach nearby health facilities | |
| Ntenda P [50]., 2019 Malawi East Africa, 1 | 3111 children and mothers | Cross-sectional | 76% WHO (2015) | High | Children born to mothers without education, children poor households, mothers with many sibling, children whose delivery occurred at home, | Inadequate health facility for vaccination, long distances to reach nearby health facilities | |
| Okenwa, U. J. et al. [51], 2019 Nigeria West Africa, 1 | 344 mothers and their infant | Cross-sectional | Not reported | High | Lack of awareness on timing of valid vaccine, | Vaccine stock-out at the immunization site | |
| Mthiyane, T. N et al. [52], 2019 South Africa South Africa 1 | 847 eligible children aged 12–59 months | Secondary data analysis | 66% WHO/UNICEF (2015) | High | Low household monthly income, unfriendly health workers, | Vaccine shortage; long distance and transportation costs to reach the clinic for immunization | Low level of education of the primary caregiver, |
| Mekonnen, A. G. et al. [53], 2019 Ethiopia East Africa, 1 | 566 children aged 12–23 months and their mothers/caregivers | Cross sectional | 39% Ethiopian demographic health survey report (2016) | High | Forgotten appointment date, the experience of child sickness with previous vaccination, and disrespectful behavior of health professionals | Long distance to the clinic | |
| Ibraheem, R. et al. [54], 2019 Nigeria West Africa, 1 | 480 mother-infant | cross-sectional | 53% Nigeria immunization coverage survey (2016) | High | Lack of antenatal care visit, vaccination on weekend/public holidays lower educational level | ||
Parental/caretaker barriers
In this systematic review, several cited parental/caretaker’ barriers were modifiable (knowledge, misconception, trust, delivery at home, long waiting time, providers’ hostility, parent’s forgetfulness, inconvenient time and language barrier). Parental/caretaker barriers are factors that impede mothers/caretakers progress in the process of their child accessing and utilizing vaccine services. It was revealed that parent perception influenced immunization of their children [1, 12–14, 21, 34–44, 48, 49]. Parents not being knowledgeable of immunization was the most frequently and consistently reported barrier to childhood immunization [2–40, 42, 44, 45, 47–50, 52]. Wiysonge et al. (2012) stated that “low parental knowledge of immunization and/or lack of access to information about childhood immunization could be an important contributor to the high burden of unimmunized children in sub-Saharan Africa”. Four studies [3, 13, 25, 26], noted that a child born to a mother with little or no knowledge of vaccination may not complete the required vaccine series. Two articles reported that delay on vaccine birth doses is associated with maternal education [18, 20]. Misconceptions about childhood immunization were recorded as major hindrance to effective utilization of immunization services in this review [1, 2, 11–14, 21, 22, 29, 31, 32, 48, 49] One article [17] reported that some parents believed that the immunity induced by vaccines is less effective than that of the natural disease, and they prefer to endure the diseases than immunization. Some caregivers were reported to believe in the efficacy of traditional medicines as an alternative to immunization and concomitant treatment by traditional healers [31, 35].
Lack of trust towards vaccines was a major reported barrier. Some community members were reported to refuse immunization services due to the belief that vaccines were ‘harmful’, ‘expired’ and could cause ‘physical disability’ and/or ‘death’ among their children [2, 17, 21, 22, 30, 32, 33, 35, 38, 45, 48, 53]. The place of delivery of a baby was reported as determinants of full immunization of a child. Delivery at health facility enhances full immunization [18, 20, 22, 27, 28, 40, 48]. Long waiting time at health facilities was frequently and consistency noted [11, 12, 31, 35, 36, 45]. Two articles [35, 53], noted that parents sometimes forgot the appointment date for the next immunization visit of their children. Others reported place/time for vaccination being unknown [11]. Inconvenient immunization time such as on weekend/public holidays was reported as a barrier [43, 54]. One study [3], indicated language as a barrier to childhood immunization.
On the other hand, we also recorded non-modifiable childhood immunization barriers of parents/caretakers. Those categorized as unmodifiable are factors that are extrinsic to the parent / provider dyad. These include occupation, financial limitations, place of residence of mother/caretaker, religion, ethnicity, family size, male partners’ support, and migration; seasonal farm work, feeling ashamed of poverty-associated reasons, and being a single mother. The role of male partners in the decision for childhood vaccination was an important barrier noted. Male partners were often cited as being against vaccinating the children. The decision for immunization was generally a joint decision between the mother and father of the child. But it was noted with strong emphasis that women were in charge of taking children for immunization and sometimes the husbands opposed immunization and stopped their wives from immunizing their children by denying them the social and financial support necessary [3, 16, 17, 22, 33, 38]. The nature of occupation of the mother/caretaker was reported as a major determinant to childhood immunization [1, 11, 14, 15, 21, 22, 25, 30]. Housewives were reported to have complied with higher coverage of full immunization status than other occupations such as merchants or public/private employees [11]. Also, mothers/caretakers were reported to be affected by seasonal factors. One study [1] stated that, “usually in the first quarter of the year in which most mothers engaged in coffee-collection and processing in coffee processing industries often did not bring their children to the next immunization schedule”. Financial limitation was a major barrier cited that hinder childhood immunization [7, 11, 13, 15, 17, 24, 27, 34, 36, 38, 40, 42, 45, 47, 50, 52]. The place of residence of the mother was reported as determinants of full immunization of a child [37, 39, 41]. One study noted that the likelihood of vaccination of a child by day 7 is higher among children residing in rural areas than those in urban and pre-urban settings [18]. Socio-cultural factors and religion were noted to have negatively impacted immunization uptake [12, 18, 19, 22, 23, 37, 48]. Ethnicity and cultural beliefs were reported barriers to vaccine utilization and coverage; certain ethnic groups within the same country were identified with low coverage. Family size was associated with the probability of a child being fully immunized. It was revealed that children from large families have low vaccine uptakes, considering the burden of other children at home in taking up immunization services [11, 13, 25, 46, 50]. Migration was also cited as a hindrance to childhood immunization coverage [30, 35, 44, 48]. Feeling ashamed of poverty-associated reasons was reported as barrier. Schwarz et al. (2009) indicated that “mothers who felt that they could not dress smartly enough for the approval of other women at the clinic were less likely to attend” [24]. Babirye et al. (2011) further revealed that “poor mothers often felt stigmatized and bullied from other women and health workers if they did not show up in good clothing” [17] Being a single mother was also a cited barrier to childhood immunization in this review [37].
Health system barriers
We noted health system barriers in this review. We describe health system barriers as inherent factors that obstruct the process of delivering vaccine and vaccine related services to it beneficiaries. These includes broken cold chain, irregular supplies and distribution of vaccines; limited human resource and infrastructures, and long distances separating health facilities from families [1–3, 11, 13–16, 19, 22, 23, 25, 29, 32, 35, 43, 44, 47–52]. Vaccine shortages at health facility level and difficulties of transporting vaccines were commonly reported to significantly hinder immunization services [1–174 3,11,14,16,19,22,23,25,33,43,47,48,52,51]. Some facilities were reported to have utilized vaccine refrigerators from nearby health centers due to poor working condition of theirs [1, 3, 32]. It was noted that due to staff limitation, only one staff often conducted immunization sessions in the catchment population [2, 3, 11, 25]. Studies [11, 13, 45, 47–50, 52, 53] also revealed that some hard-to-reach areas do not have health facilities nearby to provide childhood immunization. Health workers were reported to covers long distances on outreach services due to inadequate health centers [11, 13, 15, 43]. It was also reported that, caretakers covered long distances to reach immunization centers resulted to non-completion of vaccination series [2, 3, 13, 18, 21–26, 31, 36, 38, 40–43, 46]. Some studies [11, 13, 18, 26] attempted to analyze the associations of distance with immunization outcomes. Tefera et al. (2018) indicated that “families whose home was at least an hour from the vaccination site were less likely to be fully vaccinated (56%) than families whose home was between 30 and 59 min away (67%)”. According to Miyahara et al. 2016, “the longer the distance from vaccination site, the lower the chances of vaccination by day 7 (of life) of a child”. Poor arrangement and coordination of immunization seasons at health center level were identified as barrier [16, 38, 43, 45].
Providers barriers
In addition to the parental and health system barriers mentioned above, providers were identified as possessing barriers to immunization. Providers’ barriers are those factors that limit the process of health service providers to fully provide vaccine services to it beneficiaries. These factors include the lack of knowledge of vaccine indications and contraindications and the lack of counseling skills [3, 16, 43, 52]. The restricted vaccine opening policy (use of multi-dose vials and the limited time for their use) was noted as a barrier specifically for the BCG vaccine [18, 30, 43]. It was also cited that reminders were not sent on time about routine immunization or outreach days [48] Providers’ hostility and rude attitudes to mothers were also a reported immunization barriers in this review [15, 16, 24, 30–33, 36, 45, 52, 53].
Discussion
Our review aims at identifying major childhood immunization barriers confronting health systems, providers, and parents across sub-Saharan Africa. Understanding of these barriers will help inform decision-makers and other relevant players involved in immunization programs, and to guide health interventions aim at improving immunization coverage. The study revealed childhood immunization barriers affecting utilization and coverage in the region. We grouped these barriers under three separate domains: barriers inherent in the parents/caretakers, those specific to the health system, and those related to the providers. We acknowledge that the categorisation of barriers may be different in this review than in others. Parental barriers were more and consistently identified than providers and health systems. Several of the cited parental/caretakers’ barriers were unmodifiable. Parents/caretakers reported barriers include lack of knowledge, misconceptions, financial deprivation, lack of partners’ support, and distrust of the medical systems. Other associated factors include the number of offspring, life style, migration, place of residence, long waiting time, parent’s forgetfulness; inconvenient time, being a single mother, occupation, language barrier, seasonal farm work, and feeling ashamed of poverty-associated reasons. Health system barriers include inadequate infrastructures and cold chain maintenance; distance and poor coordination. Providers’ constraints include limited human resources, hostile attitude and knowledge.
Knowledge of vaccines is very important for effective vaccine acceptance and utilization by parents. Low vaccination coverage in children is largely a result on the lack of knowledge of vaccines of healthcare providers and parents. Parents with low education and low socioeconomic status attainment showed more uncertainty towards immunization [3, 11, 13, 15–18, 22, 24, 25, 27, 28, 30, 34–36, 40, 42, 44, 45, 48, 49]. This result was also mirrored in another systematic review conducted in middle and low income countries which revealed that, most often, strong tie exist between low socioeconomic status and low level educational; with potential to lower vaccine coverage. However, investigations to understand the dynamics of these relationships are not sufficient [55]. Thus health education programs targeting these groups are critical in increasing vaccines acceptance, utilization and coverage. Further studies to unearth the dynamics of these relationships are vital. We noted that parents held reservations towards the associated side effects of vaccines. Other expressed a total distrust of immunization programs and vaccines [2, 17, 21, 22, 30, 32, 33, 35, 38, 45, 47, 48]. This is in line with previous review of Influenza Vaccine hesitancy, which pointed out that, a lack of confidence due to low perceived effectiveness of the vaccine was a hindrance to vaccine uptake [56]. Another review outlined similar beliefs, including concerns about side effects, uncertainty toward vaccine safety, and belief in anti-vaccine theories [59]. To overcome this, immunization programs should intensify public sensitization on vaccines safety and promote effective mechanisms of addressing parents’ concerns. Healthcare workers should develop approaches that acknowledge parental concerns and respectfully try to correct their misconceptions. The attitude of male partners against immunization is often noted in this review. A study carried out in Cambodia suggested that women’s decision-making power and autonomy were relevant to maternal and child health outcomes [60] It is important to carefully consider the social contexts during program design and implementation for child immunization. We need to effectively address socio-cultural contexts by involving the entire community, and not only target mothers and female caregivers. The review also raised the pressing need for women to be empowered to overcome their financial challenges in taking their children to vaccination centers.
Equally challenging is overcoming health system barriers identified, including staff shortage, the cost of maintaining the cold chain, storage and transportation of vaccines and consumables. The long distances between health centers and the families they serve are barrier that require systemic policy changes to address. The data suggest that countries should increase government financial gross domestic product (GDP) allocation to their health sector, consistent with the recommendation in the Abuja declaration [61]. Increased financial resources would enable countries to equip and upgrade existing health facilities and to increase their numbers. Targeted resources may motivate and enable staff deployed in remote areas for effective outreach activities to maximize coverage of immunization. Poor arrangement and coordination of immunization seasons at health-center level was noted [16, 38, 43, 45] this findings reflect a review (conducted in sub-Saharan countries) focus on children and youth which noted that poorly organized services can cause delays and increase costs for beneficiaries [62]. A coordinated National Immunization Program can rationalize services, thus improve immunization uptake and regulating healthcare providers.
In this review of barriers to childhood immunization, the parental/caretaker’ barriers were mostly identified, followed by health systems and providers’ barriers. It corroborates a systematic review (studies undertaken across countries) which noted that, family characteristics, parents’ understanding about vaccines and attitude were marked factors to non-immunization of their children. These pose a challenge to immunization programs due to its complexity and require strategic interventions [63]. A published article exploring vaccine hesitancy stated that various attitudes seems to result into specific categories; for instance, vaccine refusal attitude could be as a result of having little or no knowledge about vaccine, lack of trust on the vaccine or it could as well linked to financial limitations [64]. This finding disagreed with previous systematic review conducted in middle- and low -income countries. It indicated that the main factors that impede vaccination uptake and coverage were associated with healthcare system [55]. Some of the barriers cited may be modifiable within the constraints of overstretched health systems. Others may require systemic policy changes to address. Some healthcare system related factors can be realistic to design strategies that can be implemented in a range of settings, such as training of health workers to reduce missed opportunities, improve communication, and remove barriers by enhancing outreach services.
Study limitations
Our study acknowledged and outlined few limitations. As most literatures cited are observational in nature, this study cannot confirm causation nor completely rule out confounding. A few studies also relied on survey data [7, 12, 18, 27, 37, 40, 41] with the potential for selection or nonresponse bias. Population-based data studies may be liable to misclassification or measurement error, leading to information biases. Retrospective studies of caretakers/parents beliefs are subject to recall bias. Lack of protocol registration of this review may limit the evidence to demonstrate that, components of the research plan have been fully addressed. The review also lack grey literature/unpublished literature searching with potential for publication bias. Majority of the studies were conducted in East Africa [1, 3, 11–13, 16, 17, 19–21, 25, 27, 28, 32, 34, 38, 43, 44] and West Africa [1, 15, 18, 22–24, 29–31, 33, 36, 37, 39–42, 45, 46] limiting generalizability to the rest of the continent. A quantitative meta-analysis from these studies may have been useful for analyzing quantitative trends, although the heterogeneity of the studies precluded such analyses.
Conclusion
Although various methods of improving vaccination coverage in sub-Saharan Africa have been identified, achieving the desired levels for the realization of the fullest benefits of immunization is still a major challenge. This can be achieved through combined efforts of healthcare systems and providers; and address people, the communities and societies in which they live. Aggregation of known immunization barriers and the evidence on effective interventions to address these barriers should be core component of immunization programs in Sub-Saharan Africa and elsewhere.
Supplementary information
Additional file 1. Database search terms and history. Methodological Quality Assessment tool for Qualitative and Quantitative studies. Full-text articles excluded with reasons.
Acknowledgements
We would like to thank Emmanuel Osman Kamara from the Language Art Department, Earnest Bai Koroma University of Science and Technology, Sierra Leone for his assistance with English Language editing.
Abbreviations
- DTP3
Diphtheria–tetanus-pertussis vaccine third dose
- BCG
Bacillus calmette–guérin
- PRSMA
Preferred reporting items for systematic reviews and meta- analysis
- GDP
Gross domestic product
Authors’ contributions
JBB and SX conceived the review protocol. JBB, DQ, FO were involved in the data extraction and quality assessment. JBB, LC, SX involved in data synthesis and creation of table; JBB drafted the manuscript with input from all authors. All authors read and approved the final manuscript and submission.
Funding
China Medical Board funded the study. Grant number [CMB-14-188]; the funding agency did not play any role in the preparation of this study; study design, data collection, analysis, writing and decision to submission.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
We declare none.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12889-020-09169-4.
References
- 1.Tadesse H, Deribew A, Woldie M. Explorative assessment of factors affecting child immunization in Wonago district, Gedeo zone, South Ethiopia. Arch Med Sci. 2009;5(2):233–240. [Google Scholar]
- 2.Obasoha PE, Mustapha MA, Makada A, Obasohan DN. Evaluating the reasons for partial and non-immunization of children in Wushishi local government area, Niger state, Nigeria: methodological comparison Afr J Reprod Health 2018; 22:113: 10.29063/ajrh2018/v22i4.12. [DOI] [PubMed]
- 3.Malande OO, Munube D, Afaayo RN, Annet K, Bodo B, Bakainaga A, Ayebare E, Njunwamukama S, Mworozi A E, Musyoki MA. Barriers to effective uptake and provision of immunization in a rural district in Uganda. PloS one vol. 2019; 14:2 e0212270, 10.1371/journal.pone.0212270. [DOI] [PMC free article] [PubMed]
- 4.Wolfson LJ, Gasse F, Lee-Martin S-P, Lydon P, Magan A, Tibouti A, et al. Estimating the costs of achieving the WHO-UNICEF global immunization vision and strategy, 2006–2015. Bull World Health Organ 2008; 86:27. 10.2471/blt.07.045096. [DOI] [PMC free article] [PubMed]
- 5.WHO Library Cataloguing-in-Publication Data. World health statistics 2010. Available from: https://www.who.int/whosis/whostat/2010. .
- 6.GBD 2016 Causes of Death Collaborators (2017). Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the global burden of disease study 2016. Lancet (London, England), 390(10100), 1151–1210. https://dx.doi.org/10.1016%2FS0140-6736(17)32152-9. [DOI] [PMC free article] [PubMed]
- 7.Wiysonge CS, Uthman OA, Ndumbe PM, Hussey GD. Individual and contextual factors associated with low childhood immunisation coverage in sub-Saharan Africa: a multilevel analysis. PloS one 2012; vol. 7, 5 e37905. 10.1371/journal.pone.0037905. [DOI] [PMC free article] [PubMed]
- 8.Global Vaccine Action Plan – Secretariat Annual Report 2016 Available from: www.who.int/immunization/global_vaccine_action_plan/gvap_secretariat_report_2016 Accessed: April 4,2019.
- 9.WHO - Ministerial Conference on Immunization in Africa. Historical Commitment from Africa Heads of States to Advance Immunization in Africa. Available from: http://immunizationinafrica2016.org/releases/2017/1/31/historic-commitment-from-african-heads-of-state-to-advance-immunization-in-africa. Accessed 9 Apr 2019.
- 10.Cooper S, Betsch C, Sambala EZ, Mchiza N, Wiysonge CS: Vaccine hesitancy – a potential threat to the achievements of vaccination programmes in Africa. Hum Vaccin Immunother 2018; 14: 2355. 10.1080/21645515.2018.1460987. [DOI] [PMC free article] [PubMed]
- 11.Tefera AY, Wagner AL, Mekonen BE, Carlson FB, Boulton LM. Predictors and barriers to full vaccination among children in Ethiopia. Vaccines 2018; vol. 6:22 10.3390/vaccines6020022. [DOI] [PMC free article] [PubMed]
- 12.Porth JM, Wagner AL, Teklie H, Abeje Y, Moges B, Boulton ML. Vaccine non-receipt and refusal in Ethiopia. The expanded program on immunization coverage survey, 2012. Vaccine 2019; 37:2106 10.1016/j.vaccine.2019.02.045. [DOI] [PubMed]
- 13.Kiptoo E, Kobia G, Moses M, Ngure R. Factors influencing low immunization coverage among children between 12–23 Months in East Pokot, Baringo County, Kenya Int J Vaccines 2015; 1: 00012 https://10.15406/ijvv.2015.01.00012.
- 14.Cockcroft A, Usman MU, Nymucherera OF, Emori H, Duke B, Umar NI, Andersson N. Why children are not vaccinated against measles a cross-sectional study in two Nigerian states. Arch Public Health. 2014;72:48. doi: 10.1186/2049-3258-72-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nolna SK, Bonono CR, Moncher MN, Bind T, Nolna D, Zogo PO. Factors influencing the performance of routine immunization in urban areas: A comparative case study of two cities in Cameroon Douala and Yaoundé. Vaccine 2018; 36:7549 10.1016/j.vaccine.2018.10.048. [DOI] [PubMed]
- 16.Zewdie A, Letebo M, Mekonnen T. Reasons for defaulting from childhood immunization program: a qualitative study from Hadiya zone, Southern Ethiopia BMC Public Health 2016; 16:1240 10.1186/s12889-016-3904-1. [DOI] [PMC free article] [PubMed]
- 17.Babirye J N, Rutebemberwa E, Kiguli J, Wamani H, Nuwaha F, Engebretsen IMS. More support for mothers: a qualitative study on factors affecting immunisation behaviour in Kampala Uganda. BMC Public Health 2011; 11:723. 10.1186/1471-2458-11-723. [DOI] [PMC free article] [PubMed]
- 18.Miyahara R, Jasseh M, Gomez P, Shimakawa Y, Greenwood B, Keita K, Ceesay S, D’Alessandro U, Roca A. Barriers to timely administration of birth dose vaccines in The Gambia, West Africa. Vaccine 2016; vol.34 29:3335 10.1016/j.vaccine.2016.05.017. [DOI] [PMC free article] [PubMed]
- 19.Pertet AM, Kaseje D, Otieno-Odawa CF, Kirika L, Wanjala C, Ochieng J, Jaoko M, Otieno W, Odindo D. Under vaccination of children among Maasai nomadic pastoralists in Kenya: is the issue geographic mobility, social demographics or missed opportunities. BMC Public Health 2018; 18:1389 10.1186/s12889-018-6309-5. [DOI] [PMC free article] [PubMed]
- 20.Yenit MK, Gelaw YA, Shiferaw AM. Mothers’ health service utilization and attitude were the main predictors of incomplete childhood vaccination in east-Central Ethiopia: a case-control study. Arch Public Health 2018; 76:14 10.1186/s13690-018-0261-9.
- 21.Tugumisirize F, Tumwine JK, Mworozi EA. Missed opportunities and caretaker constraints to childhood vaccination in rural area in Uganda. East Afr Med J. 2002;79:7. doi: 10.4314/eamj.v79i7.8837. [DOI] [PubMed] [Google Scholar]
- 22.Babalola S. Maternal reasons for non-immunisation and partial immunisation in northern Nigeria. J Paediatr Child Health 2011; 47:276 10.1111/j.1440-1754.2010.01956.x. [DOI] [PubMed]
- 23.Oladokun RE, Adedokun BO, Lawoyin TO Children not receiving adequate immunization in Ibadan, Nigeria: what reasons and beliefs do their mothers have? Niger J Clin Pract. 2010;13(2):173–178. [PubMed] [Google Scholar]
- 24.Schwarz NG, Gysels M, Pell C, Gabor J, Schlie M, Issifou S, Lell B, Kremsner PG, Grobusch MP, Pool R. Reasons for non-adherence to vaccination at mother and child care clinics (MCCs) in Lambaréné, Gabon. Vaccine 2009; 27:5371–5375 10.1016/j.vaccine.2009.06.100. [DOI] [PubMed]
- 25.Ismail IT, El-Tayeb EM, Omer MD, Eltahir YM, El-Sayed ET, Deribe K. Assessment of routine immunization coverage in Nyala Locality, reasons behind incomplete immunization in South Darfur State, Sudan. Asian J Med Sc 2014; 6(1):1–8. https:/doi.org/10.19026/ajms.6.5348. [PMC free article] [PubMed]
- 26.Rees H, Buch E, Ferrinho P. De L.G.M, Groenewald HT, Neethling A. Immunisation coverage and reasons associated with non-immunisation in Alexandra township, September 1988. S Afr Med J 1991: Vol. 80(8) 378–381. [PubMed]
- 27.Nadella P, Smith ER. Muhihi, A, Noor RA, Masanja H, Fawzi, WW, Sudfeld, CR. Determinants of delayed or incomplete diphtheria-tetanus-pertussis vaccination in parallel urban and rural birth cohorts of 30,956 infants in Tanzania. BMC Infect Dis 2019; 19: 188 10.1186/s12879-019-3828-3. [DOI] [PMC free article] [PubMed]
- 28.Meleko A, Geremew M, Birhanu F. Assessment of child immunization coverage and associated factors with full vaccination among children aged 12-23 months at Mizan Aman town, bench Maji zone, Southwest Ethiopia. Int J Pediatr 2017; 7976587 10.1155/2017/7976587. [DOI] [PMC free article] [PubMed]
- 29.Itimi K, Dienye PO, Ordinioha B. Community participation and childhood immunization coverage: A comparative study of rural and urban communities of Bayelsa state, south-South Nigeria. Niger Med J 2012; 53:21–25. https://dx.doi.org/10.4103%2F0300-1652.99826. [DOI] [PMC free article] [PubMed]
- 30.Kagoné M, Yé M, Nébié E, Sié A, Müller O, Beiersmann C. Community perception regarding childhood vaccinations and its implications for effectiveness: a qualitative study in rural Burkina Faso. BMC Public Health 2018; 18:324 10.1186/s12889-018-5244-9. [DOI] [PMC free article] [PubMed]
- 31.Tobin-West CI, Alex-Hart BA. Identifying barriers and sustainable solution to childhood immunization in Khana local government area of Rivers state, Nigeria Int Q Community Health Educ 2011-2012; 32:149–158. http://dx.doi.org/10.2190/IQ.32.2.e. [DOI] [PubMed]
- 32.Braka F, Asiimwe D, Soud F, Lewis RF, Makumbi I, Gust D. A qualitative analysis of vaccine safety perceptions and concerns among caretakers in Uganda. Matern Child Health J 2012; 16:1045–1052. 10.1007/s10995-011-0826-5. [DOI] [PubMed]
- 33.Ambe JP, Omotara BA, Mandu Baba M. Perceptions, beliefs and practices of mothers in sub-urban and rural areas towards measles and measles vaccination in northern Nigeria. Trop Doctors 2001; 31:89–90. https://doi.org/10.1177%2F004947550103100211. [DOI] [PubMed]
- 34.Tadesse H, Deribew A, Woldie M. Predictors of defaulting from completion of child immunization in South Ethiopia, may 2008: a case control study. BMC Public Health 2009; 9:150. https://dx.doi.org/10.1186%2F1471-2458-9-150. [DOI] [PMC free article] [PubMed]
- 35.Jani JV, De Schacht C, Jani IV, Bjune G. Risk factors for incomplete vaccination and missed opportunity for immunization in rural Mozambique. BMC Public Health 2008; 8:161. https://dx.doi.org/10.1186%2F1471-2458-8-161. [DOI] [PMC free article] [PubMed]
- 36.Eng E, Naimoli J, Naimoli G, Parker KA, Lowenthal N. The acceptability of childhood immunization to Togolese mothers: A Sociobehavioral perspective. Health Educ Q. 1991;18:97–110. doi: 10.1177/109019819101800110. [DOI] [PubMed] [Google Scholar]
- 37.Landoh DE, Ouro-Kavalah F, Yaya I, Kahn AL, Wasswa P, Lacle A, Nassoury DI, Gitta SN, Soura AB. Predictors of incomplete immunization coverage among one to five years old children in Togo. BMC Public Health 2016; 16:968. https://dx.doi.org/10.1186%2Fs12889-016-3625-5. [DOI] [PMC free article] [PubMed]
- 38.Legesse E, Dechasa W. An assessment of child immunization coverage and its determinants in Sinana District, Southeast Ethiopia BMC Pediatr 2015; 15:31. https://dx.doi.org/10.1186%2Fs12887-015-0345-4. [DOI] [PMC free article] [PubMed]
- 39.Wemakor A, Helegbe GK, Abdul-Mumin A, Amedoe S, Zoku JA, Dufie AI. Prevalence and factors associated with incomplete immunization of children (12-23 months) in Kwabre East District, Ashanti region, Ghana Arch Public Health 2018; 76:67 https://dx.doi.org/10.1186%2Fs13690-018-0315-z. [DOI] [PMC free article] [PubMed]
- 40.Adedokun ST, Uthman OA, Adekanmbi VT, Wiysonge CS. Incomplete childhood immunization in Nigeria: a multilevel analysis of individual and contextual factors. BMC Public Health 2017; 17:236 https://dx.doi.org/10.1186%2Fs12889-017-4137-7. [DOI] [PMC free article] [PubMed]
- 41.Chidiebere ODI, Uchenna E, Kenechi OS. Maternal sociodemographic factors that influence full child immunisation uptake in Nigeria. S Afr J Child Health. 2014;8(4):138–142. doi: 10.7196/SAJCH.661. [DOI] [Google Scholar]
- 42.Ekouevi DK, Gbeasor-Komlanvi FA, Yaya I, Zida-Compaore WI, Boko A, Sewu E, Lacle A, Ndibu N, Toke Y, Landoh DE. Incomplete immunization among children aged 12–23 months in Togo: a multilevel analysis of individual and contextual factors. BMC Public Health. 2018; 18:952. doi: https://dx.doi.org/10.1186%2Fs12889-018-5881-z. [DOI] [PMC free article] [PubMed]
- 43.Tadesse T, Getachew K, Assefa T, Ababu Y, Simireta T, Birhanu Z, Hailemichael Y. Factors and misperceptions of routine childhood immunization service uptake in Ethiopia: findings from a nationwide qualitative study. Pan Afr Med J. 2017;5:28. doi: 10.11604/pamj.2017.28.290.14133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Negussie A, Kassahun W, Assegid S, Hagan AK. Factors associated with incomplete childhood immunization in Arbegona district, southern Ethiopia: a case--control study. BMC Public Health 2016; 16:27. https://dx.doi.org/10.1186%2Fs12889-015-2678-1. [DOI] [PMC free article] [PubMed]
- 45.Bosu WK, Ahelegbe D, Edum-Fotwe, E, Bainson, KA, Turkson, P K Acta Tropica 1997; 68:259–267 https://doi.org/10.1016/S0001-706X(97)00094-6. [DOI] [PubMed]
- 46.Desgrées du Loû A, Pison G. Barriers to universal child immunization in rural Senegal 5 years after the accelerated Expanded Programme on Immunization. Bull World Health Organ. 1994;72:751–759. [PMC free article] [PubMed] [Google Scholar]
- 47.Sato R. Differential determinants and reasons for the non- and partial vaccination of children among Nigerian caregivers. Vaccine. 2019;38(1):63–69. doi: 10.1016/j.vaccine.2019.09.097. [DOI] [PubMed] [Google Scholar]
- 48.Akwataghibe NN, Ogunsola EA, Broerse J, Popoola OA, Agbo AI, Dieleman MA. Exploring factors influencing immunization utilization in Nigeria-A mixed methods study. Front Public Health. 2019;7:392. doi: 10.3389/fpubh.2019.00392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yismaw AE, Assimamaw NT, Bayu N, Mekonen SS. Incomplete childhood vaccination and associated factors among children aged 12–23 months in Gondar city administration, Northwest, Ethiopia 2018. BMC Res Notes. 2019;12(1):241. doi: 10.1186/s13104-019-4276-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ntenda P. Factors associated with non- and under-vaccination among children aged 12-23 months in Malawi. A multinomial analysis of the population-based sample. Pediatr Neonatol. 2019;60(6):623–633. doi: 10.1016/j.pedneo.2019.03.005. [DOI] [PubMed] [Google Scholar]
- 51.Okenwa UJ, Dairo MD, Uba B, Ajumobi O. Maternal reasons for non-receipt of valid hepatitis B birth dose among mother-infant pairs attending routine immunization clinics, south-east, Nigeria. Vaccine. 2019;37(46):6894–6899. doi: 10.1016/j.vaccine.2019.09.056. [DOI] [PubMed] [Google Scholar]
- 52.Mthiyane TN, Cohen C, Norris SA, Walaza S, Tempia S, Cohen AL, Von Mollendorf C. Factors associated with missed and delayed DTP3 vaccination in children aged 12–59 months in two communities in South Africa, 2012–2013. S Afr Med J. 2019;109(8):562–569. doi: 10.7196/SAMJ.2019.v109i8.13244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mekonnen AG, Bayleyegn AD, Ayele ET. Immunization coverage of 12-23 months old children and its associated factors in Minjar-Shenkora district, Ethiopia: a community-based study. BMC Pediatr. 2019;19(1):198. doi: 10.1186/s12887-019-1575-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ibraheem R, Abdulkadir M, Akintola M, Adeboye M. Determinants of timely presentation for birth dose vaccination at an immunization Centre in North-Central Nigeria. Ann Glob Health. 2019;85(1):20. doi: 10.5334/aogh.725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rainey JJ, Watkins M, Ryman TK, Sandhu P, Bo A, Banerjee K. Reasons related to non-vaccination and under-vaccination of children in low and middle income countries: findings from a systematic review of the published literature,1999–2009. Vaccine. 2011;29(46):8215–8221. doi: 10.1016/j.vaccine.2011.08.096. [DOI] [PubMed] [Google Scholar]
- 56.Schmid P, Rauber D, Betsch C, Lidolt G, Denker ML. Barriers of influenza vaccination intention and behavior - a systematic review of influenza vaccine hesitancy, 2005–2016. PLoS One 2017; 12(1), e0170550. 10.1371/journal.pone.0170550. [DOI] [PMC free article] [PubMed]
- 57.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta analyses: the PRISMA statement. PLoS Med 6(7): e1000097. 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed]
- 58.Pereira AJ, Quach S, Heidebrecht LC, Quan DS, Kolbe F, Finkelstein M, Kwong JC. Barriers to the use of reminder/recall interventions for immunizations: A systematic review. BMC Med Inform Dec Making. 2012;12:145. doi: 10.1186/1472-6947-12-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wilson L, Rubens-Augustson T, Murphy M, Jardine C, Crowcroft N, Hui C, Wilson K. Barriers to immunization to newcomers: A systematic review. Vaccine. 2018;36(8):1055–1062. doi: 10.1016/j.vaccine.2018.01.025. [DOI] [PubMed] [Google Scholar]
- 60.Forder JA. Attitudes towards immunization in Cambodia: A qualitative study of health worker and community knowledge, attitudes and practices in Kompong Chhnang 2002.
- 61.WHO | The Abuja Declaration. Available from: https://www.who.int/healthsystems/publications/abuja_declaration/en/. Accessed 6 Apr 2019.
- 62.Sullivan BJ, Esmaili BE, Cunningham CK. Barriers to initiating tuberculosis treatment in sub-Saharan Africa: a systematic review focused on children and youth. Glob Health Action 2017; 10(1), 1290317. 10.1080/16549716.2017.1290317. [DOI] [PMC free article] [PubMed]
- 63.Tauil MC, Sato AP, Waldman EA. Factors associated with incomplete or delayed vaccination across countries: A systematic review. Vaccine. 2016; 34, 2635–2643 http://dx.doi.org/10.1016/j.vaccine.2016.04.016. [DOI] [PubMed]
- 64.Peretti-Watel P, Larson HJ, Ward JK, Schulz WS, Verger P. Vaccine hesitancy: clarifying a theoretical framework for an ambiguous notion. PLoS Curr Outbreaks 2015; http://dx.doi.org/10.1371/currents.outbreaks.6844c80ff9f5b273f34c91f71b7fc289. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Database search terms and history. Methodological Quality Assessment tool for Qualitative and Quantitative studies. Full-text articles excluded with reasons.
Data Availability Statement
Not applicable.