Abstract
The spread of drug resistance of Plasmodium falciparum and Plasmodium vivax parasites is a challenge towards malaria elimination. P. falciparum has shown an early and severe drug resistance in comparison to P. vivax in various countries. In fact, P. vivax differs in its life cycle and treatment in various factors: development and duration of sexual parasite forms differ, symptoms severity are unequal, relapses present only in P. vivax cases and the Artemisinin-based combination therapy (ACT) is only mandatory in P. falciparum cases. We compared the spread of drug resistance for both species through two compartmental models using ordinary differential equations. The model structure describes how sensitive and resistant parasite strains infect a human population treated with antimalarials. We found that an early transmission,i.e., before treatment and low effectiveness of drug coverage, supports the prevalence of sensitive parasites delaying the emergence of resistant P. vivax. These results imply that earlier attention of both symptomatic cases and reservoirs of P. vivax are essential in controlling transmission but also accelerate the spread of drug resistance.
Author summary
The main strategy to treat and prevent malaria still relies on the use of drugs targeting Plasmodium falciparum and Plasmodium vivax parasites. Since the worldwide number of cases is still large, there is a risk of emergence of drug resistance, which is precisely the case of resistance of chloroquine for P. falciparum and P. vivax in some countries. The spread of drug resistance challenges malaria control programs due to treatment failures and consequent lower drug efficacy. This phenomenon is more frequent, accelerated, and studied in P. falciparum cases but P. vivax also presents drug resistance in some areas and the particular life cycle of P. vivax with relapses due to its latent form, an earlier transmission and more common low parasitemia densities that imposes detection difficulties. We developed a mathematical model to study drug-resistance emergence in P. vivax finding that early transmission of drug-sensitive parasites as well as infected humans without symptoms delays drug resistance. As a consequence, however, the number of P. vivax cases decreases less than the number of P. falciparum cases. These results suggest that earlier attention of all infected humans, including individuals without symptoms, might help to decrease P. vivax cases but also accelerate the spread of drug resistance.
Introduction
The World Health Organization (WHO) estimated 219 million cases of malaria in 2017, most of them caused by Plasmodium falciparum due to high presence in Africa, with 96.6% of total numbers [1]. However, P. falciparum does not maintain such high dominance in other continents, since Plasmodium vivax is diagnosed in 74.1% and 37.2% of cases in the Americas and Southeast Asia, respectively [1]. Understanding conditions that drive the emergence of drug resistance for these species is vital in the goal of ending epidemics of malaria by 2030 in the Sustainable Development Goals (SDG 3.3) in United Nations [2].
Antimalarials have been the main strategy for controlling transmission, but drug resistance has emerged to drugs for P. falciparum infection implying slower clearance rates and treatment failures [3–5]. Currently, Artemisinin-based combination therapy (ACT) has constituted first-line treatment for P. falciparum as a fast-acting artemisinin derivative plus a longer-acting partner drug [6]. However, previous studies found resistance levels and slow clearance rates using ACTs such as dihydroartemisinin-piperaquine and artesunate-mefloquine in the Greater Mekong Subregion, bringing a need for developing new treatments [7–10].
P. vivax and P. falciparum differ in their life cycles [11–13] because P. vivax has a set of particularities that challenge malaria control: development in temperate climates, production of dormant-stage parasite forms (hypnozoites), development of low parasitemia densities and earlier transmission of sexual-parasite forms [14]. By contrast, although drug resistance in P. vivax also challenges malaria control programs, chloroquine (CQ) remains as first-line treatment for P. vivax while the extended CQ use for P. falciparum spread CQ-resistance for this parasite worldwide [6, 15, 16]. Nevertheless, CQ-resistance in P. vivax already affects some regions inducing the adoption of ACTs. Also, low parasitemia densities impose detection difficulties, which contribute to underestimating the real impact of drug resistance in P. vivax [11, 17]. Previous works have compared P. vivax with P. falciparum resistance through in vivo, in vitro, and molecular assays to test resistance, drug susceptibility, and characterization of gene changes [18]. However, such studies for P. vivax present difficulties in replicating the life cycle, producing a knowledge gap in understanding drug resistance in this species [19, 20].
Mathematical models provide an understanding of drug resistance to guide the development of malaria programs [21], through both deterministic and stochastic models simulating the implementation of monotherapies and combination therapies [22]. Models also showed the contribution on the emergence of resistant strains due to factors: fitness cost, selection of resistant parasites after treatment, changes in transmission settings, efficiency in drug dose and the role of asymptomatics [21–35]. These previous works inferred that sub-optimal doses, high treatment coverage, and lower levels of immunity have a direct relation to drug resistance. However, they based their findings in P. falciparum life cycle avoiding the particular features of P. vivax, producing an inaccurate extension of model results in the case of P. vivax control programs.
Previous P. vivax models focused on exploring the effect of relapses on malaria prevalence, and Schneider and Scalante placed a feature in their model to consider the evolution of drug resistance [36] by assessing parasite selection on a genetic model. Previous works estimated that relapses cause around 80% of P. vivax cases in children in Papua New Guinea suggesting a high epidemiological effect of hypnozoites [37, 38]. This finding agrees with previous models that predict a greater P. vivax prevalence than P. falciparum in the same transmission settings due to relapses [39] and a direct relation between P. vivax prevalence and relapse frequency [40]. Elimination programs must consider a relapse treatment with primaquine (PQ). Also, previous works have inferred that a potent treatment with ACTs plus primaquine (PQ) would eliminate P. vivax in low transmission settings by implementing programs of mass drug administration [41–43]. Nevertheless, P. vivax demonstrated an unstable elimination environment, when compared to P. falciparum [41], since PQ triggers an adverse effect to individuals affected by glucose-6-phosphate-dehydrogenase deficiency (G6PD) questioning mass programs [40, 44]. Previous works also indicated that the early development of gametocytes increases P. vivax incidence [40, 45].
We aim to study the emergence and spread of P. vivax and P. falciparum drug resistance taking into account P. vivax particularities: relapses, earlier transmission, and detection difficulties due to asymptomatic cases. We developed compartmental models for both P. vivax and P. falciparum illustrating the emergence and transmission of one resistant strain on a wild-strain population under the pressure of treatments with CQ and ACTs plus addition or no PQ. We implemented equivalent epidemiological settings for human and mosquito populations to make comparable drug-resistance evolution between Plasmodium species. Our approach reveals the impact of P. vivax particularities in drug resistance filling in the gap of knowledge about P. vivax resistance.
Materials and methods
We developed mathematical models for both Plasmodium vivax and Plasmodium falciparum using ordinary differential equations (ODE) to represent the transmission of two strains: sensitive and resistant. The fundamentals from these models have origin on the well-known Ross-Macdonald model that separates human and mosquito populations by susceptible and infected individuals [46]. Additionally, we implemented a post-treatment state in humans, and we also distinguished infected states by sensitive and resistant strains.
The model structure considers only a single genotype per infected human, either sensitive or resistant. However, multiple malaria parasites with different genotypes might infect humans. Multiple-genotype infections can happen due to genetically distinct sporozoites, either from a single inoculation (co-inoculation) or multiple inoculations (superinfection). The relative importance of co-inoculation versus superinfection is setting dependent and not yet fully understood. Previous studies found that parasite density in blood-stage can limit subsequent development of new sporozoites supporting the parasite population of first-inoculated genotype [47, 48]. Hence, superinfection may be limited. Another study analyzing multiple-genotype infections found multiple parasite haploids with genetic similarity suggesting infection from a single inoculation rather than several inoculations [49]. The model presented here uses a single genotype per infected human for model simplification.
The next subsections expand model features and differences between P. vivax and P. falciparum modeling.
P. falciparum model
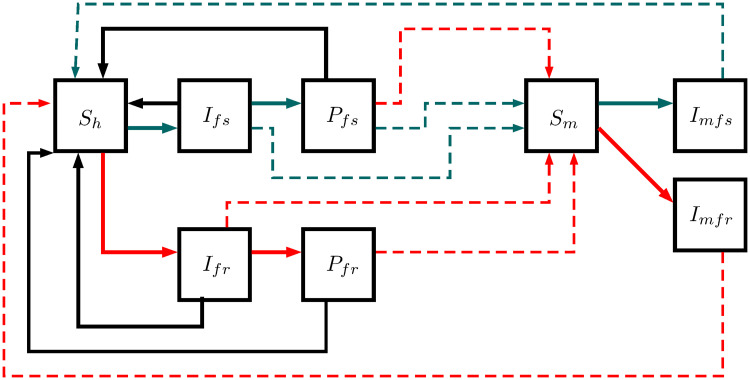
This model outlines P. falciparum transmission in five human and three mosquito states: susceptible humans Sh, infected humans by sensitive strain Ifs, post-treatment humans after sensitive infection Pfs, infected humans by resistant strain Ifr, post-treatment humans after resistant infection Pfr, susceptible mosquitoes Sm, infected mosquitoes by sensitive strain Imfs, and infected mosquitoes by resistant strain Imfr. Infected and post-treatment humans can infect susceptible mosquitoes, and then, they can become susceptible again (see Fig 1). On the other hand, infected mosquitoes remain in this state until their death due to their short life expectancy. The equations from Eqs 1 to 8 represent the measure per state; Table 1 illustrates model parameters.
Fig 1. P. falciparum model.
This structure illustrates the transmission in five human and three mosquito states: susceptible humans Sh, infected humans by sensitive strain Ifs, post-treatment humans after sensitive infection Pfs, infected humans by resistant strain Ifr, post-treatment humans after resistant infection Pfr, susceptible mosquitoes Sm, infected mosquitoes by sensitive strain Imfs, and infected mosquitoes by resistant strain Imfr. Complete lines describe the possible progressions between states, whereas dotted lines describe the parasite transmission between humans and mosquitoes. Red, gray, and black lines display the flows between pairs of states: resistant, sensitive, and recovered states.
Table 1. Model parameters.
| Parameter | Description | Value |
|---|---|---|
| m | Mosquitoes per human Nm/Nh (dimensionless) | 2435/625 [50] |
| a | Biting rate (day−1) | 0.21 [39] |
| b | Transmission probability from an infected mosquito to a susceptible human (dimensionless) | 0.5 [51] |
| η | Treatment coverage (dimensionless) | 0-1 |
| σf | Proportion of symptomatic humans infected by P. falciparum (dimensionless) | 0.9 [52] |
| σv | Proportion of symptomatic humans infected by P. vivax (dimensionless) | 0.33 [53] |
| rf | Recovery rate of untreated infected-humans by P. falciparum (day−1) | 1/287 [50] |
| rv | Recovery rate of untreated infected-humans by P. vivax (day−1) | 1/60 [54] |
| γf | Progression rate from infected to post-treatment humans affected by P. falciparum (day−1) | 1/2 [50] |
| γv | Progression rate from infected to post-treatment humans affected by P. vivax (day−1) | 1/9 [36, 55] |
| φ | Proportion of treated humans with primaquine (dimensionless) | 0-1 |
| κ | Protective period of the treatment (day) | see Table 2 |
| ϵf | Infectious period of post-treatment humans infected by P. falciparum (day) | see Table 2 |
| ϵv | Infectious period of post-treatment humans infected by P. vivax (day) | see Table 2 |
| α | Resistance cost (dimensionless) | 0-0.6 [24] |
| n | Recurrences produced by the resistant strain (dimensionless) | 1 |
| Λm | Mosquito birth rate (day−1) | 0.033 [50] |
| μm | Mosquito death rate (day−1). We assumed constant population | 0.033 |
| ca | Transmission probability from an asymptomatic human to susceptible mosquito (dimensionless) | 0.12 [56] |
| cs | Transmission probability from an infected-symptomatic human to susceptible mosquito (dimensionless) | 0.4 [56] |
| ν | Probability of transmitting a resistant parasite from a post-treatment infected by a sensitive strain (dimensionless) | see Table 2 |
| ψ | Hypnozoite relapse rate (day−1). We assumed tropical relapses | 1/60 [57] |
| ρsr | Probability of developing sensitive infection by the contact between an infected mosquito by sensitive strain and a human with latent parasites of the resistant strain (dimensionless) | 0.5 |
| ρrs | Probability of developing resistant infection by the contact between an infected mosquito by resistant strain and a human with latent parasites of the sensitive strain (dimensionless) | 0.5 |
| ϕt | Probability of post-treatment human of remaining with latent parasites (dimensionless) | 0.21 [58] |
| ϕu | Probability of an untreated-infected human of remaining with latent parasites (dimensionless) | 0.4-0.9 [59] |
| μvl | Clearance rate of latent parasites (hypnozoites) day−1 | 1/425 [39] |
| (1) |
| (2) |
| (3) |
| (4) |
| (5) |
| (6) |
| (7) |
| (8) |
with
P. vivax model
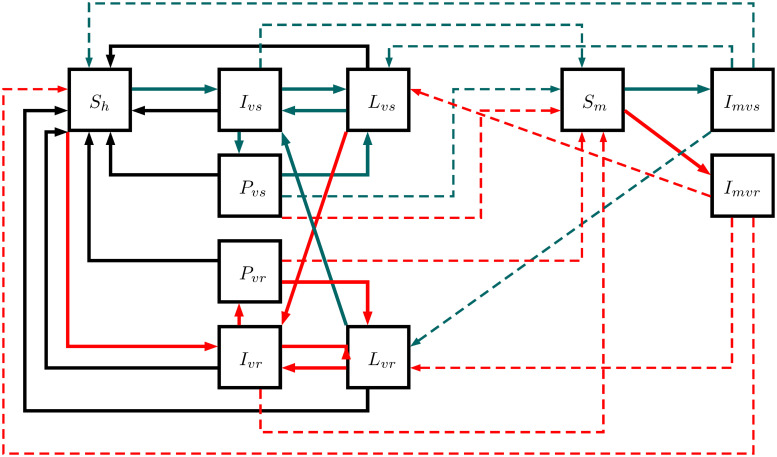
This model outlines P. vivax transmission in seven human and three mosquito states: susceptible humans Sh, infected humans by sensitive strain Ivs, humans with latent parasites of sensitive strain Lvs, post-treatment humans after sensitive infection Pvs, infected humans by resistant strain Ivr, humans with latent parasites of resistant strain Lvr, post-treatment humans after resistant infection Pvr, susceptible mosquitoes Sm, infected mosquitoes by sensitive strain Imvs, and infected mosquitoes by resistant strain Imvr. This model reproduces the same transmission interactions of P. falciparum model but involves two additional states: Lvs and Lvr. These states describe humans with dormant hypnozoites of P. vivax that cause relapses after first infection. In fact, Ivs, Ivr, Pvs and Pvr can remain with latent parasites becoming Lvs or Lvr instead susceptible. Additionally, the model allows new infections in humans with latent parasites as Fig 2 illustrates. The equations are from the Eqs 9 to 18 using the parameters in Table 1.
Fig 2. P. vivax model.
This structure illustrates the transmission in seven human and three mosquito states: susceptible humans Sh, infected humans by sensitive strain Ivs, humans with latent parasites of sensitive strain Lvs, post-treatment humans after sensitive infection Pvs, infected humans by resistant strain Ivr, humans with latent parasites of resistant strain Lvr, post-treatment humans after resistant infection Pvr, susceptible mosquitoes Sm, infected mosquitoes by sensitive strain Imvs, and infected mosquitoes by resistant strain Imvr. Complete lines reproduce the possible progressions between states while dotted lines reproduce the parasite transmission between humans and mosquitoes. Red lines display the flow of resistant parasites, gray lines display the flow of sensitive parasites, and black lines display the flow without parasites.
| (9) |
| (10) |
| (11) |
| (12) |
| (13) |
| (14) |
| (15) |
| (16) |
| (17) |
| (18) |
with
Resistance cost
Resistance cost (α) reduces parasite fitness when a mutation occurs and confers resistance on specific treatment [25]. We modeled this cost as a reduction of resistant strains by a multiplicative factor 1 − α.
Asymptomatic infections
We considered asymptomatic infections taking into account the proportion of infected humans with very low malaria parasite density infections. They act as parasite reservoirs, but their transmission rate is lower than the one of symptomatic humans. In the model, the transmission probabilities from asymptomatic and symptomatic individuals to susceptible mosquitoes occur with different probabilities ca and cs, respectively, considering ca < cs [63]. The number of individuals without symptoms is a consequence of the immunological profile in an endemic region due to previous exposition periods. Also, this number varies with parasite [52]. Hence, we considered (1 − σf) and (1 − σv) as constant proportion of asymptomatic humans infected by P. falciparum and P. vivax assuming a long exposition period before treatment.
Antimalarial treatment
Treatment coverage η varies from 0% to 100% of infected humans, adopting a single-treatment regimen. Additionally, the model also permits evaluation of treatment plus primaquine by applying a proportion φ of treated humans impacting gametocyte transmission and P. vivax hypnozoites.
Infectious period
Infected without available treatment and asymptomatic humans recover from infection at rf and rv rates for P. falciparum and P. vivax, respectively. Thus, 1/rf and 1/rv represent the average infection period, without treatment, for P. falciparum and P. vivax where 1/rf > 1/rv because P. vivax model counts only one infection and it can generate a new P. vivax relapse when infected human Iv becomes human with latent parasites Lv. On the other hand, treated humans advance to post-treatment state at γ rate with 1/γ as infectious period with 1/γv > 1/γf because the early development of gametocytes in P. vivax triggers longer infectious period before treatment than P. falciparum [52, 61]. Resistant parasites provoke recurrences, during treatment, producing more extended infectious periods than infectious periods with sensitive parasites [64]. The mean infectious time for a sensitive strain is 1/γ (infectious period), whereas the mean infectious period of a resistant strain is (n+ 1)/γ, with n recurrences. The factor n+ 1 captures humans infected by resistant parasite extending their infectious periods when a recurrence occurs.
Post-treatment period
The post-treatment period engages three dynamics: infectivity, drug half-life, and the emergence of resistant parasites. Parasite clearance of drugs such as chloroquine and artemisinin components affects differently specific parasite forms, i.e., per species [60, 65]. Infectivity depends on the duration of gametocyte presence on blood. We define ϵ as the infectious period after treatment; ϵ is longer for P. falciparum because P. falciparum gametocytes have a longer lifespan than P. vivax gametocytes (ϵf > ϵv) [36, 65]. Drug half-life κ corresponds to the time interval when treatment remains in the blood conferring a protective period [66]. The emergence of resistant parasites occurs by the selection of parasite strains under residual drug concentration, which occurs with probability ν of transmitting a resistant parasite from a post-treatment infected by a sensitive strain [23].
Basic reproduction number
We derived the basic reproduction number adopting the next generation matrix (NGM) approach proposed in [67–69]. The basic reproduction number represents the number of secondary infections generated from an initial primary case in a susceptible population. We assumed constant populations in humans (Nh) and mosquitoes (Nm) thus Λ m = μ m. NGM method requires finding the disease–free state (Sh = Nh; Sm = Nm; the remaining states equal 0) to linearize the equations and building the transmission and transition matrix to derive the basic reproduction numbers [67].
Simulation
We aim to simulate the spread of drug resistance in P. falciparum and P. vivax comparing between different treatment-regiments. We contrasted regimens between the adoption of four treatment lines: chloroquine (CQ), chloroquine plus primaquine (CQ+PQ), artemisinin-based combination therapy (ACT) with artemether-lumefantrine (ARLU) and ARLU plus PQ (ACT+PQ). The initial condition is only the presence of the sensitive strain, and Table 2 summarizes the parameters to each treatment regiment. We analyze the system of equations in R using deSolve package [70]. The simulation code is provided in S1 File.
Table 2. Treatment parameters.
| Treatment regimen | Protective period (κ) [60] | Infectious period after treatment (ϵ) [36, 60, 61] | Probability of transmitting a resistant parasite from Pfs and Pvs (ν) [62] |
|---|---|---|---|
| CQ | 30 days | 2.1 days (P. vivax), 11 days (P. falciparum) | 10−12 |
| CQ+PQ | 30 days | 2.1 days with (φ = 0.95) | 10−12 |
| ACT (artemether-lumefantrine) | 3 days | 1.55 days (P. vivax), 11 days (P. falciparum) | 10−24 |
| ACT+PQ (artemether-lumefantrine) | 3 days | 1.55 days (φ = 0.95) | 10−24 |
Malaria-transmission settings
We used parameters from the study by Chitnis et al. defining low and high transmission settings for a Ross-McDonald structure [50]. We also incorporated the parameter distinction between symptomatic and asymptomatic infectiousness from [56]. P. falciparum model showed a valid prevalence (between 0.01 and 0.324) according to the third quartile of 32374 prevalence values reported in the Malaria Atlas Project MAP for 98 countries from 1984 to 2018 [71]. MAP generated a dataset of prevalence values using parasite rate points that came from organizations of health surveys and prevalence studies in literature revision [72]. The P. vivax model used the same parameters to make comparable results and also adopted a set parameters to involve hypnozoite relapses [39, 57, 59]. In order to better understand the impact of parameters, we performed a sensitivity analysis to describe the implications of variation in model parameters on the emergence time of resistant strain that represents the moment when resistant-strain prevalence surpasses sensitive-strain prevalence.
Sensitivity analysis
Finally, we performed a sensitivity analysis of parameter models on the emergence-time of the resistant strain using Latin Hypercube Sampling (LHS) to respond at the uncertainty of estimated values and also to assess the parameter influence [73]. We implemented the analysis in R using deSolve, lhs, and sensitivity packages; the partial correlation coefficients of sensitivity function were calculated with a confidence level of 95% [70, 74, 75]. All reproducibility code is in S1 File.
Results
Basic reproduction number
We derived formulae for the basic reproduction number of sensitive and resistant strains in the cases of P. falciparum and P. vivax models (see from Eqs 19 to 22). These derivations reveal that R0, as a function of resistant cost α, cuts down R0 values of resistant strains compared to sensitive ones. As expected, recurrences increase the basic reproduction number in both cases. On the other hand, terms associated with latent P. vivax parasites reduce the basic reproduction number of both strains in the same proportion.
| (19) |
| (20) |
| (21) |
| (22) |
Simulation
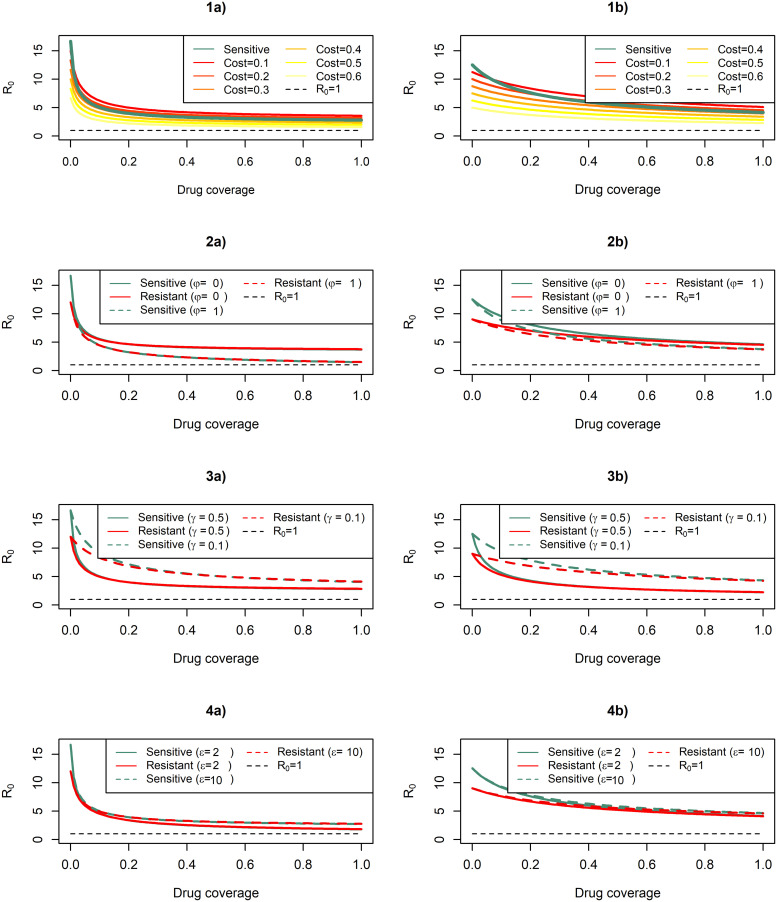
In numerical simulations, we evaluated the basic reproduction number R0 by varying cost resistance, treatment plus primaquine, and infectious time before and after treatment (see Fig 3). In general, increases in drug coverage decrease R0 values of P. falciparum at a higher rate than the ones obtained for P. vivax. Sensitive P. vivax overcomes resistant strains by R0 values at different resistance cost compared to the switch point for P. falciparum. Treatment plus primaquine influences equally R0 values of sensitives and resistant stains for both species. In general, a longer infectious period before and after treatment increases the reproduction number, but only the longer infectious time before treatment boosted the sensitive R0 to stay over the resistant R0. This effect is stronger in P. vivax because it has an early transmission before treatment.
Fig 3. Drug coverage varying the basic reproduction numbers.
The figure illustrates R0 lines for P. falciparum (figures a) and P. vivax (figures b) models dividing by sensitive and resistant strains. 1(a) and 1(b) display R0 lines of sensitive and resistant strains with different resistance cost (α); 2(a) and 2(b) display R0 lines using or non-using primaquine (φ); 3(a) and 3(b) display R0 lines at two infectious periods before treatment in days (1/γ); 4(a) and 4(b) display R0 lines at two infectious periods after treatment in days (ϵ). α = 0.28, ρ = 0.5, ϵf = 11, ϵv = 2.1, γf = 1/2 and γv = 1/9 when they are fixed; other parameters have values from Table 1.
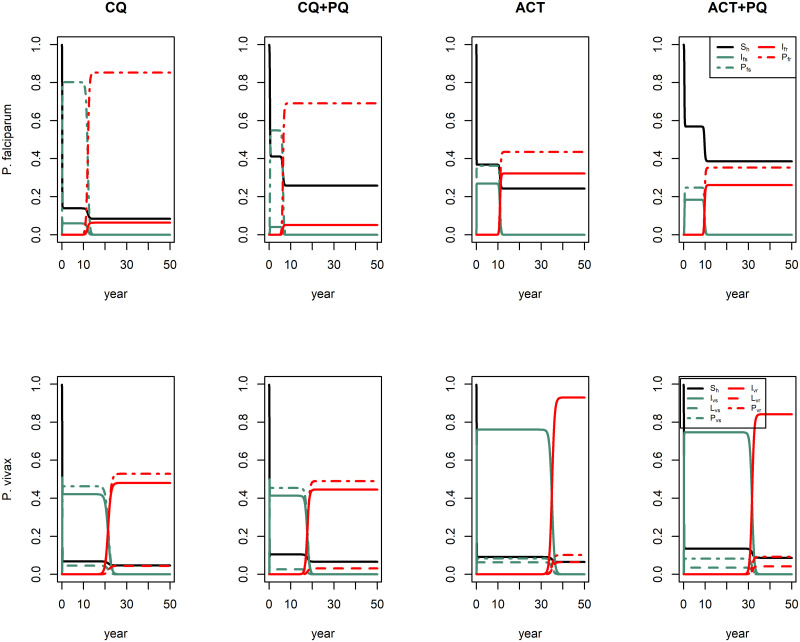
Simulations with no regimen produce a proportion of 0.98 for Ivs in P. falciparum model and 0.93 and 0.06 for Ivs and Lvs, respectively, in P. vivax model implying an equilibrium without resistant strain (see Figure A in S2 File). With this initial conditions, we implemented regimen (η = 1) obtaining a decrease in all infected proportions in comparison with no regimen but resistant strain emerged in all treatments as Fig 4 illustrates.
Fig 4. Simulation of treatment regimens.
This figure illustrates the implementation of four treatment-regimens: chloroquine CQ (κ = 30 days, ϵf = 11 days, ϵv = 2.1 days, φ = 0 and ν = 10−12), chloroquine plus primaquine CQ+PQ (κ = 30 days, ϵf = 11 days, ϵv = 2.1 days, φ = 0.95 and ν = 10−12), artemisinin-based combination therapy ACT (κ = 3 days, ϵf = 11 days, ϵv = 1.55 days, φ = 0 and ν = 10−24) and artemisinin-based combination therapy plus primaquine ACT+PQ (κ = 3 days, ϵf = 11 days, ϵv = 1.55 days, φ = 0.95 and ν = 10−24). First row shows the simulated regimens in P. falciparum model and second row shows the simulated regimens in P. vivax model.
Although emergence time of P. vivax resistant strain was slower than the one of P. falciparum resistant using all regimens, the regimens accomplished a smaller reduction in the proportion of infected humans by P. vivax. Treatment with chloroquine (CQ) contributed to a higher proportion of post-treatment humans, especially in the case of P. falciparum, and the emergence of resistant P. vivax took a time twofold as long as resistant P. falciparum. Treatment including primaquine (CQ+PQ) decreased infected and post-treatment humans of P. falciparum, and humans with latent parasites of P. vivax, but this regimen implied the emergence of resistant parasites in less time.
Regimens with artemisinin-based combination therapy delayed the emergence of resistant P. vivax three times as long as resistant P. falciparum, but this regimen affected the proportion of infected humans less than chloroquine regimen. Primaquine addition (ACT+PQ) also decreased infected and post-treatment humans of P. falciparum, and humans with latent parasites of P. vivax though the emergence of resistant parasites remained at a similar time as the ACT without primaquine.
Sensitivity analysis
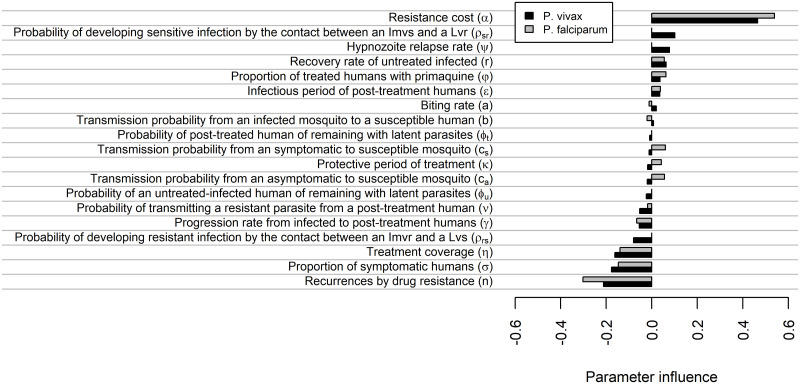
In this model, resistance cost is the most influencing parameter since this parameter delays more the emergence of resistant parasites for either P. vivax or P. falciparum (see Fig 5). Four parameters were also directly proportional but with a low parameter influence: probability of developing sensitive infection by the contact between Imvs and a Lvr ρsr (only in P. vivax), hypnozoite relapse rate ψ (only in P. vivax), recovery rate of untreated infected r and proportion of treated humans with primaquine φ. On the other hand, the number of recurrences by drug resistance obtained the most negative influence for both species implying an earlier emergence of the resistant strain. Five parameters also exhibited a negative relationship: the probability of transmitting a resistant parasite from a post-treatment human ν, progression rate from infected to post-treatment humans γ, probability of developing a resistant infection by the contact between Imvr and a Lvs ρsr (only in P. vivax), the proportion of symptomatic humans and treatment coverage. The remaining parameters impacted less, also noting that the transmission probabilities to susceptible mosquito (cs and ca) and the protective period after treatment κ only exhibited a proportional factor for P. falciparum.
Fig 5. Parameter sensitivity on the emergence-time of the resistant strain.
The figure illustrates parameter influence where -1 represents the maximum inverse relation (accelerate drug resistance), 1 represents the maximum proportional relation (delay drug resistance) and 0 represents no relation.
Discussion
We found that early transmission before treatment, asymptomatic human, and low effectiveness of drug coverage support the prevalence of sensitive parasites delaying the emergence of resistant P. vivax. The reproduction numbers of sensitive P. vivax surpassed the reproduction numbers of resistant ones when the infectious period before treatment was greater, and this usually occurs in P. vivax transmission by the early development of gametocytes [52]. This effect produces an increase in the number of P. vivax infected by a shorter incubation period of parasites as a previous model found [40]. It also implies more difficulties in P. vivax elimination and control than P. falciparum, illustrating the lowest effectiveness of current treatment regimens against P. vivax [45, 76, 77]. Previous models also indicated a lower reduction in P. vivax prevalence in same settings than P. falciparum [39, 41] but actually, P. falciparum prevalence is similar to or greater than P. vivax in the same settings suggesting that host acquisition of P. vivax immunity would play a role modulating P. vivax prevalence [78, 79].
Implications in treatment policy
Chloroquine (CQ) and Artemisinin-based combination therapy (ACT) with artemether-lumefantrine (ARLU) caused emergence of P. falciparum resistance on a similar time scale, whereas ARLU delayed the emergence of P. vivax resistance in comparison with CQ. In theory, resistance development to a set of drugs is less likely than a single drug, and this reinforces the improvement of combination therapies [62]. We capture the fact that resistance is less likely for combination therapy by using a smaller ν for ACT than CQ (Table 2). Nevertheless, our results showed that fast parasite clearance and shorter protective period of ARLU against P. falciparum avoided the transmission of sensitive parasites after-treatment, allowing the emergence period of a resistant parasite as long as the one for CQ despite the lower probability of transmitting resistant parasites with ARLU. CQ resistance in P. vivax emerged earlier than ARLU resistance, but CQ achieved a higher reduction in the prevalence of infected humans in overall simulations. These effects indicate that combination therapy evades drug resistance for a long period in P. vivax, but its shorter protective period than the one for CQ allows a prevalence increase. This result agrees with the substantial increase in P. vivax cases with ACT adoption for all Plasmodium species in Papua New Guinea and Indonesia [80]. Hence, combination therapy delays emergence of drug resistance for a long period for P. vivax than monotherapy, but it should attach a long protective period to prevent an increase in disease incidence. Indeed, dihydroartemisinin-piperaquine (DPQ) regimen, a combination therapy, is highly recommended for malaria control, since it offers a protective period as well as CQ [60]. Still, extensive use of partner drugs as monotherapy such as piperaquine alone, before combination therapy adoption, would intensify risk of resistance [81]. On the other hand, mixed infections of P. falciparum-P. vivax produce a premature exposure of P. vivax at non-adopted drugs forcing an earlier selective pressure as previous works reported [76, 81, 82]. Our simulation only considered an initial sensitive strain infection without taking into account previous resistance profile and several genotypes, with different drug susceptibility and fitness [83], limiting results to a qualitative validation of regimen adoption in a sensitive population of parasites.
Cessations and changes in drug policy have allowed the emergence of wild-type parasites in endemic zones in Africa and Asia, boosting the possibility of adopting well-known regimens as CQ and sulfadoxine-pyrimethamine [84–87]. Our model structure does not have an inverse mutation from resistant to sensitive strain, but basic reproduction numbers have a comparable structure in terms of parasite competence. If we have a treatment cessation (η = 0), R0fr = (1 − α)R0fs and R0vr = (1 − α)R0vs entail R0fs > R0fr and R0vs > R0vr, with α > 0, generating that sensitive prevalence grows up above resistance prevalence and therefore, reemergence of wild-type strain.
Impact of treatment plus primaquine
We also tested treatment regimen plus primaquine (PQ) finding that PQ decreased basic reproduction numbers and prevalence of either sensitive or resistant strains. Still, it had a lower contribution to drug-resistance. For P. falciparum, PQ helped to avoid transmission after treatment decreasing prevalence using CQ+PQ and ARLU+PQ. Still, CQ resistance occurred slightly earlier because PQ also blocked the transmission of sensitive parasites after treatment in a protective period. PQ decreases P. vivax prevalence in humans with latent parasites, but decreases less the prevalence of P. falciparum, suggesting that earlier transmission and asymptomatic individuals have a more important role in P. vivax transmission than transmission after treatment. This finding agrees with a previous study showing that early transmission in P. vivax forced greater reproduction number [45]. This result contrasts with previous studies that found relapses as the most important contributor of P. vivax prevalence instead of early transmission [41, 42]. Nevertheless, our results reinforce the adoption of regimens plus a drug to kill hypnozoites and gametocytes, because regimens plus PQ decreased prevalence, when compared to single-drug regimen. In terms of drug resistance, Schneider and Escalante suggested that a drug to kill gametocytes such as PQ could prevent drug resistance [36]. Our model only avoids all transmission of resistant strain with a 100% of PQ regimen which is implausible, given adverse effects of PQ in patients with G6PD deficiency [14, 88]. Simulation results showed an earlier emergence of drug resistance in treatments plus PQ for both Plasmodium species. In contrast, sensitivity analysis showed low influence in PQ delaying the emergence of the resistant strain. However, such results are still inconclusive due to potential disturbances in Latin hypercube sampling because φ obtained a lower influence. Therefore, our results showed that PQ might not have an essential role in drug resistance over the primary treatment regimen.
P. vivax relapses
Relapses in P. vivax constitute the principal challenge in control and elimination programs and incidence increases with more frequent relapses [39, 40, 42]. Our model structure defined relapses through hypnozoite relapse rate (ψ) and probabilities of remaining with latent parasites (φu and φt). The formula for R0v indicated that the hypnozoite relapse rate ψ has no important effect on the incidence because this term applies by the same factor in numerator and denominator. The compartmental structure of the model does not capture all the nature of relapse with hypnozoite relapse rate (ψ). Nevertheless, probabilities of remaining with latent parasites (φu and φt) help to capture this dynamic, and we found that probabilities φu and φt increased R0v and parasite prevalence, connecting with previous studies that noticed greater R0 with more relapses [39, 41]. Relapses considering drug resistance through sensitivity analysis showed relapse rate as delayer of resistance strain because relapses might benefit the transmission of sensitive parasites before the appearance of the resistant strain. These results suggest that tropical zones support sensitive P. vivax more than temperate zones because a single-sensitive infection might cause more than one sensitive infection episode delaying the emergence of resistant strain [41, 89, 90].
Effect of asymptomatics
The effect of asymptomatic individuals is key because they can support a new transmission way, providing insights into the implication of detection difficulties in P. vivax. Basic reproduction numbers expressions illustrated that proportion of symptomatic humans σ enhanced the real drug coverage ση generating smaller reproduction numbers while asymptomatic proportion (1 − σ) increases them. This result agrees with Adapa et al. presenting asymptomatics as magnifying the number of cases [45]. Simulation results exhibited a greater prevalence of P. vivax (between 40% and 75%) using all regimens in same transmission settings than P. falciparum (between 10% and 25%) and larger asymptomatic proportion in P. vivax ((1 − σv)>(1 − σf)) might explain a part of this greater prevalence. A previous study in the Solomon Islands (low transmission settings) revealed an 82.4% of P. vivax prevalence, among which only 2.9% of infected had fever implying a high impact on the transmission of asymptomatic cases linking with model results [91]. In general terms, current results provided some insights into the contributions of asymptomatic reservoirs, but the model structure has limitations. First, models here consider a fixed proportion of asymptomatic, which may vary between localities and time [92]. To perform model robustness, we performed a sensitivity analysis that illustrated σ as an accelerator of drug resistance with influence for both Plasmodium species. Drug efficacy increases when there is a large proportion of symptomatic humans, boosting the selective force. This result agrees with Kim et al. that found lower sensitive-strain fitness with higher drug efficacy [33]. Second, our model structure considers an average decay rate of infected states for both symptomatic and asymptomatic humans at the same levels. The weight of asymptomatic infection might be more significant than expected. In this case, asymptomatic individuals would have a higher impact on disease prevalence and avoiding drug resistance.
Multiple-genotype infection
The model structure here considers only single genotype infection per infected human, but there is evidence of multiple-genotype infections. Both co-inoculation and superinfection generate multiple genotypes per infected, as reported in endemic zones [93]. Our model does not represent the dynamic of parasite density in blood-stage and the genetic relationship of multiple genotype infections. However, previous studies found that parasite density in blood-stage can limit a subsequent development of new sporozoites [94, 95]. Nkhoma et al. found multiple genotype infections with a genetic relationship suggesting a higher probability of single inoculations rather than multiple ones [96]. In general, within-host models can capture better superinfection and co-inoculation because they consider independent parasite stages and parasite densities [22]. Still, we used a compartment model to provide information on the human-population level.
Model structure only allows a superinfection of humans with latent parasites through a new inoculation or activation of present hypnozoites within an activation period. In the case of activation of present hypnozoites, previous studies offered febrile-systematic episodes as activator [35, 90]. Co-activation of hypnozoites of different strains can happen after co-inoculation, but our model does not represent this dynamic because it remains unlikely. Indeed, our model only considers superinfection in a human with latent parasites mediated by ρsr and ρrs. This kind of dynamics captures the superinfection of newly inoculated parasites or activation of latent hypnozoites, either sensitive or resistant. Sensitivity analysis revealed that the parameter given by the probability ρsr of an individual with latent parasites of the resistant strain to develop a sensitive infection by inoculation from an infected mosquito with sensitive strain delays drug resistance. By contrast, the probability ρrs of a human with latent parasites of sensitive strain to develop resistant infection by mosquito bite with resistant strain accelerates resistance. This result agrees with the study by Klein et al. that shows within-host competition as a factor to delay drug resistance [35]. The present models permit to compare risk factors such as hypnozoite-activation or superinfection of humans in latent state and their implications in drug resistance, despite the limited capacity to deal with multiple-genotype infections.
In summary, our results suggest that P. vivax has a set of mechanisms to delay drug resistance that implies difficulties in control and elimination programs: earlier transmission, a higher proportion of asymptomatic cases, and relapses. However, programs focused only on symptomatic humans may obtain a weak effect against P. vivax prevalence. This strategy is not efficient to block early transmission and asymptomatic reservoirs, despite the strong treatment regimen, longer protective period and an effect killing gametocytes and hypnozoites. Strategies such as mass drug administration impact asymptomatic humans and also avoid earlier transmission, blocking the mechanisms to delay drug resistance of P. vivax, but might increase the risk of drug-resistance.
Supporting information
Code (in R language), parameters and data to reproduce simulation and figures—all figures and model results.
(RMD)
Document generated from code in S1—Code (in R language), parameters and data to reproduce simulation and figures.
(PDF)
Acknowledgments
Authors MA and DV are grateful to Dr. Michael White for providing valuable comments on our work and also to Dr. Otilia Lupi for comments and terminology revisions. DV is a CNPq/Brazil research fellow.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
MA and DV are grateful for support from Program Print-Fiocruz-CAPES, Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES, http://www.capes.gov.br), and Fundação Oswaldo Cruz (Fiocruz, http://www.fiocruz.br), and MA is grateful for the scholarship support from Instituto Oswaldo Cruz (IOC, http://www.ioc.fiocruz.br) in the graduate program. DV has support from Conselho Nacional de Desenvolvimento Científico e Tecnológico (National Council for Scientific and Technological Development - CNPq, http://www.cnpq.br, Ref. 424141/2018-3, 309569/2019-2). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. World Health Organization WHO. World Malaria Report. France: WHO Library Cataloguing-in-Publication Data:2018. [Google Scholar]
- 2.United Nations (UN). Transforming Our World: The 2030 Agenda for Sustainable Development. United Nations, New York, NY: 2015. [Google Scholar]
- 3. World Health Organization WHO. Global report on antimalarial efficacy and drug resistance: 2000-2010. Geneva: Drug Resistance and Containment Unit, Global Malaria Program,World Health Organization; 2010. [Google Scholar]
- 4. Dondorp AM, et al. Artemisinin resistance in Plasmodium falciparum malaria. Engl J Med. 2009. July; 361:455–467. 10.1056/NEJMoa0808859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WorldWide Antimalarial Research Network (WWARN): https://www.wwarn.org/about-us/our-work
- 6.World Health Organization. Italy: Guidelines for the treatment of malaria, Third edition. World Health Organization; 2015.
- 7. Noedl H, et al. Evidence of artemisinin-resistant malaria in western Cambodia. N Engl J Med. 2008. December 11;359(24):2619–20. [DOI] [PubMed] [Google Scholar]
- 8. White Nicholas J. Triple artemisinin-containing combination anti-malarial treatments should be implemented now to delay the emergence of resistance. Malar J. 2019; 18: 339 10.1186/s12936-019-2976-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Leang R, et al. Evidence of Plasmodium falciparum malaria multidrug resistance to artemisinin and piperaquine in western Cambodia: Dihydroartemisinin–piperaquine open label multicenter clinical assessment. Antimicrob Agents Chemother 2015; 59: 4719–4726. 10.1128/AAC.00835-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Carrara VI, et al. Malaria burden and artemisinin resistance in the mobile and migrant population on the Thai-Myanmar border, 1999-2011: An observational study. PLoS Med 2013; 10: e1001398 10.1371/journal.pmed.1001398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Price Ric N, et al. Global extent of chloroquine-resistant Plasmodium vivax: a systematic review and meta-analysis. Lancet Infect Dis. 2014. October;14(10):982–91. 10.1016/S1473-3099(14)70855-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Escalante AA, Cornejo OE, Rojas A, Udhayakumar V, Lal AA. Assessing the effect of natural selection in malaria parasites. Trends Parasitol. 2004. August;20(8):388–95. 10.1016/j.pt.2004.06.002 [DOI] [PubMed] [Google Scholar]
- 13. de Koning-Ward Tania F., Dixon Matthew W.A., Tilley Leann, Gilson Paul R.. Plasmodium species: master renovators of their host cells. Nat Rev Microbiol. 2016. August;14(8):494–507. 10.1038/nrmicro.2016.79 [DOI] [PubMed] [Google Scholar]
- 14. Olliaro PL, Barnwell JW, Barry A, et al. Implications of Plasmodium vivax Biology for Control, Elimination, and Research. Am J Trop Med Hyg. 2016;95(6 Suppl):4–14. 10.4269/ajtmh.16-0160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Payne D. Spread of chloroquine resistance in Plasmodium falciparum. Parasitol Today. 1987. August;3(8):241–6. 10.1016/0169-4758(87)90147-5 [DOI] [PubMed] [Google Scholar]
- 16. Peters W. Resistance in human malaria IV: 4-aminoquinolines and multiple resistance, Chemotherapy and drug resistance in malaria. London Academic Press. 1987; 2:659–786. [Google Scholar]
- 17. Liwang Cui, et al. Antimalarial Drug Resistance: Literature Review and Activities and Findings of the ICEMR Network. Am. J. Trop. Med. Hyg. 2015;93(3):57–68. 10.4269/ajtmh.15-0007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Nsanzabana C, Djalle D, Guérin PJ, Ménard D, González IJ. Tools for surveillance of anti-malarial drug resistance: an assessment of the current landscape. Malar J. 2018;17(1):75 10.1186/s12936-018-2185-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Price RN, Auburn S, Marfurt J, Cheng Q. Phenotypic and genotypic characterisation of drug-resistant Plasmodium vivax. Trends Parasitol. 2012;28(11):522–529. 10.1016/j.pt.2012.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bourgard C, Albrecht L, Kayano ACAV, Sunnerhagen P, Costa FTM. Plasmodium vivax Biology: Insights Provided by Genomics, Transcriptomics and Proteomics. Front Cell Infect Microbiol. 2018;8:34 10.3389/fcimb.2018.00034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Slater Hannah C., Okell Lucy C., Ghani Azra C.. Mathematical Modelling to Guide Drug Development for Malaria Elimination. Trends Parasitol. 2017. March;33(3):175–184. 10.1016/j.pt.2016.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Brock Aleisha R, Gibbs Carole A, Ross Joshua V, Esterman Adrian. The Impact of Antimalarial Use on the Emergence and Transmission of Plasmodium falciparum Resistance: A Scoping Review of Mathematical Models. Trop Med Infect Dis. 2017. October 15;2(4). 10.3390/tropicalmed2040054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Katherine Kay, Hastings Ian M. Measuring windows of selection for anti-malarial drug treatments. Malar J. 2015. July 31;14:292 10.1186/s12936-015-0810-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Klein EY, Smith DL, Boni MF, Laxminarayan R. Clinically immune hosts as a refuge for drug-sensitive malaria parasites. Malar J. 2008. April 25;7:67 10.1186/1475-2875-7-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Huijben Silvie, Chan Brian H.K., Nelson William A., Read Andrew F.. The impact of within-host ecology on the fitness of a drug-resistant parasite. Evol Med Public Health. 2018. June 27;2018(1):127–137. 10.1093/emph/eoy016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Artzy-Randrup Y, Alonso D, Pascual M. Transmission intensity and drug resistance in malaria population dynamics: implications for climate change. PLoS One. 2010. October 26;5(10):e13588 10.1371/journal.pone.0013588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Legros M, Bonhoeffer S. A combined within-host and between-hosts modelling framework for the evolution of resistance to antimalarial drugs. J R Soc Interface. 2016. April; 13(117): 20160148 10.1098/rsif.2016.0148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hamza A.Babiker, Amal A.H.Gadalla, Ranford-Cartwright Lisa C.. The role of asymptomatic P. falciparum parasitaemia in the evolution of antimalarial drug resistance in areas of seasonal transmission. Drug Resist Updat. 2013. Feb-Apr;16(1-2):1–9. 10.1016/j.drup.2013.02.001 [DOI] [PubMed] [Google Scholar]
- 29. Koella JC, Antia R. Epidemiological models for the spread of anti-malarial resistance. Malar J. 2003. February 19;2:3 10.1186/1475-2875-2-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Tchuenche JM, Chiyaka C, Chan D, Matthews A, Mayer G. A mathematical model for antimalarial drug resistance. Math Med Biol. 2011. December;28(4):335–55. 10.1093/imammb/dqq017 [DOI] [PubMed] [Google Scholar]
- 31. Mario Cañón, Hernando Diaz, Andrés Olarte. Mathematical model for the spread of drug resistance in Plasmodium falciparum parasite considering transmission conditions. J Theor Biol. 2017. December 21;435:1–11. 10.1016/j.jtbi.2017.09.001 [DOI] [PubMed] [Google Scholar]
- 32. Nick Scott, et al. Implications of population-level immunity for the emergence of artemisinin-resistant malaria: a mathematical model. Malar J. 2018. August 2;17(1):279 10.1186/s12936-018-2418-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kim Y, Escalante AA, Schneider KA. A population genetic model for the initial spread of partially resistant malaria parasites under anti-malarial combination therapy and weak intrahost competition. PLoS One. 2014;9(7):e101601 10.1371/journal.pone.0101601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Schneider KA, Kim Y. An analytical model for genetic hitchhiking in the evolution of antimalarial drug resistance. Theor Popul Biol. 2010;78(2):93–108. 10.1016/j.tpb.2010.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Klein EY, Smith DL, Laxminarayan R, Levin S. Superinfection and the evolution of resistance to antimalarial drugs. Proc Biol Sci. 2012;279(1743):3834–3842. 10.1098/rspb.2012.1064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Schneider Kristan A, Escalante Ananias A. Fitness components and natural selection: why are there different patterns on the emergence of drug resistance in Plasmodium falciparum and Plasmodium vivax?. Malar J. 2013. January 11;12:15 10.1186/1475-2875-12-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ross A, Koepfli C, Schoepflin S, et al. The Incidence and Differential Seasonal Patterns of Plasmodium vivax Primary Infections and Relapses in a Cohort of Children in Papua New Guinea. PLoS Negl Trop Dis. 2016;10(5):e0004582 10.1371/journal.pntd.0004582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Robinson LJ, Wampfler R, Betuela I, et al. Strategies for understanding and reducing the Plasmodium vivax and Plasmodium ovale hypnozoite reservoir in Papua New Guinean children: a randomised placebo-controlled trial and mathematical model. PLoS Med. 2015;12(10):e1001891 10.1371/journal.pmed.1001891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. White Michael T, et al. Modelling the contribution of the hypnozoite reservoir to Plasmodium vivax transmission. Elife. 2014. November 18;3 10.7554/eLife.04692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Chamchod F, Beier JC. Modeling Plasmodium vivax: relapses, treatment, seasonality, and G6PD deficiency. J Theor Biol. 2013;316:25–34. 10.1016/j.jtbi.2012.08.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Águas R, Ferreira MU, Gomes MG. Modeling the effects of relapse in the transmission dynamics of malaria parasites. J Parasitol Res. 2012;2012:921715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Roy M, Bouma MJ, Ionides EL, Dhiman RC, Pascual M. The potential elimination of Plasmodium vivax malaria by relapse treatment: insights from a transmission model and surveillance data from NW India. PLoS Negl Trop Dis. 2013;7(1):e1979 10.1371/journal.pntd.0001979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Gerardin J, Eckhoff P, Wenger EA. Mass campaigns with antimalarial drugs: a modelling comparison of artemether-lumefantrine and DHA-piperaquine with and without primaquine as tools for malaria control and elimination. BMC Infect Dis. 2015;15:144 10.1186/s12879-015-0887-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Zuber JA, Takala-Harrison S. Multidrug-resistant malaria and the impact of mass drug administration. Infect Drug Resist. 2018;11:299–306. 10.2147/IDR.S123887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Adapa SR, Taylor RA, Wang C, Thomson-Luque R, Johnson LR, Jiang RHY. Plasmodium vivax readiness to transmit: implication for malaria eradication. BMC Syst Biol. 2019;13(1):5 10.1186/s12918-018-0669-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Smith DL, et al. Ross, Macdonald, and a Theory for the Dynamics and Control of Mosquito-Transmitted Pathogens. PLoS Pathog. 2012;8(4):e1002588 10.1371/journal.ppat.1002588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Portugal S. et al. Host-mediated regulation of superinfection in malaria. Nat Med. 2011. 17:732–737. 10.1038/nm.2368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Pinkevych M. et al. Density-dependent blood stage Plasmodium falciparum suppresses malaria super-infection in a malaria holoendemic population. Am J Trop Med Hyg. 2013. November;89(5):850–6. 10.4269/ajtmh.13-0049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Nkhoma S. et al. Close kinship within multiple-genotype malaria parasite infections. Proc Biol sci. 2012; 279(1738):2589–2598. 10.1098/rspb.2012.0113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Chitnis N, Hyman JM, Cushing JM. Determining important parameters in the spread of malaria through the sensitivity analysis of a mathematical model. Bull Math Biol. 2008. July;70(5):1272–96. 10.1007/s11538-008-9299-0 [DOI] [PubMed] [Google Scholar]
- 51. Smith David L., Chris J. Drakeley, Chiyaka Christinah, Hay Simon I. A quantitative analysis of transmission efficiency versus intensity for malaria. Nat Commun. 2010. November 2;1:108 10.1038/ncomms1107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Lindblade Kim A, Laura Steinhardt, Aaron Samuels, Kachur S Patrick, Laurence Slutsker. The silent threat: asymptomatic parasitemia and malaria transmission. Expert Rev Anti Infect Ther. 2013. June;11(6):623–39. 10.1586/eri.13.45 [DOI] [PubMed] [Google Scholar]
- 53. Almeida Anne C. G., et al. High proportions of asymptomatic and submicroscopic Plasmodium vivax infections in a peri-urban area of low transmission in the Brazilian Amazon. Parasit Vectors. 2018. March 20;11(1):194 10.1186/s13071-018-2787-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Collins WE, Jeffery GM, Roberts JM. A retrospective examination of anemia during infection of humans with Plasmodium vivax. Am J Trop Med Hyg. 2003. April;68(4):410–2. 10.4269/ajtmh.2003.68.410 [DOI] [PubMed] [Google Scholar]
- 55. M. Nacher, et al. Comparison of artesunate and chloroquine activities against Plasmodium vivax gametocytes. Antimicrob Agents Chemother. 2004. July;48(7):2751–2. 10.1128/AAC.48.7.2751-2752.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Jamie T. Griffin, et al. Reducing Plasmodium falciparum Malaria Transmission in Africa: A Model-Based Evaluation of Intervention Strategies. PLoS Med. 2010. August 10;7(8). pii: e1000324 10.1371/journal.pmed.1000324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Olivia Prosper, Maia Martcheva. Impact of enhanced malaria control on the competition between Plasmodium falciparum and Plasmodium vivax in India. Math Biosci. 2013. March;242(1):33–50. 10.1016/j.mbs.2012.11.015 [DOI] [PubMed] [Google Scholar]
- 58. T. Adak, V.P. Sharma, V.S. Orlov. Studies on the Plasmodium vivax relapse pattern in Delhi, India. Am J Trop Med Hyg. 1998. July;59(1):175–9. 10.4269/ajtmh.1998.59.175 [DOI] [PubMed] [Google Scholar]
- 59. White Michael T. Variation in relapse frequency and the transmission potential of Plasmodium vivax malaria. Proc Biol Sci. 2016. March 30;283(1827):20160048 10.1098/rspb.2016.0048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Douglas NM, Anstey NM, Angus BJ, Nosten F, Price RN. Artemisinin combination therapy for vivax malaria. Lancet Infect Dis. 2010. June;10(6):405–16. 10.1016/S1473-3099(10)70079-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. White NJ Malaria parasite clearance. Malar J. 2017. February 23;16(1):88 10.1186/s12936-017-1731-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Nicholas J. White. Antimalarial drug resistance. J Clin Invest. 2004. April 15; 113(8): 1084–1092. 10.1172/JCI21682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Keillen M. Martins-Campos, et al. Infection of Anopheles aquasalis from symptomatic and asymptomatic Plasmodium vivax infections in Manaus, western Brazilian Amazon. Parasit Vectors. 2018. May 4;11(1):288 10.1186/s13071-018-2749-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.World Health Organization WHO. Methods for Surveillance of antimalarial drug efficacy. France: Global malaria programme, World Health Organization.;2009.
- 65. Bousema T, Drakeley C. Epidemiology and infectivity of Plasmodium falciparum and Plasmodium vivax gametocytes in relation to malaria control and elimination. Clin Microbiol Rev. 2011. April;24(2):377–410. 10.1128/CMR.00051-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Castelli Francesco, Odolini Silvia, Autino Beatrice, Foca Emanuele, Russo Rosario. Malaria Prophylaxis: A Comprehensive Review. Pharmaceuticals (Basel). 2010. October; 3(10): 3212–3239. 10.3390/ph3103212 [DOI] [Google Scholar]
- 67. O. Diekmann, J. A. P. Heesterbeek, M. G. Roberts. The construction of next-generation matrices for compartmental epidemic models.J R Soc Interface. 2010. June 6; 7(47): 873–885. 10.1098/rsif.2009.0386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Diekmann O., Heesterbeek J.A.P., Metz J.A.J. On the definition and the computation of the basic reproduction ratio R0 in models for infectious diseases in heterogeneous populations. J. Math. Biol. 1990; 28(4): 365–382. [DOI] [PubMed] [Google Scholar]
- 69. van den Driessche P., Watmough James. Reproduction numbers and sub-threshold endemic equilibria for compartmental models of disease transmission. Math Biosci. 2002. Nov-Dec;180:29–48. 10.1016/S0025-5564(02)00108-6 [DOI] [PubMed] [Google Scholar]
- 70.Karline Soetaert, Thomas Petzoldt, R. Woodrow Setzer, Peter N. Brown, George D. Byrne, et al. deSolve: Solvers for Initial Value Problems of Differential Equations (’ODE’,’DAE’,’DDE’). R package version 1.21. 2018.
- 71.The Malaria Atlas Project (MAP): https://map.ox.ac.uk/.
- 72. Guerra CA, Hay SI, Lucioparedes LS, et al. Assembling a global database of malaria parasite prevalence for the Malaria Atlas Project. Malar J. 2007;6:17 10.1186/1475-2875-6-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Mckay M. D., Beckman R. J., Conover W. J.. A Comparison of Three Methods for Selecting Values of Input Variables in the Analysis of Output from a Computer Code. Technometrics. 1979. May; 21(2):239–245. [Google Scholar]
- 74.Carnell R. lhs: Latin Hypercube Samples. R package version 1.0.1. 2019
- 75.Bertrand Iooss, Alexandre Janon and Gilles Pujol, with contributions from Baptiste Broto, Khalid Boumhaout, Sebastien Da Veiga, et al. sensitivity: Global Sensitivity Analysis of Model Outputs. R package version 1.16.2. 2019.
- 76. Barnadas C, Timinao L, Javati S, et al. Significant geographical differences in prevalence of mutations associated with Plasmodium falciparum and Plasmodium vivax drug resistance in two regions from Papua New Guinea. Malar J. 2015;14:399 10.1186/s12936-015-0879-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Liwang Cui, Sungano Mharakurwa, Daouda Ndiaye, Pradipsinh K. Rathod, Philip J. Rosenthal. Antimalarial Drug Resistance: Literature Review and Activities and Findings of the ICEMR Network. Am J Trop Med Hyg. 2015. September 2; 93(3 Suppl): 57–68. 10.4269/ajtmh.15-0007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Koepfli C, Colborn KL, Kiniboro B, Lin E, Speed TP, Siba PM, Felger I, Mueller I. A high force of Plasmodium vivax blood-stage infection drives the rapid acquisition of immunity in Papua New Guinean children. PLOS Neglected Tropical Diseases. 2013;7:e2403 10.1371/journal.pntd.0002403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Mueller I, Galinski MR, Tsuboi T, Arevalo-Herrera M, Collins WE, King CL. Natural acquisition of immunity to Plasmodium vivax: epidemiological observations and potential targets. Advances in Parasitology. 2013;81:77–131. 10.1016/B978-0-12-407826-0.00003-5 [DOI] [PubMed] [Google Scholar]
- 80. Kenangalem Enny, et al. Malaria morbidity and mortality following introduction of a universal policy of artemisinin-based treatment for malaria in Papua, Indonesia: A longitudinal surveillance study. PLoS Med. 2019. May; 16(5): e1002815 10.1371/journal.pmed.1002815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Chaorattanakawee S, Lon C, Chann S, et al. Measuring ex vivo drug susceptibility in Plasmodium vivax isolates from Cambodia. Malar J. 2017;16(1):392 10.1186/s12936-017-2034-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Khim N, Andrianaranjaka V, Popovici J, et al. Effects of mefloquine use on Plasmodium vivax multidrug resistance. Emerg Infect Dis. 2014;20(10):1637–1644. 10.3201/eid2010.140411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Cui L, Mharakurwa S, Ndiaye D, Rathod PK, Rosenthal PJ. Antimalarial Drug Resistance: Literature Review and Activities and Findings of the ICEMR Network. Am J Trop Med Hyg. 2015;93(3 Suppl):57–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Kublin James G, Cortese Joseph F, Njunju Eric Mbindo, Mukadam Rabia A G., et al. Reemergence of Chloroquine-Sensitive Plasmodium falciparum Malaria after Cessation of Chloroquine Use in Malawi. The Journal of Infectious Diseases. 2003;187(12):1870–1875. 10.1086/375419 [DOI] [PubMed] [Google Scholar]
- 85. Sekihara M, Tachibana SI, Yamauchi M, et al. Lack of significant recovery of chloroquine sensitivity in Plasmodium falciparum parasites following discontinuance of chloroquine use in Papua New Guinea. Malar J. 2018;17(1):434 10.1186/s12936-018-2585-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Lu F, Zhang M, Culleton RL, et al. Return of chloroquine sensitivity to Africa? Surveillance of African Plasmodium falciparum chloroquine resistance through malaria imported to China. Parasit Vectors. 2017;10(1):355 10.1186/s13071-017-2298-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Moyeh MN, Njimoh DL, Evehe MS, et al. Effects of Drug Policy Changes on Evolution of Molecular Markers of Plasmodium falciparum Resistance to Chloroquine, Amodiaquine, and Sulphadoxine-Pyrimethamine in the South West Region of Cameroon. Malar Res Treat. 2018;2018:7071383 10.1155/2018/7071383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. World Health Organization Evidence Review Group Meeting Report. Mass Drug Administration, Mass Screening and Treatment and Focal Screening and Treatment for Malaria. Geneva: World Health Organization; 2015. [Google Scholar]
- 89. Battle KE, Karhunen MS, Bhatt S, et al. Geographical variation in Plasmodium vivax relapse. Malar J. 2014;13:144 10.1186/1475-2875-13-144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. White NJ. Determinants of relapse periodicity in Plasmodium vivax malaria. Malar J. 2011;10:297 10.1186/1475-2875-10-297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Harris I, Sharrock WW, Bain LM, et al. A large proportion of asymptomatic Plasmodium infections with low and sub-microscopic parasite densities in the low transmission setting of Temotu Province, Solomon Islands: challenges for malaria diagnostics in an elimination setting. Malar J. 2010;9:254 10.1186/1475-2875-9-254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Ouédraogo M, Samadoulougou S, Rouamba T, et al. Spatial distribution and determinants of asymptomatic malaria risk among children under 5 years in 24 districts in Burkina Faso. Malar J. 2018;17(1):460 10.1186/s12936-018-2606-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Anderson TJ, Haubold B, Williams JT, Estrada-Franco JG, et al. Microsatellite markers reveal a spectrum of population structures in the malaria parasite Plasmodium falciparum. Mol Biol Evol. 2000. October;17(10):1467–82. 10.1093/oxfordjournals.molbev.a026247 [DOI] [PubMed] [Google Scholar]
- 94. Portugal S, Carret C, Recker M, et al. Host-mediated regulation of superinfection in malaria. Nat Med. 2011;17(6):732–737. 10.1038/nm.2368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Pinkevych M, Petravic J, Chelimo K, et al. Density-dependent blood stage Plasmodium falciparum suppresses malaria super-infection in a malaria holoendemic population. Am J Trop Med Hyg. 2013;89(5):850–856. 10.4269/ajtmh.13-0049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Standwell C. Nkhoma, Shalini Nair, Ian H. Cheeseman, et al. Close kinship within multiple-genotype malaria parasite infections. Proc Biol Sci. 2012. July 7; 279(1738): 2589–2598. 10.1098/rspb.2012.0113 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Code (in R language), parameters and data to reproduce simulation and figures—all figures and model results.
(RMD)
Document generated from code in S1—Code (in R language), parameters and data to reproduce simulation and figures.
(PDF)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.