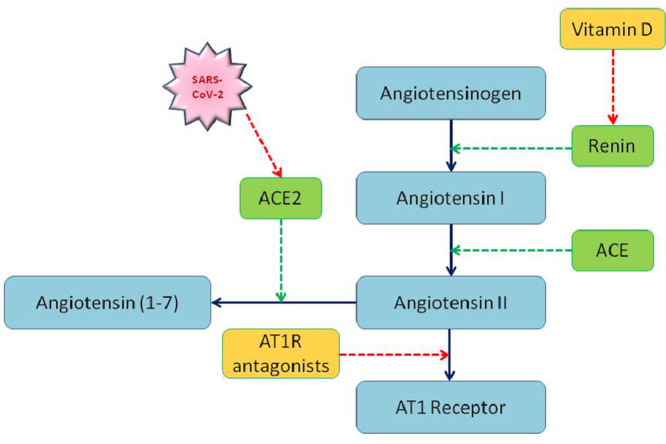
Graphical Abstract
Key Indexing Terms: Coronavirus, SARS-CoV-2, COVID-19, SARS
Abstract
Severe Acute Respiratory Distress Syndrome caused by a novel human coronavirus SARS-CoV-2 named COVID-19 and declared as a pandemic. This paper reviews the possibility of repurposing angiotensin type 1 receptor (AT1R) antagonists and vitamin D to treat COVID-19. ACE2 protein found on the cell membranes is the target of SARS-CoV-2 for entering into the host cells. Viral spike protein-binding with ACE2 down-regulates it. As ACE2 is known to protect the lung from injuries, SARS-CoV-2-induced ACE2 deficiency may expose patients to lung damage. AT1R antagonists and vitamin D increase the expression of ACE2 independently. Besides, vitamin D suppresses the compensatory increase in renin levels following the inhibition of the renin-angiotensin system by AT1R antagonists. Therefore, a combination of AT1R antagonists and vitamin D may offer protection against COVID-19 induced lung injury.
Introduction
A novel human coronavirus named SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) emerged from Wuhan, China, since Dec 2019.1 It causes Acute Respiratory Distress Syndrome (ARDS) in susceptible patients. SARS-CoV-2 binds with angiotensin-converting enzyme 2 (ACE2) molecule for entry into the human cells.2 The previous SARS-CoV infections were found to down-regulate the expression of ACE2 molecule.3 Lower ACE2 levels are implicated in lung injury, whereas higher levels are protective against lung injuries.4 Low ACE2 is also reported among aged men5 and in chronic disease conditions.4 The mortality rate of COVID-19 has been high among older people and those with pre-existing comorbidities such as diabetes and hypertension. Decreased levels of ACE2 in SARS-CoV-2 infections could predispose people to severe COVID-19 complications. Elevating the ACE2 levels in patients may protect them from the lung complications of COVID-19. Treatment with angiotensin type 1 receptor (AT1R) antagonists and vitamin D supplementation may present a simpler and effective way of improving ACE2 levels safely among patients. This review elaborates on the idea of using AT1R antagonists and vitamin D for treating serious lung complications of SARS-CoV-2.
Mechanism of SARS-CoV-2 entry into human cells
The entry mechanism of SARS-CoV-2 is similar to that of SARS-CoV. Viral spike S glycoprotein has to be primed by the host cell proteases before binding with the receptors. The SARS-CoV-2 uses ACE2 as the entry receptor.6 Viral entry is dependent on the S protein priming by host cell surface-associated transmembrane protease serine 2. In virus infectivity studies, SARS-CoV-2 could not enter the HeLa cells that did not express ACE2 proteins. The binding affinity of SARS-CoV-2 S protein with ACE2 is 10-20 folds higher than that of SARS-CoV. The lung alveolar epithelial cells, heart, kidney, and enterocytes of the small intestine express ACE2 protein.7
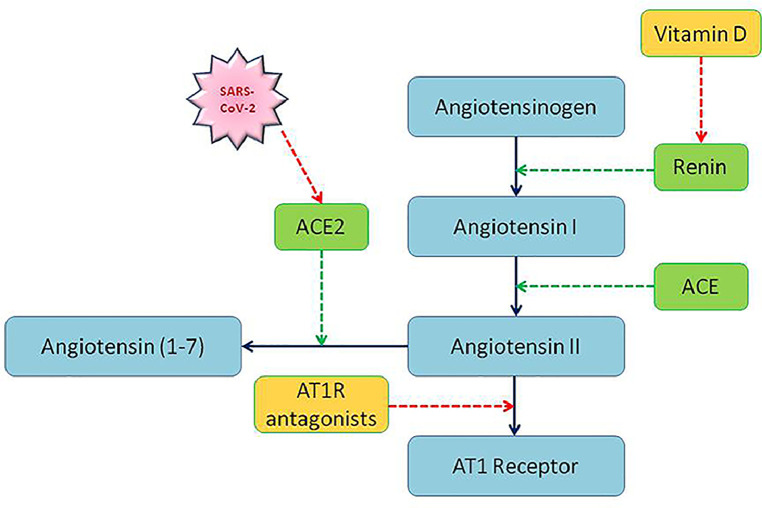
Angiotensin-converting enzyme (ACE) increases the blood pressure by converting the inactive angiotensin I to active angiotensin II which in turn binds with angiotensin type 1 receptor (AT1R) to induce vasoconstriction. ACE2 is a counter-regulatory enzyme in the renin-angiotensin system (RAS). It cleaves the angiotensin II into a potent vasodilating heptapeptide known as angiotensin 1-7.8 Binding of SARS-CoV spike protein to ACE2 in cell lines and SARS-CoV infections in animals reduced the expression of ACE2 protein. The acute lung injury (ALI) resulting from the SARS-CoV infection was shown to be mediated through the down-regulation of ACE2 in mice. ALI deteriorated after SARS-CoV spike protein administration in mice whereas, inhibition of the RAS rescued the animals. Lungs of SARS-CoV infected mice showed decreased ACE2 protein while ACE levels remained normal. ACE2 protected mice from ALI, while ACE and angiotensin II worsened it.9
ACE2 levels in patients with comorbid conditions
Angiotensin 1-7, the product of ACE2 action, has a wide range of anti-inflammatory and antioxidant properties. Infusion of angiotensin 1-7 resulted in the attenuation of vascular dysfunction and atherosclerosis in mice through the activation of Mas and angiotensin type 2 (AT2) receptors. The imbalance between angiotensin II and angiotensin 1-7 plays a crucial role in the pathophysiology of vascular diseases. Lower levels of ACE2 are implicated in several conditions such as hypertension, atherosclerosis, heart failure, diabetic nephropathy, and lung injury.4 , 10 Expectedly hypertension and diabetes have been the most common comorbidities associated with severe cases of COVID-19.11, 12, 13
ACE2 has a beneficial effect on the lungs and protects it from severe injury.14 In ACE2 deficient conditions, excessive angiotensin II causes increased vascular permeability, vasoconstriction, and inflammation in the lungs leading to ALI. ACE2 down-regulation by SARS-CoV infection was found in severe lung failure and was associated with mortality in SARS infection.9 Similarly, in SARS-CoV-2 infection, the ACE2 deficiency after the viral spike binding and the subsequent imbalance in the RAS may mediate the ALI. A recent study on the clinical and biochemical indexes of COVID-19 patients showed angiotensin II levels were markedly higher than healthy individuals and were linearly associated with the viral load and lung injury.15.
Increasing ACE2 levels as a strategy in treating COVID-19
As ACE2 protein protects the lungs, and COVID-19 patients have lower levels of ACE2, increasing the ACE2 level is likely to protect against SARS-CoV-2 induced lung injury. Therapeutic approaches to increase ACE2 levels may work as a good strategy in treating SARS-CoV-2 infections. AT1R antagonists can be used to increase ACE2 protein levels. ACE inhibitors are not preferred because they cause cough, a common adverse effect associated with their use. ACE2 being the target molecule of SARS-CoV-2 viral spike protein, increasing its level may also increase the viral load. However, the European Society of Cardiology Council on Hypertension stated that there is no evidence supporting any harmful effect of ACE inhibitors in COVID-19 infections. It even hinted about the possible beneficial effects of ACE inhibitors while referring observations from animal studies.16 Recently there are suggestions to use AT1R antagonists as a strategy of increasing ACE2 levels for treating COVID-19 infections.17, 18, 19
Effect of vitamin D on RAS
Vitamin D has a negative regulatory role on the RAS. Suppression of RAS by AT1R antagonists results in a feedback-induced compensatory increase in renin. Vitamin D blocks the rise in renin at the transcriptional level when given in combination with a RAS inhibitor such as AT1R antagonists or ACE inhibitors.20 Renin is an enzyme involved in the production of angiotensin II. It converts angiotensinogen to angiotensin I, a precursor of angiotensin II. Inhibition of renin will decrease the levels of pro-inflammatory angiotensin II and alleviate lung injury. Vitamin D was effective in attenuating the lipopolysaccharide-induced ALI in rats by modulating the RAS. It inhibited renin, ACE and angiotensin II expression and induced ACE2 levels.21 With its inhibitory effect on renin, the simultaneous administration of vitamin D may complement the effect of AT1R antagonists (Figure 1). Besides, vitamin D has a direct protective effect on the lungs. Its deficiency appeared to contribute to the ARDS22 and was associated with increased admissions to the intensive care unit and mortality in patients with pneumonia. Vitamin D status was associated with 30 days mortality rate in patients with community-acquired pneumonia.23 A retrospective study on Korean patients with ARDS showed that vitamin D deficiency was prevalent among them, and the serum levels correlated inversely with length of hospital stay and intensive care unit stay among in-hospital survivors.24
Figure 1.
Blocking renin and AT1 receptor to increase ACE2 and angiotensin (1-7).
Vitamin D inhibits pulmonary inflammatory responses and improves the host defense mechanisms against respiratory infections.25 In a meta-analysis of individual patient data from 25 randomized controlled trials, vitamin D supplementation reduced the risk of acute respiratory tract infection among participants26 A review showed the effect of vitamin D in lowering viral epidemics, respiratory tract infections, and the reduction of inflammatory responses in pneumonia.27 Recently there was a commentary about the possible benefit of vitamin D in COVID-19 patients.28
Summary
AT1R antagonists or vitamin D or a combination could prove to be beneficial in COVID-19 patients who are prone to have lung complications. However, the role of these drugs in patients who do not develop any lung injury is unclear. As there are no available proven treatments for COVID-19 infection, the possibility of using drugs like AT1R antagonists and vitamin D to prevent or lessen the severity of acute lung complications of COVID-19 needs investigation. These widely available, inexpensive drugs may help alleviate the massive burden of managing severe COVID-19 cases.
Conclusions
The present review indicates that AT1R antagonists or vitamin D or a combination may be useful in treating the lung complication of COVID-19. Appropriately designed clinical studies are needed to establish the benefit of the combination of AT1R antagonists with vitamin D.
Acknowledgment
The author would like to acknowledge the National Plan for Science, Technology and Innovation (MAARIFAH), King Abdul‐Aziz City for Science and Technology, Kingdom of Saudi Arabia, grant to the Strategic Center for Diabetes Research, the College of Medicine, King Saud University.
Footnotes
Conflicts of Interest: The author declares no conflicts of interest regarding the publication of this paper.
References
- 1.World Health Organization.Naming the coronavirus disease (COVID-19) and the virus that causes it. Country & Technical Guidance - Coronavirus disease (COVID-19). Available at:https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it. Published 2020. Accessed March 18, 2020.
- 2.Wan Y, Shang J, Graham R, et al. Receptor Recognition by the Novel Coronavirus from Wuhan: an Analysis Based on Decade-Long Structural Studies of SARS Coronavirus. Gallagher T, ed. J Virol. 2020;94 doi: 10.1128/JVI.00127-20. e00127-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dijkman R, Jebbink MF, Deijs M, et al. Replication-dependent downregulation of cellular angiotensin-converting enzyme 2 protein expression by human coronavirus NL63. J Gen Virol. 2012;93:1924–1929. doi: 10.1099/vir.0.043919-0. [DOI] [PubMed] [Google Scholar]
- 4.Tikellis C, Thomas MC. Angiotensin-Converting Enzyme 2 (ACE2) Is a Key Modulator of the Renin Angiotensin System in Health and Disease. Int J Pept. 2012;2012 doi: 10.1155/2012/256294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xie X, Chen J, Wang X, et al. Erratum to “Age- and gender-related difference of ACE2 expression in rat lung” (DOI:10.1016/j.lfs.2005.09.038) Life Sci. 2006;79:2499. doi: 10.1016/j.lfs.2006.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hoffmann M, Kleine-Weber H, Schroeder S, et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell. 2020: 1-10. doi:10.1016/j.cell.2020.02.052 [DOI] [PMC free article] [PubMed]
- 7.Zhou P, Yang X-L, Wang X-G, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Keidar S, Kaplan M, Gamliel-Lazarovich A. ACE2 of the heart: From angiotensin I to angiotensin (1–7) Cardiovasc Res. 2007;73:463–469. doi: 10.1016/j.cardiores.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 9.Kuba K, Imai Y, Rao S, et al. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus–induced lung injury. Nat Med. 2005;11:875–879. doi: 10.1038/nm1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Christos T, I. JC, M. FJ, et al. Characterization of Renal Angiotensin-Converting Enzyme 2 in Diabetic Nephropathy. Hypertension. 2003;41:392–397. doi: 10.1161/01.HYP.0000060689.38912.CB. [DOI] [PubMed] [Google Scholar]
- 11.Guan W-J, Ni Z-Y, Hu Y, et al. China Medical Treatment Expert Group for Covid-19. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020:1–13. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang D, Hu B, Hu C, et al. Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA - J Am Med Assoc. 2020:1–9. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang J jin, Dong X, Cao Y yuan, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy Eur J Allergy Clin Immunol. 2020;00:1–12. doi: 10.1111/all.14238. [DOI] [PubMed] [Google Scholar]
- 14.Imai Y, Kuba K, Rao S, et al. Angiotensin-converting enzyme 2 protects from severe acute lung failure. Nature. 2005;436:112–116. doi: 10.1038/nature03712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu Y, Yang Y, Zhang C, et al. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci China Life Sci. 2020;63:364–374. doi: 10.1007/s11427-020-1643-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Simone G de.Position Statement of the ESC Council on Hypertension on ACE-Inhibitors and Angiotensin Receptor Blockers. Position Statement.https://www.escardio.org/Councils/Council-on-Hypertension-(CHT)/News/position-statement-of-the-esc-council-on-hypertension-on-ace-inhibitors-and-ang. Published 2020. Accessed March 29, 2020.
- 17.Henry BM, Jens V, Giuseppe L. Response to the emerging novel coronavirus outbreak Read our latest coverage of the Coronavirus outbreak Rapid Response. Br Med J. 2020;368:m406. doi: 10.1136/bmj.m406. [DOI] [PubMed] [Google Scholar]
- 18.Gurwitz D. Angiotensin receptor blockers as tentative SARS-CoV-2 therapeutics. Drug Dev Res. 2020:2–5. doi: 10.1002/ddr.21656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kickbusch I, Leung G. Response to the emerging novel coronavirus outbreak. BMJ. 2020;368:m406. doi: 10.1136/bmj.m406. [DOI] [PubMed] [Google Scholar]
- 20.Li YC. Molecular mechanism of vitamin D in the cardiovascular system. J Investig Med. 2011;59:868–871. doi: 10.2310/JIM.0b013e31820ee448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xu J, Yang J, Chen J, et al. Vitamin D alleviates lipopolysaccharide-induced acute lung injury via regulation of the renin-angiotensin system. Mol Med Rep. 2017;16:7432–7438. doi: 10.3892/mmr.2017.7546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dancer RCA, Parekh D, Lax S, et al. Vitamin D deficiency contributes directly to the acute respiratory distress syndrome (ARDS) Thorax. 2015;70:617–624. doi: 10.1136/thoraxjnl-2014-206680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Remmelts HHF, van de Garde EMW, Meijvis SCA, et al. Addition of Vitamin D Status to Prognostic Scores Improves the Prediction of Outcome in Community-Acquired Pneumonia. Clin Infect Dis. 2012;55:1488–1494. doi: 10.1093/cid/cis751. [DOI] [PubMed] [Google Scholar]
- 24.Park S, Lee MG, Hong SB, et al. Effect of vitamin D deficiency in korean patients with acute respiratory distress syndrome. Korean J Intern Med. 2018;33:1129–1136. doi: 10.3904/kjim.2017.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hughes DA, Norton R. Vitamin D and respiratory health. Clin Exp Immunol. 2009;158:20–25. doi: 10.1111/j.1365-2249.2009.04001.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martineau AR, Jolliffe DA, Hooper RL, et al. Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ. 2017;356:i6583. doi: 10.1136/bmj.i6583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grant WB, Lahore H, McDonnell SL, et al. Vitamin D Supplementation Could Prevent and Treat Influenza, Coronavirus, and Pneumonia Infections. Nutrients. 2020;12:988. doi: 10.20944/PREPRINTS202003.0235.V1. [DOI] [Google Scholar]
- 28.Garami AR. Rapid Response: Re: Preventing a covid-19 pandemic - Is there a magic bullet to save COVID-19 patients? We can give it a try! Br Med J. 2020;368:m810. doi: 10.1136/bmj.m810. [DOI] [PubMed] [Google Scholar]