Abstract
Objectives. To characterize the association between social needs prevalence and no-show proportion and variation in these associations among specific social needs.
Methods. In this study, we used results from a 10-item social needs screener conducted across 19 primary care practices in a large urban health system in Bronx County, New York, between April 2018 and July 2019. We estimated the association between unmet needs and 2-year history of missed appointments from 41 637 patients by using negative binomial regression models.
Results. The overall no-show appointment proportion was 26.6%. Adjusted models suggest that patients with 1 or more social needs had a significantly higher no-show proportion (31.5%) than those without any social needs (26.3%), representing an 19.8% increase (P < .001). We observed a positive trend (P < .001) between the number of reported social needs and the no-show proportion—26.3% for those with no needs, 30.0% for 1 need, 32.1% for 2 needs, and 33.8% for 3 or more needs. The strongest association was for those with health care transportation need as compared with those without (36.0% vs 26.9%).
Conclusions. We found unmet social needs to have a significant association with missed primary care appointments with potential implications on cost, quality, and access for health systems.
The US poverty rate, established by the US Census Bureau as a measure starting from 1959, has steadily declined since inception but, at 17.8%, remains the second highest among the 35 Organization for Economic Co-operation and Development member countries.1,2 Furthermore, some US populations are disproportionately affected, with 20% of children on average nationally and 40% of children in the poorest urban and rural communities living below the federal poverty line.3 There is a growing body of research supporting the impact of poverty on health, often referred to as the social determinants of health4,5 and defined as “the conditions, in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life.”6 From an individual level, one can describe these drivers of health as unmet social needs.7 Unmet social needs are linked to increased prevalence of chronic diseases, obesity, and poorer developmental outcomes in children.4,8 Recent population health studies in the United States suggest that unmet social needs are a contributing factor to increased mortality risk on par with the leading causes of death and may account for upward of 40% of health outcomes.9–11 However, the actual mechanism by which unmet social needs drive health status is less clear.
Though population health studies continue to support the impact of unmet social needs, there is less evidence on how health systems can address this issue in practical and meaningful ways.12,13 In 2016, the American Academy of Pediatrics issued a policy statement recommending that providers screen for social needs during primary care visits.8 More recently, in 2019, the National Academies of Sciences, Engineering, and Medicine put out a report providing more detailed guidance regarding how health systems can integrate social needs assessments in practice.14
Missed medical appointments (i.e., no-shows) have an impact on health outcomes as well and may serve as a meaningful outcome for social determinants of health–based interventions. Missed appointments are costly and disruptive to health systems, and some health systems have invested in strategies to reduce no-shows as a business imperative.15,16 Past research suggests that no-show appointments are associated with increased medical costs and inefficiencies, reduced productivity and quality of care, increased ambulatory-sensitive visits in emergency departments, and suboptimized clinical outcomes.17 Social needs such as transportation access, financial considerations, health literacy, insurance status (e.g., Medicaid, Medicare, insurance with limited coverage plans), and language barriers have been associated with increased no-show appointments in the primary care setting.18–20 Unmet social needs may contribute to missed medical appointments and, thus, poorer health outcomes.
Social factors drive health status, yet the associated mechanism by which social needs influence health is unknown. It is clear, however, that health inequities have persisted over time despite changes in disease patterns and advances in medical technology and therapeutics.21 Some authors have suggested that social condition is a fundamental cause of health inequities. This proposition can be investigated by focusing on how key resources (e.g., money, power, knowledge, and status) ultimately reduce risk and increase protective factors regardless of disease type through multiple factors including access to services.22
In this study, our objective was to determine if social needs are associated with missed appointments in the primary care setting. We hypothesized that patients with unmet social needs would have a higher proportion of no-show appointments because of the extra burden imposed by lower levels of key resources. Furthermore, we presumed that this influence was not homogeneous when comparing social needs such as food insecurity or housing quality, but rather that specific social needs may have distinct influences on no-show proportions.23–25 To better elucidate possible mechanisms, we aimed to characterize the overall association between social needs prevalence and no-show proportion, as well as variation in the associations between specific social needs and no-show rates across primary care practices in a large, urban health system in Bronx County, New York.
METHODS
In 2017, the Montefiore Health System (MHS) launched a system-wide social determinants of health screening initiative to identify patients with unmet social needs at more than 19 ambulatory health care practices. A 10-item screening tool (Appendix A, available as a supplement to the online version of this article at http://www.ajph.org) was adapted to meet health system needs from a widely used, validated instrument, the Health Leads screening toolkit, after an extensive pilot process involving key stakeholders. Between April 2018 and July 2019, the ambulatory network utilized this tool at 19 participating ambulatory practices in the Bronx (17 sites) and Westchester County (2 sites), New York. Each practice had discretion to determine whom to screen and the frequency of screenings. Practice decisions were informed by a number of factors including the availability of staff (e.g., social workers, community health workers), perceived utility of universal versus targeted screenings, and provider preferences. The tool was available in 9 languages, and parents or guardians completed the screener for patients too young to respond independently. Screener results were entered into Epic, MHS’s electronic health record, and providers reviewed the results with patients and offered to connect patients to practice-based resources including community health workers and social workers.
Outcome Variables
The primary outcome was the number of no-shows to primary care appointments in the 2 years before the index visit (i.e., initial social needs screen). No-shows included same-day cancellations26 but excluded visits canceled because of changes in provider schedules. Primary care specialties included pediatrics, family medicine, general obstetrics/gynecology, and internal medicine. Appointments included in the outcome were all routine office visits, follow-ups, annual examinations, same-day appointments, nurse visits, and well-child visits. Excluded were laboratory visits, flu shot sessions, and procedure visits. We also included the total number of completed visits to account for individuals with a higher number of appointments, who would have a higher likelihood of having a missed appointment.
Study Population
We excluded respondents who did not complete 5 or more of the 10 screener questions (n = 171) from the analysis, as well as patients with no visits in the 2 years before screening, resulting in a final sample size of 41 637 unique patients.
Predictors and Covariates
The primary independent variables were the categorized number and types of social needs reported by the patient. We calculated the number of social needs based on the number of questions to which each patient responded “yes.” We then grouped this number into none, 1, 2, or 3 or more, with cutpoints selected based on the distribution of social needs. Additional covariates included age (categorized as 0–5; 6–11; 12–20; 21–34; 35–49; 50–64; and ≥ 65 years), sex, race/ethnicity (Hispanic, non-Hispanic Black, non-Hispanic White, non-Hispanic Asian/Pacific Islander, other, and a missing indicator), health insurance at the time of the screening visit (Medicaid, Medicare, commercial, and a missing indicator), the patient’s preferred language (English, Spanish, other, and a missing indicator), and whether the respondent lived in New York City (NYC) public housing (more information later in this section).
We used the Elixhauser Comorbidity Index to capture patient health status.27 Briefly, the Elixhauser Comorbidity Index is the number of 31 diagnostic criteria (e.g., uncomplicated hypertension, complicated hypertension, depression) based on International Classification of Diseases, Tenth Revision, Clinical Modification, codes from the 2 years before baseline. We categorized the measure as 0, 1, 2, 3 to 5, and 6 or more. We extracted respondent data by using MySQL to query data from the Epic Electronic Health Record Data Warehouse and using Looking Glass Clinical Analytics, version 4.4.2 (Streamline Health, Atlanta, GA), an online application supporting extraction of clinical data.28 As a proxy marker of individual socioeconomic status variables, we included the proportion of the population living below poverty at the census block group level. Area-based poverty came from the 2013–2017 American Community Survey at the block group level,29 the smallest geographic unit for which those data are available.
To geocode patient addresses to obtain public housing status and area-based measures, we used the New York State Street and Address Composite geocoding services tool for New York State addresses, and the US Census Address Batch Geocoder for non–New York State addresses.30,31 Across both methods, we successfully geocoded 97.9% of respondents. We identified patients living in NYC public housing by flagging addresses that geocoded to tax lots associated with public housing.32 We included a missing indicator for area-based poverty and public housing status for patients who were not geocoded successfully.
Analysis Approach
We calculated the overall and subgroup-specific no-show proportion. Because of evidence of overdispersion, we used negative binomial regression to derive the covariate-adjusted no-show proportion for overall social needs and each individual social need. While we also considered a zero-inflated negative binomial regression model, both models had essentially identical Akaike information criterion data and minimal quantitative differences, so we used the negative binomial model. To understand how the no-show proportion varied by subgroup, we also estimated the no-show proportion ratio, which compares the no-show proportion for those with social need(s) to those without. We incorporated robust standard errors into the models to reduce concerns regarding heteroskedasticity.
We used a 3-stepped analytic approach. First, we fit unadjusted models (model 1) that only accounted for the number of appointments as an offset variable, followed by models (model 2) similar to model 1 but also adjusting for sociodemographic variables described previously (age, sex, race/ethnicity, preferred language, payer, area-based poverty, public housing status, and patient health status via the Elixhauser Comorbidity Index). Lastly, a final set of models (model 3) adjusts for the sociodemographic variables in model 2 but also for all other social needs, as there was a modest correlation between many of these needs. Thus, model 3 estimates the association between the no-show proportion and each individual social need, taking into account all of the other social needs. To ensure that multicollinearity between social needs would not be an issue for model 3, we also estimated the variance inflation factors for each social need. We accounted for clustering of individuals by census block group in variance estimation for all analyses including area-based poverty.
Additional analyses used a similar 3-stepped approach to examine whether the association between the number and types of social needs and the no-show proportion varied for children (aged < 18 years) versus adults and, among adults, whether the association varied for those with higher health status (Elixhauser comorbidity score < 3) versus lower health status (score ≥ 3). We tested potential effect modification in the ratio of no-show proportions by age and number of comorbid conditions by including multiplicative interaction terms in the models while accounting for the full set of covariates (e.g., model 2 for overall risks and model 3 for individual risks). Because of the number of tests for interaction, we considered an interaction with a P level of less than .01 to be statistically significant. We completed statistical analyses by using Stata version 13.1 (StataCorp LP, College Station, TX) and for mapping we used ArcGIS version 10.3 (Environmental Systems Research Institute, Redlands, CA). We analyzed data in summer 2019.
RESULTS
The overall no-show appointment proportion in this sample of 41 637 participants was 26.6% in the 2 years before the social needs screening, with an average of 8 appointments and 2 no-shows per patient (Table 1). Certain population subgroups had a higher proportion of no-shows, including those who were Hispanic or non-Hispanic Black, who preferred English, who were insured through Medicaid, who lived in public housing or in a higher poverty block group, and who had a Elixhauser comorbidity index of less than or equal to 2. Our demographic data regarding representativeness of the screened population to the primary care population at participating clinics, the distribution of social needs by sociodemographics, and on the screener itself are similar to previous findings.33 Both unadjusted and adjusted models suggest that those with 1 or more social needs had a significantly higher no-show proportion (31.5%) than those without any social needs (26.3%), a 5.2-percentage-point difference representing an 19.8% increase in comparison.
TABLE 1—
Summary of Demographic Variables for Patients at an Urban Health System, With Social Risk Assessments Conducted Between April 2018 and July 2019: Bronx, NY
| No. | Average No. of Appointments (95% CI) | Average No. of No-Shows (95% CI) | No-Show Proportion, % (95% CI) | |
| Total | 41 637 | 8.0 (7.9, 8.0) | 2.1 (2.1, 2.1) | 26.6 (26.4, 26.8) |
| Age group, y | ||||
| 0–4 | 5 989 | 12.1 (11.9, 12.3) | 2.9 (2.9, 3.0) | 23.8 (23.4, 24.3) |
| 5–9 | 4 117 | 6.4 (6.2, 6.5) | 1.9 (1.9, 2.0) | 29.9 (29.2, 30.7) |
| 10–17 | 5 397 | 4.9 (4.8, 5.0) | 1.6 (1.6, 1.7) | 32.9 (32.2, 33.7) |
| 18–29 | 4 700 | 5.7 (5.6, 5.9) | 2.0 (1.9, 2.1) | 34.7 (33.9, 35.4) |
| 30–44 | 4 928 | 6.7 (6.5, 6.9) | 2.2 (2.2, 2.3) | 33.6 (32.8, 34.3) |
| 45–64 | 8 955 | 8.0 (7.9, 8.2) | 2.2 (2.2, 2.3) | 27.0 (26.6, 27.5) |
| ≥ 65 | 7 551 | 9.7 (9.5, 9.9) | 1.7 (1.7, 1.8) | 17.9 (17.5, 18.3) |
| Sex | ||||
| Male | 16 698 | 7.4 (7.3, 7.5) | 2.0 (2.0, 2.0) | 27.3 (26.9, 27.7) |
| Female | 24 939 | 8.4 (8.3, 8.5) | 2.2 (2.2, 2.2) | 26.2 (25.9, 26.5) |
| Race/ethnicity | ||||
| Hispanic | 15 589 | 8.3 (8.2, 8.5) | 2.3 (2.2, 2.3) | 27.2 (26.8, 27.6) |
| Non-Hispanic Black | 12 015 | 7.5 (7.4, 7.7) | 2.1 (2.1, 2.1) | 27.9 (27.5, 28.3) |
| Non-Hispanic White | 1 571 | 7.2 (6.8, 7.5) | 1.5 (1.4, 1.7) | 21.1 (19.9, 22.2) |
| Non-Hispanic Asian/Pacific Islander | 710 | 8.1 (7.6, 8.6) | 1.7 (1.6, 1.9) | 21.5 (20.0, 22.9) |
| Other | 150 | 7.4 (6.7, 8.2) | 1.6 (1.3, 1.9) | 20.9 (17.7, 24.0) |
| Missing | 11 602 | 8.0 (7.9, 8.1) | 2.1 (2.0, 2.1) | 25.6 (25.2, 26.0) |
| Preferred language | ||||
| English | 33 123 | 7.7 (7.6, 7.7) | 2.1 (2.1, 2.2) | 27.7 (27.5, 28.0) |
| Spanish | 6 246 | 8.9 (8.7, 9.1) | 2.0 (1.9, 2.1) | 22.9 (22.4, 23.5) |
| Other | 1 102 | 9.3 (8.9, 9.7) | 2.2 (2.0, 2.3) | 23.2 (22.0, 24.3) |
| Missing | 1 166 | 10.9 (10.5, 11.2) | 2.4 (2.3, 2.6) | 21.8 (20.8, 22.9) |
| Payer | ||||
| Medicaid | 19 220 | 8.4 (8.3, 8.5) | 2.6 (2.5, 2.6) | 30.5 (30.2, 30.9) |
| Medicare | 7 794 | 10.2 (10.0, 10.4) | 2.0 (2.0, 2.1) | 19.6 (19.2, 20.0) |
| Commercial | 13 262 | 6.0 (6.0, 6.1) | 1.5 (1.4, 1.5) | 24.6 (24.2, 25.0) |
| Missing | 1 361 | 7.8 (7.4, 8.1) | 2.6 (2.4, 2.8) | 34.1 (32.8, 35.4) |
| Block-group poverty, % | ||||
| Q1: 0–8.8 | 8 553 | 7.2 (7.1, 7.3) | 1.7 (1.6, 1.7) | 23.1 (22.2, 24.0) |
| Q2: 8.9–19.2 | 7 709 | 7.7 (7.5, 7.8) | 1.9 (1.8, 2.0) | 24.8 (23.9, 25.6) |
| Q3: 19.3–30.8 | 8 111 | 8.1 (8.0, 8.3) | 2.2 (2.1, 2.2) | 26.6 (25.9, 27.3) |
| Q4: 30.9–42.5 | 8 117 | 8.4 (8.3, 8.6) | 2.4 (2.3, 2.4) | 28.1 (27.5, 28.8) |
| Q5: 42.6–88.4 | 8 119 | 8.6 (8.4, 8.8) | 2.5 (2.5, 2.6) | 29.8 (29.0, 30.5) |
| Missing | 1 028 | 6.8 (6.5, 7.2) | 2.0 (1.8, 2.1) | 28.7 (27.9, 29.4) |
| Public housing | ||||
| Yes | 4 767 | 9.1 (8.9, 9.3) | 2.8 (2.7, 2.9) | 31.2 (30.6, 31.9) |
| No | 33 667 | 7.9 (7.9, 8.0) | 2.1 (2.0, 2.1) | 26.0 (25.7, 26.2) |
| Outside of NYC or missing | 3 203 | 6.6 (6.4, 6.8) | 1.7 (1.6, 1.8) | 25.8 (25.0, 26.5) |
| Elixhauser comorbidity index | ||||
| 0 | 11 881 | 6.3 (6.2, 6.4) | 1.7 (1.7, 1.8) | 27.7 (27.2, 28.1) |
| 1 | 9 605 | 6.6 (6.5, 6.7) | 1.9 (1.9, 2.0) | 28.9 (28.4, 29.4) |
| 2 | 5 944 | 7.3 (7.2, 7.5) | 2.0 (2.0, 2.1) | 27.9 (27.3, 28.5) |
| 3–5 | 8 481 | 9.0 (8.8, 9.1) | 2.3 (2.2, 2.4) | 25.3 (24.9, 25.8) |
| ≥ 6 | 5 726 | 12.9 (12.7, 13.2) | 3.1 (3.0, 3.2) | 23.4 (22.9, 23.9) |
Note. CI = confidence interval; NYC = New York City.
Figure 1 provides the no-show proportion ratio for the number of needs and need categories. Adjusted models reveal a positive, dose–response relationship between number of social needs and the no-show proportion. These models also highlight elevated no-show proportions for those with specific needs, including health transportation or health cost needs. Table 2 further details a significant dose–response relationship between increasing number of social needs and the no-show proportion. The dose–response between number of social needs and no-shows only modestly attenuated upon adjustment for covariates. In both unadjusted and covariate-adjusted models, there was a significant positive association between the no-show proportion and having each individual social need. The strongest association was for those with health care transportation and health care affordability needs: 33.8% and 26.2% higher, respectively, than those without (36.0% vs 26.9% and 34.2% vs 27.1%).
FIGURE 1—
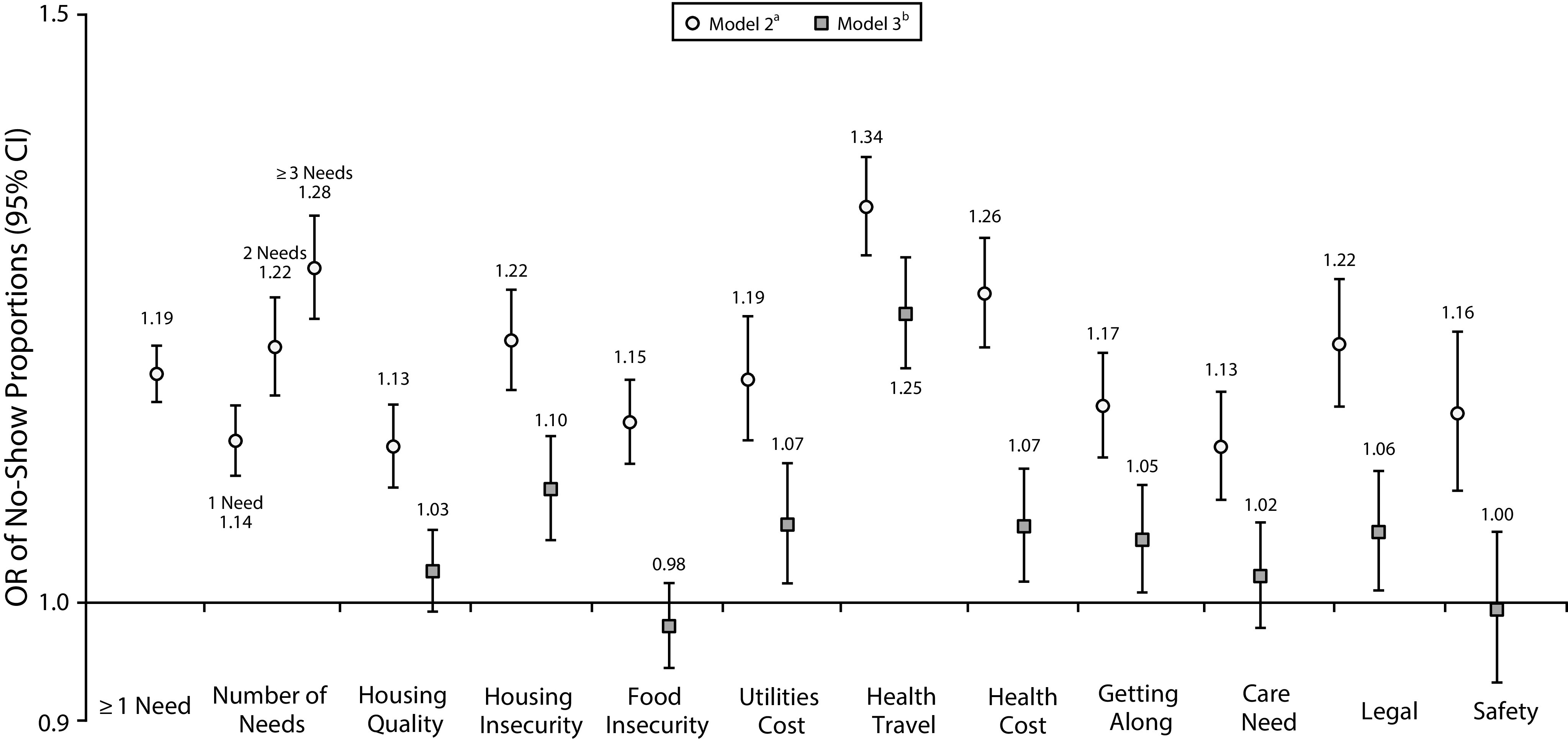
No-Show Primary Care Proportion Ratios Comparing No Social Risks to One or More, Increasing Number of Needs, and Specific Social Risk Categories for Patients at an Urban Health System: Bronx, NY, April 2018–July 2019
Note. CI = confidence interval; OR = odds ratio. The ratio of no-show proportions was estimated with a Poisson model.
aModel 2 adjusted for age, sex, race/ethnicity, preferred language, payer, area-based poverty, public housing status, and Elixhauser comorbidity score.
bModel 3 adjusted for each social need plus model 2 covariates.
TABLE 2—
No-Show Appointment Proportion Regression Models Examining Number of Social Needs and Specific Social Need Categories for Patients at an Urban Health System, With Social Risk Assessments Between April 2018 and July 2019: Bronx, NY
| No-Show Proportion, % (95% CI) |
||
| Model 2a | Model 3b | |
| No. of needs | ||
| None | 26.3 (25.9, 26.8) | . . . |
| ≥ 1 | 31.5*** (30.8, 32.2) | . . . |
| 1 | 30.0*** (29.2, 30.8) | . . . |
| 2 | 32.1*** (30.9, 33.2) | . . . |
| ≥ 3 | 33.8*** (32.6, 35.0) | . . . |
| Housing-quality need | ||
| No | 27.1 (26.6, 27.6) | 27.3 (26.8, 27.7) |
| Yes | 30.7*** (29.7, 31.7) | 28.0 (27.0, 29.0) |
| Housing-security need | ||
| No | 27.1 (26.6, 27.6) | 27.2 (26.7, 27.7) |
| Yes | 33.1*** (31.9, 34.3) | 29.8*** (28.6, 31.1) |
| Food-security need | ||
| No | 27.1 (26.6, 27.6) | 27.3 (26.8, 27.8) |
| Yes | 31.3*** (30.3, 32.3) | 26.8 (25.8, 27.8) |
| Utilities shut-off need | ||
| No | 27.2 (26.7, 27.7) | 27.2 (26.8, 27.7) |
| Yes | 32.4*** (30.9, 33.8) | 29.1** (27.6, 30.5) |
| Health care–transportation need | ||
| No | 26.9 (26.5, 27.4) | 27.0 (26.5, 27.4) |
| Yes | 36.0*** (34.8, 37.2) | 33.6*** (32.3, 34.9) |
| Health care–cost need | ||
| No | 27.1 (26.6, 27.6) | 27.2 (26.7, 27.7) |
| Yes | 34.2*** (32.8, 35.6) | 29.0** (27.6, 30.4) |
| Getting-along need | ||
| No | 27.2 (26.7, 27.7) | 27.2 (26.8, 27.7) |
| Yes | 31.8*** (30.5, 33.0) | 28.7* (27.4, 30.0) |
| Care need | ||
| No | 27.3 (26.8, 27.7) | 27.3 (26.8, 27.8) |
| Yes | 30.9*** (29.6, 32.2) | 27.9 (26.7, 29.2) |
| Legal need | ||
| No | 27.2 (26.7, 27.7) | 27.2 (26.8, 27.7) |
| Yes | 33.2*** (31.6, 34.7) | 28.9* (27.5, 30.3) |
| Safety need | ||
| No | 27.3 (26.8, 27.8) | 27.3 (26.8, 27.8) |
| Yes | 31.7*** (29.8, 33.6) | 27.2 (25.4, 29.0) |
Note. CI = confidence interval.
Sample size varies from n = 41 275 to n = 41 637; adjusted for age, sex, race/ethnicity, preferred language, payer, area-based poverty, public housing status, and Elixhauser comorbidity score.
Sample size n = 40 450; model adjusted for each social need plus model 2 covariates.
P < .05; **P < .01; ***P < .001.
In the fully adjusted model that included adjusting for each social need, the difference in the no-show proportions for those with and without each individual need attenuated. Health care transportation needs nevertheless retained the strongest statistically significant association with the no-show proportion. Specifically, those with a health care transportation need had a 24.4% higher no-show proportion than those without (33.6% vs 27.0%), the largest differential for any of the adjusted estimates in social needs.
We conducted stratified analyses based on age group and comorbidities as summarized in Table 3. We did not find any significant differences in the associations between the number and types of social needs and the no-show proportion for children versus adults. In the covariate-adjusted models, for both children and adults, the no-show proportion was positively and significantly associated with each individual social need, although for some individual needs (e.g., care need for children), the relationship was not meaningful. After we fully adjusted for each individual social need, the difference in the no-show proportions for those with and without each individual social need decreased. For adults, similar to children, the strongest association between individual social needs and the no-show proportion in the fully adjusted model was for the health care transportation need. The no-show proportion for adults with the need was 32.4% versus 26.4% for those without. Adults with a housing security need, a utilities shut-off need, and a health care cost need also had a significantly higher no-show proportion than did their counterparts without each need, while children with a getting-along need had a significantly higher no-show proportion than did their counterparts without the need.
TABLE 3—
No-Show Appointment Proportion Regression Models Examining Number of Social Needs and Specific Social Need Categories for Patients at an Urban Health System, Stratified by Age Groups and Comorbidity Scores: Bronx, NY, April 2018–July 2019
| Children (< 18 Years), No-Show Proportion, % (95% CI) |
Adults (≥ 18 Years), No-Show Proportion, % (95% CI) |
Lower Comorbidity Score (< 3), No-Show Proportion, % (95% CI) |
Higher Comorbidity Score (≥ 3), No-Show Proportion, % (95% CI) |
|||||
| Model 2a | Model 3b | Model 2c | Model 3d | Model 2e | Model 3f | Model 2g | Model 3h | |
| No. of needs | ||||||||
| None | 27.6 (27.0, 28.2) | . . . | 25.7 (25.2, 26.2) | . . . | 28.7 (28.1, 29.4) | . . . | 22.9 (22.3, 23.4) | . . . |
| ≥ 1 | 32.3*** (31.2, 33.3) | . . . | 31.1*** (30.3, 32.0) | . . . | 34.8*** (33.5, 36.1) | . . . | 27.7*** (26.8, 28.6) | . . . |
| 1 | 31.1*** (29.9, 32.3) | . . . | 29.5*** (28.5, 30.5) | . . . | 33.7*** (32.0, 35.3) | . . . | 25.9*** (24.8, 27.0) | . . . |
| 2 | 33.3*** (31.4, 35.2) | . . . | 31.5*** (30.1, 32.8) | . . . | 35.0*** (32.6, 37.3) | . . . | 28.0*** (26.5, 29.6) | . . . |
| ≥ 3 | 34.1*** (32.1, 36.2) | . . . | 33.7*** (32.4, 35.1) | . . . | 37.1*** (34.1, 40.1) | . . . | 30.2*** (28.8, 31.6) | . . . |
| Housing-quality need | ||||||||
| No | 28.3 (27.7, 28.9) | 28.4 (27.8, 29.0) | 26.5 (26.0, 27.1) | 26.7 (26.1, 27.2) | 29.5 (28.8, 30.1) | 29.6 (28.9, 30.2) | 23.8 (23.2, 24.4) | 24.0 (23.4, 24.6) |
| Yes | 31.5*** (30.1, 33.0) | 29.3 (27.9, 30.8) | 30.4*** (29.1, 31.7) | 27.3 (26.0, 28.6) | 34.5*** (32.2, 36.8) | 30.9 (28.5, 33.3) | 27.0*** (25.7, 28.4) | 24.4 (23.0, 25.7) |
| Housing-security need | ||||||||
| No | 28.3 (27.7, 28.9) | 28.4 (27.8, 29.0) | 26.4 (25.9, 27.0) | 26.5 (26.0, 27.1) | 29.4 (28.8, 30.0) | 29.4 (28.8, 30.0) | 23.7 (23.1, 24.3) | 23.8 (23.2, 24.4) |
| Yes | 33.5*** (31.2, 35.7) | 29.8 (27.6, 32.0) | 32.9*** (31.6, 34.3) | 29.7*** (28.2, 31.2) | 37.1*** (34.4, 39.8) | 33.6** (30.8, 36.4) | 29.4*** (28.0, 30.8) | 26.5*** (25.0, 28.1) |
| Food-security need | ||||||||
| No | 28.3 (27.7, 28.9) | 28.5 (27.9, 29.1) | 26.5 (26.0, 27.1) | 26.8 (26.2, 27.3) | 29.5 (28.9, 30.1) | 29.7 (29.0, 30.3) | 23.8 (23.2, 24.4) | 24.1 (23.4, 24.7) |
| Yes | 32.1*** (30.3, 33.9) | 28.2 (26.4, 30.0) | 31.0*** (29.8, 32.2) | 26.3 (25.1, 27.4) | 34.3*** (31.8, 36.8) | 28.7 (26.3, 31.1) | 27.8*** (26.6, 29.0) | 23.7 (22.5, 24.9) |
| Utilities shut-off need | ||||||||
| No | 28.4 (27.8, 29.0) | 28.5 (27.9, 29.1) | 26.6 (26.1, 27.1) | 26.6 (26.1, 27.2) | 29.5 (28.9, 30.1) | 29.5 (28.9, 30.2) | 23.9 (23.3, 24.5) | 23.9 (23.3, 24.5) |
| Yes | 31.9** (29.6, 34.1) | 28.7 (26.6, 30.8) | 33.0*** (31.2, 34.8) | 29.5** (27.6, 31.3) | 37.4*** (33.6, 41.2) | 32.7 (28.9, 36.5) | 29.4*** (27.6, 31.3) | 26.6** (24.7, 28.4) |
| Health care–transportation need | ||||||||
| No | 28.1 (27.5, 28.7) | 28.1 (27.5, 28.7) | 26.3 (25.8, 26.9) | 26.4 (25.8, 26.9) | 29.4 (28.8, 30.0) | 29.5 (28.8, 30.1) | 23.5 (22.9, 24.0) | 23.5 (22.9, 24.1) |
| Yes | 38.9*** (36.4, 41.4) | 36.6*** (33.9, 39.3) | 34.8*** (33.5, 36.1) | 32.4*** (30.9, 33.9) | 38.6*** (35.7, 41.5) | 34.1** (30.8, 37.4) | 31.1*** (29.7, 32.4) | 29.4*** (27.9, 30.9) |
| Health care–cost need | ||||||||
| No | 28.4 (27.8, 29.0) | 28.4 (27.8, 29.0) | 26.5 (25.9, 27.0) | 26.6 (26.1, 27.2) | 29.4 (28.8, 30.0) | 29.5 (28.9, 30.1) | 23.7 (23.1, 24.3) | 23.9 (23.3, 24.5) |
| Yes | 36.8*** (33.7, 39.9) | 30.3 (27.4, 33.1) | 33.2*** (31.7, 34.6) | 28.4* (26.8, 29.9) | 37.1*** (33.9, 40.2) | 32.3 (29.3, 35.3) | 29.6*** (28.1, 31.1) | 25.3 (23.7, 26.9) |
| Getting-along need | ||||||||
| No | 28.4 (27.8, 29.0) | 28.4 (27.8, 29.0) | 26.6 (26.1, 27.1) | 26.7 (26.1, 27.2) | 29.5 (28.9, 30.1) | 29.5 (28.9, 30.2) | 23.9 (23.3, 24.5) | 24.0 (23.4, 24.6) |
| Yes | 33.9*** (31.5, 36.4) | 31.3* (28.9, 33.8) | 30.9*** (29.5, 32.4) | 27.9 (26.4, 29.3) | 34.4*** (31.9, 37.0) | 31.4 (28.8, 33.9) | 27.8*** (26.1, 29.4) | 24.9 (23.3, 26.5) |
| Care need | ||||||||
| No | 28.4 (27.8, 29.0) | 28.4 (27.8, 29.0) | 26.7 (26.1, 27.2) | 26.7 (26.2, 27.3) | 29.6 (29.0, 30.2) | 29.6 (29.0, 30.2) | 24.0 (23.4, 24.6) | 24.0 (23.4, 24.6) |
| Yes | 31.2** (29.4, 33.0) | 29.0 (27.2, 30.7) | 31.2*** (29.4, 33.1) | 27.5 (25.6, 29.3) | 34.9** (31.3, 38.4) | 31.3 (27.9, 34.7) | 27.8*** (25.8, 29.8) | 24.3 (22.3, 26.3) |
| Legal need | ||||||||
| No | 28.3 (27.8, 28.9) | 28.4 (27.8, 29.0) | 26.6 (26.1, 27.1) | 26.7 (26.1, 27.2) | 29.5 (28.9, 30.1) | 29.5 (28.9, 30.2) | 23.9 (23.3, 24.5) | 24.0 (23.4, 24.6) |
| Yes | 33.7*** (31.3, 36.2) | 30.5 (28.1, 32.9) | 32.9*** (31.1, 34.7) | 27.9 (26.2, 29.6) | 38.1*** (34.0, 42.3) | 32.5 (28.7, 36.2) | 29.1*** (27.3, 30.9) | 24.8 (23.0, 26.6) |
| Safety need | ||||||||
| No | 28.5 (27.9, 29.1) | 28.5 (27.9, 29.1) | 26.7 (26.2, 27.3) | 26.7 (26.2, 27.3) | 29.6 (29.0, 30.2) | 29.6 (29.0, 30.2) | 24.0 (23.4, 24.6) | 24.0 (23.4, 24.6) |
| Yes | 33.4** (29.4, 37.4) | 27.8 (24.4, 31.3) | 30.9*** (28.8, 33.1) | 26.7 (24.6, 28.8) | 36.4*** (32.1, 40.8) | 31.8 (27.5, 36.0) | 27.2** (24.9, 29.5) | 23.4 (21.1, 25.7) |
Note. CI = confidence interval.
Sample size varies from n = 15 371 to n= 15 503; adjusted for age, sex, race/ethnicity, preferred language, payer, public housing status, and Elixhauser comorbidity score.
Sample size n = 15 048; adjusted for each social need, age, sex, race/ethnicity, preferred language, payer, area-based poverty, public housing status, and Elixhauser comorbidity score.
Sample size varies from n = 25 904 to n = 26 134; adjusted for age, sex, race/ethnicity, preferred language, payer, public housing status, and Elixhauser comorbidity score.
Sample size n = 25 202; adjusted for each social need, age, sex, race/ethnicity, preferred language, payer, area-based poverty, public housing status, and Elixhauser comorbidity score.
Sample size varies from n = 12 497 to n = 12 614; adjusted for age, sex, race/ethnicity, preferred language, payer, public housing status, and Elixhauser comorbidity score.
Sample size n = 12 184; adjusted for each social need, age, sex, race/ethnicity, preferred language, payer, area-based poverty, public housing status, and Elixhauser comorbidity score.
Sample size varies from n = 13 407 to n = 13 520; adjusted for age, sex, race/ethnicity, preferred language, payer, public housing status, and Elixhauser comorbidity score.
Sample size n = 13 018; adjusted for each social need, age, sex, race/ethnicity, preferred language, payer, area-based poverty, public housing status, and Elixhauser comorbidity score.
P < .05; **P < .01; ***P < .001.
When examining the relationship by comorbidity score subgroup, we found there was a significant positive association between the presence and number of social needs and the no-show proportion for those with both lower and higher comorbidities. As with age, however, there were no significant differences in the associations between the number and types of social needs and the no-show proportion for those with lower versus higher number of comorbidities. In the fully adjusted model, the strength of the associations attenuated for each individual social need in both comorbidity groups. However, the no-show proportion remained significantly higher for those with housing security and health care transportation needs, where the largest relative difference for both groups was for those with a health care transportation need versus those without. For the higher comorbidity group only, those with a utilities shut-off need had a significantly higher no-show proportion than did those without the need (26.6% vs 23.9%, respectively).
DISCUSSION
These findings from a study conducted in a large, diverse urban population present several important implications for health systems that serve similar communities and may have generalizable policy and operational considerations. We believe this is the first health system–wide study focused on examining the strength of association of social needs and no-show appointments in primary care. There was a significant difference in no-show behaviors and social needs in our sample of 41 637 individuals in all models. We found that after we adjusted for several covariates including demographics, census tract poverty estimates, and clinical complexity, the no-show proportion for those with 1 or more social needs was 5 percentage points higher than those without, and increasing number of social needs (≥ 2 and ≥ 3) was associated with a significantly higher proportion of missed appointments. Though, to our knowledge, previous studies have not assessed possible dose relationships, our findings are similar to a recent cross-sectional study that examined the association of any self-reported social need and patients missing more than 1 appointment in a calendar year in 2 urban primary care practices.34
Regarding the implications of these findings, we found that across this health system during the same study time period, there were 3 525 975 primary care visits. Therefore, this 5-point difference in missed appointment proportion after adjustment represents 176 298 no-show appointments that may be attributable to social needs, a stream of forgone revenue to the health system exceeding $18 million over 2 years. This finding has important health access, quality, and cost implications for health systems, especially those that serve large low-income communities.
Given that the data indicate there is not high collinearity between the social needs (variance inflation factors less than 1.33 for all needs), the attenuation in parameter estimates from model 2 to model 3 are not a result of multicollinearity, but rather can be interpreted as reflecting the independent association between each social need and the no-show proportion. Thus, in addition to a positive, graded relationship between the proportion of no-shows and number of social needs, we were able to identify the individual social needs, including health care transportation and health care cost, with the strongest association with the no-show proportion. This finding is similar to what has been reported in other studies, suggesting the influence of transportation on missed appointments.17,26 More specifically, our study prompted focused efforts to maximize patient access to nonemergency medical transport benefits and supported our health system’s advocacy efforts to optimize and preserve existing public transportation options. These may represent opportunities for health systems to target specific social needs that may disproportionately contribute to no-show appointments.
Our findings appear plausible as one could imagine how a lack of key resources may influence health-seeking behaviors. For example, our findings support that lack of access to transportation will make it harder to attend routine primary care visits. This finding supports the theory of other authors’ proposed mechanism that lack of key resources (i.e., social needs) increases risk and decreases protective factors related to health care access independent of disease type.22 Finally, we found that the strength of the association between no-show proportion and social needs did not vary for children versus adults or by comorbidity status.
Limitations
Despite the findings and possible implications of this study, there are important limitations, including significant issues related to establishing causation and temporality. First, we cannot attribute this difference in no-show appointments to a single factor, as we know patient behavior is multifactorial. We also assume that the social needs assessment taken at 1 time point is stable enough of a proxy for social risk over time. It is likely that these needs are dynamic in nature and vary. Furthermore, the timeframe of the social needs as measured in the screener vary and the outcome of interest, no-shows, is defined in the 2 years before the screener. While it would be preferable to define the outcome closer to the screener date, limiting the timeframe would have biased the sample toward less-healthy patients, as fewer healthy patients would have had at least 1 primary care visit in the 2 years before the screener. All data were collected retrospectively, and social needs assessments were cross-sectional, so it is not possible to establish temporality.
Next, although the study was large in size with more than 40 000 participants, we utilized a convenience sample with data extracted from electronic health records, which presents issues related to sampling and classification biases. We did not assess the representativeness of sample vis-à-vis the more than 300 000 patients served by this ambulatory network. These data utilized patients’ self-reported social needs that were then entered into an electronic health record by nonresearch staff. Patients may underreport social needs because of a multitude of concerns ranging from stigma to a perceived lack of benefits.
Regarding the regression modeling, we included several covariates that may have colinear relationships around measurements of relative poverty. There is also potential for an ecological fallacy in our results, as we utilized population-level data to make inferences on individual behaviors. Finally, because of this study design, even if one could address these social needs, our data do not shed any light on whether this would result in changes in health-seeking behaviors.
Public Health Implications
These data suggest that unmet social needs may contribute to health access disparities attributable to reduced primary care visits. This finding may require health systems to work more closely with public health and social service sectors as these needs may be better addressed through partnership. Understanding the epidemiology of social risk and extent of the problem through prevalence assessments is a critical first step. Next steps involve aligning public health, community-based, and practice-oriented approaches that aim to address social needs. Our data suggest that the burden or influence of certain social needs, such as transportation, may place a disproportionately higher burden on patients trying to keep medical appointments, an important finding. Our health system has invested in and continues to examine multiple approaches that may mitigate the burden of social needs, as it is unlikely 1 approach or actor alone will be sufficient to address the complexity and multifactorial influence. Public health, social service, and health service researchers need to align strategies and advance evidence-based practice through community-engaged scholarship, implementation research, and pragmatic study designs. Health systems that welcome such collaboration and acknowledge the critical impact of social needs on individual health will be best positioned to deliver the highest quality of services to the communities they serve.
ACKNOWLEDGMENTS
The authors would like to thank the Doris Duke Charitable Foundation (grant 2018169) and the Agency for Healthcare Research and Quality (K12HS026396) for their financial support of this analysis.
Note. The opinions expressed in this document are those of the authors and do not necessarily reflect the official position of Agency for Healthcare Research and Quality or the US Department of Health and Human Services.
CONFLICTS OF INTEREST
The authors have no conflicts of interest.
HUMAN PARTICIPANT PROTECTION
The study was reviewed and approved by the Albert Einstein College of Medicine institutional review board (2017-8434).
Footnotes
See also Dasgupta, p. S174.
REFERENCES
- 1.Organization for Economic Co-operation and Development. Poverty rate (indicator) 2019. [DOI] [Google Scholar]
- 2.US Census. Current Population Survey (CPS) Annual Social and Economic (ASEC) supplement. 2017. Available at: https://www.census.gov/data/tables/time-series/demo/income-poverty/cps-pov/pov-01.html?cssp=Typeahead. Accessed August 2, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Denavas-Walt C, Proctor BD. Income and poverty in the United States: 2014 Current Population Reports. US Census Bureau; 2015. Available at: https://www.census.gov/content/dam/Census/library/publications/2015/demo/p60-252.pdf. Accessed August 10, 2018. [Google Scholar]
- 4.Turney K, Lee H, Mehta N. The social determinants of child health. Soc Sci Med. 2013;95:1–5. doi: 10.1016/j.socscimed.2013.07.015. [DOI] [PubMed] [Google Scholar]
- 5.Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep. 2014;129(suppl 2):19–31. doi: 10.1177/00333549141291S206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. About social determinants of health. Available at: https://www.who.int/social_determinants/sdh_definition/en. Accessed August 2, 2019.
- 7.Alderwick H, Gottlieb LM. Meanings and misunderstandings: a social determinants of health lexicon for health care systems. Milbank Q. 2019;97(2):407–419. doi: 10.1111/1468-0009.12390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Council on Community Pediatrics. Poverty and child health in the United States. Pediatrics. 2016;137(4):e20160339. doi: 10.1542/peds.2016-0339. [DOI] [PubMed] [Google Scholar]
- 9.Magnan S. Social Determinants of Health 101 for Health Care: Five Plus Five. Vol 7. Washington, DC: National Academy of Medicine; 2017. [Google Scholar]
- 10.Galea S, Tracy M, Hoggatt KJ, DiMaggio C, Karpati A. Estimated deaths attributable to social factors in the United States. Am J Public Health. 2011;101(8):1456–1465. doi: 10.2105/AJPH.2010.300086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schroeder SA. We can do better—improving the health of the American people. N Engl J Med. 2007;357(12):1221–1228. doi: 10.1056/NEJMsa073350. [DOI] [PubMed] [Google Scholar]
- 12.Garg A, Boynton-Jarrett R, Dworkin PH. Avoiding the unintended consequences of screening for social determinants of health. JAMA. 2016;316(8):813–814. doi: 10.1001/jama.2016.9282. [DOI] [PubMed] [Google Scholar]
- 13.Beck AF, Cohen AJ, Colvin JD et al. Perspectives from the Society for Pediatric Research: interventions targeting social needs in pediatric clinical care. Pediatr Res. 2018;84(1):10–21. doi: 10.1038/s41390-018-0012-1. [DOI] [PubMed] [Google Scholar]
- 14.National Academies of Sciences. Integrating Social Care Into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health. Washington, DC: National Academies Press; 2019. Engineering, and Medicine. [PubMed] [Google Scholar]
- 15.Kheirkhah P, Feng Q, Travis LM, Tavakoli-Tabasi S, Sharafkhaneh A. Prevalence, predictors and economic consequences of no-shows. BMC Health Serv Res. 2016;16(1):13. doi: 10.1186/s12913-015-1243-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Triemstra JD, Lowery L. Prevalence, predictors, and the financial impact of missed appointments in an academic adolescent clinic. Cureus. 2018;10(11):e3613. doi: 10.7759/cureus.3613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Samuels RC, Ward VL, Melvin P et al. Missed appointments: factors contributing to high no-show rates in an urban pediatrics primary care clinic. Clin Pediatr (Phila). 2015;54(10):976–982. doi: 10.1177/0009922815570613. [DOI] [PubMed] [Google Scholar]
- 18.Kaplan-Lewis E, Percac-Lima S. No-show to primary care appointments. J Prim Care Community Health. 2013;4(4):251–255. doi: 10.1177/2150131913498513. [DOI] [PubMed] [Google Scholar]
- 19.George A, Rubin G. Non-attendance in general practice: a systematic review and its implications for access to primary health care. Fam Pract. 2003;20(2):178–184. doi: 10.1093/fampra/20.2.178. [DOI] [PubMed] [Google Scholar]
- 20.Nguyen DL, DeJesus RS, Wieland ML. Missed appointments in resident continuity clinic: patient characteristics and health care outcomes. J Grad Med Educ. 2011;3(3):350–355. doi: 10.4300/JGME-D-10-00199.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mackenbach JP, Stirbu I, Roskam A-JR et al. Socioeconomic inequalities in health in 22 European countries. N Engl J Med. 2008;358(23):2468–2481. doi: 10.1056/NEJMsa0707519. [DOI] [PubMed] [Google Scholar]
- 22.Phelan JC, Link BG, Tehranifar P. Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J Health Soc Behav. 2010;51(1 suppl):S28–S40. doi: 10.1177/0022146510383498. [DOI] [PubMed] [Google Scholar]
- 23.Ballantyne M, Rosenbaum PL. Missed appointments: more complicated than we think. Paediatr Child Health. 2017;22(3):164–165. doi: 10.1093/pch/pxx039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ofei-Dodoo S, Kellerman R, Hartpence C, Mills K, Manlove E. Why patients miss scheduled outpatient appointments at urban academic residency clinics: a qualitative evaluation. Kans J Med. 2019;12(3):57–61. [PMC free article] [PubMed] [Google Scholar]
- 25.Brown EE, Schwartz M, Shi C et al. Understanding why urban, low-income patients miss primary care appointments: insights from qualitative interviews of West Philadelphians. J Ambul Care Manage. 2020;43(1):30–40. doi: 10.1097/JAC.0000000000000316. [DOI] [PubMed] [Google Scholar]
- 26.Chaiyachati KH, Hubbard RA, Yeager A et al. Association of rideshare-based transportation services and missed primary care appointments: a clinical trial. JAMA Intern Med. 2018;178(3):383–389. doi: 10.1001/jamainternmed.2017.8336. [DOI] [PubMed] [Google Scholar]
- 27.Quan H, Sundararajan V, Halfon P et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 28.Bellin E, Fletcher DD, Geberer N, Islam S, Srivastava N. Democratizing information creation from health care data for quality improvement, research, and education—the Montefiore Medical Center experience. Acad Med. 2010;85(8):1362–1368. doi: 10.1097/ACM.0b013e3181df0f3b. [DOI] [PubMed] [Google Scholar]
- 29.US Census Bureau. American Community Survey, 2013–2017 American Community Survey 5-Year Estimates, Table C17002. American FactFinder. Available at: https://www.census.gov/newsroom/press-kits/2018/acs-5year.html. Accessed August 2, 2019.
- 30.Address Geocoder. NYS GIS Program Office. Available at: https://gis.ny.gov/gisdata/inventories/details.cfm?DSID=1278. Accessed August 27, 2019.
- 31.US Census Bureau. Geocoding Address Batch. Available at: https://geocoding.geo.census.gov/geocoder/geographies/addressbatch?form. Accessed August 27, 2019.
- 32.Chambers EC, Rehm C. Brief report: characterizing the burden of cardiometabolic disease among public housing residents served by an urban hospital system. Ethn Dis. 2019;29(3):463–468. doi: 10.18865/ed.29.3.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Heller CG, Parsons AS, Chambers EC, Fiori KP, Rehm CD. Social risks among primary care patients in a large urban health system. Am J Prev Med. 2020;58(4):514–525. doi: 10.1016/j.amepre.2019.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Berkowitz SA, Hulberg AC, Hong C et al. Addressing basic resource needs to improve primary care quality: a community collaboration programme. BMJ Qual Saf. 2016;25(3):164–172. doi: 10.1136/bmjqs-2015-004521. [DOI] [PubMed] [Google Scholar]


