Highlights
-
•
Previous research has examined the characteristics of patients receiving air medical retrieval for mental and behavioral disorders; however, the economic costs have not been studied.
-
•
This study provides evidence on the economic costs associated with air medical retrieval, finding that the majority of costs incurred were associated with hospital admission and treatment.
-
•
These findings are important in assessing the costs associated with the current approaches to mental health service provision in rural and remote communities. Future studies should determine social costs.
Abstract
Objective
Adequate mental health service provision in rural and remote Australian communities is problematic because of the tyranny of distance. The Royal Flying Doctor Service provides air medical retrieval for people in rural and remote areas. The economic impact on both the Royal Flying Doctor Service and the public hospital system for mental health–related air medical retrievals is unknown. We aimed to estimate the direct medical costs associated with air medical retrievals and subsequent hospitalizations for mental and behavioral disorders for the 2017 calendar year.
Methods
All patients with a primary working diagnosis of International Statistical Classification of Diseases and Related Health Problems, 10th Version, Australian Modification F00 to F99 (mental and behavioral disorders) who underwent an air medical retrieval were included in this cost analysis. International Statistical Classification of Diseases and Related Health Problems, 10th Edition, Australian Modification codes were mapped to Australian Refined Diagnosis Related Group codes, with hospital costs applied from the National Hospital Cost Data Collection (2016/2017). All costs are reported in 2017 Australian dollars (AUDs).
Results
One hundred twenty-two primary evacuations and 926 interhospital transfers occurred with an in-flight diagnosis of F00 to F99, most commonly psychotic disorders, including schizophrenia and schizotypal disorders. The total direct medical costs were estimated to be AUD $20,070,527. Costs for primary evacuations accounted for 13% (AUD $2,611,260), with the majority of this associated with the subsequent hospital admission (AUD $1,770,139). Similarly, the majority of the costs associated with interhospital transfers (total costs = AUD $17,459,267) were also related to hospital costs (AUD $13,569,187).
Conclusion
Direct medical costs associated with air medical retrievals for people experiencing a mental health crisis are substantial. The majority of costs are associated with hospital admission and treatment; however, the indirect (loss of productivity) and intangible (quality of life) costs are likely to be far greater.
Approximately 29% of the Australian population lives in rural or remote settings.1 The prevalence of mental health conditions in rural and remote Australia is comparable with inner regional and major city areas2; however, the burden of disease is far greater for people living in rural and remote settings.3 , 4 This is most clearly demonstrated by suicide rates, which increase in line with the degree of remoteness, ranging from 9.4 per 100,000 persons in major cities to 18.1 per 100,000 in very remote settings.5
Although the drivers of this unbalanced burden of mental health conditions are many and complex, 1 of the key factors is the supply of mental health services. The majority of mental health professionals, measured as full-time equivalent (FTE) per 100,000 population, are located in major cities. Specifically, 15.1 FTE psychiatrists per 100,000 persons are based in major cities compared with 5.7 per 100,00 in outer-regional settings, 3.8 per 100,000 in remote settings, and 1.9 per 100,000 in very remote areas of Australia.6 Similar trends are observed for mental health nurses (91.0 FTE nurses/100,000 persons in major cities, 56.9/100,000 in remote setting, and 36.3/100,000 in very remote settings) and clinical psychologists (105.3/100,000 in major cities, 35.4/100,000 in remote settings, and 27.3/100,000 in very remote settings).7
In addition to these supply-side issues, demand for mental health services differs from that in major cities and many urban centers. Although the overall prevalence of mental health conditions is similar across settings, people in rural and remote settings experience higher rates of substance use and acuity of mental health conditions along with the aforementioned rates of suicide.8 , 9 Furthermore, increased environmental challenges including drought, fires, and climate change, and the recent Coronavirus pandemic, are placing greater pressure on the mental health of many rural and remote communities.10, 11, 12, 13
In this context, the Royal Flying Doctor Service (RFDS) provides air medical retrievals for Australians living in rural and remote communities experiencing health crises, including acute mental health presentations. Patients are typically transferred by aircraft to large metropolitan or inner regional public hospitals for urgent acute care. The economic costs of this approach, including those incurred by the RFDS and public hospitals, has not been quantified.
The primary aim of this article is to determine the annual air medical retrieval and in-patient hospital-direct medical costs associated with mental and behavioral disorders from a health payer perspective. A secondary aim includes determining the mismatch of the supply and the capacity of rural and remotely located mental health services with the demand of acute presentations, with retrieval signaling as a potential proxy for this unmet need.
Methods
Setting and Perspective
The RFDS provides air medical, road ambulance, and primary health care to rural and remote areas of Australia without traditional medical services, such as those associated with the Medicare Benefits Schedule, a listing of the Medicare services subsidized by the Australian government.14 The focus of this article is on air medical retrievals for mental health crises from a health care payer perspective.15 , 16
Design and Participants
A partial economic evaluation was undertaken using routinely collected air medical data for patients diagnosed in flight with a mental and behavioral disorder (International Statistical Classification of Diseases and Related Health Problems, 10th Edition, Australian Modification [ICD-10 AM], Chapter V) between January 1, 2017, and December 31, 2017. Participants included all RFDS patients who underwent an air medical retrieval, including a primary evacuation and interhospital transfer, for mental and behavioral disorders within Australia in 2017. The majority of the RFDS air medical retrievals are conducted in Western Australia, Central Australia, Queensland, and New South Wales, with limited air medical retrievals coming from Tasmania and Victoria. Tasmania and Victoria air medical services are mainly conducted by other services; however, the RFDS in 2017/2018 conducted substantial road transportation in Victoria and Tasmania (N = 75,147).17
Data Sources
For the primary aim, data were collected and coded on each patient's in-flight working diagnosis using the ICD-10-AM coding method.18 The in-flight primary working diagnosis was based on referral assessment information and an assessment of the current medical status by the in-flight medical team, which, in this patient group, mainly consisted of a senior medical officer and/or a senior flight nurse. The in-flight primary working diagnosis was then coded by trained administrative staff and cross-checked by 2 of the authors (L.B. and F.G.). Data were collected within flight on the patient's sex, age, and indigenous status. Both paper-based and electronic methods were used in data collection. Detailed patient histories were not routinely collected. All air medical retrieval patients with a primary working diagnosis of ICD-10-AM Chapter V codes F00-F99 (mental and behavioral disorders) were included in the analysis. All other diagnoses were excluded from analysis.
We defined 2 separate types of air medical retrievals: 1) primary evacuations of a patient and 2) interhospital transfers that involve an RFDS air medical evacuation from, typically, a small regional hospital to an inner regional or major city hospital.
Cost Data
To determine the economic costs per primary evacuation, we collected the costs incurred by each RFDS section and operation (loosely state based), including the Queensland Section, Western Operations, South Eastern Section, and Central Operations. This included determining the individual primary evacuation costs by RFDS base from each section and operation. To protect patient and RFDS base confidentiality (particularly for those bases conducting a small number of retrievals), these costs were then averaged. Costs included engine hour and staffing by an RFDS registered nurse (present on all flights) and RFDS medical officer as required.
The costs for interhospital transfers were based on $2,912 per engine hour, which includes an RFDS registered nurse. For transfers in which an RFDS medical officer was also required, an additional $2,223 per hour was added to the cost of each interhospital transfer. This formula is consistent with other published literature.19
To estimate inpatient admission costs, we mapped the ICD-10-AM codes to Australian Refined Diagnosis Related Group (AR-DRG) codes provided in the National Hospital Cost Data Collection (2016/2017) (Table 1 ).20 This mapping was performed by 1 of the authors (B.d.G.) and independently checked by 2 of the authors (F.G. and M.C.). It is important to note that although there are > 40,000 ICD-10-AM codes and > 8,000 AR-DRG codes, the National Hospital Cost Data Collection only contains 807 codes. Cost data were then extracted from the 2016/2017 National Hospital Cost Data Collection for each relevant AR-DRG (Table 2 ).
Table 1.
Mapping International Statistical Classification of Diseases and Related Health Problems, 10th Edition (ICD-10), Australian Modification to Australian Refined Diagnosis Related Groups (AR-DRGs)a
| ICD-10 Description | Corresponding AR-DRG | |
|---|---|---|
| F00-F09 Organic, including symptomatic, mental disorders | F00 Dementia in Alzheimer disease | B63A Dementia and Other Chronic Disturbances of Cerebral Function, Major Complexity |
| F01 Vascular dementia | B63A Dementia and Other Chronic Disturbances of Cerebral Function, Major Complexity | |
| F02.2 Dementia in Huntington disease | B63A Dementia and Other Chronic Disturbances of Cerebral Function, Major Complexity | |
| F03 Unspecified dementia | B63A Dementia and Other Chronic Disturbances of Cerebral Function, Major Complexity | |
| F05 Delirium, not induced by alcohol and other psychoactive substances | B63A Dementia and Other Chronic Disturbances of Cerebral Function, Major Complexity | |
| F06 Other mental disorders due to brain damage and dysfunction and to physical disease | B63A Dementia and Other Chronic Disturbances of Cerebral Function, Major Complexity | |
| F07 Personality and behavioral disorders due to brain disease, damage and dysfunction | U67A Personality Disorders and Acute Reactions, Major Complexity | |
| F09 Unspecified organic or symptomatic mental disorder | U60A Mental Health Treatment W/O ECT, Sameday, Major Complexity | |
| F10-F19 Mental and behavioral disorders due to psychoactive substance use | F10 Mental and behavioral disorders due to use of alcohol | V62A Alcohol Use and Dependence, Major Complexity |
| F11 Mental and behavioral disorders due to use of opioids | V63Z Opioid Use and Dependence | |
| F12 Mental and behavioral disorders due to use of cannabinoids | V61A Drug Intoxication and Withdrawal, Major Complexity | |
| F13 Mental and behavioral disorders due to use of opioids | V64Z Other Drug Use and Dependence | |
| F15 Mental and behavioral disorders due to use of other stimulants, including caffeine | V61A Drug Intoxication and Withdrawal, Major Complexity | |
| F16 Mental and behavioral disorders due to use of hallucinogens | V61A Drug Intoxication and Withdrawal, Major Complexity | |
| F18 Mental and behavioral disorders due to use of volatile solvents | V64Z Other Drug Use and Dependence | |
| F19 Mental and behavioral disorders due to multiple drug use and use of other psychoactive substances | V61A Drug Intoxication and Withdrawal, Major Complexity | |
| F20-F29 Schizophrenia, schizotypal and delusional disorders | F20 Schizophrenia | U61A Schizophrenia Disorders, Major Complexity |
| F21 Schizotypal disorder | U61A Schizophrenia Disorders, Major Complexity | |
| F22 Persistent delusional disorders | U62A Paranoia and Acute Psychotic Disorders, Major Complexity | |
| F24 Induced delusional disorder | U62A Paranoia and Acute Psychotic Disorders, Major Complexity | |
| F23 Acute and transient psychotic disorders | U62A Paranoia and Acute Psychotic Disorders, Major Complexity | |
| F25 Schizoaffective disorders | U61A Schizophrenia Disorders, Major Complexity | |
| F28 Other nonorganic psychotic disorders | U61A Schizophrenia Disorders, Major Complexity | |
| F29 Unspecified nonorganic psychosis | U62A Paranoia and Acute Psychotic Disorders, Major Complexity | |
| F30-F39 Mood [affective] disorders | F30 Manic episode | U63A Major Affective Disorders, Major Complexity |
| F31 Bipolar affective disorder | U63A Major Affective Disorders, Major Complexity | |
| F32 Depressive episode | U63A Major Affective Disorders, Major Complexity | |
| F33 Recurrent depressive disorder | U63A Major Affective Disorders, Major Complexity | |
| F34 Persistent mood [affective] disorders | U63A Major Affective Disorders, Major Complexity | |
| F38 Other mood [affective] disorders | U63A Major Affective Disorders, Major Complexity | |
| F39 Unspecified mood [affective] disorder | U63A Major Affective Disorders, Major Complexity | |
| F40-F48 Neurotic, stress-related and somatoform disorders | F41 Other anxiety disorders | U65A Anxiety Disorders, Major Complexity |
| F43 Reaction to severe stress, and adjustment disorders | U65A Anxiety Disorders, Major Complexity | |
| F44 Dissociative [conversion] disorders | U65A Anxiety Disorders, Major Complexity | |
| F50-F59 Behavioral syndromes associated with physiological disturbances and physical factors | F50 Eating disorders | U66A Eating and Obsessive-Compulsive Disorders, Major Complexity |
| F52 Sexual dysfunction not caused by organic disorder or disease | U64A Other Affective and Somatoform Disorders, Major Complexity | |
| F53 Mental and behavioral disorders associated with the puerperium not elsewhere classified | U62A Paranoia and Acute Psychotic Disorders, Major Complexity | |
| F54 Psychological and behavioral factors associated with disorders or diseases classified elsewhere | U60A Mental Health Treatment W/O ECT, Sameday, Major Complexity | |
| F59 Unspecified behavioral syndromes associated with physiological disturbances and physical factors | U64A Other Affective and Somatoform Disorders, Major Complexity | |
| F60-F69 Disorders of adult personality and behavior | F60 Specific personality disorders | U67A Personality Disorders and Acute Reactions, Major Complexity |
| F61 Mixed and other personality disorders | U67A Personality Disorders and Acute Reactions, Major Complexity | |
| F63 Habit and impulse disorders | ||
| F68 Other disorders of adult personality and behavior | U67A Personality Disorders and Acute Reactions, Major Complexity | |
| F69 Unspecified disorder of adult personality and behavior | U67A Personality Disorders and Acute Reactions, Major Complexity | |
| F70-F79 Mental retardation | F78 Other mental retardation | U60A Mental Health Treatment W/O ECT, Sameday, Major Complexity |
| F80-F89 Disorders of psychological development | F82 Specific developmental disorder of motor function | U67A Personality Disorders and Acute Reactions, Major Complexity |
| F90-F98 Behavioral and emotional disorders with onset usually occurring in childhood and adolescence | F91 Conduct disorders | U68A Childhood Mental Disorders, Major Complexity |
| F98 Other behavioral and emotional disorders with onset usually occurring in childhood and adolescence | U68A Childhood Mental Disorders, Major Complexity | |
| Unspecified MH disorder | Unspecified MH disorder | U60A Mental Health Treatment W/O ECT, Sameday, Major Complexity |
Independent Hospital Pricing Authority. National Hospital Cost Data Collection Report, Public Sector, Round 21 (Financial year 2016-17). Canberra, Australia: Independent Hospital Pricing Authority; 2019.
Table 2.
Unit Costs
| Item | AUD ($) |
|---|---|
| Air retrieval costs (primary evacuations)a | 6,623 |
| Interhospital transfers: hourly cost for engine time and in-flight nursing careb | 2,912 |
| Interhospital transfers: hourly cost for in-flight medical officerc | 2,223 |
| AR-DRGsd B63A: Dementia and Other Chronic Disturbances of Cerebral Function, Major Complexity | 14,205 |
| U60A: Mental Health Treatment W/O ECT, Sameday, Major Complexity | 1,357 |
| U61A: Schizophrenia Disorders, Major Complexity | 16,741 |
| U62A: Paranoia and Acute Psychotic Disorders, Major Complexity | 15,488 |
| U63A: Major Affective Disorders, Major Complexity | 17,219 |
| U64A: Other Affective and Somatoform Disorders, Major Complexity | 9,599 |
| U65A: Anxiety Disorders, Major Complexity | 9,824 |
| U66A: Eating and Obsessive-Compulsive Disorders, Major Complexity | 32,701 |
| U67A: Personality Disorders and Acute Reactions, Major Complexity | 10,470 |
| U68A: Childhood Mental Disorders, Major Complexity | 17,371 |
| V61A: Drug Intoxication and Withdrawal, Major Complexity | 9,644 |
| V62A: Alcohol Use and Dependence, Major Complexity | 13,651 |
| V63Z: Opioid Use and Dependence | 7,213 |
| V64Z: Other Drug Use and Dependence | 6,287 |
AR-DRGs = Australian Refined Diagnosis Related Groups; AUD = Australian dollar.
Air retrieval costs were estimated by averaging costs incurred by each Royal Flying Doctor Service section and operation. These costs include engine hour and staffing by a Royal Flying Doctor Service registered nurse (present on all flights) and a Royal Flying Doctor Service medical office as required.
Interhospital transfer costs were based on $2,912 per engine hour and a Royal Flying Doctor Service registered nurse.
Where a Royal Flying Doctor Service medical officer was also required, an additional $2,223 per hour was added to the cost of each interhospital transfer.
Independent Hospital Pricing Authority. National Hospital Cost Data Collection Report, Public Sector, Round 21 (Financial year 2016-17). Canberra, Australia: Independent Hospital Pricing Authority; 2019.
The costs were then applied to each primary evacuation and interhospital transfer, respectively. For interhospital transfers, the costs associated for the first admission (ie, the hospital from which the patient was transferred from) were not included because no ICD-10-AM or AR-DRG data are collected for this. The total aggregate costs were estimated for both primary evacuations and interhospital transfers. To further understand where costs are incurred, the disaggregated “cost buckets” reported in the National Hospital Cost Data Collection were assessed. These disaggregated costs include ward medical, ward nursing, nonclinical salaries, pathology, imaging, allied pharmacy, critical care, operating room, emergency department, ward supplies, specialist procedure suites, prostheses, on-costs (eg, indirect salary costs such as superannuation), hotel and depreciation (ie, domestic services within the hospital that are not directly related to patient care), and emergency department (ED) product (ie, the average cost per admitted ED patient) elements. Estimated expenditure on each cost bucket was then calculated as a proportion of the total hospital costs.
To determine the secondary aim, we used the RFDS Service Planning and Operational Tool (SPOT) to map service provision throughout Australia. SPOT uses data from the Australian Bureau of Statistics and data from Health Direct to derive geographic population estimates reflective of mental health services.21 Primary evacuation statistical areas were defined according to the Australian Bureau of Statistics Statistical Area Level 3 code.22 SPOT has been designed to help determine the geographic coverage of health care in Australia. SPOT graphically represents population concentrations and health care services and calculates the proportion of the Australian population who are covered by specific health care facilities (in this case, general mental health services) within a 60-minute drive time.23 To map the location of air medical retrievals for diagnoses associated with mental health, we used Tableau mapping software (Tableau Software, Salesforce Company, Seattle, WA United States of America).24
Statistical Analysis
This study used descriptive statistics to summarize findings. Cost data were extracted from the 2016/2017 National Hospital Cost Data Collection for each AR-DRG derived from the ICD-10-AM mapping exercise. Costs associated with RFDS air medical retrievals were applied to each AR-DRG. These costs were then summed and multiplied by the number of retrievals per AR-DRG.
Expenditure based on cost buckets was extracted from the 2016/2017 National Hospital Cost Data Collection. Each item in the cost bucket was multiplied by the number of air medical transfers with the corresponding AR-DRG. Costs for each cost bucket were summed for all AR-DRGs, allowing for the calculation of the proportion of the total expenditure associated with each cost bucket. All costs are reported in 2017 Australian dollars. Analyses were conducted in Excel (Microsoft, Redmond, WA). In addition, cell sizes with 5 or less patients are supressed for confidentiality.
Ethics Approval
This project was deemed a low-risk quality assurance project by the RFDS Clinical and Health Services Research Committee, which provides oversight for RFDS research projects, on March 18, 2019. Because this project involved routinely collected data, specific patient consent forms were not required.
Results
Over the 2017 calendar year, the RFDS conducted 122 primary evacuations and 926 interhospital transfers for patients with an in-flight diagnosis associated with a mental and behavioral disorder (ICD-10-AM Chapter V F00-F99).
Availability of Services
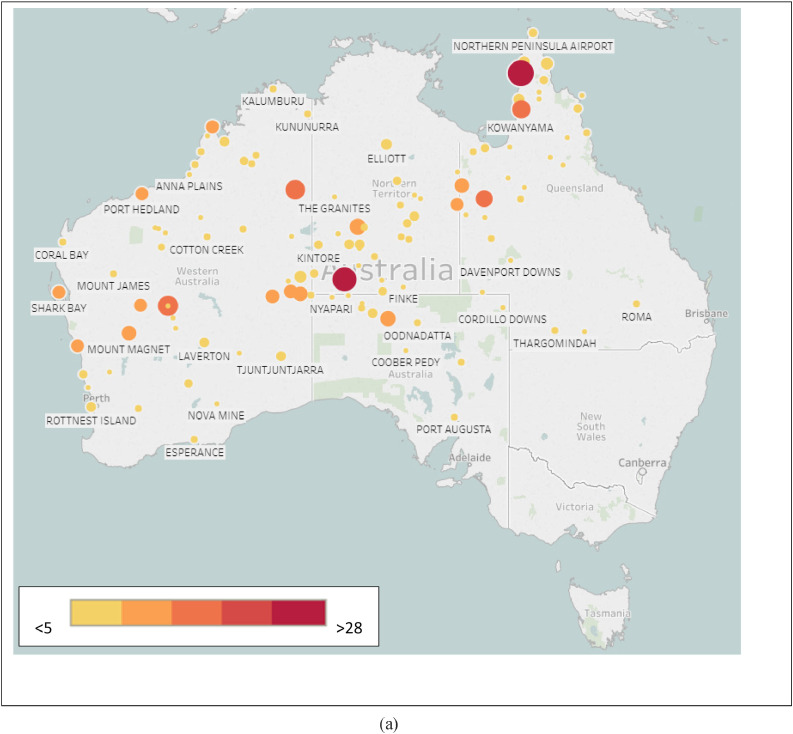
All of the primary evacuations and interhospital transfers were from remote and very remote areas to inner regional or metropolitan centers (Fig. 1 A). The primary evacuation Statistical Areas Level 3 included Alice Springs (Northern Territory) (30.4%, n = 73), The Far North (Northern Queensland) (27.1%, n = 65), Gold Fields (Western Australia) (25.8%, n = 62), and the Kimberly (17.1%, n = 41).
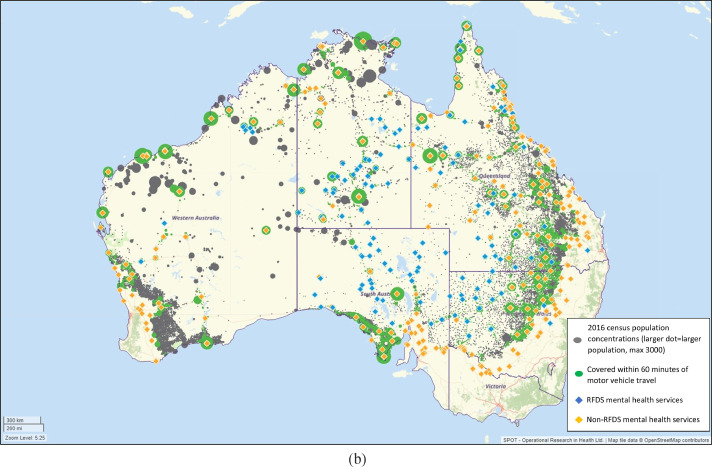
Figure 1.
A, The primary evacuation patient pickup location. B, The non-RFDS and RFDS mental health services rural and remote coverage in 2017 to 2018. *This figure estimates the rural and remote provision of mental health services and excludes metropolitan areas using HealthDirect, RFDS, and Australian Bureau of Statistics (ABS) data sources. **The dots indicate population concentrations, with larger dots equaling more people. The green dots indicate population concentrations that are able to access services within a 60-minute drive time, whereas the gray dots indicate population concentrations that are not able to access services within a 60-minute drive time.
Figure 1B provides an illustration of the supply of mental health services derived from SPOT. When looking at the general mental health service coverage within these areas reflective of population concentrations, the Gold Fields (76.2%, n = 5,690) had the highest remote and very remote population level without coverage followed by Alice Springs (32.1%, n = 13,275), Kimberly (23.3%, n = 8,577), and the Far North (9.5%, n = 1,907).
ICD-10-AM In-flight Diagnoses
For primary evacuations, the leading diagnoses were for the F20 to F29 group of psychotic disorders, including schizophrenia, schizotypal, delusional disorders, and other non–mood-related psychotic disorders (43.3%, n = 104). Schizophrenia (15.0%, n = 36), acute and transient psychotic disorders (12.1%, n = 29), and unspecified nonorganic psychosis (7.1%, n = 17) were the most common diagnoses. One fifth of mental and behavioral disorder evacuations were for F30 to F39, mood (affective) disorders (19.2%, n = 46), largely related to depressive disorders (13.8%, n = 33). F10 to F19, mental and behavioral disorders caused by psychoactive substance use, were reported for 13.3% (n = 32) of evacuations and 8.3% (n = 20) for F00 to F09, organic, including symptomatic, mental disorders. Relatively small numbers of evacuations were for F40 to F48, neurotic, stress-related, and somatoform disorders (5.4%, n = 13), and F99, unspecified mental health disorders (7.9%, n = 19). Five or less evacuations were reported for F50 to F59, behavioral syndromes associated with physiological disturbances and physical factors; F60-F69, disorders of adult personality and behavior; and F90-F98, behavioral and emotional disorders with onset usually occurring in childhood and adolescence.
Similar to primary evacuations, the majority of interhospital transfers were associated with F20 to F29, schizophrenia, schizotypal, delusional disorders, and other non–mood-related psychotic disorders (45.8%, n = 424). One fifth of the transfers were for F30 to F39, mood (affective) disorders (20.7%, n = 192); 15.1% (n = 140) were for F10 to F19, mental and behavioral disorders caused by psychoactive substance use; and 7.7% (n = 71) for F00 to F09, organic, including symptomatic, mental disorders. Small numbers of interhospital transfers were reported for F60 to F69, disorders of adult personality and behavior (3.0%, n = 28); F40 to F48, neurotic, stress-related, and somatoform disorders (2.8%, n = 26); F99, unspecified mental disorders (2.4%, n = 22); and F50 to F59, behavioral syndromes associated with physiological disturbances and physical factors (1.8%, n = 17). Five or less evacuations were reported for F90 to F98, behavioral and emotional disorders with onset usually occurring in childhood and adolescence; F80 to F89, disorders of psychological development; and F70 to F79, mental retardation.
Costs Associated With Air Medical Retrievals
The total costs for all mental and behavioral disorder air medical retrievals and subsequent hospital admissions in 2017 was $20,070,527. The cost associated with the 122 primary evacuations was estimated to be $2,611,260. Two thirds of this ($1,770,139, 68.0%) was related to in-patient admissions (AR-DRG costs) and the remaining $841,121 on air retrieval costs. Reflecting the numbers of patients, the highest combined air retrieval and in-patient costs were for U61A (Schizophrenia Disorders, Major Complexity; $654,192), U62A (Paranoia and Acute Psychotic Disorders, Major Complexity; $641,219), and U63A (Major Affective Disorders, Major Complexity; $596,050). The average cost per primary evacuation patient was $21,404.
The total cost related to interhospital transfers was $17,459,267. Similar to primary evacuations, the majority of these costs were related to in-patient admission costs ($13,569,187). Reflecting the numbers of interhospital transfers, the greatest total costs were associated with U61A (Schizophrenia Disorders, Major Complexity; $4,709,094), U62A (Paranoia and Acute Psychotic Disorders, Major Complexity; $4,099,211), and U63A (Major Affective Disorders, Major Complexity; $3,983,904). The average cost per interhospital transfer patient was $18,855 (see Table 3 for cost breakdowns for primary evacutations and interhospital transfers).
Table 3.
Total Medical Costs for Primary Evacuations and Interhospital Retrievals: 2017a
| Primary Evacuations |
Interhospital Transfers |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| AR-DRG | N | Air Retrieval Costs ($) | AR-DRG Inpatient Costs ($)b | Total Costs ($) | n | RFDS Engine Time, Nursing Costs ($)a | RFDS Medical Officer Costs ($)a | AR-DRG Inpatient Costs ($) | Total Costs ($) |
| B63A: Dementia and Other Chronic Disturbances of Cerebral Function, Major Complexity | NR | 33,115 | 71,025 | 104,140 | 62 | 203,840 | 26,676 | 880,695 | 1,111,211 |
| U60A: Mental Health Treatment W/O ECT, Sameday, Major Complexity | 8 | 52,984 | 10,856 | 63,840 | 33 | 115,024 | 15,561 | 44,795 | 175,380 |
| U61A: Schizophrenia Disorders, Major Complexity | 28 | 185,444 | 468,748 | 654,192 | 222 | 836,909 | 155,610 | 3,716,575 | 4,709,094 |
| U62A: Paranoia and Acute Psychotic Disorders, Major Complexity | 29 | 192,067 | 449,152 | 641,219 | 204 | 761,779 | 177,840 | 3,159,592 | 4,099,211 |
| U63A: Major Affective Disorders, Major Complexity | 25 | 165,575 | 430,475 | 596,050 | 192 | 611,083 | 66,690 | 3,306,131 | 3,983,904 |
| U64A: Other Affective and Somatoform Disorders, Major Complexity | NR | 33,115 | 47,995 | 81,110 | n/r | 8,445 | 0 | 19,168 | 27,643 |
| U65A: Anxiety Disorders, Major Complexity | 7 | 46,361 | 68,768 | 115,129 | 26 | 84,157 | 8,892 | 255,428 | 348,477 |
| U66A: Eating and Obsessive-Compulsive Disorders, Major Complexity | — | — | — | — | 10 | 26,208 | 0 | 327,011 | 353,219 |
| U67A: Personality Disorders and Acute Reactions, Major Complexity | NR | 19,869 | 31,410 | 51,279 | 30 | 96,970 | 17,784 | 314,092 | 428,846 |
| U68A: Childhood Mental Disorders, Major Complexity | NR | 6,623 | 17,371 | 23,994 | n/r | 13,191 | 0 | 86,857 | 100,048 |
| V61A: Drug Intoxication and Withdrawal, Major Complexity | 11 | 72,853 | 106,084 | 178,937 | 106 | 418,163 | 100,035 | 1,022,288 | 1,540,486 |
| V62A: Alcohol Use and Dependence, Major Complexity | NR | 33,115 | 68,255 | 101,370 | 30 | 113,859 | 20,007 | 409,527 | 543,394 |
| V63Z: Opioid Use and Dependence | 0 | — | — | — | NR | 6,261 | 0 | 14,425 | 20,686 |
| V64Z: Other Drug Use and Dependence | 0 | — | — | — | NR | 5,096 | 0 | 12,574 | 17,670 |
| Total | 122 | 841,121 | 1,770,139 | 2,611,260 | 192 | 3,300,985 | 589,095 | 13,569,187 | 17,459, 267 |
AR-DRG = Australian Refined Diagnosis Related Group; NR = not reported (cell size of 5 or less are suppressed for confidentiality).
Costs based on internal Royal Flying Doctor Service data.
Independent Hospital Pricing Authority. National Hospital Cost Data Collection Report, Public Sector, Round 21 (Financial year 2016-17). Canberra, Australia: Independent Hospital Pricing Authority; 2019.
Almost one third of all hospital costs (for both primary evacuations and interhospital transfers) were associated with the ward nursing cost bucket (30.2%) (Fig. 2 ). These costs are associated with nursing care provided in general wards.20 The ward medical cost bucket, which includes both salaries and wages for medical officers, accounted for 13.1% of hospital costs. Other notable cost buckets were 9.4% for ward supplies (costs for medical and surgical supplies, ward and clinical department overheads, and goods and services), 8.9% for nonclinical salaries (other costs of service provision, predominantly wages for carers such as patient care assistants), 7.9% for on-costs (eg, superannuation, fringe benefits tax, long service leave, worker's compensation, and recruitment), and 7.0% for ED product (ie, the average cost per admitted ED patient).
Figure 2.
The breakdown of all hospital inpatient costs. Deprec = depreciation; EDPro = emergency department produce.
Discussion
This is the first study to quantify the direct medical costs associated with air medical retrievals of patients experiencing mental health crises in Australian rural and remote settings. We estimated that the annual direct medical cost associated with this was $20,070,527 for 2017. Most of these costs were attributable to hospital costs, with over 50% of this expended on ward nursing staff, medical staff, and ward supplies.
Importantly, this total cost represents a substantial underestimate of both the health payer and the societal impacts of these acute mental health events in the rural and remote areas of Australia. More specifically, in regard to the direct medical costs, the costs of the first hospital (or retrieval site) admission for the 926 patients who received an interhospital transfer were not included. Furthermore, the substantial indirect costs associated with air medical retrievals have not been assessed. These costs include those associated with the lost productivity of patients, their families, and caregivers. In addition, intangible costs, largely the suffering associated with a condition that can be captured using quality of life instruments, is likely to be substantial from both a physical and, importantly, from a psychosocial perspective and has not been assessed in this study. For patients, particularly for those experiencing a first episode of psychosis, inpatient admission in addition to air medical retrieval and dislocation from usual social supports and networks can be a traumatic experience, with a recent systematic review reporting 42% of first-episode psychosis patients experienced symptoms of post-traumatic stress disorder.25 Although the impact of this experience is partially understood with patients, less is known regarding the impact and costs for families and caregivers.
Further research is required to fully understand the true costs, including indirect (loss of productivity) and intangible costs (quality of life), associated with air medical retrievals for mental health care and the current level of service provision to rural and remote communities in location. Ultimately, the implications of these health payer and societal costs need to be understood in the context of considered funding and capacity considerations for rural and remote mental health services and providers. Tough longer-term health care policy decisions are required by governments and health planners through the prism of the known economic costs for air medical retrievals, albeit as an underestimate of the likely true costs identified in this study. Additional attention and research are required to qualify the grossly under-researched costs to rural and remote communities of retrieving patients with mental and behavioral disorders out of their communities from a societal impact perspective.
The severe lack of psychiatrists, mental health nurses, psychologists, and social workers in rural and remote areas requires structural change to the supply of a qualified and competent rural and remote workforce. The recent Australian Senate inquiry into the burden of mental health conditions on rural and remote communities recommends longer-term and more flexible funding and contract processes, in addition to working with professional colleges to improve support and training of workers in rural and remote communities, with the goal of supporting high-quality workers and services to remain in communities, thereby providing consistency of service provision.26 Importantly, our article suggests that RFDS air medical retrievals are a symptom of this unmet demand and also a potential proxy for the services and capacity that currently does not exist in rural and remote communities.
To provide high-quality mental health services to rural and remote communities will require adequate resourcing. Although the costs to governments will likely be substantial, we suggest that the societal benefits that will be gained from resourcing action to meet the unmet demand are likely to outweigh these costs. In other words, the poor mental health outcomes experienced by people in rural and remote communities deserves and demands action. Furthermore, we do not understand the impact of high-acuity mental illnesses, the high rates of suicide and substance use on the indirect (productivity) and intangible (quality of life) costs for rural and remote communities, and the Australian society more broadly. It is important to quantify these costs because they are likely to be substantial and offset much of the costs related to the provision of high-quality mental health services for rural and remote communities.
A strength of this article is that it has provided annual direct medical costs associated with air medical retrievals in Australia. These costs have not been quantified before and are important because they can be used to assess the total costs associated with the current approaches to mental health service provision in rural and remote communities. A limitation of this study is that to apply hospital costs from the National Hospital Cost Data Collection, we mapped ICD-10-AM codes (of which there are > 40,000) to the 807 AR-DRG codes costed by the National Hospital Cost Data Collection. As such, the costs reported here are an estimate of the costs to governments through the public hospital system. A further limitation was that we were unable to access the ICD-10-AM codes that were listed for the initial hospital admission before interhospital transfers; therefore, we were unable to apply these costs.
In conclusion, the direct medical costs of air medical retrievals for mental and behavioral disorders in Australia's most remote communities are substantial. The societal implications of these costs to the families and communities of these regions is unknown; nevertheless, the flow-on effects of these societal costs are likely to far exceed the direct medical costs. We challenge policy and decision makers to understand these societal implications for future health policy and planning of mental health services in Australia's rural and remote communities.
Footnotes
Acknowledgment
In-flight patient data were extracted from the confidential Royal Flying Doctor Service data set, and cost data for Australian Refined Diagnosis Related Groups codes were sourced from the publicly available National Hospital Cost Data Collection (2016/2017) website.
References
- 1.Australia Bureau of Statistics . Australia Bureau of Statistics; Canberra, Australia: 2017. Regional population growth, Australia, 2016. [Google Scholar]
- 2.Australian Institute of Health and Welfare . Australian Institute of Health and Welfare; Canberra, Australia: 2019. Rural and remote health. [Google Scholar]
- 3.Coleman M, Playford D. Time to end the drought in the bush. Australas Psychiatry. 2019;27:366–368. doi: 10.1177/1039856219852296. [DOI] [PubMed] [Google Scholar]
- 4.Perkins D, Farmer J, Salvador-Carulla L, Dalton H, Luscombe G. The Orange Declaration on rural and remote mental health. Aust J Rural Health. 2019;27:374–379. doi: 10.1111/ajr.12560. [DOI] [PubMed] [Google Scholar]
- 5.Harrison J, Henley G. Australian Institute of Health and Welfare; Canberra, Australia: 2014. Suicide and hospitalised self-harm in Australia: trends and analysis. [Google Scholar]
- 6.Department of Health . 2016. Australia's Future Health Workforce – Psychiatry. Department of Health.https://www.health.gov.au/internet/main/publishing.nsf/Content/597F2D320AF16FDBCA257F7C0080667F/$File/AFHW%20Psychiatry%20Report.pdf Available at: Published 2016. Accessed April 1, 2020. [Google Scholar]
- 7.Australian Institute of Health and Welfare . 2020. Mental health services in Australia: mental health workforce tables.https://www.aihw.gov.au/reports/mental-health-services/mental-health-services-in-australia/report-contents/mental-health-workforce Available at: Published 2020. Accessed February 20, 2020. [Google Scholar]
- 8.Coleman M, Playford D. Time to end the drought in the bush. Australas Psychiatry. 2019;27:366–368. doi: 10.1177/1039856219852296. [DOI] [PubMed] [Google Scholar]
- 9.Australian Institute of Health and Welfare . Australian Institute of Health and Welfare; Canberra, Australia: 2017. National Drug Strategy Household Survey 2016: detailed findings. [Google Scholar]
- 10.Gardiner FW, Johns H, Bishop L, Churilov L. Royal Flying Doctor Service COVID-19 activity and surge modelling in Australia. Air Medical Journal. 2020 doi: 10.1016/j.amj.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bishop L, Ransom A, Laverty M. Royal Flying Doctor Service. 2017. Health care access, mental health, and preventive health: Health priority survey findings for people in the bush.https://www.flyingdoctor.org.au/assets/files/RN032_Healths_Needs_Survey_Result-no_crop_marks_P3.pdf Available at: Published 2017. Accessed July 4, 2019. [Google Scholar]
- 12.Caldwell TM, Jorm AF, Dear KB. Suicide and mental health in rural, remote and metropolitan areas in Australia. Med J Aust. 2004;181(suppl):S10–S14. doi: 10.5694/j.1326-5377.2004.tb06348.x. [DOI] [PubMed] [Google Scholar]
- 13.Austin EK, Handley T, Kiem AS. Drought-related stress among farmers: findings from the Australian Rural Mental Health Study. Med J Aust. 2018;209:159–165. doi: 10.5694/mja17.01200. [DOI] [PubMed] [Google Scholar]
- 14.Department of Health . 2018. MBS online. Australian Government.http://www.mbsonline.gov.au/internet/mbsonline/publishing.nsf/Content/Home Available at: Published 2018. Accessed June 7, 2018. [Google Scholar]
- 15.Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Oxford University Press; Oxford, UK: 2015. Methods for the Economic Evaluation of Health Care Programmes. [Google Scholar]
- 16.Husereau D, Drummond M, Petrou S. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. BMJ. 2013;346:f1049. doi: 10.1136/bmj.f1049. [DOI] [PubMed] [Google Scholar]
- 17.Royal Flying Doctor Service Victoria . 2018. Annual report. Royal Flying Doctor Service Victoria.https://rfds-media.s3.amazonaws.com/documents/RFDS_Annual_Report_2018_VICTORIA_web_2.pdf?AWSAccessKeyId=AKIA57J6V557HP5WJ6WZ&Expires=1580944769&Signature=5IPwHq4s8clhm%2BbOlKKYu5R6rvo%3D Available at: Published 2018. Accessed February 6, 2020. [Google Scholar]
- 18.World Health Organisation . 2016. International Statistical Classification of Diseases and Related Health Problems, 10th Revision.https://icd.who.int/browse10/2016/en Available at: Published 2016. Accessed January 1, 2019. [Google Scholar]
- 19.O'Connor TM, Hanks HA, Elcock MS, Turner RC, Veitch C. The medical and retrieval costs of road crashes in rural and remote northern Queensland, 2004–2007: findings from the Rural and Remote Road Safety Study. Med J Aust. 2009;190:54–56. doi: 10.5694/j.1326-5377.2009.tb02274.x. [DOI] [PubMed] [Google Scholar]
- 20.Independent Hospital Pricing Authority . IHPA; Canberra: 2019. National Hospital Cost Data Collection Report, Public Sector, Round 21 (Financial year 2016-17) [Google Scholar]
- 21.Health Direct Australia . 2018. Who we are.https://about.healthdirect.gov.au/ Available at: Published 2018. Accessed November 13, 2018. [Google Scholar]
- 22.Australia Bureau of Statistics . Australia Bureau of Statistics; Canberra, Australia: 2016. Australian Statistical Geography Standard (ASGS): Volume 1 - Main Structure and Greater Capital City Statistical Areas, July 2016. [Google Scholar]
- 23.Gardiner FW, Teoh N, Coleman M. Aeromedical retrievals of people for mental health care and the low level of clinical support in rural and remote Australia. Med J Aust. 2019;211:351–356. doi: 10.5694/mja2.50272. [DOI] [PubMed] [Google Scholar]
- 24.Tableau . 2019. Maps.https://www.tableau.com/solutions/maps Available at: Published 2019. Accessed October 11, 2019. [Google Scholar]
- 25.Rodrigues R, Anderson K. The traumatic experience of first-episode psychosis: A systematic review and meta-analysis. Schizophr Res. 2017;189:27–36. doi: 10.1016/j.schres.2017.01.045. [DOI] [PubMed] [Google Scholar]
- 26.The Australian Senate: Community Affairs References Committee . Commonwealth of Australia; Canberra: 2018. Accessibility and quality of mental health services in rural and remote Australia. Senate Inquiry Report. [Google Scholar]