Abstract
STUDY QUESTION
What is the performance of the patient-centredness of endometriosis care in a secondary and a tertiary care setting and how can it be improved?
SUMMARY ANSWER
Overall, patient-centredness was comparable in the two endometriosis care centres, but differed regarding ‘physical comfort’ and ‘continuity and transition’; both centres can learn how to improve several of their targets from the other’s strengths.
WHAT IS KNOWN ALREADY
The ENDOCARE questionnaire (ECQ) is a validated questionnaire for assessing the important quality dimension ‘patient-centredness’. Patient-centredness is associated with quality of life, although this should be explored further by larger-scale studies.
STUDY DESIGN, SIZE, DURATION
A cross-sectional survey, relying on the ECQ, was performed (during 2015 and 2016) among 407 women with surgically diagnosed endometriosis.
PARTICIPANTS/MATERIALS, SETTING, METHODS
This study was conducted in a secondary and a tertiary care centre in the Netherlands. A total of 209 Dutch-speaking women who had endometriosis surgery (2013–2014), completed the ECQ after a postal invitation and, if needed, postal reminders. The assessed outcomes were: overall patient-centredness, the patient-centredness for each of its 10 dimensions, and the patient-centred strengths and targets for improvement. Case-mix adjusted patient-centredness scores (PCS) were compared and strengths and targets for improvement were identified with a matrix modelling importance against experience. The need to improve the targets was quantified with quality impact indices.
MAIN RESULTS AND THE ROLE OF CHANCE
No difference was demonstrated between the overall PCS of the secondary and tertiary centres (respectively: 4.8 and 4.5; P = 0.15). No difference was found in PCS per dimension between the two clinics except for the secondary care centre performing better regarding ‘physical comfort’ (respectively: 4.5 and 3.0; P = 0.01) and ‘continuity and transition’ (respectively: 6.0 and 4.2; P = 0.01). The two centres had nine targets for improvement in common. The secondary and tertiary centres, respectively, had five and seven additional centre-specific targets for improvement. Cross-centre learning is encouraged as 9 out the 12 additional centre-specific targets were strengths in the other centre. The main improvement targets were being able to contact the centre in case of emergency (both centres), the involvement of a significant other (secondary centre), diagnostic delay (secondary centre), personal follow-up (tertiary centre) and disclosing the level of competence of healthcare providers (tertiary centre).
LIMITATIONS, REASON FOR CAUTION
Responders did not differ from non-responders in their stage of endometriosis, educational level, rating of endometriosis care and degree to which their complaints are suppressed. Endometriosis is a chronic condition and patient-centredness might be experienced differently at other points of the endometriosis care trajectory.
WIDER IMPLICATION OF THE FINDINGS
The ECQ is a useful tool to assess patient-centredness in both secondary and tertiary care centres. Further research should focus on how to improve endometriosis care.
STUDY FUNDING/COMPETING INTEREST(S)
No external funding was used. V.M. and C.B.L. report grants from Guerbet, grants from Merck and grants from Ferring outside the submitted work. All authors declare that they have no competing interests concerning this publication.
Keywords: endometriosis, quality of care, patient-centredness, ENDOCARE questionnaire
WHAT DOES THIS MEAN FOR PATIENTS?
One of the options to optimise quality of care is to improve patient-centredness of care. Patient-centred care is care that is respectful of patient preferences, needs and values. Patient-centred care also takes patients’ cultures and their community into account. For endometriosis care, patient-centredness can be measured by using the ENDOCARE questionnaire (ECQ).
In this study, we used the ECQ to evaluate the patient-centredness in a secondary and tertiary care centre. By doing this, we were able to compare patient-centredness between the two care centres. We found no differences in overall patient-centredness between the secondary and tertiary care centre. Furthermore, we were able to identify overlapping strengths and overlapping targets for improvement and we were able to identify the targets with the highest need to improve. The endometriosis care centres can use these results to improve their endometriosis care.
Introduction
Endometriosis is a chronic, cyclic, debilitating disease that can cause pain and/or infertility (Giudice, 2010). Women with endometriosis may require long-term hormonal, surgical and/or fertility treatment, which entails frequent consultations with doctors and other healthcare providers (Giudice, 2010). Multiple studies have shown that women with endometriosis report lower quality of live compared to women without endometriosis (Friedl et al., 2015; De Graaff et al., 2016; Marinho et al., 2018). Furthermore, women with endometriosis score higher on anxiety and depression scales compared to women without endometriosis (Sepulcri Rde and do Amaral, 2009; Chen et al., 2016).
Current guidelines for endometriosis treatment mainly focus on the effectiveness and safety of care by decreasing pain, improving quality of life and pursuing pregnancy (Practice Committee of the American Society for Reproductive Medicine, 2012, 2014; Dunselman et al., 2014). Although ‘patient-centredness’ is one of the six dimensions of quality of care (World Health Organization, 2006), quality management rarely focusses on the patient’s preferences and needs. This is especially regrettable as a recent slightly underpowered study suggested that patient-centred care experiences are associated with the healthcare outcome ‘endometriosis specific quality of life’ (Apers et al., 2018).
In order to improve patient-centred endometriosis care, it is important to understand what aspects are most important to women with endometriosis. Recently, a qualitative study identified specific patients’ needs in endometriosis management (Rowe et al., 2019). Rowe et al. found three domains of endometriosis care that could influence patient satisfaction with endometriosis care: (i) information that meets patients’ needs; (ii) being heard with empathy and respect; and (iii) technical competence. Similar domains were also found by two previous questionnaire studies investigating patient satisfaction (Lukas et al., 2018; Wygant et al., 2019).
In women with endometriosis, patient-centredness can be measured with the ENDOCARE questionnaire (ECQ), which has been validated in tertiary care centres (Dancet et al., 2011, 2012). The current study aimed to investigate patient-centredness of endometriosis care in a secondary care setting and a tertiary care setting and aimed to investigate how patient-centredness can be improved.
Materials and methods
Settings
A cross-sectional cohort study was performed (2015–2016) in two Dutch endometriosis care centres: (i) the Isala clinic, a secondary care centre and (ii) Amsterdam University Medical Center, Vrije Universiteit Amsterdam, a tertiary care centre. In the Dutch healthcare system, women with complaints are referred to a gynaecologist by their general practitioner. The general practitioner is the gatekeeper for referral to specialised (gynaecological) care in the Netherlands. Usually, women are first referred to a secondary (non-academic) care physician. The secondary care physician can refer women to a tertiary (academic) care centre, but sometimes women can also be referred to a tertiary care centre directly by their general practitioners. In the Netherlands, the patients’ organisation gives an online overview of care centres that are specialised in endometriosis.
The participating secondary care centre is specialised in endometriosis care and is a member of the Dutch association of top clinical teaching hospitals (‘Samenwerkende Topklinische opleidingsZiekenhuizen (STZ)’). The secondary care centre has an endometriosis team consisting of gynaecologists, pain specialists, radiologists, urologists, colorectal surgeons, sexologists and social workers, closely collaborating with its IVF clinic. The participating tertiary care centre is an expertise centre for severe endometriosis, recognised by the Dutch Federation of University Medical Centers. The tertiary care centre has an endometriosis team consisting of gynaecologists, pain specialists, radiologists, urologists, colorectal surgeons, pulmonologists, thorax surgeons and psychologists. The tertiary centre closely collaborates with its IVF clinic, offering advanced fertility treatments including oocyte donation and gestational surrogacy. Due to the geographical positions of both Dutch centres and to the fact that the secondary care centre refers patients to another, closer by, tertiary care centre when necessary, an overlap in patient populations was ruled out. Both care centres adhere to the same international guideline on diagnosing and treating endometriosis (Dunselman et al., 2014) and are in close collaboration with the Dutch Endometriosis Society.
Participants
All Dutch-speaking women, over 18 years of age, who underwent endometriosis surgery for treating pain and/or infertility in one of the two centres during two consecutive years (2013 and 2014), were approached for this cross-sectional survey. The diagnosis of endometriosis was surgically made and did not have to be confirmed by histology.
Recruitment
Two questionnaires, the ECQ (Dancet et al., 2011) and a short questionnaire on current treatment and perceived side effects, were sent by mail to all eligible women in 2015 and 2016. As this study was part of a larger study investigating experiences and quality of life, women received a total of three questionnaires. In case of non-response, a maximum of two reminders were sent out.
All returned questionnaires were analysed according to the manual (Dancet et al., 2012). If more than one answer was given, the most negative answer was selected for analysis as the aim of the study was to investigate which care aspects should be improved. Questionnaires were excluded from analysis if fewer than 50% of the questions had been answered.
Ten per cent of the non-responders were randomly selected using an online randomiser (www.random.org). If we did not succeed in reaching a woman after three attempts at different times during the day, the next woman on the list was contacted. The selected non-responders were questioned by telephone on whether or not they received the questionnaires, the severity of their endometriosis disease (self-reported stage of endometriosis), the severity of their endometriosis complaints (on a scale from 0 to 10), use of medication and judgement on endometriosis care (on a scale from 0 to 10) as well as their highest level of education.
The ECQ
The ECQ has proven validity and reliability on two levels: first, at country level using input from members of patient associations and patients from two tertiary care centres for endometriosis through a web-based survey (Dancet et al., 2011), and second, at the level of tertiary care centres to assess and compare patient-centredness of two tertiary endometriosis care clinics in Belgium and the Netherlands (Dancet et al., 2012).
The ECQ assesses 38 aspects of endometriosis care in one investigated endometriosis care centre. Women with endometriosis rate the importance and performance of the care aspects on a four-point Likert scale. These 38 care aspects can be grouped into the 10 dimensions of patient-centred endometriosis care: (i) respect for patients’ values, preferences and expressed needs; (ii) coordination and integration of care; (iii) information and communication; (iv) physical comfort; (v) emotional support and alleviation of fear and anxiety; (vi) involvement of significant other; (vii) continuity and transition; (viii) access to care; (ix) technical skills; and (x) endometriosis clinic staff. Examples of care aspects belonging to the specific dimensions are presented in Table I.
Table I.
Examples of care aspects per dimension.
| Dimension | Example of ECQ care aspect |
|---|---|
| 1. Respect for patients’ values, preferences and expressed needs | My complaints were taken seriously. |
| 2. Coordination and integration of care | Care was taken to plan examinations and treatments on 1 day. |
| 3. Information and communication | Everything necessary was done so that I would understand the information given. |
| 4. Physical comfort | The consultation waiting room is comfortable. |
| 5. Emotional support and alleviation of fear and anxiety | I was informed as to the psychological impact of endometriosis. |
| 6. Involvement of significant other | There were efforts to involve my partner during consultations. |
| 7. Continuity and transition | The physician who is treating me really follows up my case personally. |
| 8. Access to care | I was able to contact a caregiver with specific knowledge of endometriosis in urgent cases. |
| 9. Technical skills | I was able to rely on the expertise of the caregivers. |
| 10. Endometriosis clinic staff | The caregivers were understanding and concerned during my treatment. |
The ECQ generates different outcomes. First, the ‘percentage of negative performance (PNP)’ can be calculated using the scores on performance. PNP is a score from 0 to 100, with higher scores representing a more negative experience. Care aspects with a PNP lower than 15% indicate good performance (Slack, 1994; Dancet et al., 2012). Second, the ‘mean importance scores (MIS)’ is a score from 0 to 10, with higher scores representing more important aspects. MIS can be calculated using the scores on importance per care aspect. All care aspects with an MIS higher than the overall MIS (i.e. a mean MIS of all 38 care aspects) are considered the most important aspects. Third, ‘patient-centredness scores (PCS)’ can be calculated at dimension level as follows: MIS × (100−PNP)/100. A PCS of 0 represents the least and 10 represent the most patient-centred care. Fourth, a weighed mean overall PCS can be calculated and be adjusted for differences between clinics in case-mix, if indicated (Dancet et al., 2011, 2012).
Strengths are care aspects that are important (MIS > mean MIS) and have a fair performance (PNP < 15%). Targets for improvement are care aspects that are important (MIS > mean MIS) and have poor performance (PNP > 15%). To identify the targets for improvement with the highest need for improvement, quality impact indices (QII) were calculated for each target for improvement that was identified (QII = MIScare aspect × PNPcare aspect/100) (van Campen et al., 1998). QIIs range from 0 to 10, with a higher score representing a care aspect with a higher need for improvement.
Outcomes
The primary outcome was the overall PCS. Secondary outcomes included PCS per dimension, characteristics of non-responders, strengths and targets for improvement in endometriosis care in the secondary and tertiary care centres, and identification of targets with the highest need for improvement.
Analysis
Statistical analysis was performed using SPSS statistics (IBM version 22). All tests were two-sided, P-values below 0.05 were considered significant and no correction was made for multiple testing, given the exploratory nature of this study. The background characteristics of the respondents are presented separately for the secondary and tertiary care centres. Differences between the care centres are examined with Mann–Whitney U test. The characteristics of responders and non-responders are compared using Mann–Whitney U test and χ2 test.
Differences in patient-centredness
PCS per dimension and the overall PCS were compared between the tertiary and secondary care centres using the Mann–Whitney U test. To account for possible confounding of this comparison, we additionally performed multivariable linear regression analysis with the PCS score as a dependent variable and with care centre together with all confounding variables on which centres were found to differ significantly as independent variables. Again, this was done separately for each PCS dimension and the overall PCS. Normality of residuals of linear regression models was verified visually by means of normal-probability plots.
Strengths and targets for improvement
Strengths and targets for improvement were identified per centre and QIIs were computed for the targets for improvement.
Ethical approval
Ethical approval was granted by the institutional review board of the Amsterdam UMC, Vrije Universiteit Amsterdam (ref number 2015.174).
Results
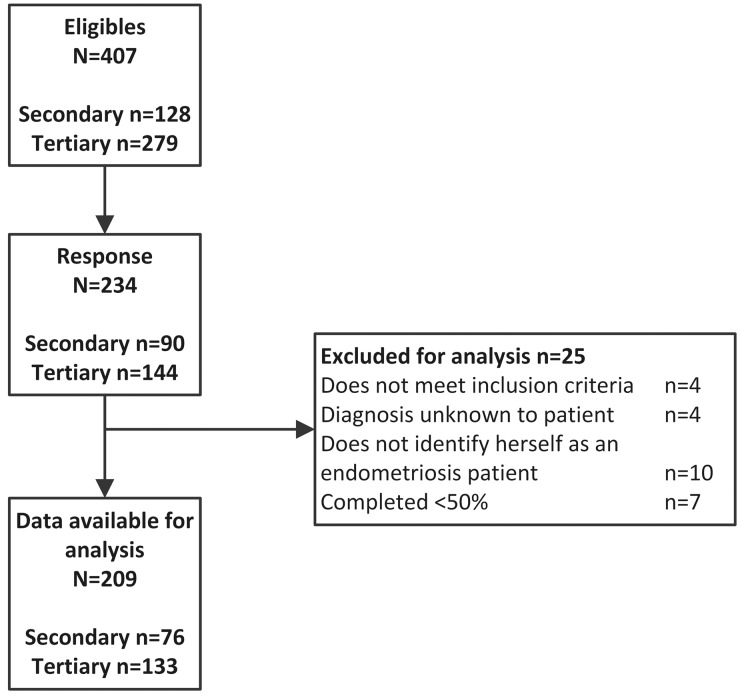
The majority of the addressed women responded (n = 234/407) and data from 209 women were included for analysis. From the secondary care centre, 76 respondents were included and from the tertiary care centre, 133 respondents were included (Figure 1).
Figure 1.
Flow chart of responders.
The background characteristics of the responding women are shown in Table II. Compared to women from the secondary care centre, women from the tertiary care centre were significantly older, had more education, and were more likely to have had a pregnancy in the past. In addition, women from the tertiary care centre had a longer doctor-related diagnostic delay, had more often asked a second opinion from at least one gynaecologist and had more often been referred to other specialists due to endometriosis-related symptoms. There were no differences between the responders and the non-responders.
Table II.
Background characteristics of respondents.
| Secondary care centre (n = 76) | Tertiary care centre (n = 133) | P-value | |
|---|---|---|---|
| Age (median (IQR)) | 34.0 (30–39) | 36.0 (33–40) | 0.02 |
| Ethnic background | 0.08 | ||
| European | 56 (73.7%) | 106 (79.7%) | |
| Other | 4 (5.5%) | 20 (15.0%) | |
| Education | <0.01 | ||
| Higher | 33 (43.4%) | 84 (63.2%) | |
| Lower | 42 (55.3%) | 49 (36.8%) | |
| Currently in an intimate partner relationship | 65 (85.5%) | 123 (92.5%) | 0.17 |
| Endometriosis complaints present at time of diagnosis | |||
| Infertility | 28 (47.5%) | 63 (56.3%) | 0.27 |
| Dysmenorrhea | 66 (88.0%) | 106 (82.2%) | 0.27 |
| Dyspareunia | 37 (60.7%) | 47 (43.9%) | 0.04 |
| Chronic pelvic pain | 33 (52.4%) | 48 (44.9%) | 0.34 |
| Endometriosis complaints present in the past year | 62 (81.6%) | 105 (78.9%) | 0.72 |
| Infertility | 30 (39.5%) | 70 (52.6%) | 0.24 |
| Dysmenorrhea | 51 (67.1%) | 65 (48.9%) | 0.06 |
| Dyspareunia | 36 (47.4%) | 57 (42.9%) | 0.67 |
| Chronic pelvic pain | 26 (34.2%) | 53 (39.8%) | 0.34 |
| Stage of endometriosis (self-reported) | |||
| Minimal/mild | 31 (40.8%) | 43 (32.3%) | 0.19 |
| Moderate/sever | 43 (56.6%) | 88 (66.2%) | |
| Diagnostic delay, years (median (IQR)) | 1.0 (0–9.5) | 2.0 (0–12) | 0.81 |
| Doctors’ delay, years (median (IQR)) | 0.0 (0–4.3) | 1.0 (0–6) | 0.01 |
| Patients’ delay, years (median (IQR)) | 0.0 (0–2) | 0.0 (0–1) | 0.13 |
| Amount of GP consultations before referral (median (IQR)) | 2.0 (1–7) | 2.0 (1–5) | 0.62 |
| Self-reported child wish characteristics | |||
| Ever been pregnant | 38 (50.0%) | 96 (72.2%) | <0.01 |
| Ever tried to conceive >12 months | 46 (60.5%) | 94 (70.7%) | 0.17 |
| Has one or more child(ren) | 32 (42.1%) | 60 (45.1%) | 0.73 |
| Wish for (more) children in future | 53 (69.7%) | 100 (75.2%) | 0.49 |
| Endometriosis pain resulted in not considering pregnancy | 11 (14.5%) | 24 (18.0%) | 0.59 |
| Second opinion of >1 gynaecologist | 20 (26.3%) | 61 (45.9%) | 0.01 |
| Referred to another specialist for endometriosis-related symptoms | 37 (48.7%) | 87 (65.4%) | 0.02 |
| Surgery by multidisciplinary team | 19 (25.0%) | 36 (27.1%) | 0.47 |
| Member of patients’ organization | 7 (9.2%) | 12 (9.0%) | 0.94 |
Patient-centredness score
The overall PCS and PCS per dimension are presented in Table III. We were not able to demonstrate a difference in the mean PCS between the two care centres after case-mix adjustment for the confounders: age, educational level, doctors’ delay, whether women have ever been pregnant, dyspareunia as a first endometriosis symptom, second opinion of more than one gynaecologist, and whether women have ever been referred to another specialist for endometriosis-related symptoms (P = 0.14). Compared to the secondary centre, the tertiary centre had a lower PCS for the dimensions ‘physical comfort’ (adjusted mean difference −0.88, 95% confidence interval −1.546 to −0.216) and ‘continuity and transition’ (adjusted mean difference −0.96, 95% confidence interval −1.71 to −0.20).
Table III.
Patient-centredness scores .
| Secondary care centre (n = 76), median (IQR) | Tertiary care centre (n = 133), median (IQR) | P-value after adjustment | |
|---|---|---|---|
| Overall PCS | 4.8 (3.9–5.7) | 4.5 (3.5–5.6) | 0.15 |
| PCS 1 Respect for patients’ values, preferences and needs | 7.0 (5.8–8.7) | 7.3 (6.0–10.0) | 0.84 |
| PCS 2 Coordination and integration of care | 4.2 (2.0–6.0) | 4.2 (3.0–6.0) | 0.27 |
| PCS 3 Information, communication and education | 6.0 (4.3–7.1) | 6.0 (4.3–7.0) | 0.54 |
| PCS 4 Physical comfort | 4.5 (3.0–6.0) | 3.0 (2.2–6.0) | 0.01 |
| PCS 5 Emotional support and alleviation of fear and anxiety | 0.9 (0.0–2.0) | 0.7 (0.0–2.0) | 0.70 |
| PCS 6 Involvement of significant others | 2.3 (0.3–4.0) | 1.9 (0.4–3.9) | 0.54 |
| PCS 7 Continuity and transition | 6.0 (4.0–8.3) | 4.2 (3.3–6.0) | 0.01 |
| PCS 8 Access to care | 4.8 (3.2–6.0) | 4.3 (3.2–6.0) | 1.00 |
| PCS 9 Technical skills | 6.0 (4.5–8.0) | 6.0 (3.9–8.0) | 0.44 |
| PCS 10 Endometriosis clinic staff | 6.0 (6.0–8.7) | 6.0 (5.0–7.3) | 0.06 |
Data are presented as the median (IQR). IQR, inter-quartile range.
Strengths and targets for improvement
As visualised in Tables IV and V, 9 strengths and 14 targets for improvement were found in the secondary care centre and 6 strengths and 17 targets for improvement were found in the tertiary care centre.
Table IV.
The secondary care centre: strenghts and targets for improvement with quality impact indices.
| Q | Targets for improvement - secondary care centre | QII |
|---|---|---|
| 1 | My complaints were taken seriously | 1.30 |
| 9 | I received practical information and advice on self-care after the operation | 1.22 |
| 10 | The information given to me by the various caregivers was uniform | 1.34 |
| 11 | I was given the opportunity to discuss my daily complaints with the caregivers | 1.07 |
| 12 | I received information on the medication that I could take to relieve my pain | 1.11 |
| 21 | There were efforts to involve my partner during consultations | 2.34 |
| 25 | I received sufficient information regarding recovery after the operation | 1.68 |
| 27 | The physician who is treating me really follows up on my case personally | 1.60 |
| 29 | The waiting time between the diagnostic examinations and the operation was acceptable | 1.22 |
| 32 | I was able to contact a caregiver with specific knowledge of endometriosis in urgent cases | 1.91 |
| 33 | The waiting time between the diagnostic examinations and/or the operation and the discussion of the result was acceptable | 1.35 |
| 35 | My physician clearly stated what complexity level of endometriosis he/she was able to treat; where necessary I was referred in good time to a specialist centre | 1.85 |
| 36 | My physicians were proactive; they did not adopt a wait-and-see approach | 1.34 |
| 37 | I received a correct diagnosis within a short timespan: the endometriosis problem was recognised as such within a short time period | 2.20 |
| Q | Strengths—secondary care centre | |
|---|---|---|
| 2 | I was given the opportunity to take part in the decision after I had received all the information | |
| 3 | I was treated like a person and not like a number | |
| 6 | Everything necessary was done so that I would understand the information given | |
| 7 | I received the information on the course of treatment and the various stages in advance so that I knew what to expect | |
| 18 | The caregivers were understanding and concerned during my treatment | |
| 19 | I was reassured whenever necessary | |
| 26 | It was clear which caregiver I could turn to with questions and/or complaints after the operation | |
| 34 | I was able to rely on the expertise of the caregivers | |
| 38 | The professional caregivers were friendly |
Bold = corresponding views in both clinics.
Italics = opposing views in both clinics: Target for improvement in one clinic and strength in the other.
Q = reference to care aspect in the ECQ.
QII, quality impact indices.
Table V.
The tertiary care centre: strenghts and targets for improvement with quality impact indices.
| Q | Targets for improvement - tertiary care centre | QII |
|---|---|---|
| 3 | I was treated like a person and not like a number | 1.64 |
| 4 | The information regarding my health problem was distributed among the caregivers involved | 1.48 |
| 6 | Everything necessary was done so that I would understand the information given | 1.20 |
| 9 | I received practical information and advice on self-care after the operation | 1.24 |
| 10 | The information given to me by the various caregivers was uniform | 1.33 |
| 11 | I was given the opportunity to discuss my daily complaints with the caregivers | 1.30 |
| 18 | The caregivers were understanding and concerned during my treatment | 1.14 |
| 19 | I was reassured whenever necessary | 1.31 |
| 25 | I received sufficient information regarding recovery after the operation | 1.38 |
| 26 | It was clear which caregiver I could turn to with questions and/or complaints after the operation | 1.58 |
| 27 | The physician who is treating me really follows up on my case personally | 3.18 |
| 30 | I was able to contact my attending physician | 1.08 |
| 32 | I was able to contact a caregiver with specific knowledge of endometriosis in urgent cases | 2.02 |
| 33 | The waiting time between the diagnostic examinations and/or the operation and the discussion of the result was acceptable | 1.07 |
| 34 | I was able to rely on the expertise of the caregivers | 1.33 |
| 35 | My physician clearly stated what complexity level of endometriosis he/she was able to treat; where necessary I was referred in good time to a specialist centre | 2.19 |
| 36 | My physicians were proactive; they did not adopt a wait-and-see approach | 1.54 |
|
| ||
| Q | Strengths—tertiary care centre | |
|
| ||
| 1 | My complaints were taken seriously | |
| 2 | I was given the opportunity to take part in the decision after I had received all the information | |
| 7 | I received the information on the course of treatment and the various stages in advance so that I knew what to expect | |
| 12 | I received information on the medication that I could take to relieve my pain | |
| 37 | I received a correct diagnosis within a short timespan: the endometriosis problem was recognised as such within a short time period | |
| 38 | The professional caregivers were friendly | |
Bold = corresponding views in both clinics.
Italics = opposing views in both clinics: Target for improvement in one clinic and strength in the other.
Q = reference to care aspect in the ECQ.
QII, quality impact indices.
Participants from the two centres had some corresponding views as the two care centres shared three strengths and nine targets for improvement as shown in bold type in Tables IV and V. In contrast, opposing views on the endometriosis care of the two centres were found as nine care aspects were identified as a strength in one care centre and as a target for improvement in the other, as shown in italics in Tables IV and V.
The most important care aspects to improve for the secondary endometriosis care centre were: (i) involvement of partner during consultations; (ii) receiving the correct diagnosis in a short time period; and (iii) the ability to contact a healthcare provider with specific knowledge of endometriosis in urgent cases (quality impact indices (QII) of 2.34, 2.20 and 1.92, respectively). The most important care aspect to improve for the tertiary endometriosis care centre were: (i) personal follow-up of the treating physician; (ii) disclosure of the level of competence of the physician; and (iii) the ability to contact a healthcare provider with specific knowledge of endometriosis in urgent cases ((QII) of 3.18, 2.19 and 2.02, respectively).
Discussion
This study identified centre-specific strengths and targets for improvement of patient-centredness of endometriosis care. Furthermore, this study found no differences in the case-mix adjusted overall PCS between a Dutch secondary and a tertiary endometriosis care centre. To our knowledge, this is the first study comparing the patient-centredness in these two types of endometriosis care centres.
In accordance with our results, no major differences were found previously in overall PCS between two tertiary care centres (Dancet et al., 2012). This could be due to the fact that only centres that already devote their attention to patient-centredness were included and therefore they show comparable care.
‘Emotional support and alleviation of fear and anxiety’ and ‘Involvement of significant others’ had a PSC below 2.5, which indicates poor performance. Dancet et al. (2012) also found a low score for ‘Emotional support and alleviation of fear and anxiety’. To address the poor performance of the aforementioned scores, it is important to understand the underlying cause. Future research should focus on identifying the underlying causes for the low PCS for the dimensions ‘Emotional support and alleviation of fear and anxiety’ and ‘Involvement of significant others’, and how to improve these scores. Women’s thoughts on the underlying causes and on possible improvement projects could be explored by organising focus groups.
When comparing the targets for improvement with an earlier ENDOCARE evaluation (Dancet et al., 2012), three corresponding targets for improvement are found: (i) receiving practical information and advice on self-care after surgery; (ii) receiving information on pain medication; and (iii) personal follow-up by the treating physician. As it seems that all endometriosis care centres need to improve these care aspects, it would be interesting to use qualitative research techniques to identify how these low scores can be improved in endometriosis centres.
Nine care aspects were identified as a strength in one care centre and as a target for improvement in the other. Specifically for those care aspects, cross-centre learning could be used to improve patients-centredness of care as also addressed by Geukens et al. (2018). The Quality Impact Indices might help healthcare providers and quality coordinators to prioritise which targets for improvement need primary assessment and improvement. The feasibility of improving endometriosis care should also be considered.
A strength of our study is that only women with surgically proven endometriosis were included. A second strength is the use of the ECQ as an instrument to measure strengths and targets for improvement of patient-centredness of endometriosis care in both a secondary endometriosis care centre and a tertiary endometriosis care centre. The ECQ proved to be valid and reliable in evaluating endometriosis care on a clinic level (Dancet et al., 2011, 2012). The PCS was adjusted for all significantly different characteristics between the two care centres. However, if we would have been able to investigate more secondary care centres and compare these with more than one tertiary care centre, this would have allowed us to reach more firm conclusions on the differences between secondary and tertiary care centres. Furthermore, the retrospective nature of the study may introduce recall bias.
The patient characteristics in both care centres did not differ significantly among responders and non-responders. This implies that the responders in our study are representative for the entire patient population in both clinics. Another limitation is that some women selected two answer options on the Likert scale. We selected the most negative answer for analysis, which might alter the outcomes. A digital version of the ECQ might eliminate this problem as only one answer option can be selected on a digital form.
Since endometriosis is a chronic disease and care is very dynamic, it is possible that care would be valued differently at different stages in life (i.e. when pursuing pregnancy versus succeeding in conceiving). Consequently, it is important to keep investigating and optimising endometriosis care. Especially in chronic diseases, there should be extra attention to optimising quality of care and focussing on patient-centredness. The first step in improving patient-centredness and thereby quality of care is identifying targets for improvement.
Previous research found that feedback to healthcare providers on quality of care alone is ‘not a sufficient enough way in improving patient-centeredness’ (Huppelschoten et al., 2013). This research group found that having a greater input from patients results in better improvement of patient-centredness (Huppelschoten et al., 2015). These researchers state that healthcare providers should be stimulated to feel the desire to improve their care. Next to that, healthcare providers’ knowledge on their provision of care and their shortcomings could be improved (Huppelschoten et al., 2013). Further research should implement these ideas in improving endometriosis care and build a framework on improving quality of care in a practical and sustainable way.
The ECQ is a validated questionnaire. However, we would advise to adapt the background questions. First, the question on whether women’s endometriosis was surgically confirmed can be omitted if centres only question women with surgically confirmed endometriosis. Second, we would advise a question about whether women became pregnant after their endometriosis treatment as this could influence their assessment of the quality of not only their life but also their care.
Conclusion
This is the first study investigating patient-centredness using the ECQ aside from the validation studies. Different strengths and targets for improvement were identified. Patient-centredness was investigated in both a secondary care centre and a tertiary care centre for endometriosis care and no difference was demonstrated between these two centres except for the dimensions ‘physical comfort’ and ‘continuity and transition’. The two centres shared three strengths and nine targets for improvement.
The ECQ, with a few minor advised alterations to the background questions, appears to be a useful tool for investigating patient-centredness. In order to tailor improvements of care, future research should focus on finding specific patients characteristics that determine the outcome of the ECQ. Next to that, the ECQ could be used as a tool to follow-up quality of improvements of care.
Authors’ roles
The study was designed with W.N., C.L., V.M., L.H. and A.S. Knowledge on the usage of the ENDOCARE questionnaire was added by E.D. and S.A. Collection and analysis of data were performed by M.H. and A.S. Final analysis was performed with help from P.V. A.S. drafted and revised the manuscript. The manuscript was critically revised and approved by all authors.
Funding
No external funding was either sought or obtained for this study.
Conflict of interest
V.M. and C.B. report grants from Guerbet, grants from Merck and grants from Ferring outside the submitted work. All authors declare that they have no competing interests concerning this publication.
References
- Apers S, Dancet EAF, Aarts JWM, Kluivers KB, D’Hooghe TM, Nelen W.. The association between experiences with patient-centred care and health-related quality of life in women with endometriosis. Reprod Biomed Online 2018;36:197–205. [DOI] [PubMed] [Google Scholar]
- Chen LC, Hsu JW,, Huang KL, Bai YM, Su TP, Li CT, Yang AC, Chang WH, Chen TJ, Tsai SJ. et al. Risk of developing major depression and anxiety disorders among women with endometriosis: a longitudinal follow-up study. J Affect Disord 2016;190;282–285. [DOI] [PubMed] [Google Scholar]
- Dancet EA, Ameye L, Sermeus W, Welkenhuysen M, Nelen WL, Tully L, De Bie B, Veit J, Vedsted-Hansen H, Zondervan KT. et al. The ENDOCARE questionnaire (ECQ): a valid and reliable instrument to measure the patient-centeredness of endometriosis care in Europe. Hum Reprod 2011;26:2988–2999. [DOI] [PubMed] [Google Scholar]
- Dancet EA, Apers S, Kluivers KB, Kremer JA, Sermeus W, Devriendt C, Nelen WL, D’Hooghe TM.. The ENDOCARE questionnaire guides European endometriosis clinics to improve the patient-centeredness of their care. Hum Reprod 2012;27;3168–3178. [DOI] [PubMed] [Google Scholar]
- De Graaff AA, Van Lankveld J, Smits LJ, Van Beek JJ, Dunselman GA.. Dyspareunia and depressive symptoms are associated with impaired sexual functioning in women with endometriosis, whereas sexual functioning in their male partners is not affected. Hum Reprod 2016;31:2577–2586. [DOI] [PubMed] [Google Scholar]
- Dunselman GA, Vermeulen N, Becker C, Calhaz-Jorge C, D’Hooghe T, De Bie B, Heikinheimo O, Horne AW, Kiesel L, Nap A. et al. ESHRE guideline: management of women with endometriosis. Hum Reprod 2014;29:400–412. [DOI] [PubMed] [Google Scholar]
- Friedl F, Riedl D, Fessler S, Wildt L, Walter M, Richter R, Schussler G, Bottcher B.. Impact of endometriosis on quality of life, anxiety, and depression: an Austrian perspective. Arch Gynecol Obstet 2015;292:1393–1399. [DOI] [PubMed] [Google Scholar]
- Geukens EI, Apers S, Meuleman C, D’Hooghe TM, Dancet EAF.. Patient-centeredness and endometriosis: definition, measurement, and current status. Best Pract Res Clin Obstet Gynaecol 2018;50:11–17. [DOI] [PubMed] [Google Scholar]
- Giudice LC. Clinical practice. Endometriosis. N Engl J Med 2010;362:2389–2398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huppelschoten AG, Aarts JW, van Empel IW, Cohlen BJ, Kremer JA, Nelen WL.. Feedback to professionals on patient-centered fertility care is insufficient for improvement: a mixed-method study. Fertil Steril 2013;99:1419–1427. [DOI] [PubMed] [Google Scholar]
- Huppelschoten AG, Nelen W, Westert GP, van Golde RJ, Adang EM, Kremer JA. Improving patient-centredness in partnership with female patients: cluster RCT in fertility care. Hum Reprodu 2015;30;5:1137–1145. [DOI] [PubMed] [Google Scholar]
- Lukas I, Kohl-Schwartz A, Geraedts K, Rauchfuss M, Wolfler MM, Haberlin F, von Orelli S, Eberhard M, Imthurn B, Imesch P. et al. Satisfaction with medical support in women with endometriosis. PLoS One 2018;13:e0208023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marinho MCP, Magalhaes TF, Fernandes LFC, Augusto KL, Brilhante AVM, Bezerra L.. Quality of life in women with endometriosis: an integrative review. J Womens Health (Larchmt) 2018;27:399–408. [DOI] [PubMed] [Google Scholar]
- Practice Committee of the American Society for Reproductive Medicine. Endometriosis and infertility: a committee opinion. Fertil Steril 2012;98:591–598. [DOI] [PubMed] [Google Scholar]
- Practice Committee of the American Society for Reproductive Medicine. Treatment of pelvic pain associated with endometriosis: a committee opinion. Fertil Steril 2014;101;927–935. [DOI] [PubMed] [Google Scholar]
- Rowe HJ, Hammarberg K, Dwyer S, Camilleri R, Fisher JR.. Improving clinical care for women with endometriosis: qualitative analysis of women’s and health professionals’ views. J Psychosom Obstet Gynaecol 2019;1–7, doi: 10.1080/0167482X.2019.1678022. [DOI] [PubMed] [Google Scholar]
- Sepulcri Rde P, do Amaral VF.. Depressive symptoms, anxiety, and quality of life in women with pelvic endometriosis. Eur J Obstet Gynecol Reprod Biol 2009;142:53–56. [DOI] [PubMed] [Google Scholar]
- Slack N. The importance-performance matrix as a determinant of improvement priority. Int J Oper Prod Manage 1994;14:59–75. [Google Scholar]
- van Campen C, Sixma HJ, Kerssens JJ, Peters L, Rasker JJ.. Assessing patients’ priorities and perceptions of the quality of health care: the development of the QUOTE-rheumatic-patients instrument. Br J Rheumatol 1998;37:362–368. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Quality of Care: A Process for Making Strategic Choices in Health Systems Geneva, Switzerland: WHO Press, 2006.
- Wygant JN,, McGuire LJ, Bush NM, Burnett TL, Green IC, Breitkopf DM.. What makes a chronic pelvic pain patient satisfied? J Psychosom Obstet Gynaecol 2019;40:239–242. [DOI] [PubMed] [Google Scholar]