Abstract
Introduction:
Health systems are increasingly interested in addressing the social determinants of health via social risk screening. The objective of this study is to understand the variability in the number and types of social risks overall and in population subgroups among primary care patients routinely screened in a large urban health system.
Methods:
Between April and December 2018, a total of 24,633 primary care patients completed a 10-item screener across 19 ambulatory sites within a health system in the Bronx, NY. The prevalence of any social risk and specific social risks was estimated overall and for population subgroups. Wald tests were used to determine statistically significant differences by subgroup. Data were analyzed in winter/spring 2019.
Results:
Twenty percent of patients presented with at least 1 social risk. The most frequently reported risks included housing quality (6.5%) and food insecurity (6.1%). Middle-aged (30–59 years) respondents (24.7%, 95% CI=23.6%, 25.7%) compared with those aged 18–29 years (17.7%, 95% CI=16.4%, 19.2%, p<0.001), and Medicaid patients (24.8%, 95% CI=24.0%, 25.5%) compared with commercially insured patients (11.8%, 95% CI=11.1%, 12.5%, p<0.001), were more likely to report social risks. The strongest predictor of housing quality risk was residing in public housing (15.1%, 95% CI=13.8%, 16.6%) compared with those not in public housing (5.6%, 95% CI=5.3%, 5.9%, p<0.001). Housing quality was the most frequently reported risk for children (aged <18 years) and older adults (aged ≥70 years), whereas, for middle-aged respondents (30–69 years), it was food insecurity.
Conclusions:
There are important differences in the prevalence of overall and individual social risks by subgroup. These findings should be considered to inform clinical care and social risk screening and interventions.
INTRODUCTION
Health systems are increasingly interested in addressing the social determinants of health (SDH) to improve health outcomes and reduce costs. SDH refers to the “conditions in the places where people live, learn, work, and play [that] affect a wide range of health risks and outcomes.”1 SDH are institutional and structural factors that require policy changes for long-term improvement. However, health systems have the opportunity to mitigate social risks, the manifestations of SDH at the individual level, through clinical interventions.2 Research has documented the impact of social risks3 on outcomes, such as food insecurity and cardiovascular risk factors,4 housing instability and emergency department visits,5 and social isolation and mortality,6 among others. Although it is difficult to quantify the exact contribution of social risks to health, there is consensus that it is a major contributor.7–10 As health care moves toward value-based payments, hospitals are incentivized to focus holistically by incorporating social needs screening and interventions into care.11–13 As a result, routine screening for social risks in health care has emerged as a strategy for addressing individual- and household-level social risks.13–15
Despite increased interest and recommendations,16,17 routine screening for social risks is not standard care,14 and as a result, only patients that communicate a risk during an encounter are referred for services. Before health systems can address social risks, they need to know the burden of risk and which patients are most likely to have multiple risks. However, large-scale and multisite studies are lacking,18 making it difficult to understand patterns of risk for distinct patient groups. There are few descriptive studies systematically assessing the prevalence of social risks overall and by population subgroups.19–23 These data could help inform how to use clinical and community-based resources to address SDH. This study examines the variability in the number and type of social risks overall and for population subgroups in the primary care setting within a large, urban health system.
METHODS
Study Population
A multidisciplinary committee across Montefiore Medical Center, a large network of hospitals, ambulatory sites, and a school of medicine in the Bronx, NY, met to pilot screening approaches to address SDH (details are in the Appendix Text, available online). Two tools were piloted; 1 homegrown tool and a modified version of the Health Leads’ screener, an externally validated tool.24 Following the pilot, a 10-item screener based on the Health Leads’ screener but supplemented with questions from the homegrown tool was implemented (Table 1). These 10 risks were selected because they are specific, actionable, and common concerns for households based on the expert opinion of the committee. The committee acknowledged the importance of upstream factors, such as racism and education, but opted to focus on those that could be readily addressed by the healthcare system or community partners.
Table 1.
SDH Screening Questions and Variable Names
| SDH screening question | Variable name |
|---|---|
| Are you worried that the place you are living now is making you sick? (has mold, bugs/rodents, water leaks, not enough heat) | Housing quality |
| Are you worried that in the next 2 months, you may not have a safe or stable place to live? (eviction, being kicked out, homelessness) | Housing instability |
| In the last 12 months, did you worry that your food could run out before you got money to buy more? | Food insecurity |
| In the last 12 months, has lack of transportation kept you from medical appointments or getting your medications? | Health travel |
| In the last 12 months, did you have to skip buying medications or going to doctor’s appointments to save money? | Health cost |
| In the past 12 months, has the electric, gas, oil, or water company threatened to shut off services to your home? | Utilities cost |
| Are you finding it hard to get along with a partner, spouse, or family members? | Getting along |
| Do you need help getting child care or care for an elderly or sick adult? | Care need |
| Do you need legal help? (child/family services, immigration, housing discrimination, domestic issues, etc)? | Legal |
| Does anyone in your life hurt you, threaten you, frighten you or make you feel unsafe? | Interpersonal violence |
Between April and December 2018, patients were given a paper version to complete while in the waiting or exam room at 19 ambulatory sites in the Bronx (n=17 sites) and Westchester County (n=2). Of 26,236 unique patients who were invited, 5.5% declined; a comparison of completers/decliners is in Appendix Table 1 (available online).
Clinics had the discretion to determine whom to screen and the frequency of screenings. Clinic decisions were informed by multiple factors, including the availability of staff (e.g., social workers and community health workers). Appendix Table 2 (available online) delineates the screening practices of clinics, including whether the clinic focused on a higher risk population, children or adults, the number of patients screened, and the proportion screened.
The tool was available in 9 languages. Parents/guardians completed the screener for patients who were too young to respond independently. After patients completed the screener, results were entered into the Epic electronic health record. Providers reviewed the results with patients and offered to connect patients to clinic-based resources. A positive screen for interpersonal violence led to an immediate social work handoff.
Measures
To understand heterogeneity in risk by population subgroups and to rank the risks, the following outcome variables were examined: having any, 1, 2, or ≥ 3 social risks and having each individual risk (Tables 2 and 3) (Figure 1). These categories were selected as only 2.7% of the sample reported ≥4 risks.
Table 2.
Number of SDH Risks Among Montefiore Patients by Patient Characteristics, April—December 2018
| Characteristic | Screened, n (%) | Comparison population,a % | Any risk, % (95% CI) | 1 risk, % (95% CI) | 2 risks, % (95% CI) | ≥3 risks, % (95% CI) |
|---|---|---|---|---|---|---|
| Total | 24,633 (100.0) | 100.0 | 20.0 (19.5, 20.5) | 10.3 (9.9, 10.7) | 4.6 (4.4, 4.9) | 5.1 (4.8, 5.3) |
| Age, years | ||||||
| 0–5 | 4,884 (19.8) | 13.5 | 18.3 (17.3, 19.4) | 10.3 (9.5, 11.2) | 4.0 (3.5, 4.6) | 4.0 (3.5, 4.6) |
| 6–11 | 3,036 (12.3) | 10.8 | 19.0 (17.6, 20.4) | 10.2 (9.2, 11.4) | 3.7 (3.1, 4.4) | 5.0 (4.3, 5.9) |
| 12–17 | 2,415 (9.8) | 9.2 | 17.2 (15.7, 18.7) | 9.7 (8.6, 11.0) | 3.7 (3.0, 4.6) | 3.7 (3.0, 4.6) |
| 18–29 (ref) | 2,798 (11.4) | 10.8 | 17.7 (16.4, 19.2) | 9.1 (8.1, 10.2) | 4.7 (4.0, 5.5) | 4.0 (3.3, 4.8) |
| 30–39 | 1,945 (7.9) | 8.4 | 23.7*** (21.8, 25.6) | 11.5** (10.1, 13.0) | 6.3* (5.3, 7.5) | 5.9** (4.9, 7.0) |
| 40–49 | 2,063 (8.4) | 9.6 | 24.9*** (23.1, 26.8) | 10.8 (9.5, 12.2) | 6.2* (5.2, 7.3) | 8.0*** (6.9, 9.2) |
| 50–59 | 2,656 (10.8) | 13.5 | 25.2*** (23.6, 26.9) | 10.8* (9.7, 12.1) | 6.4** (5.6, 7.4) | 7.9*** (7.0, 9.0) |
| 60–69 | 2,461 (10.0) | 12.4 | 21.2** (19.6, 22.9) | 11.1* (9.9, 12.4) | 4.6 (3.9, 5.5) | 5.4* (4.6, 6.4) |
| ≥70 | 2,375 (9.6) | 11.8 | 16.0 (14.5, 17.5) | 9.8 (8.7, 11.1) | 3.1 (2.5, 3.8) | 3.1 (2.5, 3.8) |
| Sex | ||||||
| Male | 10,172 (41.3) | 39.9 | 19.1** (18.3, 19.8) | 10.0 (9.5, 10.6) | 4.0*** (3.7, 4.4) | 5.0 (4.6, 5.4) |
| Female (ref) | 14,461 (58.7) | 60.1 | 20.7 (20.0, 21.3) | 10.5 (10.0, 11.0) | 5.0 (4.7, 5.4) | 5.1 (4.8, 5.5) |
| Race/ethnicity | ||||||
| Hispanic (ref) | 8,671 (50.4) | 48.9 | 23.6 (22.7, 24.5) | 11.8 (11.2, 12.5) | 5.6 (5.2, 6.1) | 6.2 (5.7, 6.7) |
| NHB | 7,103 (41.3) | 40.3 | 18.9*** (18.0, 19.8) | 9.5*** (8.9, 10.2) | 4.4** (3.9, 4.9) | 5.0** (4.5, 5.5) |
| NHW | 944 (5.5) | 7.5 | 16.5*** (14.3, 19.0) | 8.3** (6.7, 10.2) | 4.1 (3.0, 5.6) | 4.1* (3.0, 5.6) |
| NHAPI | 393 (2.3) | 2.8 | 13.2*** (10.2, 17.0) | 6.9** (4.8, 9.8) | 4.1 (2.5, 6.5) | 2.3** (1.2, 4.3) |
| NHAIAN | 92 (0.5) | 0.5 | 22.8 (15.3, 32.6) | 15.2 (9.2, 24.1) | 3.3 (1.0, 9.7) | 4.3 (1.6, 11.1) |
| Missing | 7,430 (—) | — | 17.6*** (16.8, 18.5) | 9.7*** (9.1, 10.4) | 3.8*** (3.4, 4.2) | 4.1*** (3.7, 4.6) |
| Preferred language | ||||||
| English (ref) | 19,804 (83.5) | 82.0 | 19.5 (19.0, 20.1) | 10.1 (9.7, 10.5) | 4.5 (4.2, 4.8) | 4.9 (4.6, 5.2) |
| Spanish | 3,274 (13.8) | 14.9 | 26.1*** (24.6, 27.6) | 12.9*** (11.8, 14.1) | 6.1*** (5.3, 7.0) | 7.1*** (6.3, 8.0) |
| Other | 651 (2.7) | 3.0 | 12.6*** (10.3, 15.4) | 6.1** (4.5, 8.3) | 3.7 (2.5, 5.4) | 2.8* (1.7, 4.3) |
| Missing | 904 (—) | — | 14.0*** (11.9, 16.5) | 8.6 (7.0, 10.6) | 2.5** (1.7, 3.8) | 2.9** (2.0, 4.2) |
| Insurance status | ||||||
| Medicaid | 12,144 (50.9) | 42.6 | 24.8*** (24.0, 25.5) | 12.0*** (11.5, 12.6) | 5.8*** (5.4, 6.2) | 6.9*** (6.5, 7.4) |
| Medicare | 3,763 (15.8) | 19.3 | 21.7*** (20.4, 23.1) | 11.6*** (10.7, 12.7) | 4.8*** (4.1, 5.5) | 5.3*** (4.6, 6.1) |
| Commercial (ref) | 7,947 (33.3) | 38.1 | 11.8 (11.1, 12.5) | 7.0 (6.5, 7.6) | 2.6 (2.3, 3.0) | 2.1 (1.8, 2.5) |
| Missing | 779 (—) | — | 21.7*** (18.9, 24.7) | 11.2*** (9.1, 13.6) | 5.4*** (4.0, 7.2) | 5.1*** (3.8, 6.9) |
| FQHCb | ||||||
| No (ref) | 10,469 (42.5) | 64.3 | 15.2 (14.5, 15.9) | 8.1 (7.5, 8.6) | 3.4 (3.1, 3.7) | 3.7 (3.4, 4.1) |
| Yes | 14,164 (57.5) | 35.7 | 23.6*** (22.9, 24.3) | 12.0*** (11.5, 12.5) | 5.5*** (5.2, 5.9) | 6.0*** (5.7, 64.4) |
| Value-based contract | ||||||
| No (ref) | 14,045 (57.0) | — | 18.9 (18.2, 19.5) | 9.7 (9.3, 10.2) | 4.4 (4.0, 4.7) | 4.8 (4.4, 5.2) |
| Yes | 10,588 (43.0) | — | 21.5*** (20.7, 22.3) | 11.1*** (10.5, 11.7) | 5.0*** (4.6, 5.4) | 5.4*** (5.0, 5.9) |
| Public housingc | ||||||
| No (ref) | 19,564 (88.0) | 89.3 | 19.1 (18.5, 19.6) | 9.8 (9.4, 10.2) | 4.4 (4.1, 4.7) | 4.9 (4.6, 5.2) |
| Yes | 2,658 (12.0) | 10.7 | 28.4*** (26.8, 30.2) | 16.0*** (14.7, 17.5) | 6.1*** (5.2, 7.1) | 6.3** (5.5, 7.3) |
| Area-based povertyd | ||||||
| Q1: 0.0%–8.3% (ref) | 4,703 (20.2) | 19.4 | 12.2 (11.3, 13.2) | 6.5 (5.9, 7.3) | 3.0 (2.5, 3.5) | 2.7 (2.3, 3.2) |
| Q2: 8.4%–19.2% | 4,663 (20.0) | 20.6 | 17.1*** (16.1, 18.2) | 8.7*** (7.9, 9.5) | 4.1** (3.6, 4.7) | 4.3*** (3.8, 4.9) |
| Q3: 19.3%–31.4% | 4,663 (20.0) | 20.4 | 21.0*** (19.8, 22.2) | 10.2*** (9.4, 11.1) | 5.0*** (4.4, 5.7) | 5.7*** (5.1, 6.5) |
| Q4: 31.5%–43.4% | 4,670 (20.0) | 20.8 | 23.4*** (22.2, 24.6) | 12.7*** (11.8, 13.7) | 5.2*** (4.6, 5.9) | 5.4*** (4.8, 6.1) |
| Q5: 43.5%–75.5% | 4,646 (19.9) | 18.8 | 25.9*** (24.6, 27.1) | 13.8*** (12.9, 14.9) | 5.3*** (4.7, 6.0) | 6.7*** (6.0, 7.5) |
| Area-based race/ethnicityd | ||||||
| % NHB | ||||||
| Q1: 0.0%–10.8% (ref) | 4,666 (20.0) | 23.3 | 18.8 (17.7, 19.9) | 9.8 (8.9, 10.6) | 4.3 (3.8, 4.9) | 4.7 (4.1, 5.4) |
| Q2: 10.9%–23.4% | 4,700 (20.1) | 22.1 | 21.3** (20.2, 22.5) | 10.8 (10.0, 11.7) | 5.0 (4.4, 5.7) | 5.5 (4.9, 6.2) |
| Q3: 23.5%–35.5% | 4,636 (19.9) | 18.1 | 22.1*** (21.0, 23.3) | 12.0** (11.1, 13.0) | 5.0 (4.4, 5.7) | 5.1 (4.5, 5.8) |
| Q4: 35.6%–55.9% | 4,666 (20.0) | 17.3 | 21.0** (19.8, 22.2) | 11.0 (10.1, 11.9) | 4.6 (4.1, 5.3) | 5.4 (4.8, 6.1) |
| Q5: 56.0%–100.0% | 4,677 (20.0) | 19.3 | 16.2** (15.2, 17.3) | 8.4* (7.7, 9.3) | 3.7 (3.2, 4.3) | 4.1 (3.5, 4.7) |
| % Hispanic | ||||||
| Q1: 0.0%–24.8% (ref) | 4,906 (21.0) | 24.0 | 14.3 (13.4, 15.3) | 7.8 (7.1, 8.6) | 3.2 (2.8, 3.8) | 3.3 (2.8, 3.8) |
| Q2: 24.9%–44.7% | 4,470 (19.2) | 18.2 | 17.9*** (16.8, 19.1) | 9.5** (8.7, 10.4) | 4.2* (3.7, 4.8) | 4.2* (3.7, 4.9) |
| Q3: 44.8%–59.2% | 4,675 (20.0) | 17.8 | 21.0*** (19.8, 22.2) | 10.7*** (9.8, 11.6) | 4.8*** (4.3, 5.5) | 5.5*** (4.9, 6.2) |
| Q4: 59.3%–70.7% | 4,660 (20.0) | 17.7 | 22.4*** (21.3, 23.7) | 12.0*** (11.1, 12.9) | 4.9*** (4.3, 5.6) | 5.6*** (5.0, 6.3) |
| Q5: 70.8%–98.6% | 4,634 (19.9) | 22.3 | 24.0*** (22.8, 25.2) | 12.1*** (11.2, 13.1) | 5.6*** (5.0, 6.3) | 6.3*** (5.6, 7.0) |
| Area-based rental burdend,e | ||||||
| <30% (ref) | 7,220 (31.6) | 29.2 | 17.4 (16.6, 18.3) | 9.7 (9.0, 10.4) | 3.6 (3.2, 4.0) | 4.1 (3.7, 4.6) |
| 30%–50% | 12,371 (54.1) | 56.1 | 21.2*** (20.5, 22.0) | 10.8* (10.3, 11.4) | 5.0*** (4.6, 5.4) | 5.4*** (5.0, 5.8) |
| >50% | 3,268 (14.3) | 14.6 | 21.3*** (19.9, 22.7) | 10.8 (9.8, 11.9) | 5.1*** (4.4, 5.9) | 5.4** (4.7, 6.2) |
Note: Boldface indicates statistical significance (
p<0.05,
p<0.01,
p<0.001).
The comparison population includes all patients (n=205,145) that had a primary care visit at a clinic implementing the screener during the timeframe for this study.
Indicates that the screener was completed at an FQHC
Only includes patients who live in New York City.
Area-level measures are at the Census block group level. They only include those who were successfully geocoded (n=443 were not geocoded). Residents who were geocoded to block groups with zero population (according to the Census) were excluded from the analysis for this variable.
Rental burden is defined as median gross rent as a percentage of household income in the past 12 months.
FQHC, Federally Qualified Health Center; NHAIAN, American Indian/Alaskan Native, non-Hispanic; NHAPI, Asian/Pacific Islander, non-Hispanic; NHB, black, non-Hispanic; NHW, white, non-Hispanic; Q, quintile; SDH, social determinants of health.
Table 3.
Individual SDH Risks Among Montefiore Patients by Patient Characteristics, April—December 2018
| Characteristic | Housing | Food insecurity, % (95% CI) | Access to healthcare | Getting along, % (95% CI) | Utilities cost, % (95% CI) | Care need, % (95% CI) | Legal, % (95% CI) | Interpersonal violence, % (95% CI) | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Quality, % (95% CI) | Instability, % (95% CI) | Health travel, % (95% CI) | Health cost, (95% CI) | |||||||
| Total | 6.5 (6.2, 6.8) | 4.8 (4.5, 5.1) | 6.1 (5.8, 6.4) | 4.7 (4.4, 5.0) | 3.8 (3.6, 4.1) | 3.5 (3.3, 3.8) | 3.4 (3.1, 3.6) | 3.3 (3.1, 3.5) | 3.0 (2.8, 3.2) | 1.5 (1.4, 1.7) |
| Age, years | ||||||||||
| 0–5 | 6.4** (5.7, 7.1) | 3.4 (2.9, 4.0) | 4.1 (3.6, 4.7) | 3.8 (3.3, 4.4) | 2.0*** (1.6, 2.4) | 1.9*** (1.6, 2.4) | 3.0** (2.5, 3.5) | 5.3*** (4.7, 6.0) | 3.2** (2.7, 3.7) | 0.8*** (0.6, 1.1) |
| 6–11 | 7.8*** (6.9, 8.8) | 4.4 (3.7, 5.2) | 5.7 (4.9, 6.6) | 3.4 (2.8, 4.1) | 2.4*** (1.9, 3.0) | 2.2*** (1.7, 2.8) | 4.2*** (3.5, 4.9) | 3.9** (3.2, 4.6) | 2.8* (2.3, 3.5) | 1.3 (1.0, 1.8) |
| 12–17 | 6.6** (5.7, 7.7) | 3.6 (2.9, 4.4) | 5.7 (4.9, 6.7) | 3.2 (2.6, 4.0) | 2.2*** (1.7, 2.9) | 2.4*** (1.8, 3.1) | 3.5*** (2.9, 4.3) | 1.9 (1.4, 2.5) | 2.5 (2.0, 3.2) | 1.2 (0.8, 1.7) |
| 18–29 (ref) | 4.5 (3.8, 5.3) | 4.0 (3.4, 4.8) | 4.9 (4.2, 5.8) | 4.0 (3.3, 4.8) | 4.2 (3.5, 5.0) | 5.0 (4.2, 5.8) | 1.9 (1.4, 2.4) | 2.3 (1.8, 2.9) | 2.0 (1.5, 2.6) | 1.8 (1.4, 2.4) |
| 30–39 | 6.6** (5.6, 7.8) | 6.4** (5.4, 7.5) | 7.2** (6.1, 8.4) | 5.5* (4.6, 6.6) | 5.4* (4.5, 6.5) | 6.2 (5.2, 7.4) | 4.0*** (3.2, 5.0) | 3.8** (3.1, 4.8) | 3.1* (2.4, 4.0) | 1.9 (1.4, 2.6) |
| 40–49 | 7.3*** (6.2, 8.5) | 7.0*** (6.0, 8.2) | 9.7*** (8.5, 11.1) | 6.0** (5.1, 7.1) | 6.2** (5.3, 7.4) | 6.1 (5.1, 7.2) | 4.9*** (4.1, 5.9) | 2.3 (1.7, 3.0) | 4.0*** (3.3, 5.0) | 2.5 (1.9, 3.3) |
| 50–59 | 8.4*** (7.4, 9.5) | 7.3*** (6.4, 8.4) | 9.6*** (8.6, 10.8) | 7.3*** (6.4, 8.4) | 6.1** (5.3, 7.1) | 5.1 (4.4, 6.1) | 4.9*** (4.1, 5.8) | 2.6 (2.1, 3.3) | 4.4*** (3.7, 5.2) | 2.2 (1.7, 2.9) |
| 60–69 | 6.5** (5.6, 7.5) | 5.7** (4.9, 6.7) | 6.9** (6.0, 8.0) | 6.2*** (5.3, 7.2) | 5.1 (4.3, 6.0) | 3.3** (2.7, 4.1) | 2.8* (2.2, 3.5) | 2.5 (1.9, 3.2) | 2.8* (2.2, 3.6) | 1.7 (1.3, 2.3) |
| ≥70 | 4.4 (3.6, 5.3) | 3.3 (2.7, 4.1) | 4.0 (3.3, 4.9) | 4.0 (3.3, 4.9) | 3.6 (2.9, 4.4) | 2.2*** (1.6, 2.8) | 1.8 (1.3, 2.4) | 2.8 (2.2, 3.5) | 2.2 (1.7, 2.9) | 1.0* (0.6, 1.5) |
| Sex | ||||||||||
| Male | 6.2 (5.8, 6.7) | 4.9 (4.5, 5.4) | 5.9 (5.4, 6.3) | 4.4 (4.0, 4.8) | 3.5** (3.1, 3.8) | 3.2** (2.8, 3.5) | 3.2 (2.9, 3.6) | 3.4 (3.0, 3.7) | 3.2 (2.8, 3.5) | 1.4 (1.2, 1.7) |
| Female (ref) | 6.7 (6.3, 7.1) | 4.7 (4.4, 5.1) | 6.3 (5.9, 6.7) | 4.9 (4.5, 5.2) | 4.1 (3.8, 4.5) | 3.8 (3.5, 4.1) | 3.5 (3.2, 3.8) | 3.2 (2.9, 3.5) | 2.9 (2.6, 3.2) | 1.6 (1.4, 1.8) |
| Race/ethnicity | ||||||||||
| Hispanic (ref) | 7.9 (7.4, 8.5) | 6.1 (5.6, 6.6) | 7.7 (7.1, 8.3) | 5.9 (5.4, 6.4) | 4.8 (4.4, 5.3) | 4.3 (3.9, 4.7) | 4.0 (3.6, 4.4) | 3.5 (3.1, 3.9) | 3.4 (3.0, 3.8) | 1.9 (1.6, 2.2) |
| NHB | 6.0*** (5.4, 6.5) | 4.6*** (4.2, 5.2) | 5.7*** (5.2, 6.3) | 4.1*** (3.7, 4.6) | 3.8** (3.4, 4.3) | 3.6* (3.2, 4.1) | 3.7 (3.3, 4.1) | 2.9* (2.5, 3.3) | 3.1 (2.8, 3.6) | 1.2** (1.0, 1.5) |
| NHW | 3.7*** (2.7, 5.1) | 3.8** (2.8, 5.3) | 5.7* (4.4, 7.4) | 4.9 (3.7, 6.5) | 3.5 (2.5, 4.9) | 3.5 (2.5, 4.9) | 2.1** (1.4, 3.3) | 1.8** (1.1, 2.9) | 1.8* (1.1, 2.9) | 2.4 (1.6, 3.7) |
| NHAPI | 2.3*** (1.2, 4.4) | 1.3*** (0.5, 3.0) | 4.1** (2.5, 6.6) | 3.3* (1.9, 5.7) | 4.1 (2.5, 6.6) | 1.3** (0.5, 3.0) | 1.5* (0.7, 3.4) | 2.0 (1.0, 4.0) | 3.1 (1.7, 5.3) | 0.3* (0.0, 1.8) |
| NHAIAN | 4.3 (1.6, 11.1) | 5.5 (2.3, 12.6) | 4.3 (1.6, 11.1) | 5.4 (2.3, 12.5) | 2.2 (0.5, 8.3) | 3.3 (1.1, 9.8) | 4.3 (1.6, 11.1) | 4.3 (1.6, 11.1) | 4.4 (1.7, 11.3) | 1.1 (0.2, 7.4) |
| Missing | 5.9*** (5.4, 6.5) | 3.7*** (3.3, 4.2) | 4.9*** (4.5, 5.4) | 3.8*** (3.4, 4.3) | 2.8*** (2.5, 3.2) | 2.8*** (2.4, 3.2) | 2.6*** (2.2, 3.0) | 3.7 (3.3, 4.1) | 2.5** (2.2, 2.9) | 1.3* (1.1, 1.6) |
| Preferred language | ||||||||||
| English (ref) | 6.3 (6.0, 6.7) | 4.5 (4.2, 4.8) | 5.8 (5.5, 6.1) | 4.4 (4.2, 4.7) | 3.9 (3.6, 4.2) | 3.8 (3.6, 4.1) | 3.5 (3.2, 3.7) | 3.0 (2.7, 3.2) | 2.9 (2.7, 3.1) | 1.5 (1.4, 1.7) |
| Spanish | 8.8*** (7.9, 9.9) | 7.9*** (7.1, 8.9) | 9.7*** (8.7, 10.7) | 6.9*** (6.1, 7.8) | 4.5 (3.9, 5.3) | 3.1* (2.5, 3.7) | 3.6 (3.0, 4.3) | 4.5*** (3.9, 5.3) | 3.4 (2.9, 4.1) | 1.9 (1.5, 2.4) |
| Other | 4.2* (2.9, 6.0) | 2.8* (1.7, 4.3) | 3.4* (2.2, 5.1) | 2.6* (1.6, 4.2) | 1.7** (0.9, 3.0) | 1.1** (0.5, 2.2) | 1.4** (0.7, 2.6) | 3.4 (2.2, 5.1) | 4.5* (3.1, 6.3) | 0.5* (0.1, 1.4) |
| Missing | 3.7** (2.6, 5.1) | 2.0** (1.3, 3.1) | 3.0** (2.1, 4.3) | 3.3 (2.3, 4.7) | 1.6*** (0.9, 2.6) | 1.1*** (0.6, 2.0) | 1.7** (1.0, 2.7) | 5.2*** (3.9, 6.9) | 2.7 (1.8, 4.0) | 0.7* (0.3, 1.5) |
| Insurance | ||||||||||
| Medicaid | 8.4*** (7.9, 8.9) | 6.5*** (6.0, 6.9) | 8.0*** (7.5, 8.4) | 6.3*** (5.8, 6.7) | 4.0*** (3.6, 4.3) | 4.2*** (3.8, 4.6) | 4.5*** (4.1, 4.9) | 4.5*** (4.2, 4.9) | 4.2*** (3.8, 4.6) | 1.9*** (1.6, 2.1) |
| Medicare | 6.7*** (6.0, 7.6) | 5.4*** (4.7, 6.1) | 6.8*** (6.0, 7.6) | 6.3*** (5.6, 7.1) | 5.3*** (4.7, 6.1) | 3.4* (2.8, 4.0) | 2.8** (2.3, 3.3) | 2.8*** (2.3, 3.4) | 2.9*** (2.4, 3.4) | 2.0*** (1.6, 2.5) |
| Commercial | 3.6 (3.2, 4.0) | 1.9 (1.7, 2.3) | 3.0 (2.6, 3.4) | 1.4 (1.2, 1.7) | 2.6 (2.3, 3.0) | 2.6 (2.3, 3.0) | 1.9 (1.6, 2.2) | 1.6 (1.4, 1.9) | 1.2 (1.0, 1.5) | 0.8 (0.6, 1.0) |
| Missing | 4.9 (3.6, 6.7) | 5.4*** (4.0, 7.3) | 7.0*** (5.4, 9.0) | 5.1*** (3.8, 6.9) | 7.0*** (5.4, 9.0) | 3.7 (2.6, 5.3) | 3.6** (2.6, 5.2) | 2.5 (1.6, 3.8) | 3.6*** (2.5, 5.2) | 0.9 (0.4, 1.9) |
| FQHCa | ||||||||||
| No (ref) | 4.3 (3.9, 4.7) | 3.5 (3.1, 3.9) | 4.3 (3.9, 4.7) | 3.1 (2.8, 3.5) | 2.9 (2.6, 3.2) | 3.4 (3.1, 3.8) | 2.4 (2.1, 2.7) | 2.5 (2.2, 2.8) | 2.1 (1.9, 2.4) | 1.4 (1.2, 1.6) |
| Yes | 8.1*** (7.7, 8.6) | 5.8*** (5.4, 6.2) | 7.5*** (7.1, 7.9) | 5.8*** (5.4, 6.2) | 4.6*** (4.2, 4.9) | 3.6 (3.3, 3.9) | 4.1*** (3.8, 4.4) | 3.9*** (3.6, 4.2) | 3.6*** (3.3, 4.0) | 1.6 (1.4, 1.9) |
| Value-based contract | ||||||||||
| No (ref) | 6.0 (5.6, 6.4) | 4.4 (4.1, 4.8) | 5.9 (5.5, 6.3) | 4.1 (3.8, 4.5) | 3.7 (3.4, 4.0) | 3.6 (3.3, 3.9) | 3.1 (2.8, 3.4) | 3.0 (2.7, 3.3) | 3.0 (2.7, 3.3) | 1.5 (1.4, 1.8) |
| Yes | 7.1*** (6.6, 7.6) | 5.3** (4.9, 5.8) | 6.5* (6.0, 7.0) | 5.4*** (5.0, 5.9) | 4.0 (3.7, 4.4) | 3.5 (3.1, 3.8) | 3.7* (3.3, 4.1) | 3.6* (3.3, 4.0) | 3.0 (2.7, 3.3) | 1.5 (1.3, 1.7) |
| Public housingb | ||||||||||
| No (ref) | 5.6 (5.3, 5.9) | 4.7 (4.5, 5.1) | 5.9 (5.6, 6.3) | 4.4 (4.1, 4.7) | 3.8 (3.5, 4.1) | 3.5 (3.2, 3.8) | 3.5 (3.3, 3.8) | 3.2 (3.0, 3.5) | 2.9 (2.7, 3.2) | 1.5 (1.4, 1.7) |
| Yes | 15.1*** (13.8, 16.6) | 4.9 (4.2, 5.8) | 7.3** (6.4, 8.3) | 6.4*** (5.5, 7.4) | 4.3 (3.6, 5.2) | 3.8 (3.1, 4.6) | 2.1*** (1.6, 2.7) | 4.0* (3.3, 4.8) | 4.0** (3.3, 4.8) | 1.5 (1.1, 2.1) |
| Area-based povertyc | ||||||||||
| Q1: 0%–8.3% (ref) | 2.8 (2.3, 3.3) | 2.3 (1.9, 2.8) | 3.2 (2.8, 3.8) | 2.6 (2.2, 3.1) | 2.7 (2.3, 3.2) | 3.0 (2.5, 3.5) | 1.9 (1.5, 2.3) | 2.2 (1.9, 2.7) | 1.7 (1.3, 2.1) | 1.0 (0.8, 1.4) |
| Q2: 8.4%–19.2% | 4.2*** (3.7, 4.8) | 4.5*** (3.9, 5.1) | 5.3*** (4.7, 6.0) | 3.8** (3.3, 4.4) | 4.0** (3.5, 4.6) | 3.5 (3.0, 4.1) | 3.2*** (2.7, 3.7) | 2.4 (2.0, 2.9) | 2.7** (2.3, 3.2) | 1.4 (1.1, 1.8) |
| Q3:19.3%–31.4% | 6.4*** (5.7, 7.2) | 5.3*** (4.7, 6.0) | 7.0*** (6.3, 7.8) | 5.2*** (4.6, 5.9) | 4.1*** (3.6, 4.7) | 3.4 (2.9, 4.0) | 4.2*** (3.6, 4.8) | 3.5*** (3.0, 4.0) | 3.1*** (2.6, 3.6) | 2.0*** (1.7, 2.5) |
| Q4: 31.5%–43.4% | 8.1*** (7.3, 8.9) | 5.6*** (5.0, 6.3) | 7.3*** (6.5, 8.0) | 5.5*** (4.9, 6.2) | 3.7** (3.2, 4.3) | 3.6 (3.1, 4.2) | 3.4*** (2.9, 4.0) | 4.2*** (3.6, 4.8) | 3.3*** (2.8, 3.8) | 1.4 (1.1, 1.8) |
| Q5: 43.5%–75.5% | 11.0*** (10.1, 11.9) | 5.7*** (5.0, 6.4) | 7.3*** (6.6, 8.1) | 5.9*** (5.3, 6.6) | 4.3*** (3.8, 5.0) | 4.1** (3.6, 4.7) | 4.1*** (3.5, 4.7) | 4.0*** (3.5, 4.7) | 4.1*** (3.5, 4.7) | 1.7** (1.4, 2.1) |
| Area-based race/ethnicityc | ||||||||||
| % NHB | ||||||||||
| Q1: 0%–10.8% (ref) | 5.4 (4.7, 6.0) | 4.6 (4.1, 5.3) | 6.1 (5.5, 6.9) | 4.8 (4.2, 5.4) | 3.7 (3.2, 4.3) | 3.4 (2.9, 4.0) | 3.3 (2.8, 3.8) | 3.2 (2.7, 3.8) | 2.5 (2.1, 3.0) | 1.6 (1.3, 2.0) |
| Q2:10.9%–23.4% | 7.3*** (6.6, 8.1) | 5.2 (4.6, 5.9) | 6.5 (5.9, 7.3) | 5.1 (4.5, 5.7) | 3.8 (3.3, 4.4) | 3.5 (3.0, 4.1) | 4.2* (3.7, 4.8) | 3.3 (2.8, 3.8) | 3.4* (2.9, 3.9) | 2.0 (1.6, 2.4) |
| Q3: 23.5%–35.5% | 7.5*** (6.8, 8.4) | 5.0 (4.4, 5.7) | 6.7 (6.0, 7.5) | 5.1 (4.5, 5.7) | 4.1 (3.6, 4.7) | 3.9 (3.3, 4.5) | 3.0 (2.6, 3.5) | 3.2 (2.8, 3.8) | 2.9 (2.5, 3.4) | 1.5 (1.2, 2.0) |
| Q4: 35.6%–55.9% | 7.6*** (6.8, 8.3) | 5.0 (4.4, 5.6) | 6.1 (5.4, 6.8) | 4.6 (4.0, 5.3) | 4.0 (3.5, 4.6) | 3.6 (3.1, 4.2) | 3.2 (2.8, 3.8) | 3.6 (3.1, 4.1) | 3.3* (2.8, 3.9) | 1.4 (1.1, 1.8) |
| Q5: 56.0%–100% | 4.6 (4.0, 5.2) | 3.6** (3.1, 4.1) | 4.6** (4.0, 5.2) | 3.5** (3.0, 4.0) | 3.2 (2.7, 3.7) | 3.3 (2.8, 3.8) | 2.9 (2.4, 3.4) | 3.0 (2.5, 3.5) | 2.7 (2.3, 3.2) | 1.1* (0.8, 1.4) |
| % Hispanic | ||||||||||
| Q1: 0%–24.8% (ref) | 3.3 (2.8, 3.8) | 3.0 (2.5, 3.5) | 4.0 (3.5, 4.6) | 3.1 (2.6, 3.6) | 3.1 (2.7, 3.6) | 2.9 (2.5, 3.4) | 2.6 (2.2, 3.1) | 2.4 (2.0, 2.9) | 2.1 (1.7, 2.5) | 1.1 (0.9, 1.5) |
| Q2: 24.9%–44.7% | 5.6*** (4.9, 6.3) | 3.8* (3.3, 4.4) | 5.0* (4.4, 5.7) | 4.0* (3.4, 4.6) | 3.4 (2.9, 4.0) | 3.6* (3.1, 4.2) | 2.8 (2.4, 3.4) | 3.3** (2.8, 3.9) | 2.9* (2.4, 3.4) | 1.3 (1.0, 1.7) |
| Q3: 44.8%–59.2 | 7.3*** (6.6, 8.1) | 5.4*** (4.8, 6.1) | 6.4*** (5.7, 7.1) | 4.6*** (4.0, 5.2) | 3.9* (3.4, 4.5) | 3.4 (2.9, 4.0) | 3.5* (3.0, 4.0) | 3.2* (2.8, 3.8) | 3.1** (2.7, 3.7) | 1.3 (1.0, 1.6) |
| Q4: 59.3%–70.7% | 7.9*** (7.2, 8.7) | 5.3*** (4.7, 5.9) | 6.8*** (6.2, 7.6) | 5.1*** (4.5, 5.8) | 3.9* (3.4, 4.5) | 4.0** (3.4, 4.6) | 3.7** (3.2, 4.2) | 3.4** (2.9, 3.9) | 3.5*** (3.0, 4.1) | 2.1*** (1.7, 2.5) |
| Q5: 70.8%–98.6% | 8.4*** (7.7, 9.3) | 6.0*** (5.3, 6.7) | 7.9*** (7.2, 8.7) | 6.3*** (5.6, 7.0) | 4.5*** (4.0, 5.2) | 3.8* (3.3, 4.4) | 4.1*** (3.6, 4.7) | 4.0*** (3.5, 4.6) | 3.2** (2.7, 3.8) | 1.9** (1.5, 2.3) |
| Area-based rental burdenc,d | ||||||||||
| <30% (ref) | 5.9 (5.4, 6.5) | 3.8 (3.4, 4.2) | 4.9 (4.4, 5.4) | 3.6 (3.2, 4.1) | 3.4 (3.0, 3.9) | 3.5 (3.1, 3.9) | 2.2 (1.9, 2.5) | 2.9 (2.5, 3.3) | 2.5 (2.2, 2.9) | 1.4 (1.2, 1.7) |
| 30%–50% | 6.9** (6.5, 7.4) | 5.2*** (4.8, 5.6) | 6.6*** (6.2, 7.1) | 5.2*** (4.8, 5.6) | 4.0* (3.7, 4.3) | 3.5 (3.2, 3.9) | 3.8*** (3.4, 4.1) | 3.5* (3.2, 3.8) | 3.2** (2.9, 3.6) | 1.6 (1.4, 1.9) |
| >50% | 6.7 (5.9, 7.6) | 5.1** (4.4, 5.9) | 6.5** (5.7, 7.4) | 4.7* (4.0, 5.5) | 3.9 (3.3, 4.7) | 3.7 (3.1, 4.4) | 4.4*** (3.7, 5.1) | 3.3 (2.8, 4.0) | 3.0 (2.5, 3.7) | 1.6 (1.2, 2.1) |
Note: Boldface indicates statistical significance (
p<0.05,
p<0.01,
p<0.001).
Indicates that the screener was completed at an FQHC.
Only includes patients who live in New York City.
Area-level measures are at the Census block group level. They only include those who were successfully geocoded (n=443 were not geocoded). Residents who were geocoded to block groups with zero population (according to the Census) were excluded from the analysis for this variable.
Rental burden is defined as median gross rent as a percentage of household income in the past 12 months.
FQHC, Federally Qualified Health Center; NHAIAN, American Indian/Alaskan Native, non-Hispanic; NHAPI, Asian/Pacific Islander, non-Hispanic; NHB, black, non-Hispanic; NHW, white, non-Hispanic; Q, quintile; SDH, social determinants of health.
Figure 1.
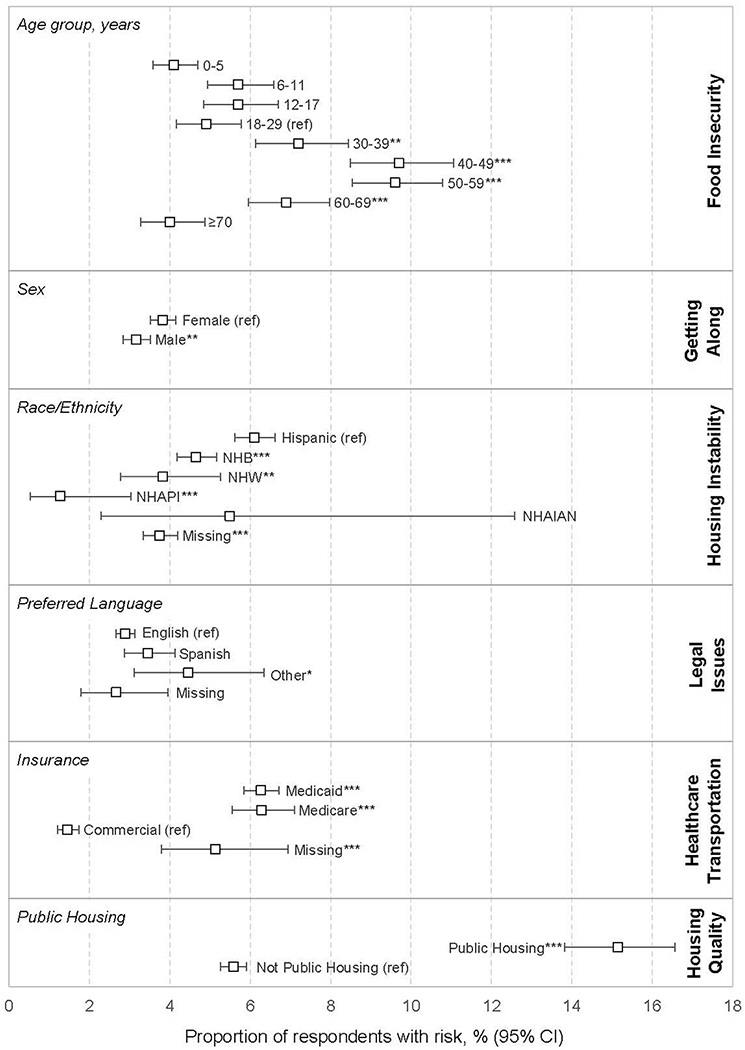
Primary findings for individual SDH risks by patient characteristics, April–December 2018. Findings in Figure 1 were selected because they were deemed the most interesting or important findings from Table 2. Complete findings can be found in Table 2. Asterisks indicate statistical significance (*p<0.05, **p<0.01, ***p<0.001). Ref indicates a reference group for the Wald test.
NHB, black, non-Hispanic; NHW, white, non-Hispanic; NHAPI, Asian/Pacific Islander, non-Hispanic; NHAIAN, American Indian/Alaskan Native, non-Hispanic; SDH, social determinants of health.
Predictor variables included age (categories: 0–5, 6–11, 12–17, 18–29, 30–39, 40–49, 50–59, 60–69, and ≥70 years), sex, race/ethnicity (Hispanic; black, non-Hispanic; white, non-Hispanic; Asian/Pacific Islander, non-Hispanic; American Indian/Alaskan Native, non-Hispanic; and a missing indicator), health insurance at the screening visit (Medicaid, Medicare, commercial, and a missing indicator), whether the screening visit was at a Federally Qualified Health Center, an indicator for whether a value-based contract covered the patient, the patient’s preferred language (English, Spanish, other, and a missing indicator), and whether the respondent lived in New York City public housing. Although parents/guardians completed the screener for children who were too young to respond, the age of the child was used in this analysis because parents’ age was not available, and social risks identified at child visits impact that child. Respondent data were extracted from the electronic health record using Looking Glass Clinical Analytics, an application supporting the extraction of clinical data.25 Patients with a value-based contract were flagged using data from the Montefiore Care Management Organization. These are patients, from all 3 payers (Medicaid, Medicare, and commercial), for whom Montefiore bears partial or full financial risk based on patient outcomes. This indicator was included as addressing social risks in this population may have a particularly high financial upside. Given the limited number of individual SES variables, area-based measures of SES, including the proportion of the Census block group population living below poverty and rental burden (given that housing insecurity was a measure of interest), were included. Because of concerns about missing individual data on race and ethnicity, the data on Census block group race and ethnicity (i.e., percentage non-Hispanic black and percentage Hispanic) were included.
To obtain public housing status and area-based measures, the addresses of those who lived in New York State (95.1%) were geocoded using the New York State Street and Address Composite geocoding services tool. After 98.5% of respondents were successfully geocoded, those who lived in public housing were identified by flagging addresses that geocoded to tax lots associated with public housing. Other area-based measures came from the 2012–2016 American Community Survey at the block group level.26 The respondents that were not geocoded (n=526) were excluded from geographic analyses.
Statistical Analysis
Respondents who did not complete ≥5 of the 10 screener questions (n=161) were excluded, resulting in a final sample size of n=24,633 patients. The prevalence of overall social risk and individual risks was estimated for each population subgroup. To determine if the prevalence of these risks varied by subgroup, Wald tests were used to estimate pairwise p-values comparing each prevalence to the a priori reference group.
In addition, to examine if the screened population was generalizable to the primary care population, the sociodemographic distributions of the screened population were compared with primary care patients with visits at the participating clinics (herein referred to as the comparison population). Proportion tests were used to test for differences in the 2 populations (Appendix Table 3, available online). The screened population was then weighted by age, race/ethnicity, and insurance distribution of the comparison population (Appendix Table 3, available online), and the prevalence of overall social risks and individual risks were estimated in weighted analyses (Appendix Tables 4 and 5, available online). Finally, the prevalence of overall social risk and individual risks was estimated stratified by targeted screening group (normal risk versus higher risk) (Appendix Tables 6 and 7, available online).
Statistical analyses were completed using Stata, version 13.1, and mapping used ArcGIS, version 10.3. The study was approved by the Albert Einstein College of Medicine IRB. Data were analyzed in winter/spring 2019.
RESULTS
This descriptive, cross-sectional study used data from screeners completed by 24,633 patients as of December 31, 2018. Patients declining the screener were more likely to be older; white, non-Hispanic; insured through Medicare; and to prefer a language other than English (Appendix Table 1, available online).
About 42% of screened respondents were children/adolescents (Table 2). More than half of the sample (58.7%) was female, and the median age was 26.1 years (51.3 years among adults). Among those with nonmissing race/ethnicity data, most respondents were Hispanic (50.4%) or black, non-Hispanic (41.3%). Most (83.5%) of the population indicated their preferred language was English; 13.8% preferred Spanish. Half were on Medicaid (50.9%). Twelve percent of New York City respondents lived in public housing. The screened population was younger than the comparison population (median age of 26.1 years vs 36.9 years), whereas patients in the comparison population were somewhat more likely to be white, non-Hispanic and have commercial insurance/Medicare.
Overall, 20% of respondents reported at least 1 social risk; 10.3% reported 1 risk, 4.6% had 2 risks, and 5.1% had ≥3 risks (Table 2). For adults, the social risk burden increased with age, peaking among those aged 50–59 years and then declining. Men had a marginally lower social risk burden compared with women. Both black, non-Hispanic and white, non-Hispanic respondents had a lower burden than Hispanic respondents. Compared with respondents preferring English, those preferring Spanish had a significantly higher risk, whereas those preferring other languages had a significantly lower risk. Additional analyses found that Hispanic respondents preferring Spanish were significantly more likely to report any risk and ≥2 risks than Hispanic respondents preferring English (26.1% vs 22.7% for ≥1 risk). Medicaid recipients were much more likely to have single and multiple social risks compared with commercially insured respondents; Medicare recipients had an intermediate burden when compared with the other groups. Respondents living in public housing were more likely to have any and multiple risks compared with those not in public housing. Area-based poverty was also associated with social risks in a dose-dependent manner.
In weighted analyses (Appendix Table 4, available online), the prevalence and patterns of social risk remained largely the same; 19.8% reported at least 1 risk compared to 20.0% in unweighted analyses. There were slight differences in the weighted analyses; for example, the difference in any risk by sex attenuated, as did the elevated risk for Spanish speakers, relative to English speakers. In analyses stratified by targeted screening group (Appendix Table 6, available online), 25.4% of respondents were screened in the higher risk context, and 74.6% were screened in the normal-risk context. A larger proportion of those screened in the higher risk context reported at least 1 social risk (25.2%) than those screened in the normal-risk context (18.2%).
Primary findings on individual social risks are in Figure 1, and additional data on individual social risks are in Table 3. The most prevalent individual risks were housing quality (6.5%) and food insecurity (6.1%). For each risk, the association between age, sex, race/ethnicity, insurance status, and other factors varied, though some consistent associations were observed. Medicaid status, middle age (30–39, 40–49, and 50–59 years), Hispanic race/ethnicity, and living in a higher-poverty neighborhood were associated with an elevated burden, whereas preferring languages other than English and Spanish was generally associated with a lower burden.
As Figure 1 shows, there were specific patterns in the most frequently reported social risks for subgroups; for example, the most frequently reported risk for children (aged <18 years) and those aged ≥70 years was housing quality, whereas young adults (aged 18–29 years) most frequently reported difficulties getting along with family members. For those aged 30–69 years, the most commonly reported risk was food insecurity. The strongest predictor of reporting a housing quality issue was residing in public housing (15.1% vs 5.6%). Women were more likely to report challenges getting along with a family member compared with men, although no major difference was observed for the interpersonal violence measure.
After weighting, the rank of social risks by prevalence remained the same, as did most patterns across subgroups (Appendix Table 5, available online). Important differences included a slight decline in the elevated risk for those aged 30–39 years, increased risk of housing instability and legal issues for male respondents, and increased risk of legal issues for those who speak other languages. The rank of social risks by prevalence for those screened in the higher risk context differed slightly than those screened in the normal-risk context, with food insecurity being the most prevalent for those in the higher risk context rather than housing quality (Appendix Table 7, available online).
DISCUSSION
This study estimates the prevalence of social risks for a large and diverse urban patient population and, based on a review of the literature, represents the largest comprehensive assessment of social risks from a large-scale health system screening initiative. The study goes beyond others by assessing the patient population from 3 specialties across 19 sites and examining the results by numerous stratifications. These results highlight population patterns that may be relevant to health systems with similar demographics and population attributes and could be used to inform interventions.
Directly comparing the overall results to other studies is challenging because of differences in the populations being screened21,23,27–31 and, more importantly, differences in the screening tools, either based on the number or types of risks being screened for23,30,32–34 or the wording of the instrument.35–38 Among more comparable studies, Berkowitz et al.20 screened 5,125 adult primary care patients in Boston, finding that 34.6% of the population had at least 1 risk. Notably, this study screened for more and different risks, namely education and employment; therefore, an estimate of 20% seems reasonable. Health systems may be hesitant to systematically screen for social risks out of concerns that the burden will be so high it will overwhelm a stretched healthcare system. However, these results, combined with the evidence that not all patients with social risks want assistance,32 suggest that it is possible if screeners target risks that are actionable, acute, and directly affect health outcomes and care.
Similar to the few previous studies that examined social risks by subgroup, this study found that respondents from racial/ethnic minority groups were more likely to have positive screenings.19–22 However, contrary to the previous literature, this study found that Hispanic respondents, rather than black, non-Hispanic respondents, had the highest-burden, which may be due to differences in immigration and compositional factors. Compared with the U.S. population, the Bronx has a higher proportion of both foreign-born black, non-Hispanic and Hispanic residents from the Caribbean and South America, as opposed to Mexico/Central America.39 Respondents who were insured through Medicaid,19,20 female,19 or preferred a language other than English20,22 were more likely to have social risks than their counterparts. Based on a review of the literature, only 2 studies found an elevated burden for middle-aged adults21,22; 1 study focused on transgender veterans, and the other was a small mixed-methods study. Aside from the large sample size, 1 important advantage of this study is that it breaks down disciplinary walls by including all age groups and 3 primary care specialties. Therefore, the specific unmet risks and the overall burden of risk could be compared across age groups, revealing that middle-aged adults have an elevated burden and social risks vary by age.
Similar to previous studies, we found that food insecurity is 1 of the most reported individual risks, alongside healthcare costs (including insurance), housing risks, transportation barriers, utilities, and child care (for pediatrics).19,20,23,28,32,33,40 Furthermore, the patterns of food insecurity in this study for specific groups of patients, specifically by age, race/ethnicity, and area-based poverty, are similar to those found for Bronx adults by the 2017 New York City Community Health Survey, a representative survey of New York City adult residents.41
This analysis identified new groups of patients that experienced the varying burden of risk. A review of the literature suggests this is the first study to examine overall social risk by public housing status, Federally Qualified Health Center status, and area-level poverty/rental burden. A strong predictor of housing quality was public housing status, which was not associated with housing instability or utility cost concerns. Previous literature shows that public housing residents are more likely to experience poor housing quality,42 and given that public housing includes utilities and is designed to provide stable housing, the latter findings are expected. Overall, living in public housing was the strongest predictor of having any social risk. Federally Qualified Health Center status is often used as a proxy for high-need populations, and the findings of an elevated burden for this population support this comparison.43,44 While previous studies have compared the burden of social risk for those whose preferred language is English or Spanish,19,22 this study was able to compare risk across groups, including other languages. Those who prefer languages other than Spanish/English had a lower burden except for legal risks (Figure 1).
Limitations
This study has several limitations. Although screening in a clinical setting can provide useful patient-specific and community-level information, findings may not be representative of community residents who do not seek/receive their care elsewhere. The intent of this analysis was not to infer the challenges faced by the general population, but rather the clinical population, upon which healthcare systems can have direct influence. Another limitation of the current implementation is that the screener is not uniformly administered, and clinics selected their target cohorts. To the extent these subpopulations have different burdens, the overall findings may not mirror true population-level distributions. However, in weighted analyses accounting for predictors of being screened, the overall social risk prevalence was unchanged, the relative ranking of individuals’ risks did not change, and the patterns of social risks by population subgroups were generally consistent. In addition, age-specific analyses are not always reflective of the age of the actual respondent, particularly in cases when parents/guardians responded for children, and should thus be interpreted cautiously. However, the screener is an assessment of household factors, which impact the child as well. Finally, self-reported social risks may understate true prevalence because patients may be reluctant or unable to answer accurately; unfortunately, no internal validation data are available to address the extent of potential underreporting and misreporting. Potential disclosure barriers include limited health literacy; feeling ashamed, embarrassed, or fearful; or feeling like staff would not be able to help.
CONCLUSIONS
Screening for social risks in the outpatient sites of a large health system provides robust new data to better understand the burden of risks for different subgroups of patients. These data can inform interventions targeted to address SDH by helping health systems identify the most prevalent risks and at-risk populations. The data also prompt discussion about the assets health systems can draw on to connect patients to resources and how to allocate resources. Descriptive data can further catalyze conversations and partnerships with community and government organizations. Finally, by capturing these data in the electronic health record, it is possible to study trends over time at the patient and subgroup levels, which can support further analyses on the impact of social risks and interventions on health outcomes.
Supplementary Material
ACKNOWLEDGMENTS
We would like to thank the leadership of Montefiore Medical Group, including the site-based leadership and champions who helped pilot and implement the screening tool. We would also like to thank Nicolette Guillou, Richard Reyf, Jacob Schutt, and Eva Franqui, who were instrumental in setting up the screening tool and providing social determinants of health reports.
Dr. Chambers is supported by grants from the National Heart, Lung, and Blood Institute (K01HL125466 and 1R03HL140265). Dr. Chambers and Dr. Rehm are supported by a grant from the National Institutes of Diabetes and Digestive and Kidney Diseases (P30 DK111022). Dr. Fiori is supported by grants from the Doris Duke Charitable Foundation (2018169) and the Agency for Health care Research and Quality, HHS (K12HS026396).
No other financial disclosures were reported by the authors of this paper.
Footnotes
SUPPLEMENTAL MATERIAL
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2019.11.011.
REFERENCES
- 1.CDC. Social determinants of health: know what affects health. www.cdc.gov/socialdeterminants/index.htm Updated January 29, 2018. Accessed May 19, 2019.
- 2.Castrucci B, Auerbach J. Meeting individual social needs falls short of addressing social determinants of health. Health Affairs Blog.. www.healthaffairs.org/do/10.1377/hblog20190115.234942/full/. Published January 2019. Accessed September 10, 2019.
- 3.Alderwick H, Gottlieb LM. Meanings and misunderstandings: a social determinants of health lexicon for health care systems. Milbank Q. 2019;97(2):407–419. 10.1111/1468-0009.12390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. 2010;140(2):304–310. 10.3945/jn.109.112573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ma CT, Gee L, Kushel MB. Associations between housing instability and food insecurity with health care access in low-income children. Ambul Pediatr. 2008;8(1):50–57. 10.1016/j.ambp.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 6.Pantell M, Rehkopf D, Jutte D, Syme SL, Balmes J, Adler N. Social isolation: a predictor of mortality comparable to traditional clinical risk factors. Am J Public Health. 2013;103(11):2056–2062. 10.2105/AJPH.2013.301261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Booske BC, Athens JK, Kindig DA, Park H, Remington PL. Country health rankings working paper. Different perspectives for assigning weights to determinants. www.countyhealthrankings.org/sites/default/files/differentPerspectivesForAssigningWeightsToDeterminantsOf-Health.pdf Published 2010. Accessed November 8, 2019.
- 8.Hood CM, Gennuso KP, Swain GR, Catlin BB. County Health Rankings: relationships between determinant factors and health outcomes.Am J Prev Med. 2016;50(2):129–135. 10.1016/j.amepre.2015.08.024. [DOI] [PubMed] [Google Scholar]
- 9.McGinnis JM, Williams-Russo P, Knickman JR. The case for more active policy attention to health promotion. Health Aff. 2002;21 (2):78–93. 10.1377/hlthaff.21.2.78. [DOI] [PubMed] [Google Scholar]
- 10.Krieger N Health equity and the fallacy of treating causes of population health as if they sum to 100%. Am J Public Health. 2017;107 (4):541–549. 10.2105/AJPH.2017.303655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adler NE, Cutler DM, Fielding JE, et al. Addressing social determinants of health and health disparities: a vital direction for health and health care. NAM Perspectives. Discussion paper. Washington, D.C.: National Academy of Medicine; Published September 19, 2016. 10.31478/201609t [DOI] [Google Scholar]
- 12.Alley DE, Asomugha CN, Conway PH, Sanghavi DM. Accountable Health Communities—addressing social needs through Medicare and Medicaid. N Engl J Med. 2016;374(1):8–11. 10.1056/NEJMp1512532. [DOI] [PubMed] [Google Scholar]
- 13.Lee J, Korba C. Social determinants of health: how are hospitals and health systems investing in and addressing social needs? https://www2.deloitte.com/content/dam/Deloitte/us/Documents/life-sciences-healthcare/us-lshc-addressing-social-determinants-of-health.pdf. Published 2017. Accessed 8 November 2019.
- 14.Billioux A, Verlander K, Anthony S, Alley D. Standardized screening for health-related social needs in clinical settings: the Accountable Health Communities screening tool. NAM Perspectives. Discussion paper. Washington, D.C.: National Academy of Medicine; Published May 30, 2017. 10.31478/201705b [DOI] [Google Scholar]
- 15.Bachrach D Addressing patients’ social needs: an emerging business case for provider investment. www.commonwealthfund.org/publications/fund-reports/2014/may/addressing-patients-social-needs-emerging-business-case-provider. Published 2014. Accessed 27 April 2019.
- 16.Council on Community Pediatrics. Poverty and child health in the United States. Pediatrics. 2016;137(4):e20160339 10.1542/peds.2016-0339. [DOI] [PubMed] [Google Scholar]
- 17.Institute of Medicine. Capturing Social and Behavioral Domains and Measures in Electronic Health Records: Phase 2. Washington, DC: The National Academies Press, 2015. [PubMed] [Google Scholar]
- 18.Gottlieb LM, Wing H, Adler NE. A systematic review of interventions on patients’ social and economic needs. Am J Prev Med. 2017;53 (5):719–729. 10.1016/j.amepre.2017.05.011. [DOI] [PubMed] [Google Scholar]
- 19.Berkowitz SA, Hulberg AC, Hong C, et al. Addressing basic resource needs to improve primary care quality: a community collaboration programme. BMJ Qual Saf. 2016;25(3):164–172. 10.1136/bmjqs-2015-004521. [DOI] [PubMed] [Google Scholar]
- 20.Berkowitz SA, Hulberg AC, Standish S, Reznor G, Atlas SJ. Addressing unmet basic resource needs as part of chronic cardiometabolic disease management. JAMA Intern Med. 2017;177(2):244–252. 10.1001/jamainternmed.2016.7691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Blosnich JR, Marsiglio MC, Dichter ME, et al. Impact of social determinants of health on medical conditions among transgender veterans. Am J Prev Med. 2017;52(4):491–498. 10.1016/j.amepre.2016.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Careyva BA, Hamadani R, Friel T, Coyne CA. A social needs assessment tool for an urban Latino population. J Commun Health. 2018;43 (1):137–145. 10.1007/s10900-017-0396-6. [DOI] [PubMed] [Google Scholar]
- 23.Gottlieb L, Hessler D, Long D, Amaya A, Adler N. A randomized trial on screening for social determinants of health: the iScreen Study. Pediatrics. 2014;134(6):e1611–e1618. 10.1542/peds.2014-1439. [DOI] [PubMed] [Google Scholar]
- 24.Health leads. Social needs screening toolkit. https://nopren.org/wpcontent/uploads/2016/12/Health-Leads-Screening-Toolkit-July-2016.pdf Published 2016. Accessed November 8, 2019.
- 25.Bellin E, Fletcher DD, Geberer N, Islam S, Srivastava N. Democratizing information creation from health care data for quality improvement, research, and education—the Montefiore Medical Center experience. Acad Med. 2010;85(8):1362–1368. 10.1097/ACM.0b013e3181df0f3b. [DOI] [PubMed] [Google Scholar]
- 26.U.S. Census Bureau. American community survey: areas published. www.census.gov/programs-surveys/acs/geography-acs/areas-published.html. Published 2018. Accessed November 8, 2019.
- 27.Friedman NL, Banegas M. Toward addressing social determinants of health: a health care system strategy. Perm J. 2018;22:18–095. 10.7812/TPP/18-095. [DOI] [Google Scholar]
- 28.Garg A, Toy S, Tripodis Y, Silverstein M, Freeman E. Addressing social determinants of health at well child care visits: a cluster RCT. Pediatrics. 2015;135(2):e296–e304. 10.1542/peds.2014-2888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hassan A, Scherer EA, Pikcilingis A, et al. Improving social determinants of health: effectiveness of a web-based intervention. Am J Prev Med. 2015;49(6):822–831. 10.1016/j.amepre.2015.04.023. [DOI] [PubMed] [Google Scholar]
- 30.Thompson T, McQueen A, Croston M, et al. Social needs and health-related outcomes among Medicaid beneficiaries. Health Educ Behav. 2019;46(3):436–444. 10.1177/1090198118822724. [DOI] [PubMed] [Google Scholar]
- 31.Waitzkin H, Getrich C, Heying S, et al. Promotoras as mental health practitioners in primary care: a multi-method study of an intervention to address contextual sources of depression. J Commun Health. 2011;36(2):316–331. 10.1007/s10900-010-9313-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gold R, Bunce A, Cowburn S, et al. Adoption of social determinants of health EHR tools by community health centers. Ann Fam Med. 2018;16(5):399–407. 10.1370/afm.2275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gottlieb LM, Hessler D, Long D, et al. Effects of social needs screening and in-person service navigation on child health: a randomized clinical trial. JAMA Pediatr. 2016;170(11):e162521 10.1001/jamapediatrics.2016.2521. [DOI] [PubMed] [Google Scholar]
- 34.Semple-Hess JE, Pham PK, Cohen SA, Liberman DB. Community resource needs assessment among families presenting to a pediatric emergency department. Acad Pediatr. 2019;19(4):378–385. 10.1016/j.acap.2018.11.009. [DOI] [PubMed] [Google Scholar]
- 35.Kangovi S, Mitra N, Grande D, et al. Patient-centered community health worker intervention to improve posthospital outcomes: a randomized clinical trial. JAMA Intern Med. 2014;174(4):535–543. 10.1001/jamainternmed.2013.14327. [DOI] [PubMed] [Google Scholar]
- 36.Katz A, Chateau D, Enns JE, et al. Association of the social determinants of health with quality of primary care. Ann Fam Med. 2018;16 (3):217–224. 10.1370/afm.2236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Page-Reeves J, Kaufman W, Bleecker M, et al. Addressing social determinants of health in a clinic setting: the WellRx pilot in Albuquerque, New Mexico. J Am Board Fam Med. 2016;29(3):414–418. 10.3122/jabfm.2016.03.150272. [DOI] [PubMed] [Google Scholar]
- 38.Prather AA, Gottlieb LM, Giuse NB, et al. National Academy of Medicine social and behavioral measures: associations with self-reported health. Am J Prev Med. 2017;53(4):449–456. 10.1016/j.amepre.2017.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.U.S. Census Bureau. 2017 American Community Survey. 1-Year Public Use Microdata Sample Data [2017], Published 2018. www.census.gov/programs-surveys/acs/data/pums.html.
- 40.Garg A, Sarkar S, Marino M, Onie R, Solomon BS. Linking urban families to community resources in the context of pediatric primary care. Patient Educ Couns. 2010;79(2):251–254. 10.1016/j.pec.2009.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.New York City Department of Health and Mental Hygiene. Community Health Survey [2017]. https://a816-healthpsi.nyc.gov/epiquery/CHS/CHSXIndex.html. Published 2017. Accessed 8 November 2019.
- 42.Chambers EC, Pichardo MS, Rosenbaum E. Sleep and the housing and neighborhood environment of urban Latino adults living in low-income housing: the AHOME study. Behav Sleep Med. 2016;14(2):169–184. 10.1080/15402002.2014.974180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chang CH, Lewis VA, Meara E, Lurie JD, Bynum JPW. Characteristics and service use of Medicare beneficiaries using Federally Qualified Health Centers. Med Care. 2016;54(8):804–809. 10.1097/MLR.0000000000000564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Signorello LB, Hargreaves MK, Blot WJ. The Southern Community Cohort Study: investigating health disparities. J Health Care Poor Underserved. 2010;21(1suppl):26–37. 10.1353/hpu.0.0245. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


