Abstract
Globally, the Coronavirus disease (COVID-19) outbreak is linked with air pollution of both indoor and outdoor environments and co-morbidities conditions of human beings. To find out the risk factor zones associated with Coronavirus disease among under-five children using pre-existing morbidity conditions and indoor air pollution (IAP) environmental factors and also with current fatality and recovery rate of COVID-19 disease in India. Data was utilized from the 4th round of the National Family Health Survey (NFHS), 2015–16, and from the Ministry of Health and Family Welfare (MoHFW) on 18th May 2020. Mean, standard deviation, and Z-score statistical methods have been employed to find out the risk factor zones i.e. to execute the objective. Findings of this study are, the states and UTs which have more likely to very higher to higher risk factors or zones of Coronavirus disease (COVID-19) are Mizoram (1.4), Meghalaya (1.27), Uttarakhand (0.92), West Bengal (0.73), Uttar Pradesh (0.66), Jammu and Kashmir (0.44), Odisha (0.33), Madhya Pradesh (0.21), Jharkhand (0.20), Bihar (0.19), Maharashtra (0.16 risk score), compared to UTs like Assam (-0.12), Rajasthan (-0.13), Goa (-0.14), Manipur (-0.17), Chandigarh (-0.19), Haryana (-0.22), Delhi (-0.27) have moderate risk factors of COVID-19, and the states and UTs like Daman and Diu (-1.18), Sikkim (-0.98), Andaman and Nicobar Islands (-0.84), Kerala (-0.69), Dadra and Nagar Haveli (-0.68), Arunachal Pradesh ( 0.-53), Karnataka (-0.42), and Nagaland (-0.36) have very low-risk zones of COVID-19 deaths. From a research viewpoint, there is a prerequisite need for epidemiological studies to investigate the connection between indoor air pollution and pre-existing morbidity which are associated with COVID-19. Well-built public health measures, including rapidly searching in high focus areas and testing of COVID-19, should be performed in vulnerable areas of COVID-19.
Keywords: Indoor air pollution, Morbidity, COVID-19, Case Fatality Ratio, Risk Factor, India
Graphical abstract
Highlights
-
•
Pre-existing childhood morbidities are risk factors of COVID-19 among under-5 children.
-
•
Children who lived in the indoor smoky environment are linked with COVID-19.
-
•
States and union territories which have in high-risk zones of Coronavirus disease in India.
1. Introduction
Coronavirus disease (COVID-19) outbreak is a global pandemic frightening the whole world amid unexpected emergence and massive spreading of novel Coronavirus (2019-nCoV) or the severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2) (WHO, 2020a, 2020b; Al-Dadah & Hing, 2020; Cucinotta & Vanelli, 2020; Jin et al., 2020; Lai et al., 2020; Peeri et al., 2020; Saha et al., 2020; Singhal, 2020; Sohrabi et al., 2020; Stahel, 2020; Wang et al., 2020). The COVID-19 is a vastly contagious disease rapidly spreading from its origin in Wuhan City, Hubei Province of China to the rest of the world in December 2019. As of May 18, 2020, the COVID-19 outbreak has hit South-East Asia with 143,750 confirmed cases; India has the 11th-largest number of confirmed cases (96,169 cases), already crossing China (WHO, 2020a, 2020b).
In indoor air pollution (IAP), from the indoor biomass combustion, the air pollutants which are emitted include suspended particulate matter (SPM), nitrogen oxides (NOx), carbon monoxide (CO), benzene (C6H6), 1, 3-butadiene (C4H6), methanol (CH2O), polycyclic aromatic hydrocarbons (PAHs), and several toxic organic compounds (World Health Organization, 2006; Sukhsohale et al., 2013; Chakraborty et al., 2014; Air Quality Expert Group, 2017). The cooking fuels which are generally burned for cooking mostly in a rural home and also in urban areas are coal, lignite, charcoal, wood, straw/shrubs/grass, agricultural crop, animal dung, etc. (IIPS, 2017) which are sufficient for the concentration of indoor air pollutants. Smoking of cigarettes, bidis, and pipes within the home or indoor environment are also other responsible factors for the increase of smoky indoor environment (Bruce et al., 2000; Gilmour et al., 2006; Chaouachi, 2009), a risk factor of the Coronavirus disease among under-five children.
The acute respiratory infection (ARI), i.e. executes signs like short and rapid breaths (IIPS, 2017), cold & cough, and fever among human beings are the primary symptoms of the Coronavirus disease (COVID-19) and the severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2) which have widespread effects because it is hazardous or risk factor for children and human beings health having a weak immune system (Jin et al., 2020; Lai et al., 2020; Peeri et al., 2020; Singhal, 2020; Wang et al., 2020; WHO, 2020a, 2020b). These symptoms are quite common among under-five children of developing countries and also in India which have impacts on children’s health (Ramani et al., 2016; Thota et al., 2018; Krishnan et al., 2015). Globally, and also in developing countries like India, the under-five children are most vulnerable groups compared to the other age classes, so we considered only under-five age group and in 2018 an estimated 5.3 million children under the age of 5 years died (UNICEF, 2019), mostly from preventable childhood morbidities. For that very reason, areas with these symptoms are vulnerable/risk zone for the COVID-19 deaths in the coming days.
Several previous studies that have analyzed the indirect effect of the COVID-19 on-air (Fattorini & Regoli, 2020; Bashir et al., 2020; Collivignarelli et al., 2020; Zambrano-Monserrate et al., 2020) and few studies specifically from that have analyzed the effect of lockdown during the COVID-19 pandemic on air quality in India i.e. PM2.5 had the highest reduction in most of the regions amid the COVID-19 lockdown (Sharma et al., 2020); again, PM10 and PM2.5 concentrations over megacity Delhi, have reduced by above 50% in comparison to the before-lockdown period in India i.e. improvement of air quality during the COVID-19 lockdown (Mahato et al., 2020).
So, compared to the other previous studies in India, this type of study is yet not done, considering this huge research gap and novelty, this study also aims to find out the risk factors associated with the Coronavirus disease (COVID-19) among under-five children using pre-existing morbidity conditions and indoor air pollution environmental factors which are solid biomass cooking fuel and indoor smoking cigarettes and also with current case fatality ratio (CFR) and recovery rate (RR) of the COVID-19 disease in the high focusing states and union territories of India which are in a risk zone. This very research would be helpful for policymakers, strategy developers, environmentalists, and public health workers to combat the future pandemic situation.
2. Data and methods
2.1. Data sources
For this study, data were utilized from the 4th round of the National Family Health Survey, 2015–16, consisting of nationally representative sample surveys. A total of 247,743 living children (0–59 months) were surveyed by the National Family Health Survey (NFHS)-4, among them the under-five children having pre-existing morbidities and indoor air pollution characteristics of the states and union territories of India were considered for this study (IIPS, 2017). The data used for this study were retrieved from the public domain after describing the objective of the study.
Data on the COVID-19 is use from the https://www.mohfw.gov.in/naming ‘COVD-19 state-wise status’, provides the most updated figures on the daily and a total number of confirmed cases, recovered or cured cases, and deaths (MoHFW, 2020) for each affected states and union territories of India. This data is provided by the Ministry of Health and Family Welfare (MoHFW), Government of India. We have collect information on confirmed cases, the number of deaths, and cured cases as on May 18, 2020, 08:00 IST (GMT+5:30) of affected states and union territories of India.
2.2. Variables used
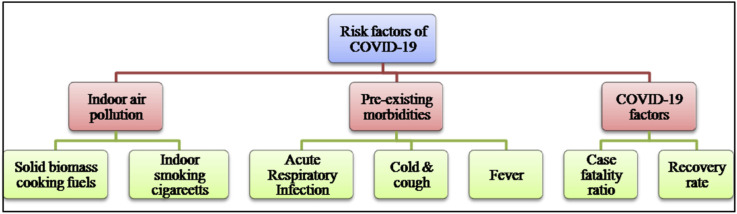
For the analysis of the study, a selection of pre-existing morbidities indicators and indoor air pollution or domestic smoky environmental indicators among under-five children household and recent COVID-19 rates were included. Pre-existing morbidities indicators include symptoms of acute respiratory infection (ARI) in the two weeks before the survey, the prevalence of cold and cough, and the prevalence of fever among under-five children. Indoor domestic smokes indicators include children’s family used smoky domestic cooking fuel and children’s mother smoke cigarettes and recent COVID-19 rates include Case Fatality Ratio (CFR) and Recovery Rate (RR) of different affected states and union territories of India (Fig. 1 ).
Fig. 1.
Conceptual framework of the study.
2.2. Methods
The prevalence of pre-existing childhood morbidities and the percentage of children’s family used indoor domestic smokes were computed using the Statistical Package and Data Science software STATA version 13.1 (StataCorp LP, College Station, TX, USA).
After that, the case fatality ratio has been calculated as the ratio of the total figure of deaths due to COVD-19 to the total figure of confirmed cases of the COVID-19. Likewise, the COVID-19 recovery rate is calculated as the ratio of the total figure of recovered cases of the COVID-19 to the total figure of confirmed cases of the COVID-19.
For identification of risk factors zone of the Coronavirus disease, the mean composite Z-score technique has been employed. All the factors which are taken for this study are positively influenced by the COVID-19 except the factor recovery rate of the COVID-19. For composing, all the selected variables must be working unidirectional manner. So, the factor recovery rate has been converted into a non-recovery rate i.e. each recovery rate of the COVID-19 of all states and UTs is subtracted from 100. After that, for each variable (X1 or X2 and so on) number of observations (states and UTs) are sum up and mean was calculated, then standard deviation was calculated as the root mean square deviation from the mean. The Z-score i.e. risk score also be calculated for identification of risk or vulnerable zones of the COVID-19 using the following formula-
All the Z-score values of all variables for each state and UTs have been calculated then mean was calculated using total Z-score value. High Z-score value indicates high-risk factors of the COVID-19 and vice versa.
3. Results
3.1. Indoor air pollution and pre-existing prevalence of morbidities among under-five children and case fatality ratio and recovery rate of the COVID-19
Table 1 represents the percentage of under-five children with indoor domestic smokes and pre-existing childhood morbidities and the COVID-19 CFR and RR in states and UTs of India. Symptoms of ARI was higher in the states like Meghalaya (5.8%), Jammu and Kashmir (5.4%), Uttar Pradesh (4.7%), Uttarakhand (4.6%), Punjab (4.1%), West Bengal ()3.3%), Jharkhand (3.2%), Haryana (3.2%) compared to other states and UTs. The prevalence of cold & cough was higher in Uttarakhand (22.15%), Meghalaya (20.21%), Mizoram (19.46%), Jammu and Kashmir (14.97%), Puducherry (14.5%), Tamil Nadu (14.37%), Uttar Pradesh (14.26%) compared to other states and UTs. The prevalence of fever was higher in Uttarakhand (24.5%), Meghalaya (23.29%), Uttar Pradesh (19.67%), Telangana (16.59%), and Goa (16.2%) compared to other states. The percentage of children family use smoky cooking fuel or biomass use was higher in the states and UTs like Bihar (88.18%), Jharkhand (86.94%), Odisha (84.1%), Meghalaya (83.67%), Assam (81.68%), Dadra and Nagar Haveli (80.77%), and West Bengal (78.09%) compared to other. The percentage of children’s mother smoke cigarettes was higher in Mizoram (15.15), Sikkim (2.29%), Arunachal Pradesh (0.59%) compared to other states and UTs of India. The case fatality rate is high in West Bengal (8.89%), Meghalaya (7.69%), Puducherry (7.69%), Goa (5.79%), Madhya Pradesh (4.98%), Himachal Pradesh (3.75%), and Maharashtra (3.62%); recovery rates are low in Maharashtra (23.26%), Odisha (26.57%), Chandigarh (26.7%), Manipur (28.57%), West Bengal (35.82%), Tamil Nadu (37.17%), Bihar (37.64%), Gujarat (39.54%) the states & UTs of India.
Table 1.
Percentage of under-five children with IAP and pre-existing morbidities and the COVID-19 Case Fatality Ratio (CFR) and Recovery Rate (RR) in India
| States & Union Territories | Pre-existing morbidities |
Indoor domestic smoky environment |
COVID-19 Case Fatality Ratio (CFR) | COVID-19 Recovery Rate (RR) | |||
|---|---|---|---|---|---|---|---|
| Symptoms of ARI (%) | Prevalence of Cold & Cough (%) | Prevalence of Fever (%) | Percentage of children family use smoky cooking fuel | Percentage of children’s mother smoke cigarettes | |||
| Andaman & Nicobar Islands | 1.5 | 12.89 | 8.62 | 25.83 | 0.00 | 0.00 | 100 |
| Andhra Pradesh | 0.5 | 5.38 | 8.33 | 41.02 | 0.00 | 2.08 | 60.49 |
| Arunachal Pradesh | 2.1 | 10.54 | 11.45 | 59.41 | 0.59 | ||
| Assam | 1.0 | 8.77 | 8.97 | 81.68 | 0.03 | 1.98 | 40.59 |
| Bihar | 2.5 | 10.33 | 12.24 | 88.18 | 0.14 | 0.63 | 37.64 |
| Chandigarh | 2.8 | 10.35 | 9.69 | 10.08 | 0.00 | 1.57 | 26.70 |
| Chhattisgarh | 2.2 | 12.49 | 13.35 | 80.77 | 0.02 | 0.00 | 68.60 |
| Dadra and Nagar Havel | 1.9 | 5.53 | 5.63 | 49.62 | 0.00 | ||
| Daman and Diu | 0.6 | 5.43 | 6.57 | 11.11 | 0.00 | ||
| Delhi | 2.4 | 10.8 | 13.4 | 2.77 | 0.08 | 1.59 | 44.61 |
| Goa | 1.4 | 14.07 | 16.2 | 17.39 | 0.15 | ||
| Gujarat | 1.4 | 9.02 | 8.94 | 55.74 | 0.01 | 5.79 | 39.54 |
| Haryana | 3.2 | 8.87 | 9.24 | 55.69 | 0.04 | 1.54 | 61.76 |
| Himachal Pradesh | 1.6 | 10.78 | 11.84 | 71.87 | 0.02 | 3.75 | 55.00 |
| Jammu and Kashmir | 5.4 | 14.97 | 13.87 | 51.66 | 0.2 | 1.10 | 48.61 |
| Jharkhand | 3.2 | 10.42 | 12.62 | 86.94 | 0.02 | 1.35 | 50.67 |
| Karnataka | 1.2 | 5.76 | 7.05 | 47.57 | 0.07 | 3.23 | 44.38 |
| Kerala | 0.8 | 8.59 | 10.54 | 47.96 | 0.12 | 0.67 | 82.70 |
| Lakshadweep | 0.9 | 12.97 | 13.87 | 59.04 | 0.6 | ||
| Madhya Pradesh | 2.1 | 10.45 | 11.36 | 76.03 | 0.04 | 4.98 | 48.28 |
| Maharashtra | 2.4 | 9.24 | 12.62 | 42.53 | 0.07 | 3.62 | 23.26 |
| Manipur | 0.7 | 12.8 | 8.25 | 60.99 | 0.25 | 0.00 | 28.57 |
| Meghalaya | 5.8 | 20.21 | 23.29 | 83.67 | 0.1 | 7.69 | 84.62 |
| Mizoram | 2.2 | 19.46 | 11.42 | 37.69 | 15.1 | ||
| Nagaland | 1.4 | 8.55 | 7.13 | 75.44 | 0.16 | ||
| Odisha | 2.4 | 12.73 | 12.86 | 84.10 | 0.04 | 0.48 | 26.57 |
| Puducherry | 3.0 | 14.5 | 11.81 | 13.69 | 0.00 | 7.69 | 69.23 |
| Punjab | 4.1 | 13.18 | 13.36 | 39.31 | 0.02 | 1.78 | 69.55 |
| Rajasthan | 2.1 | 8.53 | 9.82 | 74.61 | 0.00 | 2.52 | 57.52 |
| Sikkim | 0.3 | 3.41 | 3.8 | 46.46 | 2.29 | ||
| Tamil Nadu | 2.8 | 14.37 | 10.75 | 25.91 | 0.03 | 0.69 | 37.17 |
| Telangana | 2 | 13.89 | 16.59 | 30.07 | 0.00 | 2.19 | 63.96 |
| Tripura | 2.6 | 12.88 | 11.67 | 70.76 | 0.03 | 0.00 | 50.90 |
| Uttar Pradesh | 4.7 | 14.26 | 19.67 | 73.48 | 0.04 | 2.44 | 57.31 |
| Uttarakhand | 4.6 | 22.15 | 24.5 | 57.39 | 0.03 | 1.09 | 56.52 |
| West Bengal | 3.3 | 11.00 | 12.57 | 78.09 | 0.01 | 8.89 | 35.82 |
3.2. Mean composite risk score factors of the coronavirus disease (COVID-19) among under-five children
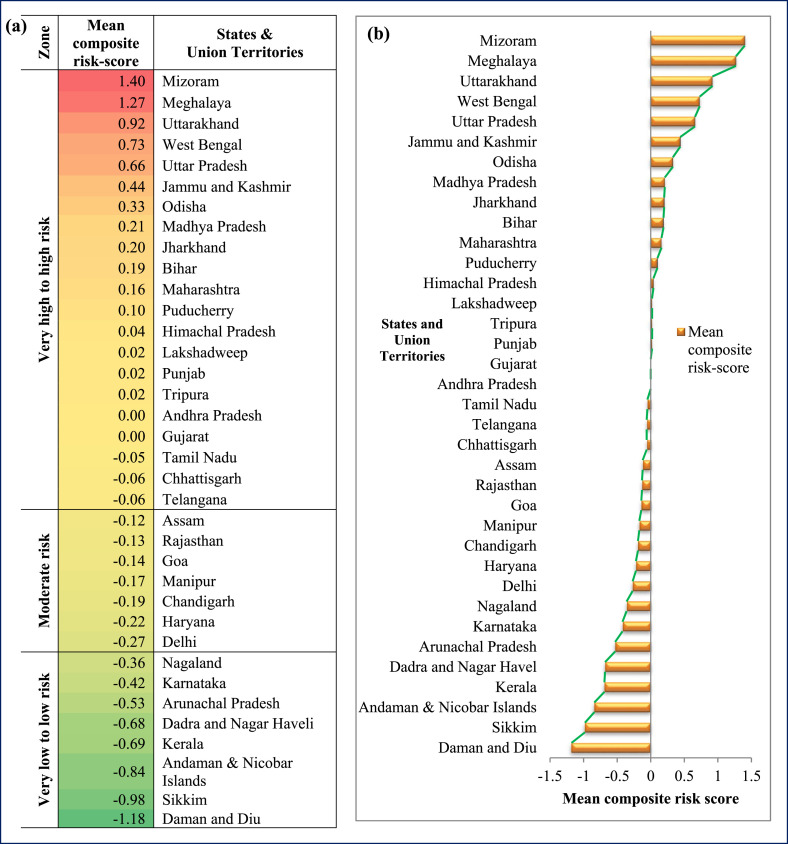
Table 2 represents, mean composite risk score of various indicators of indoor domestic smoky environment or indoor air pollution and pre-existing morbidities among under-5 children with the COVID-19 Case Fatality Ratio (CFR) and Recovery Rate (RR) in states & union territories of India. The states and UTs which have more likely to very higher to higher risk factors or zones of the Coronavirus disease (COVID-19) are Mizoram (1.4), Meghalaya (1.27), Uttarakhand (0.92), West Bengal (0.73), Uttar Pradesh (0.66), Jammu and Kashmir (0.44), Odisha (0.33), Madhya Pradesh (0.21), Jharkhand (0.20), Bihar (0.19), Maharashtra (0.16 risk score), showed in color ramp of red to yellow (Fig. 2 (a)) compared to the states and UTs like Assam (−0.12), Rajasthan (−0.13), Goa (−0.14), Manipur (−0.17), Chandigarh (−0.19), Haryana (−0.22), Delhi (−0.27) have moderate risk factors of the COVID-19, showed in color ramp of light yellow to light yellow-greenish (Fig. 2(a)) and the states and UTs like Daman and Diu (−1.18), Sikkim (−0.98), Andaman and Nicobar Islands (−0.84), Kerala (−0.69), Dadra and Nagar Haveli (−0.68), Arunachal Pradesh (0.-53), Karnataka (−0.42), and Nagaland (−0.36) showed in color ramp of green to light greenish-yellow (Fig. 2(a)) have very low-risk factors of COVID-19. The states and UTs with 0 to <1.35 composite score i.e. high (0 to −0.06), moderate (−0.12 to −0.27), and low to very low (−0.42 to −1.35) risk score factors of the Coronavirus disease (Fig. 2(b)).
Table 2.
Mean composite risk score of different indicators of indoor domestic smoky environment use and pre-existing morbidities among under-5 children with the COVID-19 Case Fatality Ratio (CFR) and Recovery Rate (RR) in states & union territories of India
| States & Union Territories | X1 | X2 | X3 | X4 | X5 | X6 | X7 | Mean composite risk-score |
|---|---|---|---|---|---|---|---|---|
| Andaman & Nicobar Islands | −0.6 | 0.4 | −0.7 | −1.1 | −0.2 | −1 | −2.6 | −0.84 |
| Andhra Pradesh | −1.3 | −1.5 | −0.8 | −0.5 | −0.2 | −0.86 | ||
| Arunachal Pradesh | −0.2 | −0.2 | −0.1 | 0.3 | 0 | −1 | −2.6 | −0.53 |
| Assam | −1 | −0.6 | −0.6 | 1.2 | −0.2 | −0.2 | 0.6 | −0.12 |
| Bihar | 0.1 | −0.3 | 0.1 | 1.4 | −0.2 | −0.7 | 0.8 | 0.19 |
| Chandigarh | 0.4 | −0.3 | −0.5 | −1.8 | −0.2 | −0.4 | 1.4 | −0.19 |
| Chhattisgarh | −0.1 | 0.3 | 0.4 | 1.1 | −0.2 | −1 | −0.9 | −0.06 |
| Dadra and Nagar Havel | −0.3 | −1.4 | −1.4 | −0.1 | −0.2 | −0.68 | ||
| Daman and Diu | −1.3 | −1.5 | −1.2 | −1.7 | −0.2 | −1.18 | ||
| Delhi | 0.1 | −0.1 | 0.4 | −2.1 | −0.2 | −0.4 | 0.4 | −0.27 |
| Goa | −0.7 | 0.7 | 1 | −1.5 | −0.2 | −0.14 | ||
| Gujarat | −0.7 | −0.6 | −0.7 | 0.1 | −0.2 | 1.3 | 0.7 | 0.00 |
| Haryana | 0.7 | −0.6 | −0.6 | 0.1 | −0.2 | −0.4 | −0.5 | −0.22 |
| Himachal Pradesh | −0.5 | −0.1 | 0 | 0.8 | −0.2 | 0.5 | −0.1 | 0.04 |
| Jammu and Kashmir | 2.3 | 0.9 | 0.5 | −0.1 | −0.1 | −0.6 | 0.2 | 0.44 |
| Jharkhand | 0.7 | −0.2 | 0.2 | 1.4 | −0.2 | −0.5 | 0.1 | 0.20 |
| Karnataka | −0.8 | −1.4 | −1.1 | −0.2 | −0.2 | 0.3 | 0.4 | −0.42 |
| Kerala | −1.1 | −0.7 | −0.3 | −0.2 | −0.2 | −0.7 | −1.6 | −0.69 |
| Lakshadweep | −1 | 0.4 | 0.5 | 0.2 | 0 | 0.02 | ||
| Madhya Pradesh | −0.2 | −0.2 | −0.1 | 0.9 | −0.2 | 1 | 0.2 | 0.21 |
| Maharashtra | 0.1 | −0.5 | 0.2 | −0.4 | −0.2 | 0.5 | 1.6 | 0.16 |
| Manipur | −1.2 | 0.3 | −0.8 | 0.3 | −0.1 | −1 | 1.3 | −0.17 |
| Meghalaya | 2.6 | 2.2 | 2.7 | 1.2 | −0.2 | 2.1 | −1.7 | 1.27 |
| Mizoram | −0.1 | 2 | −0.1 | −0.6 | 5.8 | 1.40 | ||
| Nagaland | −0.7 | −0.7 | −1.1 | 0.9 | −0.2 | −0.36 | ||
| Odisha | 0.1 | 0.3 | 0.3 | 1.3 | −0.2 | −0.8 | 1.4 | 0.33 |
| Puducherry | 0.5 | 0.8 | 0 | −1.6 | −0.2 | 2.1 | −0.9 | 0.10 |
| Punjab | 1.3 | 0.4 | 0.4 | −0.6 | −0.2 | −0.3 | −0.9 | 0.02 |
| Rajasthan | −0.2 | −0.7 | −0.5 | 0.9 | −0.2 | 0 | −0.3 | −0.13 |
| Sikkim | −1.5 | −2 | −1.8 | −0.3 | 0.7 | −0.98 | ||
| Tamil Nadu | 0.4 | 0.7 | −0.2 | −1.1 | −0.2 | −0.7 | 0.8 | −0.05 |
| Telangana | −0.2 | 0.6 | 1.1 | −0.9 | −0.2 | −0.1 | −0.6 | −0.06 |
| Tripura | 0.2 | 0.4 | 0 | 0.7 | −0.2 | −1 | 0.1 | 0.02 |
| Uttar Pradesh | 1.8 | 0.7 | 1.8 | 0.8 | −0.2 | 0 | −0.3 | 0.66 |
| Uttarakhand | 1.7 | 2.6 | 2.9 | 0.2 | −0.2 | −0.6 | −0.2 | 0.92 |
| West Bengal | 0.7 | −0.1 | 0.2 | 1 | −0.2 | 2.6 | 0.9 | 0.73 |
| Mean | 2.3 | 11.4 | 11.8 | 53.2 | 0.6 | 2.5 | 47.5 | |
| Standard Deviation (σ) | 1.3 | 4.1 | 4.3 | 24.5 | 2.5 | 2.5 | 18.6 |
X1 = Prevalence of Acute Respiratory Infections (ARI) (%), X2 = Prevalence of cold & cough (%), X3 = Prevalence of Fever (%), X4 = Percentage of children family use smoky cooking fuel (smoky environment), X5 = Percentage of children’s mother smoke cigarettes (smoky environment), X6 = Case Fatality Ratio (CFR), X7 = Non-Recovery Rate (RR).
Fig. 2.
States and union territories across India with risk factors of Coronavirus disease (COVID-19) among Under-five children.
4. Discussion
Worldwide, till May 18, 2020 as of 6:51 p.m. CEST, 4,628,903 confirmed cases of the Coronavirus disease, including 312,009 deaths have been reported and 216 countries, territories have been affected by the COVID-19 pandemic (WHO, 2020a, 2020b). In India, as of May 19, 2020 as of 08:00 IST (GMT+5:30), Ministry of Health and Family Welfare, the Government of India reported, a total of 1,01,139 confirmed cases and 3163 deaths have been reported speeded over 33 states and UTs (MoHFW, 2020).
The present study has examined the risk factors of the Coronavirus disease (COVID-19). As the Coronavirus has been associated with indoor air pollution and a smoky environment, so, there has a relationship between indoor cooking fuel used with biomass and the Coronavirus disease (COVID-19) (Afshari, 2020). The under-five children living in indoor smoky environmental conditions are most vulnerable and risk of the Coronavirus disease. This study is consistent with the study done by Ahmed et al. (2020), and a significant relationship between exposure to air pollution and deaths due to the COVID-19 was found in United States (Wu et al., 2020). They use of solid biomass for cooking fuels and burning inside their houses with poor vitalization system and no chimneys were found to direct the smoke outside in urban slums of Bangalore, India (Ghergu et al., 2016). So, we found that these indoor air pollution conditions are extremely at risk or vulnerable to the COVID-19 infection. Those people staying in an area with intense high amounts of pollutants are, therefore, more likely to develop severe respiratory conditions and also at risk of any infective disease (Conticini et al., 2020).
In this study among children’s mothers with smoking cigarettes is a risk factor of the COVID-19 among under-five children in India. This finding is in agreement with another study conducted in China, where hospitalized patients of the COVID-19 with smoking behavior were 14 times high likely to expire or die compared to the patients those were non-smokers (Liu et al., 2020), and in Saudi Arab (Alraddadi et al., 2016). The states and UTs with high case fatality ratio and air pollution are risk factors of the COVID-19 in affected states and UTS of India. This finding was similar to another study in the people’s Republic of China i.e. the high prevalence of confirmed/infected cases and deaths of severe acute respiratory syndrome Coronavirus 1 (SARS-CoV-1) were associated with air pollution (Cui et al., 2003) and in Northern Italy, higher prevalence and mortality of the COVID-19 was also associated with air pollution (Conticini et al., 2020).
Indoor air pollution or indoor domestic smoky environment and pre-existing morbidities are the risk factors of health among children with under-five age. Indoor air quality directly linked to the respiratory system of living peoples and dependence on hard biomass for cooking and burning or heating exposes respiratory health problem of children of developing countries as well as in India due to use lofty levels of indoor air pollution (Padhi and Padhy, 2008; Bruce et al., 2015; Mandal et al., 2020). Pre-existing morbidities like acute respiratory infection (ARI), cold & cough, and fever among under-five children in India have also risk factors of the Coronavirus disease (COVID-19). In earlier studies, it is found that pre-existing co-morbidities among children are risk factors of the COVID-19 death (Sinha et al., 2020; Shekerdemian et al., 2020).
5. Limitations of the study
The measurement of CFR amid the COVID-19 outbreak is not very suitable, because it is sensitive to under-reporting, testing of the COVID-19 cases and moment of reporting and robust estimation of CFR is likely possible only at the end of the COVID-19 pandemic. Recovery Rate also varies and daily changes during the pandemic situation, so these are few limitations of this study. Surveyed women have self-reported about their children’s pre-existing childhood morbidities, so there is a possibility of recall bias during the collection of information about children.
6. Conclusion
From a research viewpoint, there is a prerequisite for epidemiological studies to investigate the relationship between indoor air pollution and pre-existing morbidity which are associated with the COVID-19. More focus needs to place on improving cooking stoves and use clean indoor cooking fuels should become a top concern in the high focus vulnerable region. The children should be kept away from the kitchen during the cooking and burning of fuels. The kitchen room should have extensive space so that air pollutants smokes are not being capable to concentrate within the room for a long period, which reduces indoor air pollution, which is the risk factor of the COVID-19. Smokers of the family should also stay away from indoor house environment when smoking. Finally, well-built public health proceedings, including rapidly searching in high focus areas and testing of the COVID-19, should be performed in vulnerable areas of the COVID-19.
CRediT authorship contribution statement
Jay Saha: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Supervision, Validation, Visualization, Writing - original draft, Writing - review & editing. Pradip Chouhan: Conceptualization, Formal analysis, Investigation, Methodology, Software, Supervision, Validation, Visualization, Writing - original draft.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
This paper has been recommended for acceptance by Da Chen.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envpol.2020.115250.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Afshari R. Indoor air quality and severity of COVID-19: where communicable and non- communicable preventive measures meet. Asia Pacific Journal of Medical Toxicology. 2020;9(1):1–2. [Google Scholar]
- Ahmed F., Ahmed N.E., Pissarides C., Stiglitz J. Why inequality could spread COVID-19. The Lancet Public Health. 2020;5(5):e240. doi: 10.1016/S2468-2667(20)30085-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Air Quality Expert Group . Department for Environment, Food and Rural Affairs; Scottish Government; Welsh Government; and Department of the Environment in Northern Ireland; 2017. The Potential Air Quality Impacts from Biomass Combustion. [Google Scholar]
- Al-Dadah O., Hing C. Novel coronavirus (COVID-19): a global pandemic. Knee. 2020;27(2):279. doi: 10.1016/j.knee.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alraddadi B.M., Watson J.T., Almarashi A., Abedi G.R., Turkistani A., Sadran M., Housa A., Almazroa M.A., Alraihan N., Banjar A., Albalawi E. Risk factors for primary Middle East respiratory syndrome coronavirus illness in humans, Saudi Arabia, 2014. Emerg. Infect. Dis. 2016;22(1):49. doi: 10.3201/eid2201.151340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bashir M.F., Bilal B.M., Komal B. Environmental Research; 2020. Correlation between Environmental Pollution Indicators and COVID-19 Pandemic: A Brief Study in Californian Context; p. 109652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce N., Perez-Padilla R., Albalak R. Indoor air pollution in developing countries: a major environmental and public health challenge. Bull. World Health Organ. 2000;78:1078–1092. https://www.scielosp.org/article/bwho/2000.v78n9/1078-1092/en/#end [PMC free article] [PubMed] [Google Scholar]
- Bruce N., Pope D., Rehfuess E., Balakrishnan K., Adair-Rohani H., Dora C. WHO indoor air quality guidelines on household fuel combustion: strategy implications of new evidence on interventions and exposure–risk functions. Atmos. Environ. 2015;106:451–457. doi: 10.1016/j.atmosenv.2014.08.064. [DOI] [Google Scholar]
- Chakraborty D., Mondal N.K., Datta J.K. Indoor pollution from solid biomass fuel and rural health damage: a micro-environmental study in rural area of Burdwan, West Bengal. Int. J. Sustain. Built Environ. 2014;3(2):262–271. doi: 10.1016/j.ijsbe.2014.11.002. [DOI] [Google Scholar]
- Chaouachi K. Hookah (shisha, narghile) smoking and environmental tobacco smoke (ETS). A critical review of the relevant literature and the public health consequences. Int. J. Environ. Res. Publ. Health. 2009;6(2):798–843. doi: 10.3390/ijerph6020798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collivignarelli M.C., Abbà A., Bertanza G., Pedrazzani R., Ricciardi P., Miino M.C. Lockdown for CoViD-2019 in Milan: what are the effects on air quality? Sci. Total Environ. 2020;732:139280. doi: 10.1016/j.scitotenv.2020.139280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conticini E., Frediani B., Caro D. Can atmospheric pollution be considered a co- factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environ. Pollut. 2020:114465. doi: 10.1016/j.envpol.2020.114465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cucinotta D., Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed.: Atenei Parmensis. 2020;91(1):157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui Y., Zhang Z.F., Froines J., Zhao J., Wang H., Yu S.Z., Detels R. Air pollution and case fatality of SARS in the People’s Republic of China: an ecologic study. Environ. Health. 2003;2(1):15. doi: 10.1186/1476-069X-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fattorini D., Regoli F. Environmental Pollution; 2020. Role of the Chronic Air Pollution Levels in the Covid-19 Outbreak Risk in Italy; p. 114732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghergu C., Sushama P., Vermeulen J., Krumeich A., Blankvoort N., van Schayck O.C., de Witte L.P. Dealing with indoor air pollution: an ethnographic tale from urban slums in Bangalore. Int. J. Health Sci. Res. 2016;6:348–361. [Google Scholar]
- Gilmour M.I., Jaakkola M.S., London S.J., Nel A.E., Rogers C.A. How exposure to environmental tobacco smoke, outdoor air pollutants, and increased pollen burdens influences the incidence of asthma. Environ. Health Perspect. 2006;114(4):627–633. doi: 10.1289/ehp.8380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iips I.C.F. International Institute for Population Sciences (IIPS); Mumbai, India: 2017. National Family Health Survey (NFHS-4), 2015–16.http://rchiips.org/nfhs/NFHS- 4Reports/India.pdf [Google Scholar]
- Jin Y., Yang H., Ji W., Wu W., Chen S., Zhang W., Duan G. Virology, epidemiology, pathogenesis, and control of COVID-19. Viruses. 2020;12(4):372. doi: 10.3390/v12040372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnan A., Amarchand R., Gupta V., Lafond K.E., Suliankatchi R.A., Saha S., Rai S., Misra P., Purakayastha D.R., Wahi A., Sreenivas V. Epidemiology of acute respiratory infections in children-preliminary results of a cohort in a rural north Indian community. BMC Infect. Dis. 2015;15(1):462. doi: 10.1186/s12879-015-1188-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai C.C., Shih T.P., Ko W.C., Tang H.J., Hsueh P.R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and corona virus disease-2019 (COVID-19): the epidemic and the challenges. Int. J. Antimicrob. Agents. 2020:105924. doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu W., Tao Z.W., Wang L., Yuan M.L., Liu K., Zhou L., Wei S., Deng Y., Liu J., Liu H.G., Ming Y. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chin. Med. J. 2020 doi: 10.1097/CM9.0000000000000775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahato S., Pal S., Ghosh K.G. Science of the Total Environment; 2020. Effect of Lockdown amid COVID-19 Pandemic on Air Quality of the Megacity Delhi, India; p. 139086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandal S., Zaveri A., Mallick R., Chouhan P. 2020. Impact of Domestic Smokes on the Prevalence of Acute Respiratory Infection (ARI) Among Under-five Children: Evidence from India. Children and Youth Services Review; p. 105046. [DOI] [Google Scholar]
- MoHFW . Government of India; New Delhi: 2020. COVID-19 Statewise Status.https://www.mohfw.gov.in/ [Google Scholar]
- Padhi B.K., Padhy P.K. Domestic fuels, indoor air pollution, and children’s health: the case of rural India. Ann. N. Y. Acad. Sci. 2008;1140(1):209–217. doi: 10.1196/annals.1454.015. [DOI] [PubMed] [Google Scholar]
- Peeri N.C., Shrestha N., Rahman M.S., Zaki R., Tan Z., Bibi S., Baghbanzadeh M., Aghamohammadi N., Zhang W., Haque U. The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: what lessons have we learned? Int. J. Epidemiol. 2020 doi: 10.1093/ije/dyaa033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramani V.K., Pattankar J., Puttahonnappa S.K. Acute respiratory infections among under-five age group children at urban slums of gulbarga city: a longitudinal study. J. Clin. Diagn. Res.: J. Clin. Diagn. Res. 2016;10(5):LC08. doi: 10.7860/JCDR/2016/15509.7779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha J., Barman B.B., Chouhan P. 2020. Lockdown for COVID-19 and its Impact on Community Mobility in India: an Analysis of the COVID-19 Community Mobility Reports, 2020. Children And Youth Services Review; p. 105160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma S., Zhang M., Gao J., Zhang H., Kota S.H. Effect of restricted emissions during COVID-19 on air quality in India. Sci. Total Environ. 2020;728:138878. doi: 10.1016/j.scitotenv.2020.138878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shekerdemian L.S., Mahmood N.R., Wolfe K.K., Riggs B.J., Ross C.E., McKiernan C.A., Heidemann S.M., Kleinman L.C., Sen A.I., Hall M.W., Priestley M.A. Characteristics and outcomes of children with coronavirus disease 2019 (COVID-19) infection admitted to US and Canadian pediatric intensive care units. JAMA Pediatr. 2020 doi: 10.1001/jamapediatrics.2020.1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singhal T. A review of coronavirus disease-2019 (COVID-19) Indian J. Pediatr. 2020:1–6. doi: 10.1007/s12098-020-03263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha I.P., Harwood R., Semple M.G., Hawcutt D.B., Thursfield R., Narayan O., Kenny S.E., Viner R., Hewer S.L., Southern K.W. 2020. COVID-19 Infection in Children. The Lancet. Respiratory Medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohrabi C., Alsafi Z., O’Neill N., Khan M., Kerwan A., Al-Jabir A., Iosifidis C., Agha R. World Health Organization declares global emergency: a review of the 2019 novel Coronavirus (COVID-19) Int. J. Surg. 2020 doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stahel P.F. 2020. How to Risk-Stratify Elective Surgery during the COVID-19 Pandemic? [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sukhsohale N.D., Narlawar U.W., Phatak M.S. Indoor air pollution from biomass combustion and its adverse health effects in central India: an exposure-response study. Indian J. Community Med.: Off. Publ. Ind. Assoc. Prevent. Soc. Med. 2013;38(3):162. doi: 10.4103/0970-0218.116353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thota S., Ladiwala N., Sharma P.K., Ganguly E. Fever awareness, management practices and their correlates among parents of under five children in Urban India. Int. J. Contemp. Pediatr. 2018;5(4):1368. doi: 10.18203/2349-3291.ijcp20182525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF . 2019. Children: Reducing Mortality, Key Facts.https://www.who.int/news-room/fact-sheets/detail/children-reducing-mortality [Google Scholar]
- Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Who . World Health Organization. World Health Organization; 2020. WHO Coronavirus Disease (COVID-19) Dashboard.https://www.who.int/ [Google Scholar]
- World Health Organization . World Health Organization; 2006. Air Quality Guidelines: Global Update 2005: Particulate Matter, Ozone, Nitrogen Dioxide, and Sulfur Dioxide. [Google Scholar]
- World Health Organization . vol. 10. World Health Organization; 2020. (Coronavirus Disease 2019 (COVID-19): Situation Report). [Google Scholar]
- Wu X., Nethery R.C., Sabath B.M., Braun D., Dominici F. 2020. Exposure to Air Pollution and COVID-19 Mortality in the United States. medRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zambrano-Monserrate M.A., Ruano M.A., Sanchez-Alcalde L. Science of the Total Environment; 2020. Indirect effects of COVID-19 on the environment; p. 138813. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.