Abstract
While cognitive-behavioral therapy for hoarding disorder (HD) has resulted in significant reductions in symptoms, most individuals continue to have significant hoarding symptoms following treatment. This investigation sought to extend the literature on the behavioral treatments for hoarding by examining (1) group cognitive rehabilitation and exposure/sorting therapy (CREST) and (2) group exposure therapy (ET) for hoarding. Participants in both studies reported significant decreases in hoarding symptom severity from baseline to post-treatment on all primary outcome measures using mixed-effects linear regression models with the intent to treat sample. Participants who received group CREST reported statistically significant reductions in anxiety, depression, and overall severity at post-treatment, while participants who received group ET did not. Results provide preliminary evidence for both group CREST and group ET as effective treatments for hoarding disorder.
Keywords: Hoarding, Behavior therapy, Treatment
Introduction
Hoarding disorder (HD) is characterized by a persistent difficulty discarding possessions, combined with the perceived need to save items and distress associated with discarding them regardless of their actual value (American Psychiatric Association 2013). Those difficulties result in the accumulation of possessions that clutter living or work spaces such that activities for which those spaces were intended are precluded. A diagnosis of HD is given if the hoarding behavior or clutter leads to marked distress and/or impairment in functioning (American Psychiatric Association 2013). HD affects approximately 2–6% of the general population (Bulli et al. 2014; Iervolino et al. 2009). In the absence of effective treatment, HD follows a chronic, unremitting course (Ayers et al. 2010; Tolin et al. 2010) that significantly interferes with functioning and diminishes quality of life (Ayers et al. 2012; Saxena et al. 2011). HD is associated with considerable morbidity, including increased rates of comorbid psychopathology (e.g., anxiety and depression); functional interference across social, occupational, and family domains; co-occurring chronic medical conditions; and greater health risks (e.g., risks of falls, fire, poor nutrition; Diefenbach et al. 2013). Clearly, HD represents a significant public health concern that is costly to both the individual and society (Tolin et al. 2008).
Cognitive behavioral therapy (CBT) is the most well-studied psychosocial intervention for HD. Based on the cognitive behavioral model of HD (Frost and Hard 1996), CBT is comprised of intervention strategies intended to target hypothesized core maintaining factors, including (1) motivational interviewing to facilitate motivation to change and enhance treatment adherence; (2) graded exposure to discarding possessions as well as non-acquiring through building tolerance to resist urges to acquire new items; (3) cognitive restructuring of distorted or unhelpful thinking patterns and beliefs; and (4) training in developing and maintaining an organizational system to reduce clutter in the home (Steketee and Frost 2014). A recent meta-analysis of 12 HD samples found that CBT resulted in statistically significant and large reductions in HD symptom severity (average Hedges’ g = 0.82; Tolin et al. 2015). However, changes in functional impairment were only moderate (Hedges’ g = 0.52), and rates of clinically significant change ranged from 24 to 43%. Thus, although CBT results in significant improvements in symptoms and functional impairment, most individuals continue to display symptom profiles following treatment that are closer to the HD clinical range compared to the normative range.
Cognitive rehabilitation and exposure/sorting therapy (CREST; Ayers et al. 2014, 2017) was developed in response to research demonstrating that neurocognitive impairments are common in adults with HD (Woody et al. 2014). CREST integrates Compensatory Cognitive Training (CCT; Twamley et al. 2012, 2015, 2017) to ameliorate executive functioning deficits characteristic of HD with graded exposure to discarding possessions and resisting urges to acquire. Exposure therapy for hoarding disorder involves exposing the patient to the distress of possibly discarding an item they may later want. Thus, patients are exposed to the sense of uncertainty they experience when deciding whether or not to discard a possession.
The CCT strategies utilized in CREST are designed to help individuals with HD improve prospective memory (i.e., remembering to-do things in the future by planning and setting priorities), problem solving skills (e.g., making decisions, creating steps, and finding solutions), and cognitive flexibility (e.g., finding alternative solutions). Two studies provided initial evidence for the efficacy of CREST delivered via individual sessions (Ayers et al. 2014, 2017). An open trial found that older adults with HD who completed CREST experienced significant and large improvements in hoarding severity from pre- to post-treatment (Ayers et al. 2014). A randomized controlled trial of 58 older adults diagnosed with HD revealed that CREST resulted in significantly greater improvement on measures of hoarding severity, activities of daily living, and general anxiety compared to geriatric case management (CM; Ayers et al. 2017). Similar treatment effects were observed on measures of clutter volume and depression; however, between group comparisons were not statistically significant. Treatment gains were maintained at the 6-month follow-up assessment. Thus, CREST appears to be a promising new treatment approach for HD.
The present investigation sought to extend prior literature on the treatment of hoarding by conducting two different studies about group treatment for hoarding disorder. First, the efficacy of CREST to date has been evaluated using individual treatment sessions only. Establishing the efficacy of CREST administered within a group treatment format would be potentially valuable as a way to reduce therapist burden and cost. A recent meta-analysis of CBT for HD found that group versus individual administered CBT did not differ in terms of treatment response (Tolin et al. 2015). However, incorporating additional strategies targeting executing functioning deficits may prove difficult in a group format, thereby diminishing treatment effects or resulting in higher attrition. Thus, the aim of Study 1 was to examine treatment response following CREST administered to individuals with HD within a group context. We hypothesized that CREST administered in a group format would result in significant and large reductions in hoarding symptoms from pre- to post-treatment, and that symptom improvement would be maintained through a 6-month follow-up assessment period.
Second, the efficacy of exposure therapy (ET) alone for HD has yet to be established. Initial qualitative evidence suggests that the exposure component of CBT is perceived by patients as being most effective (Ayers et al. 2012). Moreover, establishing the efficacy of a distilled form of behavioral treatment may be valuable in terms of facilitating dissemination efforts (Cougle 2012). Thus, the aim of Study 2, conducted concurrently with Study 1, was to evaluate the effects of an exposure-focused group-based intervention for HD intended to help patients manage the distress associated with discarding possessions and resisting urges to acquire new items. We hypothesized that exposure therapy administered in a group format would result in significant and large reductions in hoarding symptoms from pre- to post-treatment, and that symptom improvement would be maintained through a 6-month follow-up assessment period. Finally, we benchmarked the magnitude of treatment effects and response rates from both studies against existing hoarding treatment efficacy findings (Ayers et al. 2017; Tolin et al. 2015).
Materials and Methods
The study was approved by the institutional review boards of the University of California, San Diego and the VA San Diego Healthcare System. No monetary compensation was provided for participation, and informed consent was obtained from all individual participants included in the study. Details of the recruitment methods have been previously published (Ayers et al. 2015).
Participants
Participants were recruited from March 2013 to May 2014 from the San Diego community. Participants were included if they were 18 years of age or older, could speak and read English, were able to participate in face-to-face group psychotherapy, met the DSM-5 criteria for a primary diagnosis of HD as determined by clinical interview, and scored ≥ 20 on the UCLA Hoarding Severity Scale (UHSS; Saxena et al. 2015) and ≥ 40 on the Savings Inventory-Revised (SI-Frost et al. 2004). Final HD diagnosis was determined by a consensus conference including at least two therapists with expertise in hoarding, supervised by a licensed clinical psychologist (C.R.A.).
Participants were excluded if they met diagnostic criteria for current substance abuse, history of psychosis, and active suicidal ideation as determined by the Mini International Neuropsychiatric Interview (M.I.N.I.; Sheehan et al. 1998), screened positive for dementia by scoring less than 21 on the Montreal Cognitive Assessment (MoCA; Nasreddine et al. 2005), if they were currently engaged in other forms of psychotherapy, or if their hoarding symptoms were due to a secondary condition [e.g., obsessive–compulsive disorder (OCD), traumatic brain injury], as per DSM-5 criteria.
Assessments
The assessment battery was administered at baseline, 3 months (mid-treatment), and 6 months (post-treatment) in person and at, 9, and 12 months over the phone. Baseline, mid-treatment, and post-treatment assessments were conducted by Master’s level clinical psychology graduate students who received 15 h of training. Raters were not blind to study condition. Phone assessments were conducted by research assistants with at least 20 h of assessment training.
The primary outcome measures were the saving inventory revised (SI-Frost et al. 2004) and the clutter image rating (CIR; Frost et al. 2008; Dozier et al. 2016). Secondary outcome measures included the Hospital Anxiety and Depression Scale (HADS; Zigmond and Snaith 1983), the Activities of Daily Living in Hoarding Scale (ADL-H; Frost et al. 2013), and the Clinical global improvement (CGI; Guy 1976) Severity and Improvement scales. Higher scores represent more severe symptoms for all measures. The CIR, HADS, and CGI were administered at baseline and post-treatment (6 months) assessments only.
The SI-R is a 23-item self-report Likert scale of excessive acquisition, difficulty discarding, and clutter. Items are summed for a total score ranging from 0 to 92; scores over 40 are indicative of clinically severe hoarding symptoms (Frost et al. 2004). The SI-R has been validated for use in older adults (Ayers et al. 2016) and demonstrated adequate reliability in the current combined sample (α= 0.90).
The CIR is a three-item graphic measure of clutter level in the bedroom, kitchen, and living room. Participants identify which picture most resembles the level of clutter in their home. Pictures are numbered 1–9, ranging from no clutter to severe clutter. Reliability of the CIR in the current combined sample was adequate (α = 0.78).
The HADS is a 14-item self-report measure which includes anxiety (7 items) and depression (7 items) subscales. Scores greater than 10 on either subscale indicate a likely case of anxiety or depression. There was adequate reliability in the current combined sample for both the anxiety subscale (α = 0.81) and the depression subscale (α = 0.86).
The ADL-H is a 15-item self-report assessment of impairment from hoarding behaviors. Items are rated from 1 (“can do easily”) to 5 (“unable to do”), or (“not applicable”). Items are averaged to create a mean score. The ADL-H has been found to discriminate between hoarding and non-hoarding samples (Frost et al. 2013) and demonstrated good reliability in the current combined sample (α = 0.93).
The CGI Severity scale is 7-point clinician rating ranging from 1 (“normal”) to 7 (“extremely ill”). The CGI Improvement scale is a clinician rating of treatment response ranging from 1(“very much improved”) to 7 (“very much worse”).
Enrollment and Group Assignment
Study patient flow is depicted in Fig. 1. Eighty of the 155 individuals (52%) who called to express interest were consented and assessed for eligibility, of which 60 (75%) were enrolled. Participants meeting enrollment criteria were assigned to each treatment study based on clinician availability, with 25 participants assigned to Study 1 (CREST) and 35 participants assigned to Study 2 (ET). Participants did not have a choice in study assignment. Four groups were run for each study. The CREST study had group sizes of 6, 5, 8, and 6. The ET study had group sizes of 6, 6, 10, and 13.
Fig. 1.
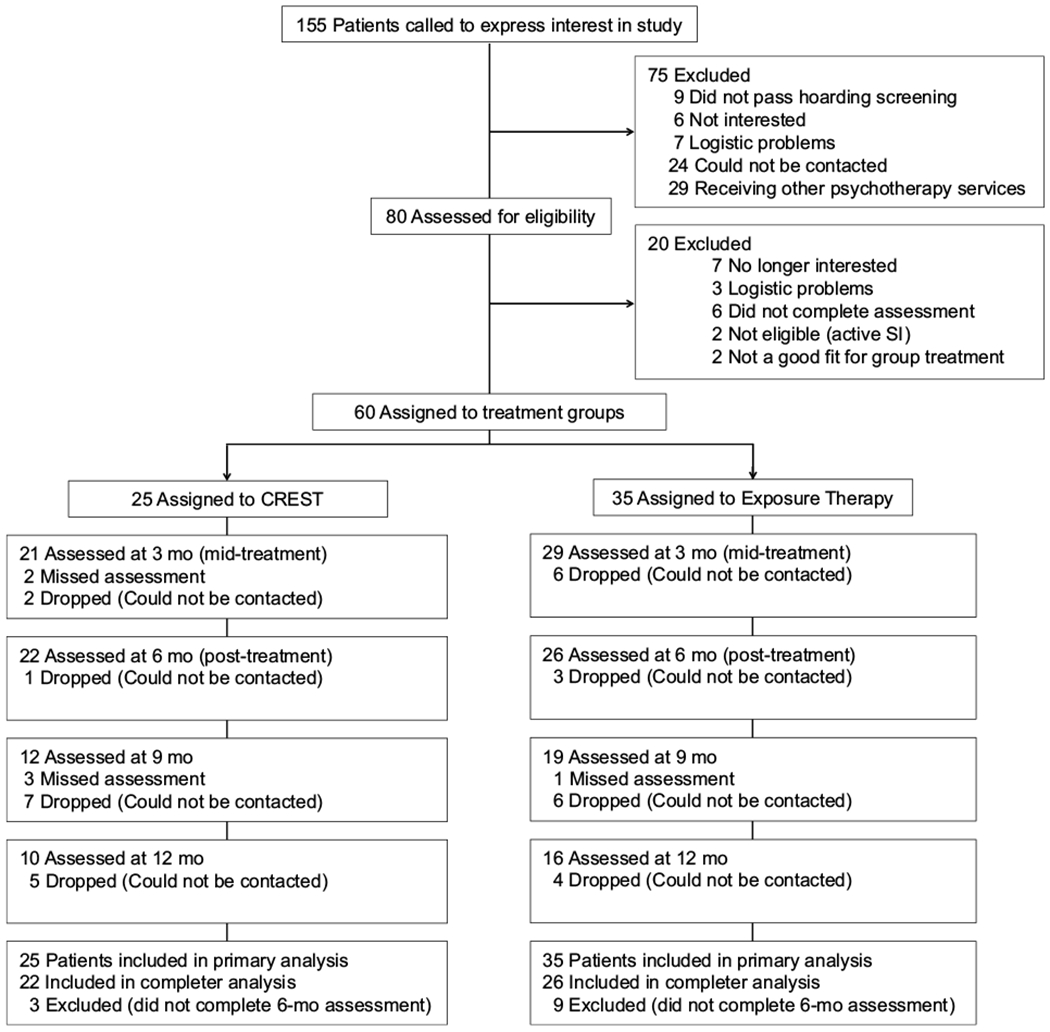
Flow of participants through each phase of the study
Interventions
The treatment for both studies was conducted by advanced doctoral students in clinical psychology. Therapists were trained in both CREST and ET. The training for ET explicitly addressed the importance of not discussing the CCT skills during sessions. Weekly 1 h supervision of the therapists was provided by a licensed clinical psychologist with experience in the treatment of hoarding disorder. Videotapes were reviewed in supervision as needed. Treatment cross-contamination issues were addressed in supervision as needed. Each group therapy session consisted of two graduate students and at least one undergraduate research assistant.
All participants received a therapy manual (of either the CREST or ET protocol) to use throughout the course of treatment. Both treatment protocols included daily homework exercises to be completed in the therapy manuals. Each group session began with a brief discussion of homework completion. The CREST protocol was composed of seven sessions of CCT and 19 sessions of exposure. The CCT skills in the CREST protocol were geared towards prospective memory (calendar use, linking tasks, automatic places, using a “to-do” list), cognitive flexibility (brain storming), and problem solving (6-step problem solving method, planning). Participants in the CREST groups were provided with a pocket calendar and encouraged to use the calendar to prioritize and plan out future activities, including daily sorting sessions at home. Prioritization was taught by encouraging participants to separate their to-do lists into “nice to-do” and “need to-do.” Participants who stated they had difficulty finding time for daily sorting were encouraged to examine their to-do lists and re-evaluate if they could schedule fewer “nice to-do” activities each day in order to make more time for sorting. During the brain-storming module, participants were encouraged to generate 15 different ways to “get rid of items.” Problem solving was taught using the DBEST acronym (Define the problem; Brainstorm solutions; Evaluate each solution; Select a solution to try; Try the solution; Evaluate the solution). If a participant identified a barrier to treatment, he or she was encouraged to use the DBEST problem solving method to overcome the obstacle. Finally, participants were taught how to plan out larger to-do activities (e.g., reducing clutter in the kitchen such that the stove can be used) by breaking the goal or project down into smaller steps to be accomplished over time. The CCT skills were reviewed as needed during the exposure sessions to facilitate participants using the skills to overcome any treatment barriers.
The ET protocol was composed of 26 sessions of exposure only. The in-session exposures were designed to expose participants to the distress of making decisions about their items (i.e., whether or not to keep or discard each item). During the exposure sessions, participants developed discarding hierarchies for their homes based on their anticipated levels of distress for sorting different rooms (e.g., living room versus kitchen versus bedroom). Participants were instructed to bring in boxes of unsorted items from areas of mild to moderate distress. Instructions for sorting (e.g., take items from the top of the box, only handle an item once) were discussed and posted during the group exposure sessions. Participants were asked to record their subjective level of distress every 5 min during the group sorting exposures. Clinicians and undergraduate research assistants worked with participants individually during the group sorting exercises as needed. Participants were asked to sort daily and record the length of time they sorted and to record their subjective levels of distress every 5 min on a record sheet included in their treatment manual. Clinicians reviewed the record sheets during check-in.
To address possible excessive acquisition of items, participants were asked to track all incoming items (whether purchased or free) for the first 2 weeks of the exposure treatment. Tracking sheets were reviewed and discussed with clinicians during the check-in portion of the sessions. If acquiring was identified as excessive, participants developed acquiring hierarchies based on their anticipated levels of distress for not acquiring items from frequently-visited places or stores (e.g., thrift store versus grocery store). Acquisition exposures (e.g., going to a thrift store, shopping and placing desired items in a cart, then put the items back and leave the store without purchasing any items) were then assigned as homework. Participants were asked to record their subjective level of distress during acquiring exposures on a worksheet included in their treatment manual. The worksheet was then reviewed by clinicians the following session during check-in.
Four of the 26 sessions for both study protocols took place in each participant’s home. The home visit sessions took place towards the end of each treatment protocol. The post-treatment assessments were scheduled following the completion of the 26 group sessions.
Data Analysis
Both studies were both analyzed in the following manner. All analyses were performed using Stata version 13.0 (StataCorp 2013). Linear mixed models with random intercepts were used to evaluate the change in outcome variables over time, both for the treatment phase (0–6 months) and follow-up phase (6–12 months). Due to the large attrition between post-treatment assessment and the follow-up assessments, the follow-up analyses are presented for only participants who completed at least one follow-up assessment. The demographic and baseline characteristics of the full and follow-up samples were compared using ×2 analyses and Welch’s t tests to account for any unequal variance.
All longitudinal analyses (0–6 months) were conducted on an intent-to-treat (ITT) basis and then among completers only. The ITT analyses were conducted using the data from all enrolled participants. Treatment response was defined as achieving sub-clinical levels of hoarding severity (< 41 total score on the SI-R or < 4 mean score on the CIR) or a score of 2 (much improved) or 1 (very much improved) on the CGI Improvement scale. Participants without information at post-treatment were categorized as non-responders. Within-group effect size was calculated as Cohen’s d using the mean difference in baseline and post-treatment scores for the completer sample for all outcome measures.
Because a substantial minority of the participants in both studies had previously engaged in psychotherapy for hoarding disorder, ×2 analyses were used to determine if previous individual psychotherapy affected treatment response.
Results
Study 1: Group CREST
Baseline participant characteristics (n = 25) are presented in Table 1. The majority of participants were women (72%) and Caucasian (76%). The average age was 55 and average education was 15 years. Forty percent of participants met DSM-IV-TR criteria for an anxiety disorder (excluding OCD) and 68% of participants met DSM-IV-TR criteria for a mood disorder (see Table 1). Twenty-four percent of participants met DSM-IV-TR criteria for OCD. Eighty-eight percent of participants completed post-treatment assessment at 6 months. Forty percent of participants were retained through the 12-month follow-up assessment.
Table 1.
Baseline participant characteristics
| Study 1: CREST (n = 25) | Study 2: ET (n = 35) | |
|---|---|---|
| Age, mean (SD) | 55.48 (2.22) | 61.06 (1.47) |
| Education, mean (SD) | 15.24 (0.47) | 15.58 (0.36) |
| Women, n (%) | 18 (72.00) | 26 (74.29) |
| Race, n (%) | ||
| White | 19 (76.00) | 28 (80.00) |
| Black | 0 | 2 (5.71) |
| Asian | 2 (8.00) | 2 (5.71) |
| Hispanic | 2 (8.00) | 1 (2.86) |
| Biracial | 2 (8.00) | 1 (2.86) |
| Other | 0 | 1 (2.86) |
| Marital status, n (%) | ||
| Never married | 9 (36.00) | 10 (29.41) |
| Married or living with someone | 6 (24.00) | 8 (23.53) |
| Separated/divorced | 9 (36.00) | 13 (38.24) |
| Widowed | 0 | 2 (58.82) |
| Employment status, n (%) | ||
| Retired | 5 (20.00) | 12 (35.29) |
| Employed full- or part-time | 11 (44.00) | 15 (44.12) |
| Unemployed | 9 (36.00) | 7 (20.59) |
| Baseline assessment scores, mean (SD) | ||
| SI-R | 58.84 (12.33) | 57.24 (12.75) |
| CIR | 4.04 (1.65) | 4.11 (1.49) |
| ADL-H | 29.00 (2.97) | 31.17 (2.03) |
| HADS anxiety | 9.76 (1.03) | 9.56 (0.77) |
| HADS depression | 8.28 (1.05) | 7.97 (0.82) |
| CGI severity | 3.76 (0.23) | 3.73 (0.21) |
| Presence of comorbid diagnosis, n (%) | ||
| Obsessive–compulsive disorder (OCD) | 6 (24.00) | 5 (14.29) |
| Any anxiety disorder (non-OCD) | 10 (40.00) | 11 (31.43) |
| Any mood disorder | 17 (68.00) | 20 (57.14) |
| Taking psychotropic medications, n (%) | 15 (60.00) | 13 (37.14) |
| No. of medical conditions | 2.25 (0.47) | 2.69 (0.34) |
ADL-H activities of daily living-hoarding, CGI clinical global impressions, CIR clutter image rating, CREST cognitive rehabilitation and exposure/sorting therapy, ET exposure therapy, HADS Hospital Anxiety and Depression Scale, SI-R savings inventory-revised
Baseline Through Post-Treatment Assessment
Mean observed scores at baseline, mid-treatment (3 months), and post-treatment (6 months) are presented in Table 2. Participants reported significant decreases in symptom severity from baseline to post-treatment on all primary and secondary outcome measures [time effect (Table 2)], using mixed-effects linear regression models with the ITT sample (Figs. 2, 3). The completer sample demonstrated a similar pattern of results.
Table 2.
Observed mean (SD) scores on baseline to post-treatment outcome measures across treatment for 25 adults receiving cognitive rehabilitation and exposure/sorting therapy (CREST) for hoarding disorder
| Assessment | Active treatment (0–6 months) |
||||||
|---|---|---|---|---|---|---|---|
| Time Point |
Average % changea | d (95% CI) a | Time effect |
||||
| Baseline (n = 25) | 3 months (n = 21) | 6 months (n = 22) | β (SE) | p | |||
| SI-R | 58.84 (12.33) | 55.55 (10.59) | 45.14 (16.48) | − 21.18 | 0.84 (0.22–1.45) | − 12.55 (2.57) | < .001 |
| CIR | 4.04 (1.65) | – | 2.97 (1.82) | − 24.04 | 0.53 (−.07–1.13) | − 0.96 (0.19) | < .001 |
| ADL-H | 29.00 (12.94) | 24.72 (6.25) | 24.65 (11.50) | − 16.75 | 0.40 (− .24–1.05) | − 3.35 (1.10) | .002 |
| HADS anxiety | 9.76 (5.13) | – | 8.00 (4.72) | − 19.27 | 0.38 (− .22–.98) | − 1.87 (0.76) | .014 |
| HADS Depression | 8.28 (5.26) | – | 6.14 (4.53) | − 25.76 | 0.45 (− .15–1.05) | − 2.14 (0.56) | < .001 |
| CGI severity | 3.76 (1.13) | – | 2.94 (1.21) | − 21.18 | 0.66 (0.02–1.30) | − 0.93 (0.23) | < .001 |
ADL-H activities of daily living-hoarding, CGI clinical global impressions, CIR clutter image rating, HADS Hospital Anxiety and Depression Scale, SI-R savings inventory-revised
Analyses were mixed-effects linear regression models using the ITT sample
Calculated using completer sample (n = 22). Positive effect sizes indicate symptom improvement
Fig. 2.
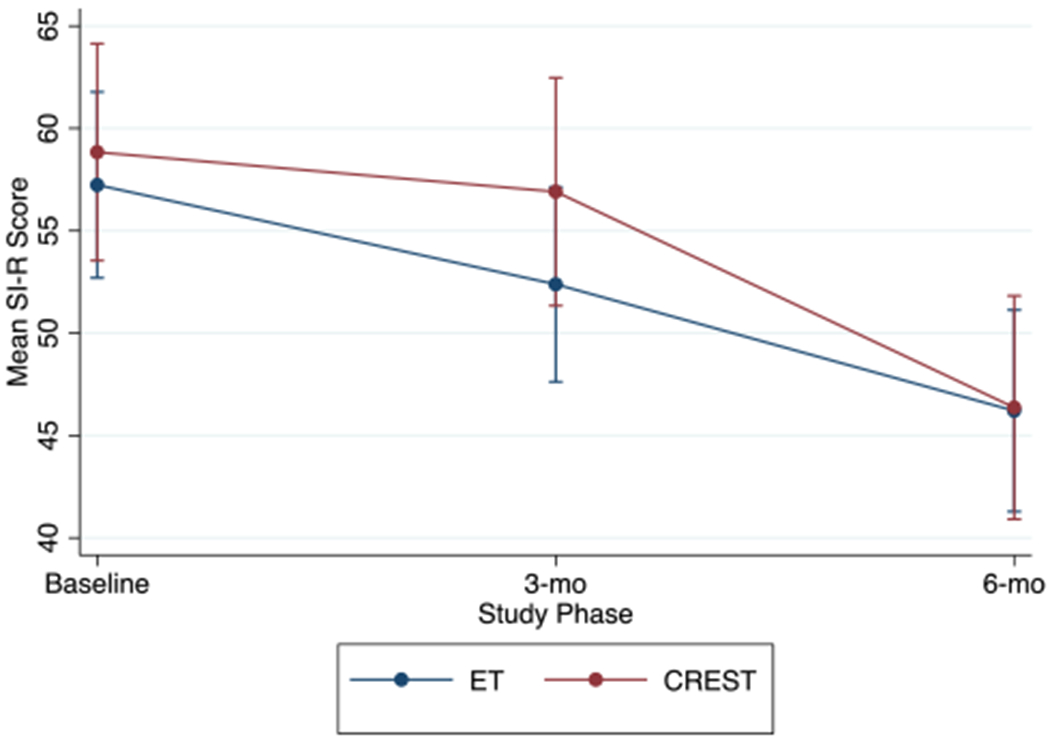
Hoarding symptom severity across active treatment on savings inventory-revised (SI-R) for participants receiving group cognitive rehabilitation and exposure/sorting therapy (CREST) (n = 25) or Exposure Therapy (ET) (n = 35) for hoarding disorder. aData are predicted values based on mixed models with standard error bars
Fig. 3.

Hoarding symptom severity across active treatment on Activities of Daily Living-Hoarding (ADL-H) for participants receiving group cognitive rehabilitation and exposure/sorting therapy (CREST) (n = 25) or exposure therapy (ET) (n = 35) for hoarding disorder. aData are predicted values based on mixed models with standard error bars
There was a large effect size for the completer sample change score between baseline and post-treatment assessment on the SI-R Total [d = 0.84, (95% CI 0.22–1.45)], a medium effect size on the CIR [d = 0.53, (95% CI − 0.07–1.13)], and a small-to-medium effect size on the ADL-H [d = 0.40, (95% CI − 0.24–1.05)]. Thirty-two percent of participants were classified as treatment responders on the SI-R; 68% were classified as treatment responders on the CIR; and 44% were classified as treatment responders on the CGI Improvement scale.
Follow-up Sample Analyses
There were no significant differences between participants who did and did not complete at least one follow-up assessment on any of the assessed demographic variables, including age, [t (24.13) = 0.12, p = .45] years of education [t (21.40) = 0.44, p = .33], gender [×2 (1) = 3.48, p = .06], race [% Caucasian, ×2 (1) = 0.36, p = .55], marital status [% married, ×2 (1) = 2.39, p = .12], and employment status [% employed, ×2 (1) = .02, p = .90]. There were also no differences between participants who did and did not complete at least one follow-up assessment on the percent with comorbid OCD [×2 (1) = 0.36, p = .5], anxiety disorder [×2 (1) = 1.73, p = .19] or mood disorder (×2 (1) = 0.20, p = .65], the percent taking psychotropic medication(s) (×2 (1) = 0.24, p = .62)]], or the number of medical conditions [t (15.70) = 0.74, p = .23].
There were no differences in baseline severity scores between participants who did and did not complete at least one follow-up assessment on the SI-R Total [t (24.41) = 0.74, p = .23)], the CIR [t (23.98) = 0.22, p = .42], ADL-H [t (7.05) = 0.21, p = .42], HADS Anxiety [t (19.77) = 0.88, p = .19], HADS Depression [t (21.24) = 0.44, p = .33)] and the CGI severity [t (22.89) = 0.12, p = .45].
Mean observed scores at baseline, mid-treatment (3 months), post-treatment (6 months), and follow-up assessments (9 and 12 months) for the follow-up sample (n = 14) are presented in Table 3. Participants in the follow-up sample reported significant decreases in symptom severity from baseline to post-treatment on all primary and secondary outcome measures, with the exception of the HADS Anxiety scale, using mixed-effects linear regression models with the follow-up sample [time effect (Table 3)].
Table 3.
Observed mean (SD) scores on outcomes measures across time for the follow-up sample only (n = 14) for a study of group cognitive rehabilitation and exposure/sorting therapy (CREST) for hoarding disorder
| Assessment | Active treatment (0–6 months) |
Follow-up (6–12 months)a |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Time point |
Average % change | d (95% CI) | Time effect |
Time point |
Time effect |
||||||
| Baseline (n = 14) | 3 months (n = 13) | 6 months (n = 14) | β (SE) | p | 9 months (n = 12) | 12 months (n = 10) | β (SE) | p | |||
| SI-R | 57.21 (12.89) | 56.67 (11.69) | 44.64 (15.05) | − 21.97 | 0.90 (0.10–1.67) | − 12.57 (3.30) | < .001 | 40.25 (24.55) | 50.40 (21.43) | 2.76 (4.06) | .493 |
| CIR | 3.98 (1.71) | – | 2.93 (1.77) | − 26.38 | 0.60 (− .16–1.35) | − 1.05 (0.21) | < .001 | – | |||
| ADL-H | 29.54 (10.33) | 25.08 (6.57) | 24.15 (7.74) | − 18.25 | 0.59 (− .20–1.37) | − 4.35 (1.51) | .004 | 23.20 (8.38) | 25.25 (7.46) | − .07 (1.84) | .970 |
| HADS Anxiety | 8.93 (4.48) | – | 7.86 (4.55) | − 11.98 | 0.24 (− .51–.98) | − 1.07 (0.91) | .240 | – | |||
| HADS Depression | 7.86 (4.91) | – | 6.00 (4.77) | − 23.66 | 0.38 (− .37–1.13) | − 1.86 (0.67) | .006 | – | |||
| CGI Severity | 3.79 (1.12) | – | 2.75 (1.14) | − 27.44 | 0.92 (0.10–1.72) | − 1.10 (0.31) | < .001 | – | |||
Analyses were mixed-effects linear regression models using the ITT sample This sample was comprised of participants who completed at least one follow-up assessment
ADL-H activities of daily living-hoarding, CGI clinical global impressions, CIR clutter image rating, HADS Hospital Anxiety and Depression Scale, SI-R savings inventory-revised
These analyses assessed the change from the post-treatment assessment (at 6 months from baseline) through the follow up assessments (at 9 and 12 months from baseline)
There was a large effect size for the follow-up sample change score between baseline and post-treatment assessment on the SI-R Total [d = 0.90, (95% CI 0.10–1.67)] and a medium effect size on the CIR [d = 0.60, (95% CI − 0.16–1.35)] and on the ADL-H [d = 0.59, (95% CI − 0.20–1.37)]. Thirty-six percent of participants who completed at least one follow-up assessment were classified as treatment responders on the SI-R; 79% were classified as treatment responders on the CIR; and 57% were classified as treatment responders on the CGI Improvement scale. There was no significant difference between the participants who did and who did not complete at least one follow-up assessment on the percentage of the sample classified as treatment responders [SI-R: ×2(1) = 0.20, p = .65; CIR: ×2 (1) = 1.63, p = .20; CGI Improvement: ×2 (1) = 2.23, p = .14]
Mixed-effects linear regression models with the follow-up sample indicated no symptom change from post-treatment assessment through 12-month follow-up assessment on the two measures administered at follow-up, the SI-R (β = 2.76, p = .493]; Fig. 4) and the ADL-H (β = − 0.07, p = .970; Fig. 5). Paired t tests suggested that the changes from 9- to 12-month follow-up were non-significant for both the SI-R [t (6) = 1.62, p = .08] and the ADL-H [t (5) = 0.67, p = .27)
Fig. 4.
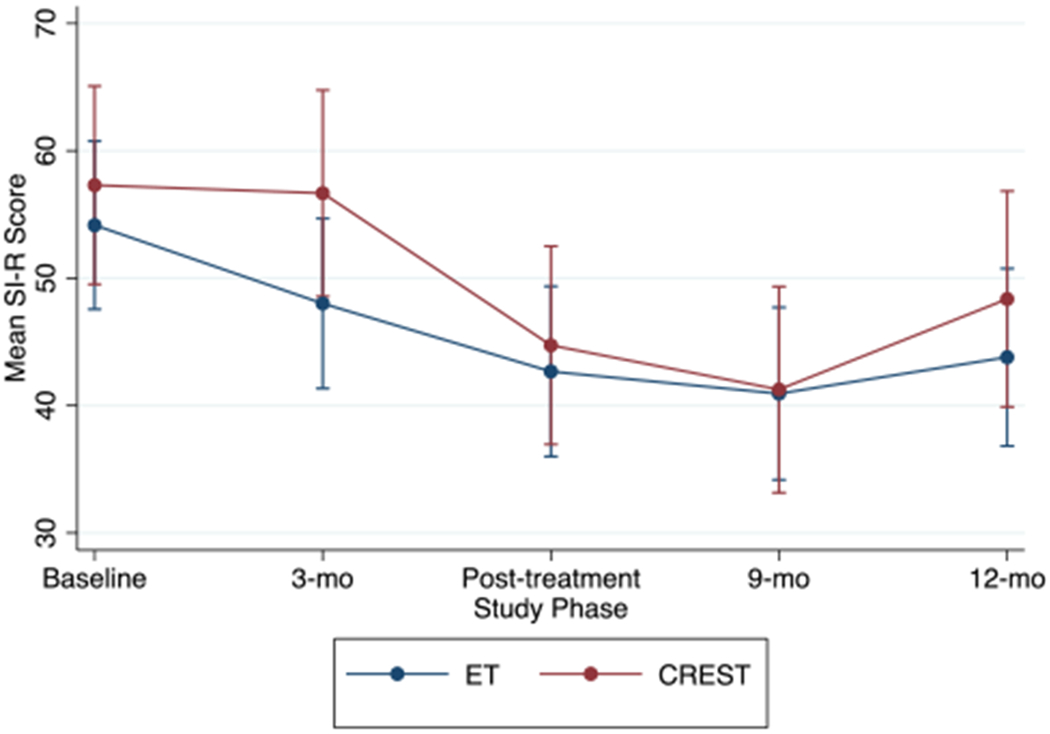
Hoarding symptom severity across active treatment on savings inventory-revised (SI-R) for participants who completed at least one follow-up assessment after receiving group cognitive rehabilitation and exposure/sorting therapy (CREST) (n = 14) or Exposure Therapy (ET) (n = 20) for hoarding disorder. aData are predicted values based on mixed models with standard error bars
Fig. 5.

Hoarding symptom severity on activities of daily living-hoarding (ADL-H) for participants who completed at least one follow-up assessment after receiving group cognitive rehabilitation and exposure/sorting therapy (CREST) (n = 14) or exposure therapy (ET) (n = 20) for hoarding disorder. aData are predicted values based on mixed models with standard error bars
Study 2: Group Exposure Therapy
Baseline participant characteristics (n = 35) are presented in Table 1. Similar to Study 1, the majority of participants were women (74%) and Caucasian (80%). The average participant was 61 years old and had 16 years of education. Thirty-one percent of participants met DSM-IV-TR criteria for an anxiety disorder (excluding OCD) and 57% of participants met DSM-IV-TR criteria for a mood disorder (see Table 1). Fourteen percent of participants met DSM-IV-TR criteria for OCD. Seventy-four percent of participants completed post-treatment assessment at 6 months. Forty-six percent of participants were retained through the 12-month follow-up assessment.
Baseline Through Post-Treatment Assessment
Mean observed scores at baseline, mid-treatment (3 months), post-treatment (6 months), and follow-up assessments (9 and 12 months) are presented in Table 4. Participants reported significant decreases in symptom severity from baseline to post-treatment on the SI-R, CIR, and ADL-H [time effect (Table 4)], using mixed-effects linear regression models with the ITT sample (Figs. 2, 3); however, there was no significant decrease in symptoms on the HADS Anxiety and Depression scales or on the CGI Severity scale (all p > 0.05). The completer sample demonstrated a similar pattern of results.
Table 4.
Observed mean (SD) scores on outcome measures across treatment for 35 adults receiving exposure therapy (ET) for hoarding disorder
| Assessment | Active treatment (0–6 months) |
||||||
|---|---|---|---|---|---|---|---|
| Time point |
Average % change | d (95% CI)a | Time effect |
||||
| Baseline (n = 35) | 3 months (n = 29) | 6 months (n = 26) | β (SE) | p | |||
| SI-R | 57.24 (12.75) | 52.18 (14.30) | 45.67 (14.41) | − 18.78 | 0.82 (0.24–1.40) | − 10.91 (1.64) | < 0.001 |
| CIR | 4.11 (1.49) | – | 3.11 (1.52) | − 18.80 | 0.48 (− .08–1.03) | − 0.80 (0.18) | < 0.001 |
| ADL-H | 31.17 (11.10) | 28.16 (9.60) | 25.40 (7.08) | − 14.13 | 0.46 (− .14–1.06) | − 4.51 (1.03) | < 0.001 |
| HADS Anxiety | 9.56 (4.37) | – | 8.92 (4.37) | − 2.94 | 0.06 (− .49–.62) | − 0.61 (0.77) | 0.431 |
| HADS Depression | 7.97 (4.65) | – | 6.38 (3.92) | − 11.27 | 0.21 (− .35–.76) | − 1.10 (0.59) | 0.062 |
| CGI Severity | 3.73 (1.18) | – | 3.8 (0.96) | 0.26 | 0.01 (− .54–.56) | 0.06 (0.21) | 0.788 |
Analyses were mixed-effects linear regression models using the ITT sample
ADL-H activities of daily living-hoarding, CGI clinical global impressions, CIR clutter image rating, HADS Hospital Anxiety and Depression Scale, SI-R savings inventory-revised
Calculated using completer sample (n = 26). Positive effect sizes indicate symptom improvement
There was a large effect size for the completer sample change score between baseline and post-treatment assessment on the SI-R Total [d = 0.82, (95% CI 0.24–1.40)] a medium effect size on the CIR [d = 0.48, (95% CI − 0.08–1.03)], and a small-to-medium effect size on the ADL-H [d = 0.46, (95% CI − .14–1.06)]. Twenty-six percent of participants were classified as treatment responders on the SI-R; 51% were classified as treatment responders on the CIR; and 34% were classified as treatment responders on the CGI improvement scale.
Post-hoc analyses were run to determine if the larger size of two of the ET groups impacted treatment outcomes. There was no significant difference in the number of sessions attended between the two smaller ET groups and the two larger ET groups (mean number of sessions 19.36 vs. 15.87; t (32) = 1.58, p = .06]. Furthermore, participants in the larger ET groups were not any more likely to be classified as treatment responders on any of the treatment outcome measures than were participants in the smaller ET groups, including the SI-R [×2 (1) = 0.78, p = .38)], the CIR [×2 (1) = 0.70, p = .40], and the CGI [×2(1) = 0.01, p = .93]
Follow-up Sample Analyses
There were no significant differences between participants who did and did not complete at least one follow-up assessment on any of the assessed demographic variables, including age [t (27.21) = 1.13, p = .13] years of education [t (26.84) = 1.49, p = .07], gender [×2 (1) = 0.01, p = .91], race [% Caucasian, ×2 (1) = 2.92, p = .09]], marital status [% married, ×2 (1) = 0.06, p = .81], and employment status [% employed, ×2 (1) = .02, p = .90]. There were also no differences between participants who did and did not complete at least one follow-up assessment on the percent with comorbid OCD [×2 (1) = 0.70, p = .40], anxiety disorder [×2 (1) = .89, p = .34]or mood disorder [×2 (1) = 2.81, p = .09], the percent taking psychotropic medication(s) [×2 (1) = 2.95, p = .09], or the number of medical conditions [t (23.56) = 0.35, p = .37] Although there were no statistically significant differences in baseline severity scores between participants who did and did not complete at least one follow-up assessment on the SI-R Total [t (24.89) = 1.66, p = .05]] and the CGI Severity [t (23.64) = 1.65, p = .06], participants who did not complete at least one follow-up assessment reported significantly higher clutter levels at baseline on the CIR [t (26.93) = 2.44, p = .01), significantly higher levels of impairment on the ADL-H [t (19.10) = 1.95, p = .03], and significantly higher levels of psychiatric symptoms on the HADS Anxiety [t (31.83) = 1.73, p = .047) and HADS Depression scales [t (24.44) = 1.90, p = .03].
Mean observed scores at baseline, mid-treatment (3 months), post-treatment (6 months), and follow-up assessments (9 and 12 months) are presented in Table 5 for the follow-up sample (n = 20). Participants in the follow-up sample reported significant decreases in symptom severity from baseline to post-treatment on the SI-R, CIR, and ADL-H using mixed-effects linear regression models with the follow-up sample [time effect (Table 5]. There was no significant decrease in symptoms on the HADS Anxiety and Depression Scales or on the CGI Severity Scale (all ps > 0.05].
Table 5.
Observed mean (SD) scores on outcomes measures for the follow-up sample only (n = 20) for a study of group exposure therapy (ET) for hoarding disorder
| Assessment | Active treatment (0–6 months) |
Follow-up (6–12 months)a |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Time point |
Average % change | d (95% CI) | Time effect |
Time point |
Time effect |
||||||
| Baseline (n = 20) | 3 months (n = 20) | 6 months (n = 20) | β (SE) | p | 9 months (n = 19) | 12 months (n = 16) | β (SE) | p | |||
| SI-R | 54.15 (10.99) | 47.79 (12.73) | 43.00 (13.69) | − 20.59 | 0.90 (0.23–1.56) | − 11.37 (2.00) | <.001 | 40.67 (16.53) | 42.56 (19.45) | 1.18 (2.57) | .644 |
| CIR | 3.60 (1.22) | – | 2.75 (1.07) | − 23.61 | 0.74 (0.10–1.38) | − 0.85 (0.22) | <.001 | – | |||
| ADL-H | 27.89 (8.77) | 23.94 (6.03) | 23.33 (5.26) | − 16.35 | 0.62 (− .09–1.31) | − 4.54 (1.16) | < .001 | 22.71 (6.02) | 26.14 (8.61) | 2.79 (0.99) | .005 |
| HADS Anxiety | 8.65 (4.80) | – | 8.11 (4.21) | − 6.24 | 0.12 (−.51–.75) | − 0.77 (0.86) | .373 | – | |||
| HADS Depression | 6.80 (4.40) | – | 5.89 (4.24) | − 13.38 | 0.21 (− .42–.84) | − 1.02 (0.66) | .121 | – | |||
| CGI Severity | 3.45 (1.05) | – | 3.65 (0.93) | 5.80 | − 0.20 (− .82–.42) | 0.20 (0.24) | .406 | – | |||
Analyses were mixed-effects linear regression models using the ITT sample. This sample was comprised of participants who completed at least one follow-up assessment
ADL-H activities of daily living-hoarding, CGI clinical global impressions, CIR clutter image rating, HADS Hospital Anxiety and Depression Scale, SI-R savings inventory-revised
These analyses assessed the change from the post-treatment assessment (at 6 months from baseline) through the follow up assessments (at 9 and 12 months from baseline)
There was a large effect size for the follow-up sample change score between baseline and post-treatment assessment on the SI-R Total (d = 0.90, (95% CI 0.23–1.56)], a medium-to-large effect size on the CIR [d = 0.74, (95% CI 0.10–1.38)], and a medium effect size on the ADL-H [d = 0.62, (95% CI − 0.09–1.31)]. Forty percent of participants who completed at least one follow-up assessment were classified as treatment responders on the SI-R; 80% were classified as treatment responders on the CIR; and 50% were classified as treatment responders on the CGI improvement scale. A significantly greater percentage of participants who completed at least one follow-up assessment were classified as treatment responders compared with participants who did not complete at least one follow-up assessment [SI-R: ×2 (1) = 4.99, p = .03; CIR: ×2 (1) = 15.25, p < .001; CGI Improvement: ×2 (1) = 5.11, p = .02]
Mixed-effects linear regression models with the follow-up sample indicated no symptom change from post-treatment assessment through 12 month follow-up assessment on the SI-R [β = 1.18, p = .644; Fig. 4], but there was a significant increase in symptom severity on the ADL-H (β = 2.79, p = .005; Fig. 5). Paired t tests suggested that the changes from 9-month to 12-month follow-up were non-significant on the SI-R [t (14) = 1.46, p = .08), but were significant on the ADL-H [t (12) = 2.15, p = .03]
Potential Effect of Previous Hoarding Treatment
Across both studies, 12 participants had received previous individual treatment for hoarding. Of the participants in study 1 (CREST), one participant had previously engaged in individual CREST and three participants had previously engaged in individual case management for hoarding. Of the participants in study 2 (ET), six participants had previously engaged in individual CREST and two participants had previously engaged in individual case management for hoarding. Post-hoc analyses of the data suggest that the inclusion of these individuals did not affect the outcomes of the current studies. There was no significant difference in allocation of participants with previous treatment between the two studies (×2 (1) = .43, p = .51). Furthermore, participants who had previous treatment were not significantly less likely to be classified as treatment responders for either study on the SI-R [Study 1: ×2 (1) = 0.11, p = .74; Study 2: ×2 (1) = 0.75, p = .36], CIR [Study 1: ×2 (1) = .11, p = .74; Study 2: ×2 (1) = 0.51, p = .48), or on the CGI [Study 1: ×2 (1) = 1.86, p = .17; Study 2: ×2(1) = 0.05, p = .83]
Discussion
The goals of this investigation were to evaluate the initial efficacy of two group-based interventions for adults with HD: a group-based version of CREST and a group-based exposure only treatment. Participants in both studies demonstrated significant reductions in hoarding severity and clutter, as well as improved scores in activities of daily living. Despite the similarities in improvement on hoarding and daily functioning in participants from both studies, only study 1 (CREST) participants reported significant decreases in symptoms of anxiety and depression. Furthermore, only study 1 participants were rated has having significant improvement on the CGI Severity scale. Treatment gains on hoarding symptom severity were maintained by participants in both studies for the 6 months following treatment.
The current studies were composed of mostly female (72–74%) and middle-aged participants (average age 55–61), which is consistent with the demographics of previous treatment studies for hoarding (average proportion of women 76%; mean age 58.7; Tolin et al. 2015). The current studies also demonstrated similar rates of participants taking psychiatric medications (37–60%) to previous hoarding studies (44.6%; Tolin et al. 2015).
The two studies both demonstrated large pre-to post-treatment effect sizes on overall hoarding severity (SI-R: CREST: d = 0.84, ET: d = 0.82), which is consistent with the effect size for overall hoarding severity observed in a meta-analysis of group and individual CBT treatment for hoarding (Hedges’ g = 0.82; Tolin et al. 2015), but lower than the effect size observed for pre-to post-treatment changes for individual CREST (d = 1.71; Ayers et al. 2017). Furthermore, although a substantial portion of participants in both studies were classified as treatment responders on the SI-R (CREST: 32%; ET: 26%), CIR (CREST: 68%; ET: 51%) and CGI Improvement scale (CREST: 44%; ET: 34%), these results are lower than were previously observed for participants who received individual CREST (SI-R: 64%; CIR: 88%; CGI Improvement: 78%) (Ayers et al. 2017).
Both studies had high retention rates during the active treatment phase (CREST = 88% retained at post-treatment assessment, ET = 74% retained at post-treatment assessment), underscoring the high level of motivation of HD patients to participate in treatment, even in a group format. These results are consistent with the retention rates observed in previous studies of psychotherapy for hoarding, which have ranged from 67–100% for group psychotherapy and 55–100% for individual psychotherapy (Thompson et al. 2017).
The overall investigation had several limitations including small sample size, differences in number of participants in each group, and lack of randomization. The CREST group sizes (6, 5, 8, 6) were smaller than the ET group sizes (6, 6, 10, 13). Participants in the larger ET groups attended an average of 3.5 sessions fewer than did participants in the smaller ET groups. Although participants in the two larger ET groups were not less likely to respond to treatment than the participants in the two smaller ET groups, the limited number of groups prevents any definitive conclusions about the potential effect of group size on treatment outcomes. Furthermore, the smaller group sizes seen in the CREST study may have inflated the effect of the treatment; future studies should investigate both CREST and ET in a range of group sizes.
Furthermore, raters were not blind to treatment condition, which may have impacted results on the CGI. Our participants were not excluded if they had psychiatric medication changes, previous individual CREST, previous case management for hoarding, or bipolar disorder. While this may represent a more real-world sample, it could also potentially dampen or confound our results. For instance, if someone started a medication during treatment, this may have bolstered symptom reduction. Twenty percent of the participants in the current studies were previously enrolled in hoarding treatment. Although this may signal that the participants did not benefit from previous treatment and may be resistant and/or have a greater degree of psychopathology than the typical hoarding patient, we did not find that these participants were less likely to be classified as treatment responders in either of the studies.
Finally, the lack of consistent follow-up data was a major limitation of the current investigation. Only 10 of the 22 participants assessed at post-treatment in the CREST groups (45%) and 16 of the 26 participants assessed at post-treatment in the ET groups (62%) completed the final follow-up assessment. In contrast, a recently published trial of individual treatment outcomes for elderly hoarding patients had much higher rates of follow-up completion (84% for individual CREST and 95% for individual case management) (Ayers et al. 2017). This discrepancy may have been due to the use of volunteer research assistants, rather than permanent study staff, for the tracking and execution of the follow-up assessments for the current investigation. Because of the large amount of contact attempts required to effectively engage hoarding patients (Ayers et al. 2015), it is likely that many of the participants in the current investigation did not receive the requisite amount of calls in order to complete the follow-up assessments. Thus, any conclusions about the effect of CREST and ET in a group setting should be considered tentative.
Conclusions
Results provide preliminary evidence for both group ET and group CREST as effective treatments for reducing hoarding symptoms. ET may require less training, but CREST has small to medium additional effects on anxiety and depressive symptom severity and may result in more global improvement. Considering the deleterious social, occupational, family, and health problems associated with hoarding disorder (Diefenbach et al. 2013) and the resource intensive nature of the individual CREST, the group CREST results are particularly promising.
Future directions include an adequately powered randomized controlled trial of group ET versus CREST, as well as individual ET and CREST, utilizing typical inclusion and exclusion criteria for psychotherapy outcome studies. Given the amount of literature on CBT for hoarding, future work should explore the differences between CREST, that uses cognitive rehabilitation, and CBT that relies on cognitive therapy. To date, we are uncertain the mechanisms of action and essential elements of effective behavioral treatment for hoarding disorder.
Acknowledgments
Funding This study was funded by a Career Development Award (CSRD-068-10S) and a Merit Award (CLNA-005-14S) from the Clinical Science R and D Program of the Veterans Health Administration awarded to Catherine Ayers, Ph.D., ABPP. The contents do not reflect the views of the Department of Veterans Affairs or the United States Government.
Footnotes
Conflict of Interest Catherine R. Ayers, Mary E. Dozier, Charles T. Taylor, Tina L. Mayes, James O. E. Pittman, Elizabeth W. Twamley declare that they have no conflict of interest.
Compliance with Ethical Standards
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Animal Rights Statement No animal studies were carried out by the authors for this article.
Informed Consent Informed consent was obtained from all individual participants included in the study.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental health disorders: DSM-5. Washington, DC: American Psychiatric Publishing. [Google Scholar]
- Ayers CR, Bratiotis C, Saxena S, & Wetherell JL (2012). Therapist and patient perspectives on cognitive-behavioral therapy for older adults with hoarding disorder: A collective case study. Aging & Mental Health, 16, 915–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayers CR, Dozier ME, Mayes TL, Espejo EP, Wilson A, Iqbal Y, & Strickland K (2015). Treatment recruitment and retention of geriatric participants with hoarding disorder. Clinical Gerontologist, 38, 235–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayers CR, Dozier ME, Twamley ET, Granholm E, Saxena S, Mayes TL, & Wetherell JL (2017). Cognitive rehabilitation and exposure/sorting therapy for hoarding disorder among older adults: A randomized controlled trial. The Journal of Clinical Psychiatry. 10.4088/JCP.16m11072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayers CR, Dozier ME, Wetherell JL, Twamley EW, & Schiehser DM (2016). Executive functioning in participants over age of 50 with hoarding disorder. The American Journal of Geriatric Psychiatry, 24, 342–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayers CR, Najmi S, Mayes T, & Dozier ME (2015). Hoarding disorder in older adults. American Journal of Geriatric Psychiatry, 23, 416–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayers CR, Saxena S, Espejo E, Twamley EW, Granholm E, & Wetherell JL (2014). Novel treatment for geriatric hoarding disorder: An open trial of cognitive rehabilitation paired with behavior therapy. The American Journal of Geriatric Psychiatry, 22, 248–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayers CR, Saxena S, Golshan S, & Wetherell JL (2010). Age at onset and clinical features of late life compulsive hoarding. International Journal of Geriatric Psychiatry, 25, 142–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayers CR, Schiehser D, Liu L, & Wetherell JL (2012). Functional impairment in geriatric hoarding participants. Journal of Obsessive-Compulsive and Related Disorders, 1, 263–266. [Google Scholar]
- Bulli F, Melli G, Carraresi C, Stopani E, Pertusa A, & Frost RO (2014). Hoarding behaviour in an Italian non-clinical sample. Behavioural and Cognitive Psychotherapy, 42, 297–311. [DOI] [PubMed] [Google Scholar]
- Cougle JR (2012). What makes a quality therapy? A consideration of parsimony, ease, and efficiency. Behavior Therapy, 43, 468–481. [DOI] [PubMed] [Google Scholar]
- Diefenbach GJ, DiMauro J, Frost R, Steketee G, & Tolin DF (2013). Characteristics of hoarding in older adults. The American Journal of Geriatric Psychiatry, 21, 1043–1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dozier ME, Wetherell JL, Twamley EW, Schiehser DM, & Ayers CR (2016). The relationship between age and neurocognitive and daily functioning in adults with hoarding disorder. International Journal of Geriatric Psychiatry, 31, 1329–1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frost RO, & Hartl TL (1996). A cognitive-behavioral model of compulsive hoarding. Behaviour Research and Therapy, 34, 341–350. [DOI] [PubMed] [Google Scholar]
- Frost RO, Hristova V, Steketee G, & Tolin DF (2013). Activities of daily living scale in hoarding disorder. Journal of Obsessive-Compulsive and Related Disorders, 2, 85–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frost RO, Steketee G, & Grisham J (2004). Measurement of compulsive hoarding: Saving inventory-revised. Behaviour Research and Therapy, 42, 1163–1182. [DOI] [PubMed] [Google Scholar]
- Frost RO, Steketee G, Tolin DF, & Renaud S (2008). Development and validation of the clutter image rating. Journal of Psychopathology and Behavioral Assessment, 30, 193–203. [Google Scholar]
- Guy W (1976). Clinical global impression scale. The ECDEU assessment manual for psychopharmacology-revised Vol. DHEW Publ No ADM, 76, 218–222. [Google Scholar]
- Iervolino AC, Perroud N, Fullana MA, Guipponi M, Cherkas L, Collier DA, & Mataix-Cols D (2009). Prevalence and heritability of compulsive hoarding: A twin study. American Journal of Psychiatry, 166, 1156–1161. [DOI] [PubMed] [Google Scholar]
- Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, … Chertkow H. (2005). The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. Journal of the American Geriatrics Society, 53, 695–699. [DOI] [PubMed] [Google Scholar]
- Saxena S, Ayers CR, Dozier ME, & Maidment KM (2015). The UCLA hoarding severity scale: Development and validation. Journal of Affective Disorders, 175, 488–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saxena S, Ayers CR, Maidment KM, Vapnik T, Wetherell JL, & Bystritsky A (2011). Quality of life and functional impairment in compulsive hoarding. Journal of Psychiatric Research, 45, 475–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan D, Lecrubier Y, Sheehan KH, Sheehan K, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, & Dunbar G (1998). Diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry, 59, 22–33. [PubMed] [Google Scholar]
- StataCorp. (2013). Stata Statistical Software: Release 13. College Station, TX: StataCorp LP. [Google Scholar]
- Steketee G, & Frost RO (2014). Compulsive Hoarding and Acquiring: Therapist Guide (2nd ed.). New York: Oxford University Press. [Google Scholar]
- Thompson C, de la Cruz LF, Mataix-Cols D, & Onwumere J (2017). A systematic review and quality assessment of psychological, pharmacological, and family-based interventions for hoarding disorder. Asian Journal of Psychiatry, 27, 53–66. [DOI] [PubMed] [Google Scholar]
- Timpano KR, Exner C, Glaesmer H, Rief W, Keshaviah A, Brähler E, & Wilhelm S (2011). The epidemiology of the proposed DSM-5 hoarding disorder: Exploration of the acquisition specifier, associated features, and distress. The Journal of Clinical Psychiatry, 72, 780–786. [DOI] [PubMed] [Google Scholar]
- Tolin DF, Frost RO, Steketee G, Gray KD, & Fitch KE (2008). The economic and social burden of compulsive hoarding. Psychiatry Research, 160, 200–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolin DF, Frost RO, Steketee G, & Muroff J (2015). Cognitive behavioral therapy for hoarding disorder: A meta-analysis. Depression and Anxiety, 32, 158–166. [DOI] [PubMed] [Google Scholar]
- Tolin DF, Meunier SA, Frost RO, & Steketee G (2010). Course of compulsive hoarding and its relationship to life events. Depression and Anxiety, 27, 829–838. [DOI] [PubMed] [Google Scholar]
- Turner K, Steketee G, & Nauth L (2010). Treating elders with compulsive hoarding: A pilot program. Cognitive and Behavioral Practice, 17, 449–457. [Google Scholar]
- Twamley EW, Savla GN, Zurhellen CH, Heaton RK, & Jeste DV (2008). Development and pilot testing of a novel compensatory cognitive training intervention for people with psychosis. American Journal of Psychiatric Rehabilitation, 11, 144–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twamley EW, Thomas KR, Burton CZ, Vella L, Jeste DV, Heaton RK, & McGurk SR (2017). Compensatory cognitive training for people with severe mental illnesses in supported employment: A randomized controlled trial. Schizophrenia Research. 10.1016/j.schres.2017.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twamley EW, Thomas KR, Gregory AM, Jak AJ, Bondi MW, Delis DC, & Lohr JB (2015). CogSMART compensatory cognitive training for traumatic brain injury: Effects over 1 year. The Journal of Head Trauma Rehabilitation, 30, 391–401. [DOI] [PubMed] [Google Scholar]
- Twamley EW, Vella L, Burton CZ, Heaton RK, & Jeste DV (2012). Compensatory cognitive training for psychosis: Effects in a randomized controlled trial. The Journal of Clinical Psychiatry, 73, 1212–1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woody SR, Kellman-McFarlane K, & Welsted A (2014). Review of cognitive performance in hoarding disorder. Clinical Psychology Review, 34, 324–336. [DOI] [PubMed] [Google Scholar]
- Zigmond AS, & Snaith RP (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67, 361–370. [DOI] [PubMed] [Google Scholar]


