Abstract
The SARS-2 pandemic which has moved with frightening speed over the last 5 months has several synergies with another older, and far more neglected airborne disease, tuberculosis. Patients with tuberculosis are not only more likely to be infected by SARS-CoV-2 but also likely to have adverse outcomes once infected. The sequelae of more severe forms of COVID-19 in patients who have recovered from TB but have residual compromised lung function, are also likely to be devastating. These diseases share almost identical bio-social determinants like poverty, overcrowding, diabetes and pollution and some clinical similarities. The consequences of the COVID-19 pandemic, and our global response to it with lockdowns, are likely to leave a profound and long-lasting impact on TB diagnosis and control, potentially leading to an additional 6.3 million cases of TB between 2020 and 2025, and an additional 1.4 million TB deaths during this time. Novel solutions will need to be urgently devised or else TB control targets will never be met and indeed may be set back by 5–8 years.
Keywords: COVID-19, Tuberculosis, Synergistic effects, MDR-TB, SARS-CoV-2
“We live in evolutionary competition with microbes: bacteria and viruses. There is no guarantee that we will be the survivors.”
Joshua Lederberg, Nobel Prize winning molecular biologist.
1. Introduction
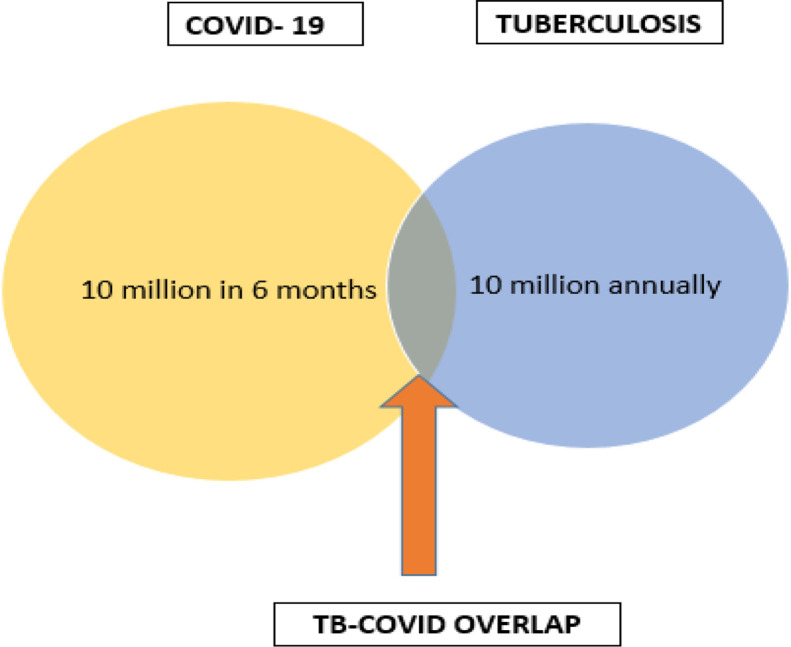
This article looks at the looming impact and interactions of two airborne diseases: one as old as human civilization itself, the other unknown to the world till a few months ago. Tuberculosis is, of course, a destroyer of large swathes of humanity over the centuries and, according to latest estimates, one which has latently infected approximately 2 billion people, caused active infection in 10 million annually, and killed 1.5 million in 2018 globally. The COVID-19 epidemic caused by the novel SARS-CoV-2 virus, since being declared a pandemic, has infected around 15 million people globally and resulted in almost half a million deaths: frightening speed for a disease that was unknown 6 months ago. These two respiratory epidemics are bound to collide and impact one another (Fig. 1 ) adversely, and the objective of this review is to look at this interaction, and the dual epidemic that will ensue.
Fig. 1.
TB-COVID-19 overlap.
2. Are patients with TB at increased risk of infection and negative outcomes from COVID-19?
A consistent finding in this pandemic is that patients with co-morbidities are more likely to be afflicted by the virus. A meta-analysis of 8 studies and 46,248 patients with confirmed COVID-19 infection by molecular diagnostics showed that co-morbidities were powerful predictors of the need for hospitalization and poor outcomes. Patients with pre-existing chronic respiratory disease were more than two times more likely to be infected (odds ratio of 2.46).1 An observational study from the epicenter of the pandemic in Wuhan, suggested that individuals with latent or active TB were more susceptible to SARS-CoV-2 infection.2 They found infection with Mycobacterium tuberculosis to be a more common co-morbidity for COVID-19 (36%), than diabetes (25%), hypertension (22%), ischaemic heart disease (8%) and COPD (6%). They also found M. tuberculosis co-infection to be linked to more severe COVID-19 and more rapid progression. Although this study was limited by its small size and observational nature, it showed the first tantalizing links between TB and COVID-19. Of the 36 COVID-19 cases in their series 36% had a positive interferon-γ release assay (IGRA) test result, 3 had active TB (1 MDR-TB), and 5 were recovered TB patients with 3 demonstrating old TB calcifications on chest scans. The percentage of COVID-19 patients with positive IGRA test results was approximately double compared to the estimated frequency of latent TB infection (LTBI) with M. tuberculosis in the general population in rural China, which is approximately 15–18%. Despite the small sample size, this study raises the concern that LTBI is likely to be an important independent risk factor for susceptibility to SARS-COV-2 infection.
3. Shared bio-social determinants
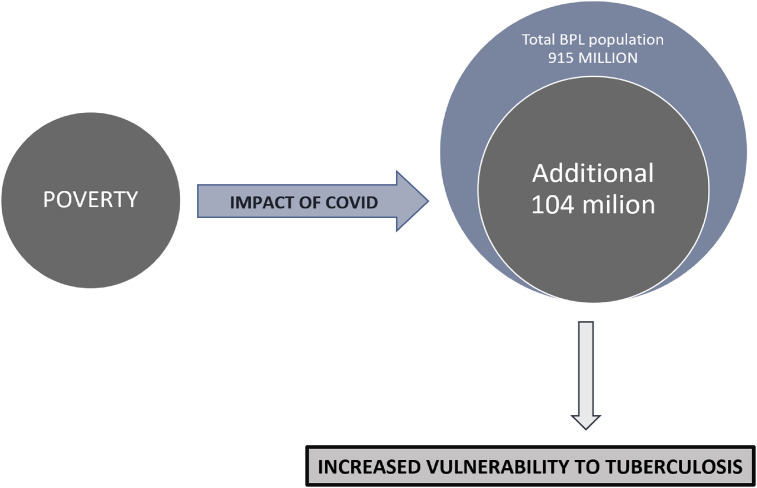
TB and COVID-19 share many common bio-social determinants as shown in Fig. 2 . Some of the major ones are discussed in this section.
Fig. 2.
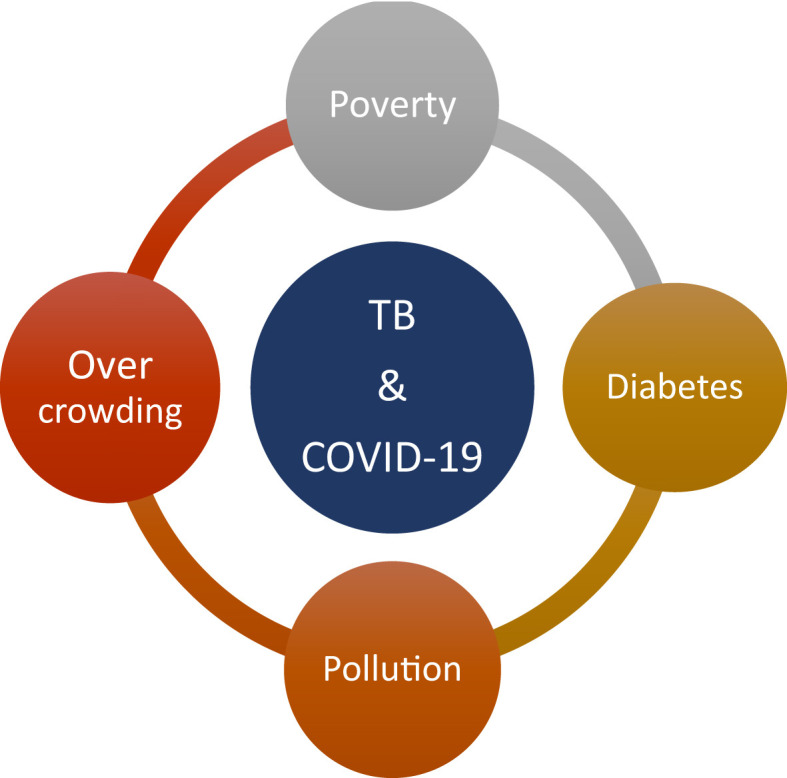
Shared BIO-SOCIAL determinants.
3.1. Poverty
COVID-19 has already cruelly exposed the fault lines between rich and poor. The link with poverty is an example of this bi-directional interaction between COVID-19 and TB. A recent analysis by researchers at the United Nations University (UNU) show that the economic downturn due to COVID-19 and the lockdown is likely to tip 104 million additional Indians to below the World Bank-determined poverty line of $3.2 a day for lower-middle-income countries.3 In effect, this would swell the ranks of India's poorest to 915 million, increasing the proportion of Indians currently below the poverty line from 60% to 68%, levels last seen in the country more than a decade ago. This increase in the population living in poverty due to Coronavirus could then exacerbate increased numbers of patients with TB (Fig. 3 ).
Fig. 3.
Impact of COVID-19 on poverty in India and resulting increased vulnerability to TB. (BPL: below poverty line).
3.2. Overcrowding
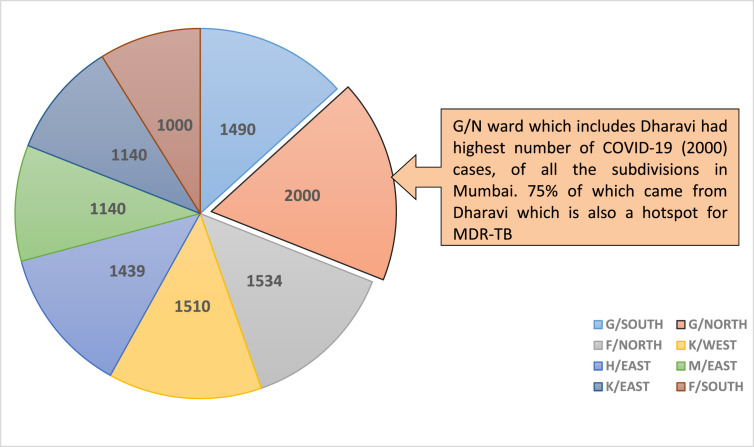
Overcrowding is another major risk factor for both airborne diseases. A staggering 60% of all patients with COVID-19 in India have been reported in five of India's most overcrowded cities: Mumbai, Delhi, Ahmedabad, Chennai and Pune. Mumbai is the worst hit, accounting for almost 20% of all the cases in India. Interestingly this city is also the epicenter of India's TB and MDR-TB epidemic. Even within Mumbai, the ward (district) with the highest number of patients with COVID-19 is Dharavi (G/North Ward), the site of Asia's most densely populated slum. This is also the ward in Mumbai (Fig. 4 ) with the highest TB prevalence rates in the city. Thus COVID-19 and TB both target and expose the same groups of vulnerable populations.4
Fig. 4.
Ward wise COVID-19 patients in Mumbai.
3.3. Pollution
Air pollution has long been a risk factor for pulmonary TB. It is now recognized to be equally important for COVID-19 infection. A study looked at COVID-19 fatalities in four of the countries that have been hit hardest by the virus: Germany, France, Italy and Spain found 78% of deaths occurred in five regions in northern Italy and Spain, which were also the most heavily polluted.5
3.4. Diabetes
Diabetes has emerged as a major co-morbidity for COVID-19 as it has long been for tuberculosis. Whilst diabetic patients have a significantly high risk of developing active TB,6 it has also emerged as a major comorbidity for COVID-19 patients. A recently published meta analyses of 6452 patients from 30 different studies showed that diabetes was consistently associated with poor composite outcomes in COVID-19 patients (relative risk, RR, 2.38, p < 0.001). Diabetes also emerged as a major predisposing factor for death (RR 2.12) for severe COVID-19 (RR 2.45), and for ARDS (RR 4.64).7
4. Effects of COVID-19 on TB
The link between TB and COVID-19 is likely to be bi-directional. The temporary immunosuppression induced by tuberculosis may increase the susceptibility of patients to COVID-19, and COVID may, in turn, also increase susceptibility to TB. In a study from Wuhan, 76% of 522 COVID-19 patients had significant depletions in their T-cell lymphocyte counts.8 Both CD4 and CD8 counts were severely reduced, and the surviving T cells appeared to demonstrate “functional exhaustion”. This T cell depletion and dysfunction may promote the development of active TB in patients with LTBI.
4.1. COVID-19 is likely to have both direct and indirect effects on patients with TB
4.1.1. Direct effects
Large numbers of patients who have TB or have recovered from it are left with fibrotic scarred lungs, compromised lung function and the effects of COVID-19 can be particularly devastating in this patient population. It is estimated that more than half of all TB survivors have some form of persistent pulmonary dysfunction (both obstructive and restrictive) despite microbiological cure, leaving millions of patients potentially more susceptible to the effects of superimposed COVID infection.
5–10% of patients with COVID-19 develop severe ARDS, needing prolonged ICU stay with ventilator and subsequent oxygen requirement. Because we are a only few months into the pandemic, it remains unclear as yet what the long-term consequences of severe COVID-19 may be but it is likely that significant numbers of these patients may be left with some degree of pulmonary fibrosis. In a study done on 70 patients with COVID pneumonia, serial CT scans revealed that the majority (94%) of patients had mild to substantial residual abnormalities on their last CT scan done just prior to discharge, a median of 24 days from symptom onset.9 Whilst the most common CT pattern observed was ground glass opacities (GGO's), a range of other interstitial patterns was also observed. Whilst further serial follow ups will be needed, these findings suggest significant numbers of patients could be left with residual fibrosis. In most autopsy series published to date, the most common lung finding in patients who have died from COVID-19 is diffuse alveolar damage (DAD), a pattern of lung injury seen in ARDS from many other causes. This post-COVID pulmonary fibrosis, superimposed on the fibrosis caused by the sequelae of pulmonary TB, is likely to result in even more devastating disability.
4.1.2. Indirect effects
Of equal concern are the indirect effects COVID-19 will have on TB. On March 24th the Indian prime minister announced a sudden and complete nationwide lockdown which now represents the largest and longest lockdown of any population in history. Hospitals and clinics took on the responsibility of treating COVID-19 patients, relegating most other diseases to the sidelines. At the Hinduja Hospital, a large and very busy tertiary care hospital where some of us practice, the total number of OPD visits fell by 85% from 32,000 in the month of April 2019 to just 4800 in April 2020. It is likely that TB patients are likely to face great hardships at this time with reduced access to diagnostic and treatment services. They are less likely to venture out of their houses to visit chemists, DOTS centers, and private doctors. TB notification rates have, as a consequence, fallen greatly across the country. In India, weekly counts of reported cases dropped by 75% in the 3 weeks following lockdown commencement (March 24th) compared to an average of 45,875 weekly cases during the previous weeks of 2020.10 This drop was attributable to a combination of factors including delays in entering the data onto the real-time national online TB surveillance system, reduced attendance to health services, reassignment of health personnel, and a reduction in TB testing and detection. China reported similar reductions of 20% in the national TB case detection rate in February 2020, when the pandemic first commenced, compared to February 2019.10 The pandemic and the prolonged lockdown which was the response to it, adversely affects every aspect of TB care. Irregular, erratic, unsupervised and uninterrupted treatment is likely to occur which is the recipe for treatment failure and possible amplification of drug resistance.
A study commenced by the STOP TB Partnership in collaboration with Imperial College and Johns Hopkins University modeled that each month of lockdown in India could cause an additional 40,685 cases annually from TB over the next 5 years adding up to a total of 151,120 (5.7%) increase in TB deaths in India.11 The study also estimated that in India, patient care seeking delays would increase by 50%, probability of diagnosis per visit to provider would drop by 70% and MDR-TB completion rate in the public or any engaged private sector would drop to as low as 25%.
5. Clinical similarities and differences between COVID-19 and TB
Whilst tuberculosis and COVID-19 are both transmitted by the airborne route it generally takes more prolonged contact with an infected patient to spread TB unlike SARS-CoV-2 which is more easily transmitted. Both diseases share the three cardinal symptoms of cough, fever and breathlessness. As our knowledge of COVID-19 grows we have begun to realise that apart from the upper and lower respiratory tract a host of other organ systems can also be affected (as in TB) along with some unique and distinctive symptoms like anosmia and ageusia.
The most immediate difference is of course in the speed of onset and progression. Unlike COVID-19 where symptoms generally occur within a median of 5 days of exposure to an infected case, the symptoms of TB, when they develop, are generally of a more gradual onset, and progress over a period of weeks or months. Infection with M. tuberculosis may uniquely manifest only as LTBI wherein the bacilli remain quiescent in the body and the patient is asymptomatic and non-infectious to others. This state of infection is indirectly defined by the presence of a positive IGRA or tuberculinskin-test and it is assumed that the majority of individuals with LTBI will never develop TB within their lifetime.
Another interesting difference is that SARS-CoV-2 can be spread by a patient who is asymptomatic and looks and feels well, unlike TB where the index case is almost always symptomatic and unwell. The bacterial burden builds up during weeks to months in active TB as opposed to SARS-CoV-2 where the viral load peaks within days.12 Despite these differences and perhaps because of the more chronic and gradual nature of initial TB symptoms, the basic reproductive number (R0 value), defined as the expected number of secondary cases produced by a single infectious case in a completely susceptible population is around 3.55 to 4.3 for TB whilst it is reported to be 2.2 for SARS-CoV-2.13
Despite the global panic caused by the novel coronavirus, its mortality at this stage of the pandemic is felt to be around 2–5% whilst untreated TB is by far the more deadly disease carrying a mortality of close to 50%. Certain forms of tuberculosis like miliary TB and TB meningitis are even more fulminant and invariably fatal if left untreated with mortalities far higher than even the highest projected mortality estimates for COVID-19.
Of course, a major difference is that whilst drugs to treat TB have been around for over 75 years, at this early stage of the pandemic apart from remdesivir (which improves time to clinical improvement but does not impact mortality),14 and dexamethasone (which has been shown to decrease mortality).15 We have no effective drugs for SARS-CoV-2. Some of these clinical differences are highlighted in Table 1 .
Table 1.
Comparison of TB and COVID-19.
| TB | COVID-19 | |
|---|---|---|
| How it is spread | Airborne | Droplet spread |
| How it is diagnosed | Sputum tests for those with cough. Other samples depending on symptoms and site of infection | Nasal & throat swabs and/or sputum tests |
| Pathogen | Mycobacterium tuberculosis complex | Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) |
| Size | 2–4 micrometres in length and 0.2–0.5 um in width | 65–125 nm in diameter |
| Infectiousness (R0) | 3.55–4.3 people infected per one person with TB | Currently average of 2.2 people infected per one person with COVID-19 |
| Prevalence (India) | 186.6 to 295.9/1 lakh population (2.2 million cases/year) | Approximately 94,000 active cases; Total cases 1,91,000 (as of June 1,2020) |
| Average daily cases (India) | 7370 | 1331 |
| Average deaths/day (India) | 1230 | 38 |
| Prevention | Prevention measures include TB preventive therapy for those with known contacts with TB and good respiratory hygiene measures | Social distancing, good respiratory hygiene measures and handwashing with soap for at least 20 seconds |
| Treatment | Antibiotics. Drug-sensitive TB for 6–12 months Drug resistant TB for 9–24months |
Supportive treatments currently. Many drug trials under way |
| Vaccine | BCG has some protective effects particularly for children | Trials ongoing |
6. BCG vaccine: established in TB, possible role in COVID 19
Since its introduction, over a century ago, M. bovis Bacille Calmette Guérin (BCG) remains the most widely used and safe vaccine in the world, having been given to over 4 billion individuals to date. BCG vaccine has several, beneficial, off-target effects on the immune system, conferring protection against a wide spectrum of respiratory viruses, bacteria and parasites. A 25 year study of 150,000 children in 33 countries16 showed respiratory tract infections were reduced by 40% in BCG vaccinated children. The vaccine has also been shown to reduce the severity of infections by viruses with identical structure to that of SARS-CoV in controlled trials.17 Miller and colleagues first raised the intriguing epidemiological hypothesis that countries with universal BCG vaccine in place seemed to have reduced mortality from COVID-19.18 Of course, such interpretation of ecological data is weak and circumstantial, being based on population rather than individual data, and being prone to confounding, cannot hope to provide definite proof of causality. Despite this, the hypothesis is seen to have enough merit for clinical studies in health care workers and in the elderly population in Germany to investigate whether the vaccine candidate VPM1002, a BCG based vaccine is also effective against SARS-CoV-2.19 Clinical trials are also underway in Australia and The Netherlands: the BCG-CORONA trial (Reducing health care workers absenteeism through BCG vaccine)20 and the BRACE trial (BCG vaccination to protect healthcare workers against COVID-19).21 Whilst the results of these trials are eagerly awaited, the WHO has released a cautionary statement recommending against the use of BCG vaccine for the prevention of COVID-19 outside of clinical trials. The statement cautions that BCG is already in short supply globally, and diverting BCG from TB to COVID-19 might result in neonates not getting the BCG vaccine where it's use is long established in, protecting children from contracting disseminated TB and meningitis.
7. Diagnostic similarities between TB and COVID-19
The RT-PCR test is highly specific, but sensitivity is dependent on the time of testing and the type of specimen. RT-PCR positivity is highest in bronchoalveolar lavage specimens (93%) followed by sputum (72%), followed by nasal swab (63%) and pharyngeal swab (32%).22
Testing all suspects and their contacts is one of the main tenets of public health for containing the pandemic, but in most countries testing capacity has fallen woefully short. As of 19th May, India's tests per million population remains one of the lowest in the world, at 1700/million per head of population, compared to 29,412 for the U.K., 50,381 for Russia and 51,347 for Italy.23 Despite the low testing, the number of cases in India has been steadily increasing and crossed the 1.5 million mark recently.
As a part of its efforts to scale up testing capacity and speed, the Indian Council of Medical Research (ICMR) recommended on April 10th, that the machines used for diagnosing drug resistant tuberculosis: TrueNAT and GeneXpert, be utilised for screening and confirmation of COVID 19 cases.24 Since then, nearly 130,000 screening tests for SARS-CoV-2 have already been done using these machines. The TrueNat machine when used for SARS-CoV-2 testing involves a two step process with samples screened first for the E and then, if positive, for the RdRp gene targets. The GeneXpert platform screens for E and N2 gene targets in a single step. Thus, a commonly used TB platform is doubling up to help diagnose SARS-CoV-2 with almost point of care (POC) speed. Yet another example of shared ground between TB and COVID-19. India has large numbers off GeneXpert and TrueNat machines and already conducts in excess of 100,000 of these tests for TB a day. The rapid turnaround time (1 hour with the TrueNat and 40 minutes with the GeneXpert) and the use of a platform familiar to labs across the country are clear advantages which will help to considerably boost testing capabilities for SARS-CoV-2. TB experts and activists are however concerned at yet another shift in focus from TB to COVID-19. Although India aims to eliminate TB by 2025, the present political and economic focus on COVID-19 has already result in a shift in priorities.
Thus COVID-19 will affect TB diagnosis by all of a combination of: 1) Delayed health seeking due to restriction of patient movements during lockdown, 2) Reduced availability of health care staff, and 3) Xpert and TrueNat TB machines and other lab facilities being used for COVID response. Modelling experts believe this combination will reduce the probability of TB diagnosis per visit to a provider by 70% across India.11 Large numbers of missed cases are likely to occur, the full impact of which will only be apparent in the months ahead. Because normal TB services will be unable to reduce this expanded pool rapidly to pre-lockdown levels, these cases will continue to contribute to transmission for years to come.
8. Treatment
Of all the achievements in medicine, the successful treatment with chemotherapy of tuberculosis has been the one with the greatest impact on society. Since the first anti-TB drug, streptomycin was discovered in 1945, a number of anti-TB medications have been developed over the last 70 years and used in combination therapy regimens. The recent discovery of newer agents like bedaqualine, delamanid and pretomanid have further improved the outlook of patients with MDR-TB. For SARS-CoV-2 by contrast, at this early stage of the pandemic, apart from remdesivir which improves time to clinical improvement,14 there are no effective agents available as yet.
TB treatment is no different in people with or without COVID-19 infection. Patients on anti-TB drugs whether for latent TB, drug sensitive TB or MDR-TB should continue their treatment, uninterrupted, even if they acquire COVID-19, to increase chances of cure and reduce transmission and development of drug-resistance. Experience on co-management of both COVID-19 infection and TB remains limited but two important drug interactions between TB drugs and COVID therapies need to be highlighted. Lopinavir/ritonavir a widely used antiretroviral drug combination has recently received attention for its possible role in the treatment of SARS-CoV-2. When used with rifampicin there is a drug interaction which can potentially increase rifampicin levels resulting in serious hepatotoxicity.25 When co-administered, the lopinavir levels and hence efficacy may also be reduced. Lopinavir/ritonavir also significantly increases the levels of bedaquline resulting in QTc prolongation and increased risk of cardiac arrhythmias.26 Careful ECG monitoring is recommended if these drugs must be co-administered.
9. Possible solutions
9.1. Telemedicine
Digital health interventions are changing healthcare delivery globally and are increasingly being used to support TB treatment in diverse settings. As the COVID-19 pandemic spreads globally, more countries are putting in place containment and mitigation strategies to stop the transmission of the virus and to ease the burden on health systems. The disruption in routine health services and the need for social distancing has posed a significant challenge for TB programmes to carry out routine operations and to provide the necessary care for people and communities affected by TB. Thus, TB programmes need to rely on alternative options, such as digital health technologies, including virtual care and community-monitoring solutions, to rapidly bring required TB services to the people and communities affected. Confronted with the largest and longest lockdown in history in India, travel restrictions made it impossible for our regular TB patients to travel to reach us for their routine check-ups and collection of novel life-saving medicines, like bedaquiline. Our response at the Hinduja Hospital where we run an MDR-TB clinic has been to convert to telemedicine in an attempt to ensure continuity of care, recognising that irregular and interrupted treatment is a recipe for amplification or resistance. We found it is possible to use telemedicine to virtually assess patients’ symptoms, enquire about and manage adverse drug reactions, ensure compliance with their complex drug regimens, and give precautionary advice regarding measures to be taken to keep them safe from COVID-19. When questioned, 70% of our patients actually preferred the convenience of this form of follow up to in-person visits, as it saved travel time and long waiting hours in the OPD.27
9.2. Programmatic
TB programs must prepare themselves for major difficulties ahead as a consequence of the COVID-19 pandemic and it is anticipated that the effects on these patients will be devastating. Up to 6.3 million more people are predicted to develop TB between now and 2025 and 1.4 million additional deaths expected as cases go undiagnosed and untreated during lockdown. This is likely to set back global efforts to end TB by 8 years according to modelling data released by Stop TB.11 Whilst the level of individualised personal care we have tried to provide for each TB patient with telemedicine is difficult to scale up to programmatic level, there are a number of suggestions that can apply to patients being managed in TB programmes. These are tabulated in Table 2 .
Table 2.
Programmatic considerations for TB patients in the days of COVID.
| Ensure proper communication by using virtual means |
| Early procurement and careful planning of local drug distribution and transportation |
| Use appropriate digital adherence and support tools |
| Ensure necessary psycho-social, nutritional and economic support |
| Shift to injection-free all-oral MDR-TB regimen |
| Telemedicine where possible at least to manage adverse events |
| Family member as treatment supporter |
10. Concluding remarks
The impact of a novel viral infection, SARS-CoV-2, on an ancient bacterial disease, tuberculosis, is likely to be devastating. Just as another virus, HIV did to TB control more than 3 decades ago, the effect of SARS-CoV-2 is likely to be set back global TB control by several years. With both diseases sharing common bio-social predispositions, the impact to TB patients and programmes is likely to be most acutely felt in the developing world. This article looks at synergies and differences between these two diseases and explores solutions that may help mitigate the impact of COVID-19 on tuberculosis.
Conflicts of interest
The authors have none to declare
References
- 1.Yang J., Zheng Y., Gou X., et al. Prevalence of comorbidities and its effects in coronavirus disease 2019 patients: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–95. doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu Y., Bi L., Chen Y., et al. Active or latent tuberculosis increases susceptibility to COVID-19 and disease severity. medRxiv. March 2020 doi: 10.1101/2020.03.10.20033795. 2020.03.10.20033795. [DOI] [Google Scholar]
- 3.lockdown: World's biggest lockdown to push 12 million into extreme poverty - The Economic Times. https://economictimes.indiatimes.com/news/economy/indicators/worlds-biggest-lockdown-to-push-12-million-into-extreme-poverty/articleshow/76056756.cms?from=mdr. Accessed June 2, 2020.
- 4.Drug resistant TB flourishes in Govandi, Dharavi; cases spiral to 2,500 across Mumbai | Mumbai News - Times of India. https://timesofindia.indiatimes.com/city/mumbai/Drug-resistant-TB-flourishes-in-Govandi-Dharavi-cases-spiral-to-2500-across-Mumbai/articleshow/26009006.cms. Accessed June 2, 2020.
- 5.Ogen Y. Assessing nitrogen dioxide (NO2) levels as a contributing factor to coronavirus (COVID-19) fatality. Sci Total Environ. 2020;726:138605. doi: 10.1016/j.scitotenv.2020.138605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arora V.K., Chopra K.K. Journey of tuberculosis control in India. Indian J Tubercul. 2019;66(1):178–183. doi: 10.1016/j.ijtb.2019.02.002. [DOI] [PubMed] [Google Scholar]
- 7.Huang I., Lim M.A., Pranata R. Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia – a systematic review, meta-analysis, and meta-regression: diabetes and COVID-19. Diabetes Metab Syndrome Clin Res Rev. 2020;14(4):395–403. doi: 10.1016/j.dsx.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Diao B., Wang C., Tan Y., et al. Reduction and functional exhaustion of T cells in patients with coronavirus disease 2019 (COVID-19) Front Immunol. 2020;11:827. doi: 10.3389/fimmu.2020.00827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang Y., Dong C., Hu Y., et al. Temporal changes of CT findings in 90 patients with COVID-19 pneumonia: a longitudinal study. Radiology. March 2020:200843. doi: 10.1148/radiol.2020200843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Glaziou P. 2020. Predicted Impact of the COVID-19 Pandemic on Global Tuberculosis Deaths. [DOI] [Google Scholar]
- 11.Stop TB partnership . Dev by Stop TB Partnersh Collab with Imp Coll Avenir Heal Johns Hopkins Univ USAID; 2020. The Potential Impact of the COVID-19 Response On Tuberculosis In High-Burden Countries : A Modelling Analysis; pp. 1–7. [Google Scholar]
- 12.To K.K.W., Tsang O.T.Y., Leung W.S., et al. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study. Lancet Infect Dis. 2020;20(5):565–574. doi: 10.1016/S1473-3099(20)30196-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cascella M., Rajnik M., Cuomo A., Dulebohn S.C., Di Napoli R. StatPearls Publishing; 2020. Features, Evaluation and Treatment Coronavirus (COVID-19) [PubMed] [Google Scholar]
- 14.Beigel J.H., Tomashek K.M., Dodd L.E., et al. Remdesivir for the treatment of covid-19 — preliminary report. N Engl J Med. May 2020 doi: 10.1056/NEJMoa2007764. [DOI] [PubMed] [Google Scholar]
- 15.Horby P., Lim W.S., Emberson J.R., et al. Dexamethasone in hospitalized patients with Covid-19 — preliminary report. N Engl J Med. July 2020 doi: 10.1056/NEJMoa2021436. NEJMoa2021436. [DOI] [Google Scholar]
- 16.de Castro M.J., Pardo-Seco J., Martinón-Torres F. Nonspecific (heterologous) protection of neonatal BCG vaccination against hospitalization due to respiratory infection and sepsis. Clin Infect Dis. 2015;60(11):1611–1619. doi: 10.1093/cid/civ144. [DOI] [PubMed] [Google Scholar]
- 17.Arts R.J.W., Moorlag S.J.C.F.M., Novakovic B., et al. BCG vaccination protects against experimental viral infection in humans through the induction of cytokines associated with trained immunity. Cell Host Microbe. 2018;23(1):89–100. doi: 10.1016/j.chom.2017.12.010. e5. [DOI] [PubMed] [Google Scholar]
- 18.Miller A, Reandelar MJ, Fasciglione K, Roumenova V, Li Y, Otazu GH. Correlation between Universal BCG Vaccination Policy and Reduced Morbidity and Mortality for COVID-19: An Epidemiological Study. doi:10.1101/2020.03.24.20042937.
- 19.Grode L., Ganoza C.A., Brohm C., Weiner J., Eisele B., Kaufmann S.H.E. Safety and immunogenicity of the recombinant BCG vaccine VPM1002 in a phase 1 open-label randomized clinical trial. Vaccine. 2013;31(9):1340–1348. doi: 10.1016/j.vaccine.2012.12.053. [DOI] [PubMed] [Google Scholar]
- 20.Reducing Health Care Workers Absenteeism in Covid-19 Pandemic through BCG Vaccine - Full Text View - ClinicalTrials.Gov.
- 21.BCG Vaccination to Protect Healthcare Workers against COVID-19 - Full Text View - ClinicalTrials.Gov.
- 22.Sethuraman N., Jeremiah S.S., Ryo A. Interpreting diagnostic tests for SARS-CoV-2. JAMA, J Am Med Assoc. 2020 doi: 10.1001/jama.2020.8259. [DOI] [PubMed] [Google Scholar]
- 23.COVID-19 Map - Johns Hopkins Coronavirus Resource Center.
- 24.Machines Used for Testing Drug-Resistant TB Can Be Now Used for Confirming COVID-19 Cases- the New Indian Express.
- 25.Murphy R.A., Marconi V.C., Gandhi R.T., Kuritzkes D.R., Sunpath H. Coadministration of lopinavir/ritonavir and rifampicin in HIV and tuberculosis Co-infected adults in South Africa. PloS One. 2012;7(9) doi: 10.1371/journal.pone.0044793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pandie M., Wiesner L., McIlleron H., et al. Drug–drug interactions between bedaquiline and the antiretrovirals lopinavir/ritonavir and nevirapine in HIV-infected patients with drug-resistant TB. J Antimicrob Chemother. 2016;71(4):1037–1040. doi: 10.1093/jac/dkv447. [DOI] [PubMed] [Google Scholar]
- 27.Udwadia Z., Sharma S., Mullerpatan J.B. 2020. Effective use of telemedicine in Mumbai with a cohort of XDR TB patients on BDQ during COVID-19. doi:Lung India (awaiting publication) [DOI] [PMC free article] [PubMed] [Google Scholar]