Abstract
A health care system and a Medicaid payer partnered to develop an educational intervention and payment redesign program to improve timely postpartum visits for low-income, high-risk mothers in New York City between April 2015 and October 2016. The timely postpartum visit rate was higher for 363 mothers continuously enrolled in the program than for a control group matched by propensity score (67% [243/363] and 56% [407/726], respectively; P < .001). An innovative partnership between a health care system and Medicaid payer improved access to health care services and community resources for high-risk mothers.
Many low-income women fail to get appropriate medical follow-up after delivery, putting their long-term health at risk. We evaluate a multifaceted program (behavioral educational intervention and payment redesign) designed to increase rates of timely postpartum visits according to Healthcare Effectiveness Data and Information Set (HEDIS) guidelines from the National Committee for Quality Assurance. A large health system and a Medicaid payer partnered to implement this program for women identified as high risk.1
INTERVENTION
Our evidence-based behavioral intervention provided education about health conditions (hypertension, gestational diabetes, and depression), important health behaviors (nutrition and exercise), and common postpartum symptoms; taught self-management skills; enhanced social support; and connected patients with community resources and health care services.1 The intervention addressed transportation needs, linked participants with community resources, and addressed specific psychosocial needs of enrollees. A payment reform component included a cost-sharing arrangement between the health care system and the Medicaid payer to cover costs related to employing a social worker and community health worker, and financial incentives for completed postpartum visits.
PLACE AND TIME
The program enrolled women insured by Healthfirst who delivered between April 2015 and October 2016 at Mount Sinai Hospital, a large tertiary hospital in New York City.
PERSON
Eligible participants included women aged 18 years and older who spoke Spanish or English and had at least 1 of the following: gestational diabetes, hypertension, positive screen for depression, late registration for prenatal care (> 20 weeks), or residence in neighborhoods considered at high risk for diabetes or hypertension according to the New York City Department of Health and Mental Hygiene. A total of 217 women refused to participate, three withdrew from the program, and three were not found in the health insurance claims database. Claims data were available for 506 mothers.
PURPOSE
The purpose of the program was to increase the number of low-income, high-risk women who have a timely postpartum care visit using a behavioral educational intervention and payment redesign.
IMPLEMENTATION
The intervention was implemented by a social worker and a community health worker in English and Spanish. The program combined education during the postpartum hospital stay, a call at one to two weeks after delivery, 3 to 12 additional calls depending on patient needs, and written educational materials. The payment reform component included a cost-sharing arrangement between the health care system and the Medicaid payer to cover costs related to employing the social worker and community health worker. Small financial incentives ($10) in the form of enhanced payments for completed postpartum visits by the payer were rolled out 12 months following the implementation of the intervention. Patients received round-trip public transportation and incentives ($10) for attending their postpartum visit. Nonfinancial incentives included education for physicians, nurses, social workers, and registrars on the importance of the postpartum visit and on the clinical topics of gestational diabetes, hypertension, and postpartum depression.
EVALUATION
The primary outcome was completion of the postpartum visit as defined by HEDIS (i.e., a visit with an obstetrics or primary care clinician between 21 and 56 days after delivery2,3); 363 women were eligible for this measure by meeting HEDIS continuous enrollment requirements. Secondary outcomes included rates of any postpartum or gynecologic health care visit up to 90 days after delivery and plan enrollment at six months and one year after delivery. A total of 377 women in the intervention group had at least 90 days of enrollment in the plan after delivery.4 To measure plan enrollment at 6 and 12 months, we included all 506 women identified in Healthfirst data systems (Figure 1).
FIGURE 1—
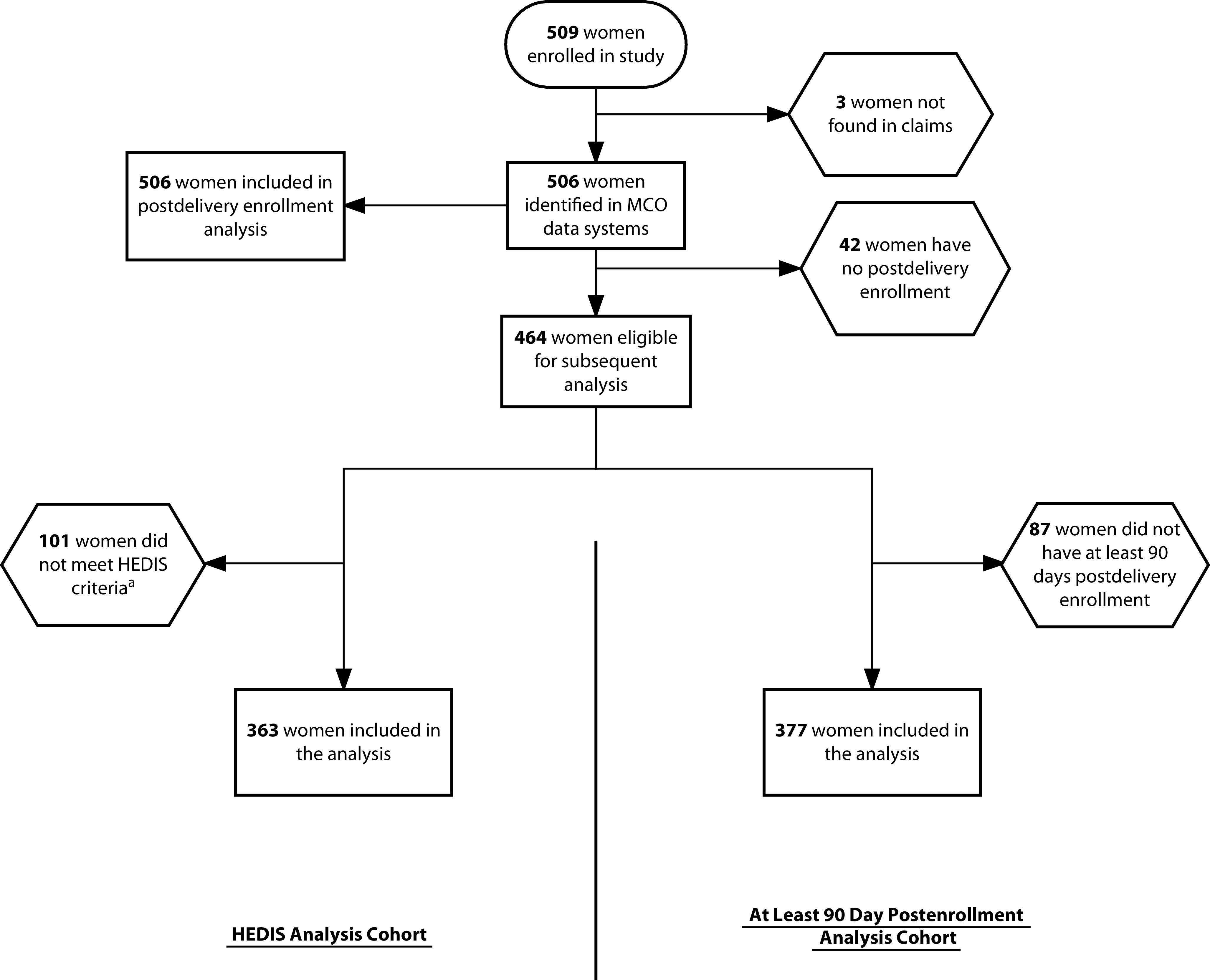
Chart Showing High-Risk Mothers Enrolled in Study: New York City, April 2015–October 2016
Note. HEDIS = Healthcare Effectiveness Data and Information Set; MCO = managed care organization.
aIn order to be eligible for the HEDIS denominator, members must have at least 43 days of continuous enrollment in the health plan prior to delivery and 56 days of continuous enrollment after delivery.
We used claims data from 2014 to 2017, with the episode of care defined as 9 months prior to delivery and up to 12 months after delivery. We used propensity score matching to compare timely postpartum visits for mothers enrolled in the program versus a similar group of mothers enrolled in the same Medicaid plan who gave birth in 2015 and 2016. We generated matched comparison groups using a greedy nearest neighbor matching method at a 2:1 control-to-intervention ratio; to perform this method, we used the MatchIt package in R.5 We generated propensity scores through logistic regression using enrollment in the intervention as the dependent variable. Explanatory variables included mother’s age, language, neighborhood6; days enrolled in plan prior to delivery; and diagnoses of hypertension, gestational diabetes, or mental illness in claims from the prior 12 months.
Of 506 women enrolled in the intervention, 29% spoke Spanish, 13% had hypertension, 10% had diabetes, and 3% had depression or mental illness (Table 1).
TABLE 1—
Characteristics of Intervention and Matched Comparison Groups for Study Participants: New York City, 2015–2016
| Before Propensity Score Matching |
After Propensity Score Matching Comparison Group (Enrollment n = 754), Mean or % (No.) | |||
| Matching Variable | Intervention Group (Enrollment n = 506), Mean or % (No.) | Comparison Group (Enrollment n = 50 487), Mean or % (No.) | Standardized Difference | |
| Age, y | 28.91 | 29.11 | 0.035 | 29.03 |
| Language | ||||
| English | 70.4 (356) | 63.9 (32 283) | 0.137 | 70.6 (714) |
| Spanish | 29.1 (147) | 25.2 (12 742) | 0.086 | 28.7 (290) |
| Other | 0.6 (3) | 10.8 (5 462) | 0.452 | 0.4 (4) |
| Clinical high risk | ||||
| Diabetes | 10.47 (53) | 12.69 (6 408) | 0.069 | 11.17 (113) |
| Hypertension | 12.65 (64) | 6.59 (3 328) | 0.206 | 11.26 (114) |
| Mental illness | 2.96 (15) | 2.7 (1 365) | 0.016 | 2.57 (26) |
| Predelivery enrollment days | 356.66 | 351.66 | 9 | 345.14 |
Note. UHF = United Hospital Fund. UHF zip code results not shown; matching based on UHF neighborhood codes was successful (standardized difference < 0.2).
In analyses using propensity score matching, compared with women in the control group, program participants had higher rates of postpartum visits in the HEDIS-defined time period (66.9% vs 56.0%; P < .001) and higher rates of all postpartum outpatient or gynecologic care up to 90 days after delivery (90.2% vs 83.4%; P = .002). Similarly, program participants were more likely to be enrolled with the Medicaid plan than mothers in the matched comparison group at six months after delivery (79.1% [400/506] vs 73.3% [742/1012]; P = .015) and at one year after delivery (71.0% [359/506] vs 66.3% [671/1012]; P = .067), although this was not statistically significant at one year after delivery.
ADVERSE EFFECTS
Assessing postpartum care utilization of low-income, high-risk women with Medicaid coverage is challenging given plan enrollment and disenrollment patterns.
SUSTAINABILITY
Lessons learned from this initiative include the importance of aligning incentives between a Medicaid managed care organization and a large health care system, the need to cost share to support team-based care, and the value and challenges of advancing an equity agenda within a health care system that can meaningfully improve outcomes. Our findings should be of interest to health care systems and payers as the landscape of health care delivery continues to move toward value-based models.
PUBLIC HEALTH SIGNIFICANCE
A novel partnership between a health care system and a Medicaid payer increased postpartum visits among high-risk, low-income mothers. The follow-up rate was higher for visits that occurred within 90 days after delivery, a period consistent with current recommendations for postpartum care from the American College of Obstetricians and Gynecologists.7
Our program demonstrates the importance of including multiple stakeholders, patient education, care coordination, clinician and staff education, and community and medical resources to implement a successful new care model. The current gap in the literature is sizable regarding the needs of underserved women, especially in relation to the complex factors affecting postpartum nonattendance; these include barriers due to limited flexibility of services offered by facilities, proficiency of providers, and health insurance coverage. Our study attempted to comprehensively address these challenges.
This is one of few initiatives that have integrated health care systems, payers, physicians, and social workers to address access to care and social determinants of health for underserved women. Although our program had challenges with the provision of financial incentives and the refusal rate, our study adds important knowledge regarding the types of interventions that are needed by health care systems and payers to increase access to maternal care for underserved women.
ACKNOWLEDGMENTS
Support for this research was provided by the Robert Wood Johnson Foundation, Grant I. D. 72557 (E. A. Howell), “Reducing Disparities in Care for High-Risk Postpartum Women Through Redesign of Payment and Delivery Systems.”
Note. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the Robert Wood Johnson Foundation.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to disclose.
HUMAN PARTICIPANT PROTECTION
The Program for the Protection of Human Subjects (the institutional review board) at the Icahn School of Medicine at Mount Sinai approved this study under GCO#14-1033.
Footnotes
See also Dasgupta, p. S174.
REFERENCES
- 1.Howell EA, Padron NA, Beane SJ et al. Delivery and payment redesign to reduce disparities in high risk postpartum care. Matern Child Health J. 2017;21(3):432–438. doi: 10.1007/s10995-016-2221-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Committee for Quality Assurance. Prenatal and postpartum care (PPC) 2019. Available at: https://www.ncqa.org/hedis/measures/prenatal-and-postpartum-care-ppc. Accessed December 3, 2019.
- 3.Health Insurance Marketplace. Quality rating system measure technical specifications. September 2015. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/QualityInitiativesGenInfo/Downloads/2016-QRS-Measure-Technical-Specifications.pdf. Accessed May 14, 2020.
- 4.National Committee for Quality Assurance. Proposed changes to existing measure for HEDIS®1 2020: prenatal and postpartum care (PPC) 2019. Available at: https://www.ncqa.org/wp-content/uploads/2019/02/20190208_08_Perinatal_Depression.pdf. Accessed December 3, 2019.
- 5.Ho DE, Imai K, King G, Stuart EA. MatchIt: nonparametric preprocessing for parametric causal inference. J Stat Softw. 2011;42(8):1–28. [Google Scholar]
- 6.New York City Health Dept. NYC UHF 42 neighborhoods. Available at: http://a816-dohbesp.nyc.gov/IndicatorPublic/EPHTPDF/uhf42.pdf. Accessed December 3, 2019.
- 7.ACOG committee opinion no. 736: optimizing postpartum care. Obstet Gynecol. 2018;131:e140–e150. doi: 10.1097/AOG.0000000000002633. [DOI] [PubMed] [Google Scholar]


