Abstract
The COVID-19 pandemic has had an unprecedented impact on the delivery of healthcare services around the globe. This has resulted in important loss of life for our communities, including health professionals that have been exposed to the disease in their workplace. A human factors approach to the recent changes introduced due to the pandemic can help identify how we can minimize the impact of human error in these circumstances. We hereby present a case study illustrating the application of human factors in the difficult times we are going through at present.
Level of Evidence V This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Keywords: Human factors, Pandemic, COVID-19, Plastic surgery
The COVID-19 pandemic has been a major disruptor for health services worldwide, including plastic surgery [1]. During this period, a series of adaptations have been introduced to maintain the safe delivery of urgent operations. However, the consequences of increased pressure on healthcare staff from a well-being point of view are still unknown.
Exhaustion and stress are well documented contributing factors for medical errors. As surgical services go back to pre-pandemic caseload levels, a human factors approach can be particularly useful to mitigate a “second wave” of mistakes related to pre-operative care.
A patient that had previously undergone a breast reduction presented to our service with a postoperative infection that required admission for intravenous antibiotics. Surgical debridement and lavage was performed, with tissue samples sent for microbiology cultures. Unfortunately, specimens were mislabeled with the details of a different patient. Two days later, the mistake was identified, and no harm was caused.
An investigation identified that a junior nurse, who had recently joined the team, mistakenly used a sticker with a different patient’s details to label the specimen pot. It came to light that this nurse had worked several extra shifts to cover for colleagues quarantined during the pandemic. The correct samples were analysed in due course and our patient received adequate treatment making a full recovery. Albeit, her hospital stay may well have been prolonged by this incident.
Human factors as the discipline that studies interactions between humans and their working system can help to identify and prevent human errors that could derive from stress related to the pandemic [2]. Health care, as a complex human activity, is prone to errors. The contributing role of human factors in this situation is to improve the understanding of causative factors within the interactions between practitioners, devices, physical environment, characteristics of the organization, and wider disruptors such as the COVID-19 pandemic. This allows learning from adverse events and effectively addresses ways to increase patient safety.
A systematic search strategy was designed to inquire for articles using a human factors approach to enhance patient care and staff well-being during the pandemic in relation to plastic surgery. We were not able to retrieve any results.
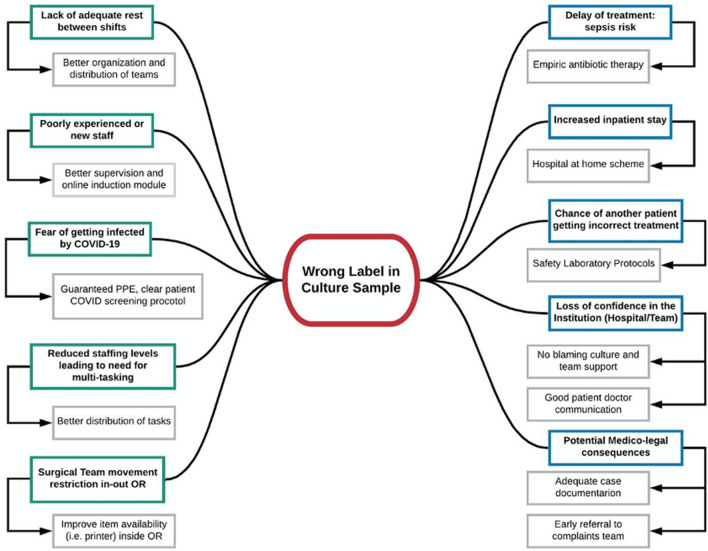
For our case, two separate human factors appraisal methods were used. A bow-tie diagram can clearly display how systemic factors can contribute to or mitigate the effects of a clinical error [3]. The “top event” in the centre is the undesired situation at which no adverse consequences have occurred yet, but there is a potential to cause harm. Potential threats that have the power to trigger the top event are located at the left side of the scheme, along with preventive barriers that prevent these threats from happening. On the right side, the protective barriers that mitigate harmful consequences derived from the “top event” are noted, such as in Fig. 1. The Systems Engineering Initiative for Patient Safety (SEIPS) 2.0 [4] human factors methodology allows analysing an incident from systemic angles, allowing us to learn from this situation and avoid further errors (Table 1).
Fig. 1.
The bow-tie diagram from the event
Table 1.
SEIPS 2.0 analysis for our case
| SEIPS 2.0 domains | |
|---|---|
| Tools and technology | Patient details are printed on sticky labels inside the OR. When a printer fails, the information is sent to a printer outside. COVID-19 has restricted the flow of personnel in and out of the OR, which may lead to having to ask other members of staff to collect these labels |
| Organization | Hospital had to recruit personnel with short notice. Formal induction was replaced by on-the-job training |
| Internal environment | Perceived temperature in theatre can rise to uncomfortable levels due to use of PPE |
| External environment | Staff living with vulnerable people were asked to live in separate accommodation, impacting on support networks and normal rest patterns |
| Tasks | Double checking by two members of staff is a routine practice. However, reduced staffing levels resulted in no one available to perform this |
| Personal factors | Fear for contracting COVID-19 may have influenced usual practices, while implying a constant distraction |
The identified threats that contributed to the incident hereby presented are varied, including the expedited recruitment of health workers during the pandemic without adequate induction, fatigue derived from reduced staffing levels, and fear of contracting COVID-19. The latter has been further exacerbated by the reports of increased risk of exposure among healthcare staff. Therefore, professionals may limit patient contact and communication channels may be impaired by the use of personal protective equipment (PPE).
The pandemic has forced health institutions to react to the global circumstances, without necessarily appreciating its unpredictable consequences. Some of these have affected protective barriers such as adequate rest after on-call duties and asking professionals to isolate from their support network. Some factors have even involved supranational discussions, such as the global lack of PPE, resulting in reduced supplies at points of care.
A human factors perspective on these types of issues provides not only better understanding on why mistakes happen and how systems fail in preventing patients from being harmed. Within the surgical team, the surgeon is only one part of the chain of reliance, which also includes the anaesthetist, nurses, operating room assistants, among others. Human factors offer the possibility of training clinicians in principles and techniques that can improve patient safety [5].
The COVID-19 pandemic has had a direct impact on patients and staff that have contracted the disease. However, the whole spectrum of consequences within the healthcare sector is still to be completely understood. Human factors offer systematic ways of understanding these processes and learn from our mistakes, along with identifying potential solutions in rapidly evolving circumstances. The benefits of acknowledging its potential contribution may prove its relevance even after this unusual period, when demand for elective surgery is likely to go back to pre-pandemic levels.
Author Contribution
All authors contributed to the writing of the manuscript.
Funding
This study was funded entirely by its authors.
Compliance with Ethical Standards
Conflict of interest
None declared.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Nikkhah MD. COVID-19 the great disruptor. J Plast Reconstr Aesthet Surg. 2020 doi: 10.1016/j.bjps.2020.05.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shorrock S, Williams C. Human factors and ergonomics in practice: improving system performance and human well-being in the real world. Boca Raton: CRC Press; 2016. [Google Scholar]
- 3.Abdi Z, Ravaghi H, Abbasi M, et al. Application of Bow-tie methodology to improve patient safety. Int J Health Care Qual Assur. 2016;29:425–440. doi: 10.1108/IJHCQA-10-2015-0121. [DOI] [PubMed] [Google Scholar]
- 4.Holden RJ, Carayon P, Gurses AP, et al. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics. 2013;56:1669–1686. doi: 10.1080/00140139.2013.838643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prado AS, Parada F. The “chain of reliance” in plastic surgery. Plast Reconstr Surg. 2009;124:462e–463e. doi: 10.1097/PRS.0b013e3181bf7ff5. [DOI] [PubMed] [Google Scholar]