BACKGROUND
The ongoing pandemic of COVID-19 has become a focus of global research as many characteristics of this virus are still being defined.1 The most common symptoms currently associated with COVID-19 include fever, cough, and fatigue.2 Rhabdomyolysis is rarely seen and was only reported in 0.2% of patients in a study of 1099 patients in China.2
Common etiologies of rhabdomyolysis include trauma, strenuous exercise, prolonged immobilization, seizure, and toxins, including illicit substances such as cocaine, alcohol, and drugs including statins.3–5 Other viral infections including influenza A and other coronaviruses such as SARS have been associated with rhabdomyolysis.6,7 One case report from China describes SARS-CoV-2-associated rhabdomyolysis; however, in that case report, kidney function remained normal and rhabdomyolysis was not the presenting concern.8 Here, we present a case of severe rhabdomyolysis leading to acute kidney injury (AKI) as the primary presenting feature of COVID-19.
CASE REPORT
A 51-year-old man with a history notable for hypertension, recent diagnosis of non-insulin-dependent diabetes mellitus type 2 (HgbA1c of 7.6%), obstructive sleep apnea, and chronic kidney disease stage 2 presented to the emergency department with a chief concern of 2 days of diffuse myalgias including his chest, back, arms, and legs. The patient exercised regularly at the gym 5 days a week and primarily performed resistance exercises. Due to his general malaise, he had not gone to the gym for 1 week prior to presentation. He described his presenting myalgias as similar in quality to muscle soreness from exercise but much more severe. Ultimately, he presented to care because his pain had become intolerable.
He also described a slight dry cough and mild chills but no fevers. He denied any shortness of breath or sore throat. He had no recent trauma or immobilization. He denied any new medications or diet, weight loss, or exercise supplements. He did not have any recent alcohol intake or use of illicit substances including cocaine or amphetamines. He had no recent travel or sick contacts. He did not have any family history of rhabdomyolysis, other muscle or metabolic disorders, kidney disease, reactions to anesthesia, or thyroid disease.
In the emergency department, the patient had a fever of 103 °F, tachypnea with respiratory rates initially in the 20s–30s, and cough. He was saturating well on room air when awake but required 4 L of oxygen while asleep given his sleep apnea. Exam was notable for a lack of respiratory distress with lungs clear to auscultation and the patient able to speak in full sentences. All muscle compartments were soft and nontender; no muscular weakness was noted. Physical exam was overall unremarkable. Laboratory abnormalities included the following: positive SARS-CoV-2 RT-PCR on initial nasopharyngeal swab, WBC of 3.8 K/μL (reference 4.00–10.00 K/μL) with 16.8% lymphocytes (reference 18–41%) and absolute lymphocyte count of 0.64 K/μL (reference 0.72–4.10 K/μL), BUN 32 mg/dL (reference 6–23 mg/dL), creatinine 2.48 mg/dL with a baseline of 1.3 (reference 0.50–1.2 mg/dL), AST 715 U/L (reference 10–50 U/L), ALT 122 U/L (reference 10–50 U/L), troponin T-hs Gen5 110 ng/L (reference 0–14 ng/L), procalcitonin 0.57 ng/mL (reference 0.00–0.08 ng/mL), CRP 64.4 mg/L (reference 0.0–3.0 mg/L), LDH greater than 2150 U/L, the limit of the assay (reference 135–225 U/L), and creatine kinase (CK) 339,500 U/L(reference 39–308 U/L). Urinalysis was notable for 3+ blood and 2+ protein. Urine sediment was notable for 1 RBC, 6 WBCs, and granular casts. He did not have electrolyte derangements at presentation. Chest X-ray was notable for ill-defined left basilar opacities read as possibly representing atelectasis. The patient’s most recent TSH in 2017 and his TSH during admission were within normal limits.
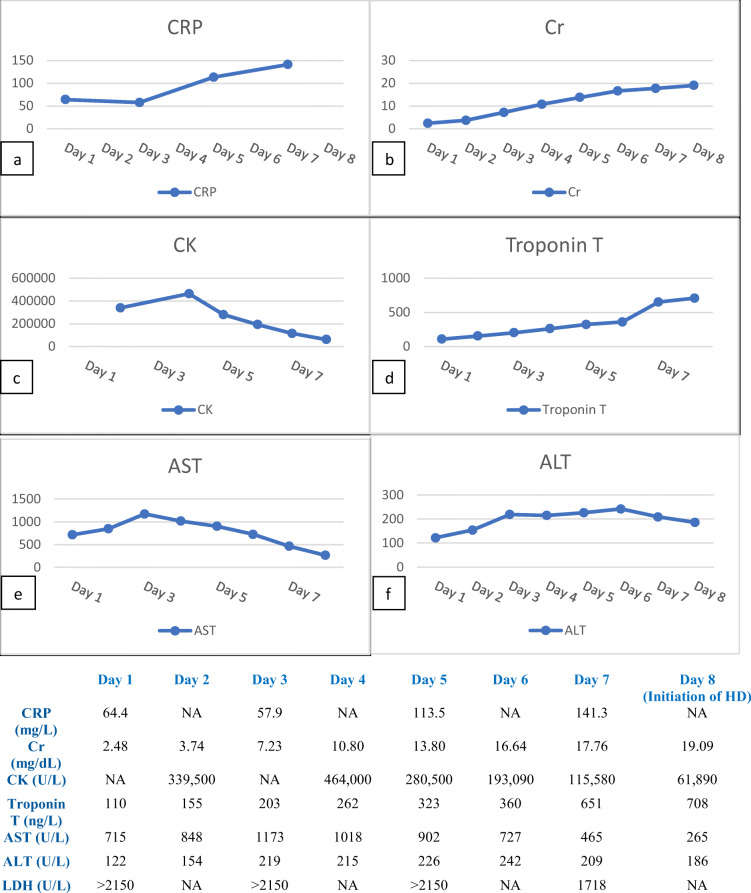
The patient’s laboratory abnormalities were thought to primarily be secondary to COVID-19. His kidney injury was presumed due to his SARS-CoV-2 infection driven rhabdomyolysis, as careful history and physical identified no other etiologies of rhabdomyolysis. Peak serum myoglobin of 15,175 mg/L (reference 0.0–71.0 mg/L) occurred on day 5, and peak urine myoglobin of > 5000 mcg/L also occurred on day 5 (greater than assay, reference ≤ 21 mcg/L). An aldolase level of 39.4 U/L (reference < 7.7 U/L) was seen on day 7 (Fig. 1).
Figure 1.
Laboratory values during the first 8 days of admission prior to hemodialysis. CRP, C-reactive protein; Cr, serum creatinine; CK, serum creatine kinase; Troponin T, 5th-generation (high-sensitivity) cardiac troponin T; AST, aspartate aminotransferase; ALT alanine aminotransferase; LDH, lactate dehydrogenase.
While there were no proven treatments for COVID-19 at the time of the patient’s hospitalization, our treatment teams considered several of the most commonly utilized experimental therapies at our institution including remdesivir, hydroxychloroquine, and tocilizumab as possible treatments for this patient’s COVID-19 disease. Given his profound kidney impairment and markedly elevated AST and ALT, the risks of treatment were felt to outweigh the uncertain benefit of these experimental therapies. Additionally, the patient’s clinical picture was not consistent with cytokine storm, offering another reason to defer tocilizumab.
The patient initially received standard therapy for rhabdomyolysis with aggressive intravenous fluids on the first 2 days of admission. However, as the patient became increasingly oliguric producing only 180 mL of total urine output over the 2nd day of admission, intravenous fluids were discontinued, and a diuretic challenge was initiated given concern for evolving volume overload. This consisted of intravenous chlorothiazide and furosemide, and this regimen was slowly decreased until the patient was urinating spontaneously on day 8 of admission. To prevent severe electrolyte derangements necessitating urgent dialysis, the patient intermittently received aluminum hydroxide, sevelamer carbonate, calcium acetate, and sodium zirconium cyclosilicate. Additionally, his bicarbonate dropped to a nadir of 14 mmol/L on day 3 of admission. In order to treat the acidosis, the patient was given a bicarbonate infusion and then transitioned to oral bicarbonate. Despite these interventions, the patient ultimately required initiation of hemodialysis on day 8 given worsening mental status, primarily somnolence, secondary to uremia. Troponin T-hs continued to rise during hospitalization to a peak of 708 ng/L on day 8. Serial EKGs demonstrated no evidence of ST elevations concerning for myopericarditis. The troponin elevation was hypothesized to most likely be secondary to his significantly elevated CK levels given the cross-reactivity between CK and 5th-generation high-sensitivity troponin T.9
After initiating intermittent hemodialysis, the patient’s laboratory abnormalities began to improve as early as the next day. On day 9, the patient’s creatinine was 15.95, and all inflammatory markers including troponin were down trending. The patient was ultimately discharged on day 15 following placement of a tunneled dialysis catheter for ongoing outpatient dialysis.
DISCUSSION
To our knowledge, this is one of the first cases of SARS-CoV-2 infection presenting with severe rhabdomyolysis requiring dialysis to be reported, as well as one of the first case reports of COVID-19-associated rhabdomyolysis outside of China. Many viral infections, including infections caused by the SARS-CoV-2 virus, can present with nonspecific myalgias that may be severe. This case illustrates that myalgias in COVID-19 disease can represent frank rhabdomyolysis. It is important that clinicians are aware of this potential manifestation of COVID-19 disease, as prompt diagnosis and management of rhabdomyolysis with volume administration can prevent severe and, occasionally, permanent kidney injury.10 This is of particular note given that it is in contrast to the conservative fluid management strategy otherwise currently being recommended for management of COVID-19.11 Prompt management of rhabdomyolysis and preservation of kidney function are of additional importance given that several experimental treatments proposed for COVID-19 such as remdesivir and hydroxychloroquine are contraindicated in severe kidney failure,12 and severe kidney failure status in this patient prevented utilization of such experimental therapies.
The pathogenesis of rhabdomyolysis in infection with SARS-CoV-2 is unclear. Possible mechanisms may include direct muscle invasion by SARS-CoV-2 versus oversized immunologic response to the virus causing collateral muscle damage.
While frank rhabdomyolysis may be rare, elevated CK levels were identified in 13.7% of patients2 in one large cohort of COVID-19 disease from China, suggesting some component of muscle injury may be relatively common. Additionally, evidence of myocardial injury is being frequently reported in COVID-19 patients and may represent a common underlying mechanism.13,14
In contrast to rhabdomyolysis, acute kidney injury appears to be common in patients with COVID-19. In studies of 1099 and 278 patients infected with SARS-CoV-2 in China, between 0.5 and 4% of patients had acute kidney injury.2,15 Acute kidney injury increases morbidity and likely mortality of these patients.16 Furthermore, the requirement of renal replacement therapy (RRT) complicates management, particularly in settings where resources (dialysis machines and staff) may be limited. It is important to exclude reversible and/or treatable causes of AKI early in order to prevent the need for RRT.
We hypothesized that kidney injury in this case was due to heme pigment-associated acute tubular necrosis from SARS-CoV-2 infection driven rhabdomyolysis. While it is possible that there was a component of direct cellular injury from the virus via ACE2 in kidney cells, this is speculative.17 There has been recent work showing renal tropism of SARS-CoV-2 as well as the enrichment of the RNA of genes in multiple kidney cell types hypothesized to facilitate SARS-CoV-2 infection including ACE2, transmembrane serine protease 2 (TMPRSS2), and cathepsin L (CTSL).18 Viral RNA has also been recovered from urine samples in several studies.19–21 It is unclear whether one of several proposed therapies for COVID-19 would have proven beneficial in either reducing the duration of illness or severity of rhabdomyolysis. However, once our patient had established acute tubular necrosis (ATN) from heme pigment exposure, it is unlikely that treatment of the viral infection with specific therapies would have changed the course of his kidney injury or prevented the need for hemodialysis. Given his high creatinine kinase and oliguria on presentation, it is likely this patient already had acute tubular necrosis on presentation. It remains to be demonstrated whether proposed therapies for COVID-19 affect kidney recovery and the need for RRT.
This case additionally highlights the care needed in interpreting laboratory perturbations in COVID-19. While myocarditis and pericarditis have been reported as potential manifestations of SARS-CoV-2 infection, here, we identify a patient with multiple elevated inflammatory markers and rising troponin that was ultimately deemed most likely to be secondary to cross-reactivity between severely elevated CK levels and the 5th-generation high-sensitivity troponin assay.22,23 Highlighting this occurrence may be helpful in assessing other patients with SARS-CoV-2 infection and simultaneously elevated CK and troponin levels.
In conclusion, this case suggests that severe rhabdomyolysis can be the presenting symptom of SARS-CoV-2 infection. In a study of clinical features of patients in Wuhan, China, 44% of patients were noted to present with myalgias.24 Given that myalgias can be an early presenting symptom of rhabdomyolysis, rhabdomyolysis should be suspected in patients who present with severe myalgias. We suggest measuring serum creatinine kinase early in such patients. In addition, caution may be advisable when considering myocarditis or pericarditis in the setting of elevated CK levels in SARS-CoV-2-infected patients.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Authorship
All authors had full access to all of the medical data pertaining to the reported paper and take responsibility for the integrity and the accuracy of the data report and literature review.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization. Coronavirus disease 2019 (COVID-19): situation report, 59. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200319-sitrep-59-covid-19.pdf?sfvrsn=c3dcdef9_2 accessed on 31 May, 2020
- 2.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DS, Du B. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020. [DOI] [PMC free article] [PubMed]
- 3.Huerta-Alardín AL, Varon J, Marik PE. Bench-to-bedside review: Rhabdomyolysis–an overview for clinicians. Crit Care. 2004;9(2):158. doi: 10.1186/cc2978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Melli G, Chaudhry V, Cornblath DR. Rhabdomyolysis: an evaluation of 475 hospitalized patients. Medicine. 2005;84(6):377–85. doi: 10.1097/01.md.0000188565.48918.41. [DOI] [PubMed] [Google Scholar]
- 5.McMahon GM, Zeng X, Waikar SS. A risk prediction score for kidney failure or mortality in rhabdomyolysis. JAMA Intern Med. 2013;173(19):1821–7. doi: 10.1001/jamainternmed.2013.9774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cabeça TK, Bellei N. Human coronavirus NL-63 infection in a Brazilian patient suspected of H1N1 2009 influenza infection: description of a fatal case. J Clin Virol. 2012;53(1):82–4. doi: 10.1016/j.jcv.2011.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen LL, Hsu CW, Tian YC, et al. Rhabdomyolysis associated with acute renal failure in patients with severe acute respiratory syndrome. Int J Clin Pract. 2005;59(10):1162–6. doi: 10.1111/j.1368-5031.2005.00540.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jin M, Tong Q. Rhabdomyolysis as Potential Late Complication Associated with COVID-19. Emerg Infect Dis. 2020;26(7). [DOI] [PMC free article] [PubMed]
- 9.Westermann D, Neumann JT, Sörensen NA, Blankenberg S. High-sensitivity assays for troponin in patients with cardiac disease. Nat Rev Cardiol. 2017;14(8):472. doi: 10.1038/nrcardio.2017.48. [DOI] [PubMed] [Google Scholar]
- 10.Ron D, Taitelman U, Michaelson M, Bar-Joseph G, Bursztein S, Better OS. Prevention of acute renal failure in traumatic rhabdomyolysis. Arch Intern Med. 1984;144(2):277–80. doi: 10.1001/archinte.1984.00350140077012. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization. Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected: Interim guidance V 1.2. https://www.who.int/publications-detail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected accessed on 9 April, 2020.
- 12.Sise ME, Baggett MV, Shepard JO, Stevens JS, Rhee EP. Case 17-2020: A 68-Year-Old Man with Covid-19 and Acute Kidney Injury. N Engl J Med. 2020; doi:10.1056/NEJMcpc2002418. [DOI] [PMC free article] [PubMed]
- 13.Lippi G, Lavie CJ, Sanchis-Gomar F. Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): Evidence from a meta-analysis. Prog Cardiovasc Dis. 2020. [DOI] [PMC free article] [PubMed]
- 14.Clerkin KJ, Fried JA, Raikhelkar J, Sayer G, Griffin JM, Masoumi A, Jain SS, Burkhoff D, Kumaraiah D, Rabbani L, Schwartz A, Uriel N. Coronavirus Disease 2019 (COVID-19) and Cardiovascular Disease. 2020. [DOI] [PubMed]
- 15.Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and corona virus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. 2020:105924. [DOI] [PMC free article] [PubMed]
- 16.Cheng Y, Luo R, Wang K, Zhang M, Wang Z, Dong L, Li J, Yao Y, Ge S, Xu G. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020. [DOI] [PMC free article] [PubMed]
- 17.Fan C, Li K, Ding Y, Lu WL, Wang J. ACE2 expression in kidney and testis may cause kidney and testis damage after 2019-nCoV infection. medRxiv. 2020. [DOI] [PMC free article] [PubMed]
- 18.Puelles VG, Lütgehetmann M, Lindenmeyer MT, Sperhake JP, Wong MN, Allweiss L, Chilla S, Heinemann A, Wanner N, Liu S, Braun F, Lu S, Pfefferle S, Schröder AS, Edler C, Gross O, Glatzel M, Wichmann D, Wiech T, Kluge S, Pueschel K, Aepfelbacher M, Huber TB. Multiorgan and Renal Tropism of SARS-CoV-2. N Engl J Med. 2020; doi:10.1056/NEJMc2011400. [DOI] [PMC free article] [PubMed]
- 19.Wang W, Xu Y, Gao R, Lu R, Han K, Wu G, Tan W. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020. [DOI] [PMC free article] [PubMed]
- 20.Peng L, Liu J, Xu W, Luo Q, Deng K, Lin B, Gao Z. 2019 Novel Coronavirus can be detected in urine, blood, anal swabs and oropharyngeal swabs samples. medRxiv. 2020. [DOI] [PMC free article] [PubMed]
- 21.To KKW, Tsang OTY, Leung WS, Tam AR, Wu TC, Lung DC, Yip CCY, Cai JP, Chan JMC, Chik TSH, Lau DPL. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study. Lancet Infect Dis. 2020. [DOI] [PMC free article] [PubMed]
- 22.Hu H, Ma F, Wei X, Fang Y. Coronavirus fulminant myocarditis saved with glucocorticoid and human immunoglobulin. Eur Heart J. 2020. [DOI] [PMC free article] [PubMed]
- 23.Inciardi RM, Lupi L, Zaccone G, Italia L, Raffo M, Tomasoni D, Cani DS, Cerini M, Farina D, Gavazzi E, Maroldi R. Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020. [DOI] [PMC free article] [PubMed]
- 24.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]