Abstract
Background
Resumption of elective surgery during the current coronavirus disease 2019 pandemic crisis has been debated widely and largely discouraged. The aim of this prospective cohort study was to assess the feasibility of resuming elective operations during the current and possible future peaks of this coronavirus disease 2019 pandemic.
Methods
We collected data during the peak of the current pandemic in the United Kingdom on adult patients who underwent elective surgery in a “COVID-19-free” hospital from April 8 to May 29, 2020. The study included patients from various surgical specialties. Nonelective and pediatric cases were excluded. The primary outcome was 30-day mortality postoperatively. Secondary outcomes were the rate of coronavirus disease 2019 infections, new onset of pulmonary symptoms after hospitalization, and requirement for admission to the intensive care unit.
Results
A total of 309 consecutive adult patients were included in this study. No patients died nor required intensive care unit admission. Operations graded “Intermediate” were the most performed procedure representing 91% of the total number. One patient was diagnosed with a coronavirus disease 2019 infection after being transferred to the nearest local emergency hospital for management of postoperative pain secondary to common bile duct stone and was successfully treated conservatively on the ward. No patient developed pulmonary complications. Three patients were admitted for greater than 23 hours. Twenty-seven patients (8.7%) developed complications. Complications graded as 2 and 3 according to the Clavien-Dindo classification occurred in 14 and 2 patients, respectively.
Conclusion
This prospective study shows that, despite the severity and high transmissibility of novel coronavirus 2 disease, COVID-19-free hospitals can represent a safe setting to resume many types of elective surgery during the peak of a pandemic.
Introduction
The current pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has spread rapidly across the world affecting more than 114 countries,1 leading to the rapid increase in demand to create capacity across health care systems already overstretched in many areas. The world had to change suddenly the way health care was provided. Such relevant changes occurred primarily in the critical care setting, such as the intensive care unit (ICU) and high dependency units. Subsequently, numerous guidelines were published that advised postponing or cancelling elective surgical services.2 , 3 , 4 , 5 , 6 , 7
The aim of these extreme measures was to protect not only the patients from in-hospital viral transmission and associated postoperative respiratory complications but the health care workers as well. Health care professionals from surgeons to radiology technicians were also being freed and redeployed to support other specialties in high demand. The cancelling of elective procedures meant a large backlog of cases. The CovidSURG Collaborative Group projected that the total number of adult elective operations cancelled worldwide has been 28,404,603 during the 12 week peak (2,367,050 per week), accounting to over 2,000,000 per week.8 Given this, there was even more pressure on services to resume elective surgery, including urgently needed operations such as cancer cases. To meet this demand, the National Health Service (NHS) England and NHS Improvement in collaboration with the Independent Healthcare Providers Network collectively reached a national agreement with health care providers in the private sector to secure all available capacity in England. In particular, local agreements were established to facilitate resuming NHS elective surgical services.9 The Royal College of Surgeons of England also advocated creating “COVID-19-free” sites at private hospitals where possible.2
Although limited, the evidence surrounding the continuation and the resumption of elective services has not been positive so far. A recent global study published in The Lancet by A Bhangu et al showed an overall mortality rate of 18.9% in patients who underwent elective surgery and who were diagnosed with SARS-CoV-2 infection preoperatively. Furthermore, the total rate of respiratory complications for both emergency and elective operations was found to be as high as 51.7%. As a result, the authors suggested that noncritical procedures should be postponed.10 A second retrospective study reported the outcome of patients who underwent elective surgeries at hospitals in China. All 34 patients were postoperatively diagnosed with SARS-CoV-2 infection and 7 died.11 It is important to note that both these studies reported patient outcomes derived from centers that were not COVID-19-free.
We present here the first study showing prospective data on planned elective surgery performed in a COVID-19-free hospital during the peak of the novel coronavirus pandemic. We aim to demonstrate that with rigorous patient selection and strict protocols it can be safe to resume elective surgery in dedicated COVID-19-free hospitals.
Materials and methods
Design
This single center, prospective, observational study includes patients who were admitted and underwent any type of elective operation at a private hospital, the BMI Chiltern Hospital (BMI CH), between April 8, 2020 and May 29, 2020. All the data collected for the study were routine with no change to clinical practice. All elective operations in adult patients during this time were included. Nonelective and pediatric cases were excluded. The project was registered with the Clinical Effectiveness Department at Stoke Mandeville Hospital under the reference PCG014. It was deemed that ethical approval was not required for this study. This study was also registered in the Research Registry #5780.
Evidence before this study
We searched MEDLINE (PubMed) regularly while writing this manuscript to ascertain that this was the first study to report on elective surgery performed in a COVID-19-free hospital. Key words included “elective surgery,” “COVID-19,” and “non-urgent surgery.” Key words were combined using Boolean Operators, and MeSH terms were exploded throughout. All abstracts generated from the search were read and full-text publications of those abstracts meeting the search criteria on initial screening were reviewed by all 4 authors to confirm no studies reporting on elective surgery in COVID-19-free hospitals were missed.
COVID-19-free hospital
The definition of a COVID-19-free hospital we chose comprises a “COVID-19-free building” where there are no inpatients with suspected or proven SARS-CoV-2 infections. However, if necessary, it was possible to allow patients to remain overnight. Sufficient space must be available to allow for social distancing between patients. In our COVID-19-free hospital, every patient was allocated a single occupancy room with en-suite facilities. No accompanying persons were allowed into the hospital with the patients. Furthermore, all nonmedical health care professionals working at our COVID-19-free hospital were employees at the BMI CH and did not work in any other NHS facilities, theoretically with minor work-related exposure risk to the coronavirus compared with frontline staff who had been working at COVID-19-hot sites. The only staff members who could be potentially exposed in their workplace to the novel coronavirus were operating surgeons and anesthesiologists who were also working in other settings.
In order to limit the number of these health care professionals into the BMI CH, only senior trainees and consultants were permitted to deliver services at the COVID-19-free site. In accordance with local government guidelines, all staff members wore dedicated scrubs for sessional use while at the COVID-19-free hospital.12 No uniforms were worn outside of the clinical settings or when traveling. Utilization of the increased shower facilities was encouraged to further minimize infection risk. In addition, health care professionals were screened for symptoms and temperature on entrance to the hospital. Staff were excluded if they failed that screen and directed to NHS testing facilities and isolation as per government protocols. Staff did not return to work at any site until they were cleared from an occupational health viewpoint and had isolated for the required time. No formal asymptomatic staff testing was undertaken. The term COVID-19-free refers to patients only and does not include potentially asymptomatic health care professionals.
Patient selection
A total of 309 consecutive adult patients age 18 and over who underwent any elective operative procedure performed in an operating theater under general or local anesthetic were included in this analysis. This study includes patients from various specialties including breast surgery, urology, pain service, general surgery, trauma and orthopedics, plastic surgery, gynecology, and ear, nose, and throat surgery.
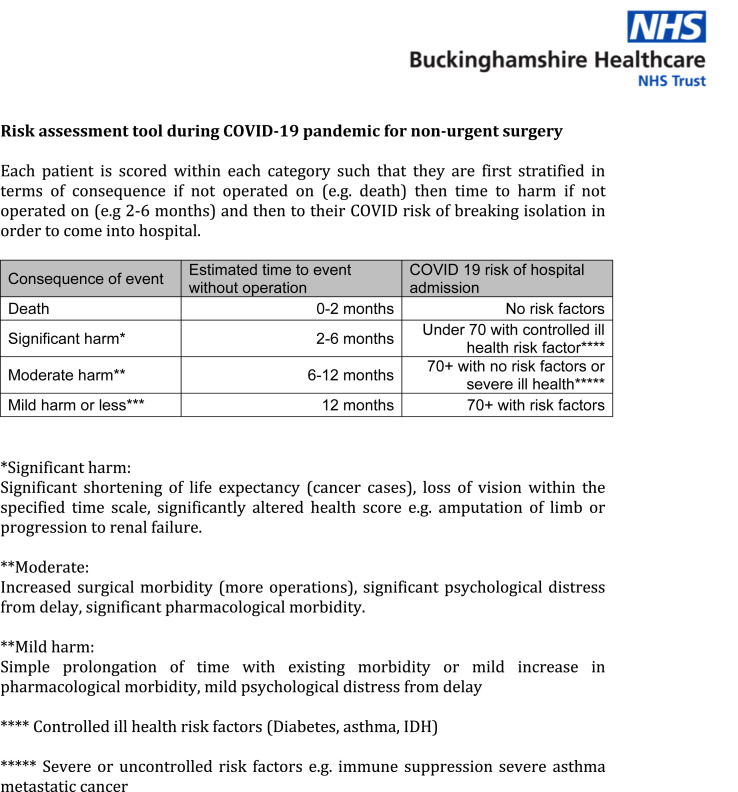
Cases were chosen from a traffic-light-based system derived from a risk stratification tool developed by the surgical leads from each specialty (Fig 1 ). All cases were vetted by the most senior operating clinicians who had final approval on chosen cases based on urgency, practicality, and those that could be carried out as day-cases or 23-hour stays. All cases included were also deemed low risk for complications
Fig 1.
Risk assessment tool during COVID-19 pandemic for non-urgent surgery.
A rigorous and well-established patient selection pathway was designed. Patients considered for an operation in this setting were contacted by telephone by their named consultant to explain the procedure and to elicit their consent and ensure suitability. Patients were asked if they experienced recently any of the most common clinical features of a COVID-19 infection, such as any fever, cough, dyspnea, myalgia, anosmia, or other respiratory symptoms.13 Moreover, we investigated if they were cohabiting with anyone who suffered symptoms of COVID-19 or who was self-isolating as per governmental guidelines. The telephone assessment was recorded on the hospital electronic medical record.
As national guidance was introduced, the preoperative process was refined to include detailed instructions to patients to self-isolate for at least 14 days before and 14 days after the procedure. During the data collection, we followed the daily updates of the guidance from the Royal College of Surgeons England.2 Starting from April 29, 2020, all patients undergoing elective surgery must have had a negative swab test within 72 hours from the day of the scheduled procedure.14 All patients signed a consent form clearly documenting the potential risk for contracting a COVID-19 infection during hospitalization and its possible sequelae.
Demographics, clinical data, and follow-up
Comorbidities and body mass index (BMI) were assessed for all patients undergoing an operative procedure, and an American Society of Anesthesiologists physical status classification (ASA) score was assigned after anesthesiologist review (Table I ). Basal temperature was checked and recorded for each patient at the entrance of the BMI CH and before being transferred to the theater suite. Vitals signs, such as blood pressure, heart rate, respiratory rate, and saturation on room air were checked and recorded as per our standard preoperative check list. As stated by the European Society of Surgical Oncology, and because of the junior doctor redeployment to critical areas such as the ICU, the majority of operations were performed by consultants, specialty and associate specialists, or higher surgery trainees (also called registrars).15
Table I.
General demographic data
| No (%) | |
|---|---|
| Variable | Total (N = 309) |
| Age, y | |
| Mean (SD) | 61.9 (17.2) |
| Age group | |
| ≤45 | 54 (17.5) |
| 46–64 | 106 (34.3) |
| 65–74 | 66 (21.4) |
| 75–84 | 54 (17.45) |
| ≥85 | 29 (9.38) |
| Sex | |
| Female | 167 (54.0) |
| Male | 142 (46.0) |
| ASA classification | |
| I | 98 (31.7) |
| II | 181 (58.6) |
| III | 29 (9.4) |
| IV | 1 |
| Temperature on admission | |
| ≤37.1 | 292 (94.5) |
| 37.2–37.8 | 17 (5.5) |
| ≥37.9 | 0 |
| Comorbidities | |
| Asthma | 22 (7.1) |
| Atrial fibrillation | 26 (8.4) |
| Cerebral vascular disease | 21 (6.8) |
| CKD | 12 (3.9) |
| COPD | 12 (3.9) |
| Hypertension | 88 (28.5) |
| Ischemic heart disease | 20 (6.5) |
| Type 2 diabetes mellitus | 15 (4.9) |
| BMI | |
| Mean (SD) | 26.82 (4.9) |
| Not recorded | 5 (1.1) |
| <18.5 | 3 (1) |
| 18.5–24.9 | 108 (35.0) |
| 25.0–34.9 | 171 (55.3) |
| 35–44.9 | 21 (7.0) |
| >45 | 1 |
CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease.
Follow-up was carried out for 30 days postoperatively; the electronic medical records from hospitals and general practitioners were searched on a daily basis to assess if there were complications, hospital reattendances, or general practitioner visits.
Primary outcome of the study was 30-day mortality. Secondary outcomes were COVID-19 infection, pulmonary complications, and rate of intensive therapy unit/ICU admission requirement.
Operating theater facilities
No changes were made to theater air flow conditions. Our local standard operating procedure was used to decrease exposure and to affect as few staff members as possible; intubation took place in theater with a minimum time of 5 minutes passed thereafter before other staff could enter, thus ensuring that sufficient air changes had occurred, thereby designed to decrease the risk of aerosol contamination to less than 1%.16 Extubation of patients took place in theater with minimal staff present and subsequent cleaning delayed for at least after 5 minutes thereafter for the reason previously described. Every patient, once stable, was transferred to the recovery suite wearing a surgical mask where at least 2 meters distance was allocated between patients. Every member of the team wore appropriate personal protective equipment (PPEs), including double gloves, fluid repellent coveralls or long-sleeved gowns, eye protection, and masks with a filtering face piece score of 3.12 , 16 Masks were 3M 8833/1863 (3M United Kingdom, Berkshire, United Kingdom). All staff members underwent rigorous fit testing for the above masks before being allocated to operating lists.
Results
The study demographics are summarized in Table I. In total, 309 patients underwent an elective operation at the BMI CH between April 8 and May 29, 2020. The mean age (± standard deviation) of patients was 61.9 ± 17.2. Of the 309 patients included in the study, 167 (54.0%) were women, and 142 (46.0%) were men. Comorbidities were recorded during the preoperative anesthetic assessment. Hypertension was the most common comorbidity reported in 88/309 patients; this was followed by atrial fibrillation and asthma found in 26/309 and 22/309, respectively; 31.7% (98) of the patients included had an ASA score of I, 58.6% (181) had an ASA of II, 9.4% (29) had an ASA of III, and only 1 patient had an ASA of IV. Notably, 292/309 (94.5%) of the patients had a basal temperature at admission less than 37.1 °C; 17/309 (5.5%) had a basal temperature between 37.2 °C and 37.8 °C. None of the patients admitted had a temperature greater than 37.9 °C.
A summary of the operations performed by each of the specialties is available in Table II . All the operations were classified either as “Minor” or “Intermediate” complexity operations.
Table II.
Description of operative details
| No (%) | |
|---|---|
| Surgical Specialty | Total (N = 309) |
| Breast surgery | 45 (14.56) |
| Axillary node dissection | 2 |
| Deconstruction of DIEP of breast ± reconstruction | 2 |
| Mastectomy & SLNB ± ANC | 8 |
| Re-excision breast margin | 4 |
| Simple mastectomy | 4 |
| WLE ± SLNB | 6 |
| WG-WLE ± SLNB | 16 |
| WLE & ANC | 3 |
| ENT surgery | 2 (0.64) |
| Insertion of grommets | 1 |
| Pan-endoscopy | 1 |
| General surgery | 22 (7.11) |
| Femoral hernia repair | 2 |
| Laparoscopic cholecystectomy | 10 |
| Open inguinal hernia repair | 4 |
| Paraumbilical hernia repair | 1 |
| Unilateral thyroid lobectomy | 5 |
| Gynecology | 13 (4.20) |
| Hysteroscopy, uterine biopsy ± coil insertion | 9 |
| Laparoscopic ovarian cystectomy | 1 |
| LLETZ ± diathermy of vaginal warts | 2 |
| WLE of vulva | 1 |
| Orthopedics | 37 (11.97) |
| Ankle syndesmosis reconstruction | 1 |
| Anterior cervical decompression and fusion | 2 |
| Arthroscopy of the knee | 1 |
| Carpal tunnel decompression | 7 |
| Cervical laminectomy/laminoplasty | 5 |
| Lumbar spine decompression | 1 |
| MUA, closed reduction ± K wire fixation | 5 |
| ORIF (clavicle, malleolus, radius, Lis-Franc injury) | 9 |
| Tendons repairs (biceps, quadriceps, great toe) | 5 |
| Total shoulder replacement | 1 |
| Pain management | 26 (8.41) |
| PRF of major nerve trunk | 15 |
| Facet joint injection ± denervation | 10 |
| Neurostimulation of peripheral nerve | 1 |
| Plastic surgery | 122 (39.48) |
| Excision of cancerous skin lesion + FTSG | 13 |
| Excision biopsy of skin lesion ± local flap | 13 |
| Excision of cancerous skin lesion (MM, BCC, SCC) | 64 |
| Axillary regional lymphadenectomy | 2 |
| Shave biopsy of skin lesion | 1 |
| Ulnar nerve decompression | 1 |
| WLE excision of cancerous lesion (MM, BCC, SCC) | 28 |
| Urology | 42 (13.59) |
| Cystoscopy + biopsy | 12 |
| Cystoscopy + biopsy + right ureteroscopy | 1 |
| Cystoscopy + insertion of SPC + urethral dilatation | 1 |
| Orchidectomy ± open inguinal hernia repair | 3 |
| Rigid cystoscopy ± change of stent | 4 |
| Rigid ureteroscopy & ureteric stent removal | 4 |
| Rigid ureteroscopy and fragmentation of ureteric stone ± stent insertion | 5 |
| TURBT | 10 |
| TURP | 2 |
| Grade of operation | |
| Minor | 28 (9.0) |
| Intermediate | 281 (91.0) |
| Type of anesthesia | |
| General | 158 (51.1) |
| Local | 151 (48.9) |
| Grade of operating surgeon | |
| Consultant | 249 (80.6) |
| Associate specialist | 18 (5.8) |
| Registrar | 42 (13.6) |
ANC, axillary node clearance; BCC, basal cell carcinoma; DIEP, deep inferior epigastric perforator; ENT, ear, nose and throat; FTSG, full-thickness skin grafting; LLETZ, large loop excision of the transformation zone; MM, malignant melanoma; MUA, manipulation under anesthesia; ORIF, open reduction and internal fixation; PRF, pulsed radiofrequency; SCC, squamous cell carcinoma; SLNB, sentinel lymph node biopsy; TURBT, transurethral resection of bladder tumor; TURP, transurethral resection of the prostate; WG, wire guided; WLE, wide local excision.
None of the patients were suspected to have COVID-19 before admission. One patient, who was originally planned as a day case, remained as in inpatient overnight for supplementary postoperative analgesia. The next morning, she was transferred to the local emergency hospital for further investigations concerning her upper abdominal pain. This investigation and her subsequent management could not be undertaken at the BMI CH as this was a weekend with no senior resident medical staff present nor the facility to intervene if a complication occurred. She underwent an urgent magnetic resonance cholangiopancreatography, which confirmed a suspected common bile duct stone; this required an endoscopic retrograde cholangiopancreatography and stone removal, which was uncomplicated. Incidentally, after transfer, she developed low oxygen saturations and was subsequently diagnosed as COVID-19 positive on a real-time reverse transcriptase–polymerase chain reaction assay of nasopharyngeal swab. She stayed for a total of 4 days and was discharged home with no further symptoms.
None of the 309 patients developed pulmonary complications. No patients were readmitted after discharge. Two more patients stayed greater than 23 hours for postoperative analgesia and for social reasons, respectively. Of the 27 patients (8.7%) who developed complications after their operation, the complications graded according to the Clavien-Dindo classification,17 13 (4.2%) were grade 1, 12 (4%) were grade 2, and 2 (1%) were 3a. Of these 27 patients who developed complications, 25 underwent intermediate operations, while 2 underwent minor operations (Table III ).
Table III.
Operative outcome, readmission, and complications
| No (%) |
|
|---|---|
| N = 309 | |
| Duration of stay | |
| <23 h | 306 |
| 24–72 h | 2 |
| >72 h | 1 |
| Complications | 27 (8.7) |
| Abscess | 1 |
| Epidural hematoma | 1 |
| Hematoma | 1 |
| CBD retained stone | 1 |
| Breast seroma | 8 |
| Urinary retention | 2 |
| Urinary tract infection | 2 |
| Wound dehiscence | 1 |
| Wound infection | 10 |
| Hospital Readmission | |
| None | 0 |
| ITU admissions | |
| None | 0 |
| Pulmonary complications | |
| No | 309 (100) |
| Pneumonia | 0 |
| ARDS | 0 |
| Deaths | |
| None | 0 |
| 30-d mortality | |
| None | 0 |
| Clavien-Dindo classification | |
| I | 13 (4.2) |
| II | 12 (3.9) |
| IIIA–IIIB | 2 |
| IVA–IVB | 0 |
| V | 0 |
| COVID-19 PCR swab | |
| Preoperatively | 104 (33.7) |
| Postoperatively | 1 |
ARDS, acute respiratory distress syndrome; CBD, common bile duct; ITU, intensive therapy unit; PCR, polymerase chain reaction.
Discussion
To the best of our knowledge, this is the first study to provide prospectively collected data on elective surgery performed in a true COVID-19-free hospital during the current coronavirus-2 pandemic. Globally as of June 27, 2020, there have been 9,653,048 confirmed cases of COVID-19, including 491,128 deaths, reported by the World Health Organization.18 The United Kingdom has been severely affected and currently, with 43,514 confirmed cases, has the greatest death toll in Europe and is third in the world after the Unites States and Brazil.19 Because millions of elective operations have been cancelled or postponed worldwide,8 a huge backlog of elective procedures has accumulated, increasing the demand of already pressured health care systems. Therefore, NHS England reached a national agreement with the private sector health care providers in the private sector to facilitate resuming NHS elective surgical services. We resumed elective surgery at a local, independent, private COVID-19-free hospital on April 8, 2020.
In other studies, Lei et al described the characteristics and outcomes11 of 34 patients who underwent elective surgical procedures in Wuhan Hospital from January 1 to February 5, 2020 and developed COVID-19 pneumonia; 15 (44%) required ICU care, and 7 died after ICU admissions resulting in a high mortality rate of 21%. This represents one of the first available retrospective studies; however, there were many acknowledged limitations. Only a small number of patients were included in their study, with no rigorous patient selection and no patient self-isolation or testing before operation. As described by the authors, if they knew these patients were COVID-19 positive, they would not have operated on them considering they were all elective cases. Moreover, no information about PPEs and safety measures were disclosed in the article.
A second study published recently in The Lancet by Bhangu et al10 showed that postoperative pulmonary complications occur in half of patients with symptomatic perioperative SARS-CoV-2 infection and are associated with high mortality. In particular, the authors reported a mortality rate of 19% in patients who underwent elective operations; of these, 9% had a diagnosis of SARS-CoV-2 infection preoperatively and 91% postoperatively, respectively. From these concerning findings, the authors advocated a greater threshold and a serious reconsideration of elective surgical services during the current pandemic, suggesting postponing all nonurgent operations. Although more than 1,100 patients were included in this study, we believe that the conclusions are drawn on data derived from heterogeneous health care systems and from countries hit by the pandemic at different times and, therefore, should be interpreted with caution. In addition, laboratory testing for SARS-CoV-2 infection were not standardized across the participating centers nor were radiologic findings. Furthermore, data included patients who underwent both emergency and elective surgery, and none of the participating hospitals were COVID-19 free at the time of the data collection.
We believe our study has relevant implications for the future resumption of elective operations and other types of surgical/interventional procedures, especially in the event of a second wave of COVID-19. Although the results presented in this study account for only 6 weeks of elective surgical activity and on a small cohort, the 30-day mortality rate and the absence of important adverse outcomes are quite different from the above mentioned studies.10 , 11 Currently, there is no other similar published data, prospectively collected in a completely COVID-19-free setting, which proves that resuming elective surgery is feasible and safe. Of the 309 patients who underwent elective surgery at the BMI CH, no one died, none required critical care admission, and at most only 1 patient developed COVID-19 positivity, probably infected before our elective operation, because she turned positive on postop day 1. Another strength of our study is the comprehensive search for complications and reattendances guaranteeing that no data were missed. We acknowledge that our processes of establishing suitability for the elective operation relied initially on the self-declaration of patients to their symptoms and household isolation status, especially at the beginning of the study when no national guidelines were disseminated. This reliance, unfortunately, led to an incorrect preoperative risk assessment in the case of the 1 patient who tested positive for COVID-19 in the postoperative period. This patient was aware that her cohabiting partner had been diagnosed with SARS-CoV-2 infection but did not disclose this information despite multiple prompts. This patient did not require invasive ventilation, was managed conservatively on the surgical ward at another hospital after being transferred for pain control as explained above, and made a full recovery without complications. None of the medical and nonmedical health care professionals involved in her care tested positive for SARS-CoV-2 infection nor did any patient who was operated on the same day. This highlights how following established guidelines and protocols on social distancing, PPEs, and single-room allocation can minimize the risk of cross-contamination.
To avoid COVID-19 related pre- and postoperative complications for both the patient and health care workers, health care providers should carefully inform patients about the risks they may encounter if they are not wholly accurate in answering the preoperative assessment questions. This situation should become less relevant as a consequence of routine preoperative testing.
Before considering resuming any elective surgical service, it is paramount to consider the capabilities of the health care facilities while maintaining the safety of patients and health care professionals involved.
In conclusion, we believe that creating COVID-19-free hospitals represents a solution for decreasing the pressure on health care systems even if a second or third pandemic surge was to occur.
The absence of adverse outcomes in COVID-19-negative patients supports the safety of a COVID-19-free setting; however, it must be remembered that careful patient selection and the reconfiguration of the elective service are crucial.
Conflict of interest/Disclosure
All authors declare no conflict of interest.
Funding/Support
None
Acknowledgments
We would like to express our gratitude for the ongoing help and support to all the staff of the BMI Chiltern Hospital as well as Buckinghamshire Healthcare NHS Trust, and to Alexandre Battaglia for his input in the data analysis.
References
- 1.World Health Organization (WHO) WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020; 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
- 2.Royal College of Surgeons of England Recovery of surgical services during and after COVID-19; 2020. https://www.rcseng.ac.uk/coronavirus/recovery-of-surgical-services/
- 3.American College of Surgeons COVID-19: Recommendations for management of elective surgical procedures; 2020. https://www.facs.org/covid-19/clinical-guidance/elective-surgery
- 4.Zarrintan S. Surgical operations during the COVID-19 outbreak: should elective surgeries be suspended? Int J Surg. 2020;78:5–6. doi: 10.1016/j.ijsu.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chew M.H., Tan W.J., Ng C.Y., Ng K.H. Deeply reconsidering elective surgery: worldwide concerns regarding colorectal surgery in a COVID-19 pandemic and a Singapore perspective. Singapore Med J. 2020 doi: 10.11622/smedj.2020070. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iacobucci G. Covid-19: all non-urgent elective surgery is suspended for at least three months in England. BMJ. 2020;368:m1106. doi: 10.1136/bmj.m1106. [DOI] [PubMed] [Google Scholar]
- 7.Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) SAGES and EAES recommendations regarding surgical response to COVID-19 crisis; 2020. https://www.sages.org/recommendations-surgical-response-covid-19/
- 8.COVIDSurg Collaborative Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020 doi: 10.1002/bjs.11746. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.NHS. COVID-19 Partnership working with the Independent Sector Providers and the Independent Healthcare Providers Network (IHPN): Letter from Neil Permain; 2020. https://www.england.nhs.uk/coronavirus/publication/partnership-working-with-the-independent-sector-providers-and-the-ihpn/
- 10.COVIDSurg Collaborative Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020 doi: 10.1016/s0140-6736(20)31182-x. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lei S., Jiang F., Su W. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. 2020 doi: 10.1016/j.eclinm.2020.100331. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.GOV.UK. Reducing the risk of transmission of COVID-19 in the hospital setting; 2020. https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control/reducing-the-risk-of-transmission-of-covid-19-in-the-hospital-setting. Accessed May 11, 2020.
- 13.Richardson S., Hirsch J.S., Narasimhan M. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323:2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Royal College of Surgeons of England Updated Intercollegiate General Surgery Guidance on COVID-19; 2020. https://www.rcseng.ac.uk/coronavirus/joint-guidance-for-surgeons-v2/
- 15.The European Society of Surgical Oncology (ESSO) Statement on COVID-19: Advice for surgical oncologists on cancer service provision; 2020. https://www.essoweb.org/media/documents/esso-statement-on-covid-19.pdf
- 16.https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/893320/COVID-19_Infection_prevention_and_control_guidance_complete.pdf
- 17.Clavien P.A., Barkun J., de Oliveira M.L. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187–196. doi: 10.1097/SLA.0b013e3181b13ca2. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization (WHO) Coronavirus disease (COVID-19): Situation report—159; 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200627-covid-19-sitrep-159.pdf?sfvrsn=93e027f6_2
- 19.GOV.UK. Coronavirus cases in the UK: Daily updated statistics; 2020. https://www.gov.uk/guidance/coronavirus-covid-19-information-for-the-public. Accessed June 27, 2020.