The coronavirus disease 2019 (COVID-19) pandemic, originally observed in Wuhan, China, has led to an unprecedented overload of healthcare systems.1 , 2 The large-scale implementation of a strictly surveilled public health policy, consisting of movement restrictions and generalized lockdowns, halted the progression of the disease and proved determinant in the management of this critical situation. However, numerous consequences were unavoidably observed. Among the common measures applied to prevent COVID-19 spread was the postponement of elective surgical procedures, resulting in the deprivation of guideline-directed therapeutic approaches for a wide variety of conditions.
In the case of cardiac surgery, previous reports have highlighted the impact of prolonged time on the surgical waiting list on mortality.3, 4, 5, 6 Therefore, we aimed to assess the effect of COVID-19 pandemic on cardiac surgery workload in Greece, a country that has remarkably managed to contain the COVID-19 by rapid and effective implementation of restrictive measures.
This is a retrospective analysis of data collected from Cardiac Surgery departments in Greece in 2 large volume hospitals of the National Health System belonging to the larger Metropolitan area of Athens (Hippokratio General Hospital, Athens and Evangelismos General Hospital, Athens). Based on an ad hoc design form, we collected demographic data (such as age and gender) as well as the indication for operation. Data were collected for the period from 16th January 2020 and up to 7th April (pre- and during pandemia outbreak) and from the equivalent (COVID-19 outbreak) time period of 2019. The study was approved by the Ethics Committee of each institution and was carried out in accordance with the Declaration of Helsinki (1989).
Data from 583 cardiac surgery procedures were collected. The application of movement restrictions (12/3/2020-7/5/2020) was considered the era of COVID-19 pandemic in Greece (Time Period 3), with the equivalent time period in 2019 (Time Period 1, 12/3/2019-7/5/2019) and the time period directly before Time Period 3 (Time Period 2, 16/1/2020-11/3/2020) serving as baseline.
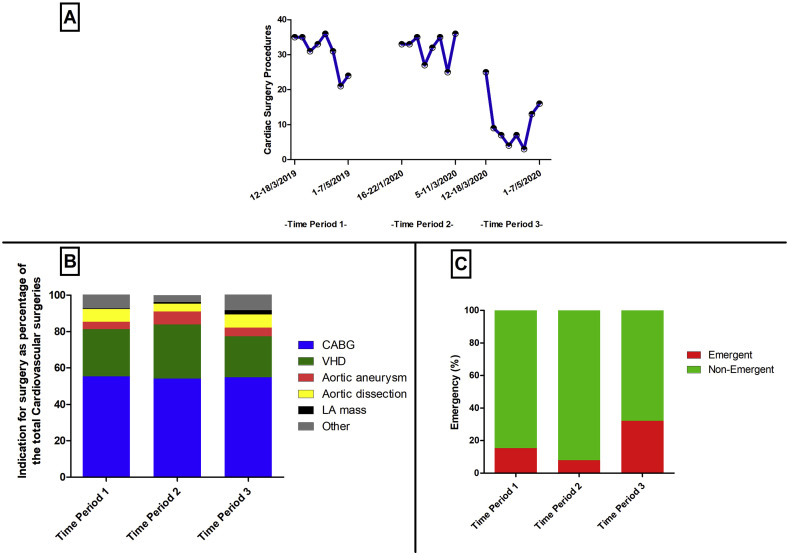
The cumulative number of operations as well as the etiology of the procedure per examined time period are displayed in Table 1 . We observed a significantly lower number of cardiac surgery operations during the period of COVID-19 pandemic (Time period 1: 246 vs. Time Period 2: 253 vs. Time Period 3: 84, p < 0.001) (Fig. 1 A). In contrast, the rate of emergent procedures was greatly increased (Time period 1: 15.5% vs. Time Period 2: 7.9 vs. Time Period 3: 32.1, p < 0.001) (Fig. 1C). As far as the indication for the operation was concerned, no major differences were observed in the underlying etiologies for cardiosurgical procedures (namely coronary artery bypass grafting, valvular heart disease, aortic diseases, left atrial mass, etc.) (Fig. 1B).
Table 1.
Comparison of cardiac surgery procedures between preCOVID-19 outbreak time period (Time Period 2), COVID-19 outbreak time period of 2020 (Time Period 3) and the equivalent time period of 2019 (Time Period 1).
| Time Period 1 (12/3/2019-7/5/2019) | Time Period 2 (16/1/2020-11/3/2020) | Time Period 3 (12/3/2020-7/5/2020) | % change | p | |
|---|---|---|---|---|---|
| Number | 246 | 253 | 84∗,† | −67% | <.001 |
| Age (years) | 66.8 ± 10.1 | 66.2 ± 11.0 | 64.5 ± 13.1 | .27 | |
| Male gender (%) | 168 (68.5) | 188 (73.4) | 65 (77.4) | .24 | |
| Emergency (%) | 38 (15.5) | 20 (7.9)∗ | 27 (32.1)∗,† | +26% | <.001 |
| Procedure type | |||||
| CABG (%) | 136 (55.3) | 138 (54.1) | 46 (54.8) | −67% | .37 |
| VHD (%) | 64 (26.0) | 76 (29.8) | 19 (22.6) | −75% | |
| Aortic aneurysm (%) | 10 (4.1) | 18 (7.1) | 4 (4.8) | −78% | |
| Aortic dissection (%) | 17 (6.9) | 11 (4.3) | 6 (7.1) | −45% | |
| LA mass (%) | 1 (0.4) | 2 (0.8) | 2 (2.4) | 0% | |
| Other (%) | 18 (7.3) | 10 (3.9) | 7 (8.3) | −22% | |
COVID-19: coronavirus disease, CABG: coronary artery bypass grafting, LA: left atrial, VHD: valvular heart disease.
Denotes statistically significant result (p < 0.05) in comparison to Time Period 1.
Denotes statistically significant result (p < 0.05) in comparison to Time Period 2% change denotes numerical differences in cases between Time Period 2 and Time Period 3.
Fig. 1.
Data from cardiac surgery departments before and during the time of COVID-19 outbreak in Greece. Panel A: Cardiac surgeries according to date before and during the COVID-19 outbreak in Greece. Panel B: Etiology of cardiac surgeries as a percentage of the total cardiac surgeries according to date before and during the COVID-19 outbreak in Greece. Panel C: Cardiac surgeries according to emergency before and during the COVID-19 outbreak in Greece.
In our retrospective analysis, we detected a significant drop in the number of cardiac surgeries performed in 2 large-volume hospitals of Athens, Greece, during the period of COVID-19 pandemic, when compared with an equivalent time period of 2020 before the COVID-19 outbreak or to an equivalent time period of 2020. Conversely, the percentage of emergency operations rose dramatically.
It is emphasized that the postponement of surgical procedures as part of the public health policy for COVID-19 spread prevention, has resulted in a significant increase of emergent cardiac surgical operations and a concomitant dramatic reduction of the elective procedures. However, because of the nature of cardiovascular diseases, the lack of prompt guideline-directed surgical management may account for catastrophic consequences (i.e., ruptured aortic aneurysm and acute aortic dissection), leading to an emergency operation (Table 2 ).
Table 2.
Key public health issues arose from the lockdown measures for COVID-19 outbreak on cardiac surgery procedures.
|
|
|
|
In conclusion, the COVID-19 pandemic has resulted in considerable delays and reduced overall number of cardiac surgical procedures due to the implementation of restrictive measures in the healthcare facilities. Future studies should address the impact of such delays on the morbidity and mortality of patients needing cardiac surgery.
Funding
None received.
Acknowledgments
None.
Footnotes
Peer review under responsibility of Hellenic Society of Cardiology.
References
- 1.Burki T.K. Coronavirus in China. Lancet Respir Med. 2020;8:238. doi: 10.1016/S2213-2600(20)30056-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hui D.S., Azhar E.I., Madani T.A. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health - The latest 2019 novel coronavirus outbreak in Wuhan, China. Int J Infect Dis. 2020;91:264–266. doi: 10.1016/j.ijid.2020.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.da Fonseca V.B.P., De Lorenzo A., Tura B.R., Pittella F.J.M., da Rocha A.S.C. Mortality and morbidity of patients on the waiting list for coronary artery bypass graft surgery. Interact Cardiovasc Thorac Surg. 2018;26:34–40. doi: 10.1093/icvts/ivx276. [DOI] [PubMed] [Google Scholar]
- 4.Filis K., Tsioufis C., Sianou A., Triantafillou K., Sigala F., Galyfos G. Critical evaluation on proper antithrombotic treatment in different groups of patients undergoing vascular surgery. Hellenic J Cardiol. 2018;59:313–316. doi: 10.1016/j.hjc.2018.04.006. [DOI] [PubMed] [Google Scholar]
- 5.Dragasis S., Liakos C.I., Kafkas N. Radial artery as a graft for coronary artery bypass surgery in the era of transradial catheterization. Hellenic J Cardiol. 2018;59:150–154. doi: 10.1016/j.hjc.2018.01.009. [DOI] [PubMed] [Google Scholar]
- 6.Xu Y., Li Y., Bao W., Qiu S. MIDCAB versus off-pump CABG: Comparative study. Hellenic J Cardiol. 2019 doi: 10.1016/j.hjc.2018.12.004. [DOI] [PubMed] [Google Scholar]