Abstract
Little is known about pathogenic affective processes that cut across diverse mental disorders. The current study examines how dynamic features of positive and negative affect differ or converge across internalizing and externalizing disorders in a diagnostically diverse urban sample using bivariate dynamic structural equation modeling. One-hundred fifty-six young women completed semi-structured clinical interviews and a 21-day ecological momentary assessment protocol with seven assessments of affective states per day. Internalizing and externalizing dimensions of psychopathology were modeled using confirmatory factor analysis of mental disorders. After controlling for externalizing disorders, internalizing disorders were associated with higher negative affective mean intensity, higher negative affective variability (i.e., unique innovation variance), and lower positive affective variability. Conversely, externalizing disorders were associated with less persistent positive affect (i.e., lower inertia) and more variable positive emotionality. Results suggest internalizing and externalizing disorders have distinct affective dynamic signatures, which have implications for development of tailored interventions.
Keywords: affective dynamics, psychopathology, internalizing disorders, externalizing disorders, ecological momentary assessment
Most forms of mental illness are characterized by emotional experiences that are managed ineffectively, resulting in intense, variable, or prolonged affective episodes (American Psychiatric Association [APA], 2013). Such patterns of short-term temporal change or persistence of emotional experiences, i.e., affective dynamics, provide insight into how emotions become dysregulated across variants of psychopathology (Kuppens & Verduyn, 2015; Trull, Lane, Koval, & Ebner-Priemer, 2015). Recent innovations in intensive longitudinal (e.g., experience sampling, ecological momentary assessment [EMA], and other ambulatory assessment methods) have improved the study of affective dynamics in people’s daily lives with high levels of temporal granularity and ecological validity. In spite of this progress, the affective dynamics literature has produced inconsistent findings regarding associations between affective dynamic features and mental disorders (Houben, Noortgate, & Kuppens, 2015). Most prior studies have compared affective dynamics among those with one disorder to healthy controls without psychopathology, which limits our ability to identify dynamic emotional patterns that are either unique to any specific disorder or shared across several disorders. Thus, uncertainty remains regarding the roles of comorbidity and diagnostic covariation, and whether there are domains of emotional problems that cut across specific syndromes (Ebner-Priemer et al., 2015; Santangelo et al., 2016).
There is strong empirical evidence that mental disorders are not categorically distinct entities, but rather, are organized along higher-order dimensions, i.e., internalizing (e.g., depressive, anxiety disorders) and externalizing (e.g., antisocial personality disorder, substance-related disorders) spectra (Kotov et al., 2017). Additionally, evidence suggests that some dynamic features such as affective inertia and variability seem to characterize problems spanning the internalizing and externalizing dimensions (Houben et al., 2015). Thus, such dynamic features of affective experience may be excellent transdiagnostic indicators of vulnerability or severity and contributors to high rates of comorbidity across diagnoses. Nonetheless, the relationships between higher-order dimensions of psychopathology and affective dynamics have not been explicitly studied within a single transdiagnostic sample. It therefore remains unclear whether certain pathogenic affective dynamics characterize specific disorders (e.g., major depressive disorder) or higher-order dimensions of psychopathology more broadly (e.g., internalizing disorders). In addition, associations between affective dynamics and externalizing disorders remain understudied and poorly understood.
Because differing affective dynamic patterns may call for distinct interventions, a better understanding of how affective dynamics vary (or not) across pathological presentations could significantly enhance treatment efforts. Moreover, elucidating the affective dynamics that are common or distinct across internalizing and externalizing spectra would help to refine clinical theories regarding the nature of emotion dysregulation in various clinical presentations. Hence, the current study examines how dynamic features of positive and negative affect differ or converge across internalizing and externalizing disorders in a diagnostically diverse sample. We first review the findings and limitations of existing literature on affective dynamics in various mental disorders.
Affective Dynamics and Psychopathology
A range of affective dynamic constructs have been described using diverse terminology and methods of assessment (Krone, Albers, Kuppens, & Timmerman, 2018; Kuppens & Verduyn, 2015). Though not technically a temporal dynamic, mean intensity (i.e., the within-person average level of an emotion across repeated measures) is an important aspect of an individual’s emotional profile that is robustly associated with psychological well-being (Krone et al., 2018; Spindler, Stopsack, Aldinger, Grabe, & Barnow, 2016). Intensive longitudinal studies (e.g., using EMA) have demonstrated that high negative affect (NA) and low positive affect (PA) mean intensity characterize individuals with social anxiety disorder (Kashdan & Farmer, 2014), borderline personality disorder (BPD; Ebner-Priemer et al., 2015), depression (Erbas, Ceulemans, Lee Pe, Koval, & Kuppens, 2014), and high levels of neuroticism (Erbas et al., 2014; Miller, Vachon, & Lynam, 2009), which itself is associated with internalizing problems (Kotov, Gamez, Schmidt, & Watson, 2010). Evidence of associations between NA and PA mean intensity in daily life and externalizing problems is sparse. However, disinhibition-related traits (i.e. low conscientiousness and agreeableness) are associated with both low PA (Carstensen, Pasupathi, Mayr, & Nesselroade, 2000; Komulainen et al., 2014), and externalizing problems (Ruiz, Pincus, & Schinka, 2008), suggesting that externalizing disorders may be associated with low PA but not necessarily high NA. Notably, internalizing and externalizing disorders are rarely examined concurrently in existing EMA research, limiting firm conclusions about the extent to which differences in NA and PA mean intensity are transdiagnostic versus disorder-specific.
Although there is limited research examining affect intensity and externalizing pathology utilizing intensive longitudinal methods, there is research using retrospective self-report of NA and PA; however, this work has yielded conflicting results. For instance, pathological gambling (MacLaren, Fugelsang, Harrigan, & Dixon, 2011) and substance use disorders (Cheetham, Allen, Yucel, & Lubman, 2010; Elkins, King, McGue, & Iacono, 2006) have been associated with elevated NA and mixed results for PA. Aggressive behavior, however, may be associated with low PA, particularly with respect to social relationships (Fanning, Berman, & Guillot, 2012), and psychopathy has been tied to low PA and elevated NA (Garcia, Adrianson, Archer, & Rosenberg, 2015). Other work has failed to find evidence of a link between PA and externalizing pathology (Watson, Stasik, Ellickson-Larew, & Stanton, 2015).
Inertia and variability are commonly studied features characterizing temporal persistence and fluctuation of emotions, respectively (Krone et al., 2018; Kuppens & Verduyn, 2015). Inertia (e.g., autoregression, carry-over) refers to the degree to which an emotion persists from one occasion to the next (Kuppens, Allen, & Sheeber, 2010), with higher inertia indicating less flexibility to adapt to changing circumstances. Variability describes the amplitude of deviations from an individual’s mean level over time (Krone et al., 2018), usually quantified as a within-person standard deviation (SD). Variability metrics that take inertia into account, such as the mean squared successive difference (MSSD) between consecutive emotion measurements (Trull et al., 2008), capture moment-to-moment fluctuations, with higher levels indicating a more unstable emotional profile (i.e., affective instability). Greater variability per se is generally thought to reflect heightened affective reactivity to internal or external events. Some affective dynamic models, such as the Flex3 model (Hollenstein, 2015), highlight the importance of dynamic (real-time) flexibility within a particular context as distinct from reactive flexibility, which occurs in response to shifting contexts, environments, or situations.
Though some degree of inertia and variability of emotions is considered normative (Cunningham, Dunfield, & Stillman, 2013; Kuppens, Oravecz, & Tuerlinckx, 2010), and the role of emotional inertia may vary on the basis of emotional context (Koval, Sütterlin, & Kuppens, 2016), higher levels of both have been linked to a wide range of psychopathology. Specifically, a recent meta-analysis of 79 short-term affective dynamics studies (Houben et al., 2015) suggested that higher NA and PA inertia and variability were associated with multiple types of symptomatology, although effect sizes were generally smaller for PA dynamics. However, PA variability was not uniformly associated with maladaptive constructs. For example, PA variability was positively associated with extraversion, negatively associated with depression, and marginally positively associated with positive emotionality (Houben et al., 2015). Another recent study found that higher PA instability predicted subsequent increases in life satisfaction, suggesting that PA instability might reflect adaptive flexibility and reactivity to environmental input, including positive or rewarding events (Spindler et al., 2016). These findings are consistent with research suggesting that depressed individuals demonstrate less contextually appropriate sensitivity to positive as well as negative stimuli (Bylsma, Morris, & Rottenberg, 2008). Overall, greater NA variability appears to be largely transdiagnostic across the internalizing and externalizing spectra, but the nature of relations between PA variability and psychopathology may be more complex. Furthermore, no studies have examined associations between inertia and externalizing symptoms. Thus, it remains unclear whether NA and PA inertia characterize affective dynamics across both internalizing and externalizing disorders.
Augmentation and blunting describe how changes in one emotion relate to near-term changes in another emotion (Pe & Kuppens, 2012). Positive cross-lagged coefficients indicate that increased experience of one emotion predicts an increase in another emotion at a successive time point (i.e., augmentation), whereas negative coefficients indicate increased experience of one emotion precedes decreased experience of another (i.e., blunting). Elevated levels of augmentation and blunting (e.g., stronger connections between distinct emotions over time) are thought to reflect a densely connected emotional network (Pe et al., 2014), which may reflect an emotional system that is more resistant to change and impermeable to external influences (Kuppens & Verduyn, 2015). These dynamics have not been well-studied in relation to psychopathology yet hold great potential for improving our understanding of emotion regulation processes.
Covariation describes the extent to which different emotional experiences occur together, and is commonly calculated with correlations between multiple emotions assessed at the same time (Krone et al., 2018; Kuppens & Verduyn, 2015). Negative correlations between positive and negative emotions (i.e., when stronger increases in PA are accompanied by stronger concurrent decreases in NA, and vice-versa) indicate greater affective polarization (Rafaeli, Rogers, & Revelle, 2007). Greater affective polarization in daily life (i.e., experiencing emotional states as all-good or all-bad) is associated with depression and anxiety (Coifman, Bonanno, & Rafaeli, 2007; Hamaker, Asparouhov, Brose, Schmiedek, & Muthén, 2018) as well as BPD and impulsive behaviors such as risky sexual behavior, substance use, and self-injury (Coifman, Berenson, Rafaeli, & Downey, 2012). These data suggest that polarized affective experiences may be transdiagnostic indicators of pathology across internalizing and externalizing symptoms. These results are consistent with the dynamic affect model (Zautra, Potter, Reich, Waner Schaie, & Powell Lawton, 1997), which suggests that increased emotional intensity (consistent with many types of psychopathology) will contribute to within-person increases in affective polarization.
Limitations of Prior Studies
Although most studies have only examined affective dynamics in a single diagnostic group relative to healthy controls, there is evidence of common affective patterns across various disorders on the internalizing spectrum (Ebner-Priemer et al., 2015; Santangelo et al., 2016; Trull et al., 2015). However, the affective dynamics that uniquely characterize externalizing disorders such as antisocial personality disorder are largely unknown. To date, no studies have examined how internalizing and externalizing symptoms are associated with temporal dynamics of emotions in a single transdiagnostic sample. Such research could aid in delineating pathogenic affective dynamics that are common across all psychopathology versus those that are specific to either high-order dimensions (e.g. internalizing, externalizing) or specific diagnostic categories (e.g. depression, social anxiety, BPD).
Another limitation of previous studies is that affective dynamic constructs have usually been examined in isolation without accounting for their covariation with other dynamics (e.g., studying variability without considering inertia or mean affective intensity), which may produce biased or inaccurate estimates of dynamic components (Krone et al., 2018). Additionally, the majority of previous studies overlooked patterns of cross-lagged associations or covariance among two or more emotions in the context of other dynamic features such as inertia and variability. Most prior studies have also used statistical methods that assume equal spacing between repeated measures; however, unequally spaced observations characterize most experience sampling data. Ignoring differences in the intervals between assessments produces inaccurate estimates of true serial autocorrelation (Oravecz, Tuerlinckx, & Vandekerckhove, 2011).
Recent innovations in dynamic multilevel modeling (e.g., dynamic structural equation models (DSEM)) can address many of these methodological limitations. It is now possible to model (as random effects) individual differences in overall means, autoregressive coefficients, cross-lagged effects, residual variances, and their covariance, while also specifying a specific time interval of interest to account for unequal spacing between assessments (Asparouhov, Hamaker, & Muthén, 2018; Hamaker et al., 2018; Jongerling, Laurenceau, & Hamaker, 2015). In this context, the random residual variance (i.e., innovation variance) represents the portion of within-person variability that cannot be predicted by the previous observations or other variables in the model. The innovation variance is of substantive interest as a measure of individual differences in reactivity or exposure to internal or external factors that influence emotional states, such as stressful interactions, substance use, positive events, or sleep quality.
Moreover, with methods such as DSEM it is now possible to examine multiple affective processes simultaneously to understand cross-lagged effects (i.e., affective augmentation or blunting) and covariance of innovations (i.e., affective differentiation or polarity), in addition to mean intensity, inertia, and innovation variance. For instance, Hamaker et al. (2018) used a DSEM framework to examine the dynamics of both PA and NA assessed via daily self-reports. Their results suggested that in young adults, becoming “stuck” in negative affectivity (higher NA inertia) and greater polarization of PA and NA (more negative covariance of innovations) are characteristic of depressive symptoms and appear to perpetuate them.
Goals and Hypotheses of the Current Study
The overarching goal of the current study was to examine relations between empirically identified higher-order dimensions of psychopathology and multiple affective dynamics in a diagnostically diverse, urban sample of young women. We used bivariate multilevel cross-lagged models of ecological momentary assessment (EMA) data within a DSEM framework (Asparouhov et al., 2018; Hamaker et al., 2018) to address many of the limitations in prior studies. Specifically, we estimated multiple temporal dynamic features of PA and NA simultaneously, including mean intensity, inertia, variability (i.e., innovation variance), augmentation and blunting (i.e., cross-lags), and covariance (i.e., polarization) at the hourly level. We then examined transdiagnostic dimensions of psychopathology (derived from confirmatory factor analysis [CFA] of diagnostic categories obtained via clinician-administered semi-structured diagnostic interviews) as predictors of all affective dynamics in a multivariate DSEM. Based on previous studies examining the structure of psychopathology (Eaton et al., 2011; Kotov et al., 2017; Krueger, McGue, & Iacono, 2001), we expected that two factors, representing internalizing and externalizing dimensions, would emerge from CFA of the diagnostic categories. Given previous findings (for reviews, see Houben et al., 2015 and Krone et al., 2018), we also hypothesized that greater levels of internalizing psychopathology would be associated with (1) higher NA mean intensity, inertia, and variability, (2) lower PA mean intensity and, (3) more NA and PA blunting and polarization. Though evidence for affective dynamics and externalizing disorders is sparse, we tentatively hypothesized that externalizing disorders would be associated with lower PA mean intensity, higher NA variability, and affective polarization.
Method
Participants and Recruitment Procedures
The current study is a secondary data analysis of data collected from a subsample of young women from the ongoing Pittsburgh Girls Study (PGS) who were recruited for a substudy on young women’s personality features. Participants were recruited for the substudy based on recent reports of impulsive aggression and/or self-harm, difficulties that are associated with significant emotion dysregulation and that occur across the internalizing and externalizing spectra (Conway, Latzman, & Krueger, 2019; Prinstein, Boergers, & Vernberg, 2001). The larger PGS from which the sample was drawn involves an urban community sample of 2,450 women who were initially recruited in 1999 and 2000 when they were ages 5 to 8 years old. PGS participants were identified by oversampling from neighborhoods in which at least 25% of families were living at or below poverty level (see Keenan et al., 2010 for further details on PGS recruitment and study design). Participants over the age of 18 from the PGS were first identified for the current substudy based on self-reports of recent verbal, physical, or relational aggressive behavior, suicidality, or self-injury within the last year via items administered annually in the PGS assessment battery. Women who were identified in the first stage were then contacted by telephone for further screening to ascertain whether they had engaged in externalized aggressive behavior (e.g., yelling/screaming, insulting or calling someone names, hitting or punching someone, threatening to beat someone up, etc.), self-injurious behavior, or suicidal ideation or behavior in the last month. Women who endorsed any of these behaviors in the past month were invited to participate in the current substudy. Screening procedures are further described in Scott et al. (2017).
One hundred and sixty-six women were recruited and consented to participate. Four participants were excluded from further analyses due to insufficient EMA data (completing less than 5 of 42 scheduled assessments during week 1 of the EMA, followed by no assessments in subsequent weeks). An additional 6 participants were excluded due to failure to complete the diagnostic interviews at baseline, leaving 156 women with usable data for the current analysis. Participants ranged in age from 18 to 24 (M = 21.53, SD = 1.58). Consistent with the diverse demographics of the PGS, 72% of participants self-identified as racial or ethnic minority (70% African American; 2% multi-racial; 4% Hispanic/Latina) and 51% reported receipt of public assistance benefits at the time of enrollment.
Assessment Procedures and Measures
Participants completed semi-structured diagnostic interviews (described below) in the laboratory followed by a 21-day EMA protocol. All study procedures were approved by the University of Pittsburgh Institutional Review Board (Protocol Number PRO13050549). This project was conducted in accordance with the Declaration of Helsinki. Participants were compensated for their participation.
Diagnostic Interviews.
Psychiatric disorders were assessed using the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I; First, Gibbon, Spitzer, & Williams, 1997) and the Structured Clinical Interview for DSM-IV Personality Disorders (SIDP-IV; Pfohl, Blum, & Zimmerman, 1997).1 Interviewers were post-baccalaureate, masters, or doctoral-level clinicians who were trained by the first author (LNS). The present analyses were restricted to current (i.e., not lifetime) disorders that affected 5% or more of our sample. Prevalence rates for each diagnosis are presented in Table 1. A randomly selected set of interviews (n = 25; 16%) were videotaped and rated by an independent clinical judge for calculation of interrater reliability. Kappas (κ) were calculated for diagnoses with frequencies of 5% or more in the reliability sample. The average kappa across diagnostic categories was κ = .81 (SD = .15; Range = .62 – 1.0).
Table 1.
Prevalence rates for current clinical diagnoses that were most common (affecting > 5%) in the study sample (N=156)
| n | % | |
|---|---|---|
| Alcohol use disorder | 8 | 5.1 |
| Antisocial personality disorder | 14 | 9.0 |
| Borderline personality disorder | 23 | 14.7 |
| Drug use disorder | 31 | 19.9 |
| Dysthymia | 8 | 5.1 |
| Generalized anxiety disorder | 13 | 8.3 |
| Major depressive disorder | 25 | 16.0 |
| Panic disorder | 8 | 5.1 |
| Posttraumatic stress disorder | 21 | 13.5 |
| Social Phobia | 10 | 6.4 |
| Specific Phobia | 11 | 7.1 |
Ecological Momentary Assessment of Positive and Negative Affect.
After completion of diagnostic interviews, participants were trained to use a touch screen smart phone on which they completed a 21-day web-based EMA protocol consisting of a daily morning assessment and six daily random prompts to assess their current mood (see Scott et al., 2017 for additional description of the EMA protocol). At each assessment, participants were asked to rate on 5-point Likert scales (1 = not at all, 5 = extremely) the extent to which they experienced different emotions “in the past 15 minutes.” This wording was used to reduce zero inflation of affect ratings commonly seen in momentary assessments in which participants respond regarding their affect as they are filling out the survey, rather than how they were feeling prior to the survey prompt. Items assessing general positive and negative affective states were drawn from the Positive and Negative Affect Schedule – Extended version (Watson & Clark, 1999). PA and NA scales were created by calculating the mean of positive items and the mean of negative items for each person at each measurement occasion. For each scale, between- and within-person reliability estimates were calculated using methods described by Cranford et al. (2006). The scales used, their corresponding items, and between- and within-person reliability estimates for each scale were: NA (ashamed, guilty, hostile, irritable, scared, sad, lonely; .98 and .74); PA (excited, proud, happy, cheerful, joyful, delighted; .99 and .90). Intraclass correlation coefficients (ICCs), which represent the proportion of between-person variability in repeated measures from the EMA protocol, were .38 for NA and .42 for PA. Thus, more than half of the variability in these measures was within individuals over time. Participants completed an average of 112 EMA reports (SD = 31.56), which corresponds to 76% of possible reports. A total of 17,465 observations were included for analysis. Prior simulation studies (Schultzberg & Muthen, 2018) have shown that DSEM performs well when the number of subjects and observations are both greater than 100, as is the case in the current study. Given the semi-random assessment schedule, the distribution of time intervals between assessments varied widely but was positively skewed, with a modal value of 1.6 hours and a median of 2.2 hours. Thus, the majority of assessments were less than 2 hours apart, which informed our decision to model the data at the hourly interval as further described below.
Analytic Procedures
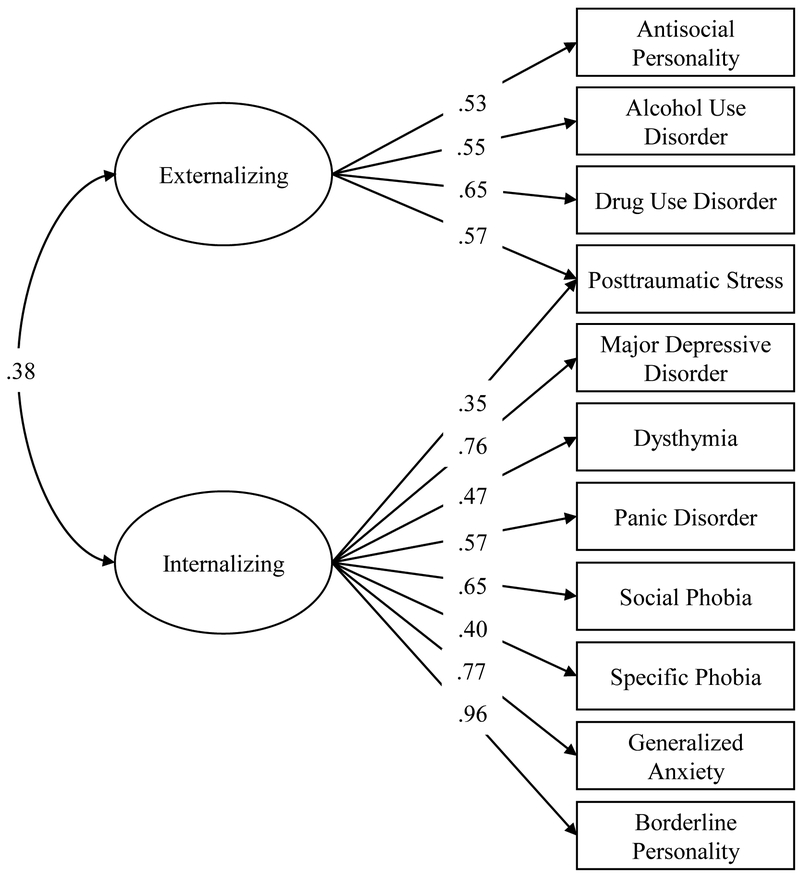
Analyses were conducted using Mplus version 8.2 (Muthén & Muthén, 2017). We first used CFA to identify higher-order constructs underlying disorders that affected 5% or more of our sample (see Table 1). Based on disorders that were common in our sample as well as prior literature on structural models of psychopathology (Eaton et al., 2011; Kotov et al., 2017; Krueger et al., 2001), we constructed our initial model with two factors: 1) Internalizing, which included major depressive disorder (MDD), dysthymic disorder, panic disorder, social phobia, specific phobia, posttraumatic stress disorder (PTSD), generalized anxiety disorder, and BPD; and 2) Externalizing, comprised of BPD, antisocial personality disorder, alcohol use disorder, and drug use disorder (collapsed across individual drug abuse/dependence diagnoses).
All diagnostic categories were entered as categorical variables and the WLSMV estimator was used. Standard indices were examined to evaluate model fit, including chi-square (χ2), Comparative Fit Index (CFI), Tucker-Lewis Index (TLI), and root mean squared error of approximation (RMSEA). Excellent model fit is indicated by a non-significant χ2 test, CFI and TLI values > .95, and RMSEA values < .05 (Hu & Bentler, 1999). For well-fitting models, we examined the pattern of factor loadings to identify improper solutions (e.g., standardized factor loadings > 1) and determine if any diagnoses should be removed from the model based on weak or negative factor loadings (i.e., standardized loadings < .3). We also examined modification indices (MI) to determine if any theoretically defensible cross-loadings should be allowed (based on MI > 5). Nested models were compared using the DIFFTEST option in Mplus, which calculates the χ2 difference test for WLSMV estimation. Once the best-fitting CFA model was identified, we extracted the factor scores to be used as predictors in subsequent analyses.
Next, we modeled the hour-to-hour temporal dynamics of NA and PA using bivariate multilevel cross-lagged models estimated using DSEM in Mplus version 8.2 (Muthén & Muthén, 2017). Specifically, we estimated a first-order vector autoregressive (VAR(1)) model with Bayesian Markov Chain Monte Carlo (MCMC) estimation and default (i.e., non-informative) priors. The DSEM framework has several advantages for intensive longitudinal data analysis: 1) repeated measures of NA and PA are automatically decomposed into within and between-person variance using latent mean centering, avoiding the downward bias in autoregressive parameters associated with sample mean centering; 2) multiple random effects and their covariances can be modeled simultaneously; 3) unequal intervals between observations due to random sampling or missed assessments can be accommodated by specifying the time interval of interest for time-lagged associations (e.g., TINTERVAL command); and 4) missing data are imputed automatically by sampling from the conditional posterior distribution at each iteration of the MCMC algorithm. Because we were interested in short-term temporal dynamics and most observations were less than two hours apart, we specified one-hour increments as the time interval of interest by setting the TINTERVAL function to a value of 1, scaled to the unit of hours. With this specification, covariance coverage was > 23%, which is well above the minimum recommended coverage for DSEM based on prior simulations (Asparouhov, Hamaker, & Muthén, 2018). Our model specifications mirrored those used in a similar study of the temporal dynamics of NA and PA at the daily level (see Hamaker et al., 2018, for technical details). We allowed all random effects to covary with each other at the between-persons level. All models were estimated using default (i.e., non-informative) priors, 50,000 iterations, and two MCMC chains. Model convergence was checked using the proportional scale reduction (PSR) indices for each parameter and by examining trace plots for irregularities (e.g., trends and cycles). PSR values close to one suggest model convergence.
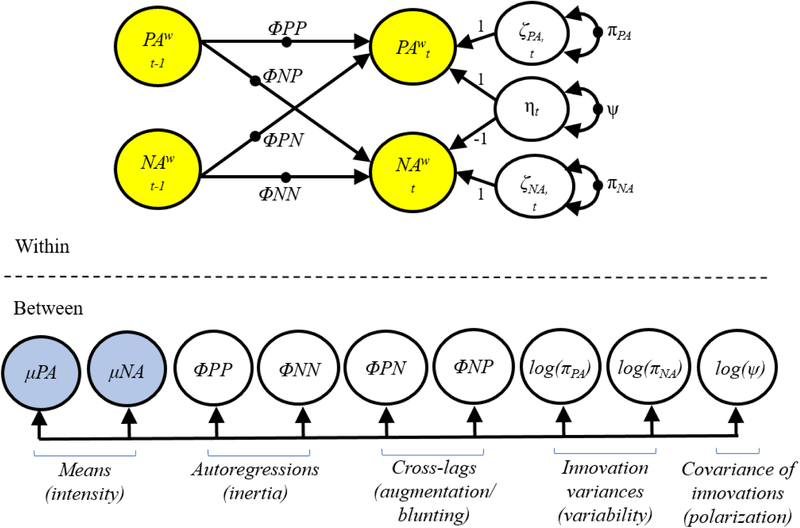
We first estimated an unconditional bivariate multilevel VAR(1) model with no between-person covariates, which included nine random effects (depicted in Figure 1): individual differences in mean intensity of PA and NA (indicated by the random means μPA and μNA); inertia of PA and NA from one hour to the next (reflected in higher autoregressive coefficients, ΦPP and ΦNN); augmentation or blunting (reflected in cross-lagged regressions, ΦPN and ΦNP); variability of PA and NA (indicated by the random log of the unique parts of the innovations, i.e., innovation variances, log(πPA) and log(πNA)); and affective polarization as indicated by associations between the unique parts of the innovations of PA and NA within each hour (captured in the log of negative covariance between the innovations, log(ψ)). As in Hamaker et al. (2018), we specified a common factor for the covariance of the innovations with factor loadings of 1 and −1 for PA and NA to aid in model convergence. The resulting parameter is modeled as the log of the negative covariance at the between-persons level. The predicted covariance of the innovations can thus be calculated by taking the exponentiated predicted log of the negative covariance, and multiplying by −1 (see Hamaker et al., 2018, for details and formulas). Generally, a more strongly negative predicted covariance of innovations suggests more polarization such that within-hour increases in NA are accompanied by same-time decreases in PA, and vice-versa.
Figure 1.
Path diagram for the unconditional bivariate multilevel VAR(1) model for positive affect (PA) and negative affect (NA) with nine random effects: individual differences in mean intensity of PA and NA; random means μPA and μNA); inertia of PA and NA from one hour to the next (autoregressive coefficients, ΦPP and ΦNN); augmentation or blunting (cross-lagged regressions, ΦPN and ΦNP); variability of PA and NA (random log of the unique parts of the innovations, i.e., innovation variances, log(πPA) and log(πNA)); and affective polarization as indicated by associations between the unique parts of the innovations of PA and NA within each hour (captured in the log of negative covariance between the innovations, log(ψ)). The final unconditional and conditional models included two additional random effects of time regressed on PA and NA (not shown). This figure was adapted from Hamaker et al., 2018.
After establishing convergence of the unconditional model, we estimated a conditional DSEM model in which all random effects at the between-person level were regressed on the factors extracted using CFA, allowing us to test hypotheses regarding associations between higher-order dimensions of psychopathology and affective dynamics. Given that nearly three quarters of the sample identified as minority race/ethnicity and more than half were receiving public assistance linked with household income below the national poverty level, we decided a priori to include minority race or ethnicity (0 = White and Non-Hispanic; 1 = African American, Multi-racial, or Hispanic/Latina) and low socioeconomic status (SES; 0 = not receiving public assistance; 1 = receiving public assistance) as covariates (i.e., predictors of all random effects at the between-persons level) in the final model. We also explored several other factors (e.g., number of EMA entries completed, participant age, education) as potential between-person covariates, but these did not emerge as significant predictors and were omitted from subsequent analyses.
Results
Confirmatory Factor Analysis
The initial two-factor CFA model fit the data well according to all fit indices (χ2[42] = 40.30, p = .55; CFI and TLI ≥ 1; and RMSEA < .001), but examination of the pattern of factor loadings indicated model misspecification with the cross-loading of BPD on both factors. Specifically, BPD had a standardized factor loading greater than one on the internalizing factor and a negative loading on the externalizing factor. Therefore, we re-specified the model with BPD loading only on the internalizing factor. The revised, more constrained model demonstrated excellent fit to the data according to all fit indices (χ2[43] = 41.14, p = .55; CFI and TLI ≥ 1; and RMSEA < .001) with no significant decrement in model fit compared to the initial model (Δχ2[1] = 0.55, p = .45). All factor loadings were within the expected range and statistically significant. However, an MI > 5 suggested that PTSD should be allowed to cross-load on the externalizing factor. This is consistent with evidence of high rates of comorbidity of PTSD with both internalizing and externalizing disorders (Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995; Miller & Resick, 2007). Hence, the model was again re-specified to allow PTSD to load on both internalizing and externalizing factors. This second revised model fit the data well (χ2[42] = 35.24, p = .76; CFI and TLI ≥ 1; and RMSEA < .001) and resulted in a significant improvement in model fit in comparison to the model with no cross-loadings (Δχ2[1] = 5.82, p = .02). Though the loading of PTSD on internalizing disorders was no longer statistically significant (p = .13), the magnitude of this loading (.35) and the improvement in model fit led us to retain this version of the two-factor model. Alternative models were explored, e.g., one-factor, three-factor, second-order hierarchical, and bifactor models, but these resulted in either worse fit or nonconvergence. Therefore, we accepted the revised two-factor model (depicted in Figure 2) as the best-fitting model for the diagnostic data. We extracted factor scores for each participant from this model to be used as predictors in subsequent analyses to examine the relations between these two transdiagnostic dimensions of psychopathology and affective dynamics. Additional details on the alternative CFA models tested and evidence for the suitability of the extracted factors for further analysis are provided in the Supplemental Analyses section of the Supplemental Material available online.
Figure 2.
Final confirmatory factor analysis model of psychopathology factors with standardized factor loadings and correlations. All parameters are statistically significant at p < .05 except for the standardized loading of posttraumatic stress disorder on internalizing (p = .13).
Unconditional DSEM
We tested unconditional DSEMs of affective dynamics with and without time as a random effect (i.e., PA and NA at each timepoint regressed on person-mean-centered amount of time elapsed since the first entry across the 21-day protocol). These models suggested that levels of NA and PA showed significant decreases over time, with significant between-person variability in these trajectories. These trends may reflect participant reactivity, i.e., a change in behavior resulting from the act of completing self-report assessments repeatedly over time (Korotitsch & Nelson-Gray, 1999; Shiffman, Stone, & Hufford, 2008). To adjust for trends, we included the random effects of time on PA and NA at the within-persons level. Thus, our final unconditional DSEM model contained a total of 11 random effects (i.e., two random trends and nine random affective dynamics parameters). The highest PSR value in the unconditional model was 1.004, suggesting good model convergence. Results of the final unconditional DSEM model can be found in Table S1 in the Supplemental Material available online. Note that, with Bayesian estimation, exact p values for two-tailed significance tests are not available. Statistical significance is determined by estimating a credibility interval (CI) for each parameter, and 95% CIs that do not include 0 indicate statistical significance at α = .05. For the interested reader, we provide biserial correlations between affective dynamics (random effects extracted for each participant from the unconditional DSEM) and each individual diagnostic category in Table S3 in the Supplemental Material available online.
Conditional DSEM
In the conditional DSEM, the 11 random effects described above (i.e., two random trends and nine random affective dynamics parameters) were regressed on minority race, low SES, and the extracted internalizing and externalizing factors. Covariances of predictors and outcomes were also estimated. Prior to testing the full conditional model, we examined collinearity diagnostics, including variance inflation factor (VIF) and tolerance statistics, which revealed no evidence for multicollinearity among the predictors (VIFs > 1 and < 2; tolerance ≥ .62). Unstandardized fixed effects (means), regression parameters, and effect sizes (f2) for internalizing and externalizing factors on each of the nine random affective dynamics from the final conditional model are presented in Table 2. The highest PSR value in the final conditional model was 1.008, suggesting good model convergence. Full unstandardized and standardized results from the final conditional DSEM are provided in the Supplemental Material available online. Note that the results reported here focus primarily on unique associations that emerge when controlling for both internalizing and externalizing problems and their covariation in the same model. To aid in the interpretation of the full conditional model results, we also provide results from analyses with only internalizing or externalizing as predictors of affective dynamics (after controlling for demographic covariates) in the Supplemental Materials available online (see Supplemental Analyses and Final Conditional Model Results).2
Table 2.
Unstandardized estimates (posterior means), 95% credibility intervals (CIs), and effect sizes (f2) from the conditional multilevel model
| Between-person predictors of random effects | |||||||
|---|---|---|---|---|---|---|---|
| Estimated mean | Externalizing Factor | f2 | Internalizing Factor | f2 | |||
| PA mean intensity (mean; μPA) | 1.85 [1.66, 2.05] | −0.04 [−0.42, 0.34] | .01 | −0.05 [−0.29, 0.18] | .01 | ||
| NA mean intensity (mean; μNA) | 1.25 [1.18, 1.33] | −0.03 [−0.18, 0.12] | .01 | 0.17 [0.07, 0.27] | .10 | ||
| PA inertia (autoregression; ΦPP) | 0.47 [0.38, 0.55] | −0.24 [−0.40, −0.08] | .08 | 0.05 [−0.06, 0.14] | .01 | ||
| NA inertia (autoregression; ΦNN) | 0.45 [0.35, 0.54] | −0.04 [−0.23, 0.14] | .01 | 0.06 [−0.06, 0.17] | .02 | ||
| NAt-1→PAt augmentation (cross-lag; ΦPN) | −0.18 [−0.30, −0.08] | −0.02 [−0.21, 0.17] | .01 | 0.01 [−0.10, 0.12] | .01 | ||
| PAt-1→NAt augmentation (cross-lag; ΦNP) | −0.04 [−0.06, −0.02] | 0.002 [−0.04, 0.04] | .01 | −0.02 [−0.04, 0.01] | .04 | ||
| PA variability (innovation variance; log(πPA)) | −1.84 [−2.19, −1.48] | 0.71 [0.01, 1.42] | .04 | −0.47 [−0.91, −0.04] | .04 | ||
| NA variability (innovation variance; log(πNA)) | −4.22 [−4.74, −3.72] | 0.06 [−0.93, 1.06] | .01 | 0.97 [0.37, 1.58] | .08 | ||
| Polarization (negative covariance of innovations; log(ψ)) | −3.91 [−4.36, −3.46] | 0.66 [−0.25, 1.56] | .03 | 0.18 [−0.40, 0.76] | .02 | ||
Note. N = 156 (17,465 observations). CIs are presented in brackets. Bold type indicates effects that are statistically significant based on CIs that do not include zero. Effect sizes (f2) were calculated for effects of internalizing and externalizing based on model R2 values from models with and without each of these variables (see Supplemental Materials for all conditional model results and R2 values). Effects of covariates (i.e., time at the within-person level; race/ethnicity and low SES at the between-person level) and covariances among predictors and dependent variables (random effects) were also estimated (see Supplemental Materials for these parameter estimates and fully standardized results for all conditional models).
Partially consistent with our hypotheses, both with and without externalizing problems in the model, internalizing disorders were associated with greater NA mean intensity (μNA) and NA variability (i.e., NA innovation variance, log(πNA)). In addition, the internalizing factor was associated with lower PA variability (PA innovation variance, log(πPA)), but this emerged only after controlling for externalizing disorders. Thus, internalizing disorders were uniquely associated with more intense and variable NA and less variable PA. Contrary to hypotheses, internalizing problems were not significantly associated with greater NA inertia (ΦNN), PA mean intensity (μPA), augmentation or blunting (ΦPN,i and ΦNP,i), or polarization (log(ψi)) in any model. Unexpectedly, in models with and without internalizing disorders, externalizing psychopathology was associated with lower PA inertia (i.e., ΦPP). Only after controlling for internalizing disorders, externalizing disorders were also associated with greater PA variability (PA innovation variance, log(πPA)). These findings suggest that externalizing disorders are uniquely associated with more fleeting and variable PA. It should be noted, however, that all effect sizes were quite small according to Cohen’s (1988) criteria (i.e., f2=.02 and .15 corresponding to small and medium, respectively). The most robust effect emerged for the association between internalizing disorders and NA mean intensity (f2=.10).
Discussion
This is the first study to examine how superordinate dimensions of psychopathology relate to multiple dynamic features of NA and PA at the hourly level in daily life. As hypothesized, two factors representing internalizing and externalizing dimensions emerged from CFA of categorical diagnoses. Partially consistent with our expectations, greater internalizing disorders were associated with higher NA mean intensity and variability (i.e., innovation variance), as well as lower PA variability, after controlling for externalizing disorders. These findings suggest that internalizing disorders are uniquely associated with greater overall negative affectivity and reactivity to internal or external events, which may reflect greater stress sensitivity combined with less reward sensitivity. Results did not support our hypotheses regarding associations between internalizing disorders and NA inertia, PA mean intensity, cross-lagged associations (i.e., augmentation/blunting), or polarization of NA and PA. Also contrary to our expectations, externalizing disorders were associated with lower PA inertia and higher PA variability after controlling for internalizing disorders, and they were not associated with lower PA mean intensity, higher NA variability, or affective polarization.
Our results suggest that disorders along the internalizing spectrum reflect a greater tendency to experience negative emotion, but not necessarily more persistent emotion, extremes of emotion (as with polarization), or affective blunting. Our finding that internalizing disorders are linked to more intense and variable NA, as well as less variable PA, is consistent with the character of these disorders and their underlying personality constructs. In particular, evidence from prior studies suggests that internalizing disorders are characterized by elevated neuroticism (Kotov et al., 2010), which is linked to higher negative emotionality, lower positive emotionality, and more negative affective variability and reactivity to stressors (Komulainen et al., 2014). Though we did not find an association between internalizing disorders and low PA mean intensity, the negative association between internalizing disorders and PA variability may reflect less flexibility and reactivity to positive or rewarding input (Spindler et al., 2016). These results are consistent with prior findings demonstrating that depressed individuals display low PA variability (Houben et al., 2015) and less sensitivity to positive stimuli (Bylsma et al., 2008). Our results expand on prior work by demonstrating that these dynamics characterize internalizing disorders more broadly, rather than depression specifically.
Although we anticipated internalizing pathology to be associated with affective polarization based on prior work (Coifman et al., 2007; Hamaker et al., 2018), this was not the case in the present study. This may be due to the concurrent modeling of NA mean intensity, which was associated with internalizing symptoms and was also significantly correlated with NA-PA polarization (see Table S2 in online Supplemental Materials). This finding is consistent with the dynamic affect model (Zautra et al., 1997), which suggests that high emotional intensity contributes to within-person increases in affective polarization. This result further underscores the importance of modeling different affective dynamics in the multivariate context to account for the dependencies between different dynamic features.
Our results for externalizing disorders are more novel and distinct than those for internalizing symptoms. Our study is the first to demonstrate a negative association between externalizing disorders and PA inertia, suggesting that increases in positive emotions are more fleeting in young women with more externalizing pathology. Furthermore, when both internalizing and externalizing disorders were included in the same model, externalizing disorders were associated with greater PA variability, whereas internalizing disorders were associated with less PA variability. Though higher PA variability has been associated with several maladaptive constructs in previous studies (Houben et al., 2015), these findings have been mixed, and some studies suggest that PA variability is adaptive (Spindler et al., 2016). Our results suggest that heightened PA variability is uniquely associated with externalizing problems in a multivariate model that accounts for NA and various affective dynamics, but only after controlling for internalizing disorders, which are associated with the opposite pattern (i.e., less PA variability). Greater variability in positive affect among individuals with externalizing disorders could potentially reflect hypersensitivity to reward cues. This pattern is consistent with behavioral studies (Murray, Waller, & Hyde, 2018) and Gray’s reinforcement sensitivity theory (Gray, 1982, 1987), which claims externalizing disorders are characterized by heighted activation of the behavioral activity system (BAS) combined with hypoactivation of the behavioral inhibition system (BIS). Given our observation in the current study of more fleeting PA among those with externalizing disorders, it is plausible to speculate that the transience of positive emotional experiences in these individuals may lead to increased sensation-seeking behaviors to alleviate boredom or to boost PA (Cloninger, 1987; Zuckerman, 1996). Thus, externalizing disorders may be characterized by a sensitive BAS that is prone to activation, but once activated, may quickly become deactivated, leading to the repetitive reward-seeking behaviors characteristic of externalizing disorders, such as substance use or impulsive behavior. These interpretations are speculative, however, and should be further explored in future work.
Some noteworthy patterns of covariation emerged from the CFA of individual disorders. First, BPD did not load on the externalizing factor, which diverges from several prior studies (Eaton et al., 2011; Kotov et al., 2017; Krueger et al., 2001). However, one study found that BPD was more strongly associated with externalizing disorders in men than in women (James & Taylor, 2008; Johnson et al., 2003). Hence, the exclusive loading of BPD on the internalizing factor may be due in part to the all-female sample. Furthermore, even when BPD does cross-load on both dimensions, internalizing problems typically account for more BPD variance than externalizing problems (Eaton et al., 2011). Nonetheless, the factor loading of BPD on the internalizing factor in the current study was unusually high (.96), indicating that internalizing disorders accounted for 92% of the variance in BPD. In addition, we did not expect PTSD to load on both internalizing and externalizing disorders, though this result is consistent with prior findings of internalizing and externalizing posttraumatic stress disorder subtypes (Miller & Resick, 2007; Wolf, Miller, Harrington, & Reardon, 2012).
Strengths of this study include the intensive repeated assessment of affect (i.e., 7 times daily for 21 days) and the use of advanced statistical tools to model several affective dynamics simultaneously, allowing us to control for covariation among different dynamic features of affect. Another important improvement from prior literature was our ability to model innovation variance. This approach takes inertia and other affective dynamics into account to assess variability of affect from one occasion to the next. In addition, whereas most previous work has ignored differences in time lags between repeated assessments, we addressed unequally spaced observations explicitly in the model and can thus draw conclusions about a specific time interval of one hour.
Another strength and innovative aspect of the current study is our examination of how higher-order dimensions of psychopathology in a transdiagnostic at-risk sample relate to multiple affective dynamics. Comorbidity in psychiatric diagnoses is the norm, rather than the exception (Kessler, Chiu, Demler, Merikangas, & Walters, 2005), and recent innovations in the field support the validity of transdiagnostic approaches to psychiatric concerns (c.f., Hierarchical Taxonomy of Psychopathology, Kotov et al., 2017, and NIMH Research Domain Criteria, Krueger & DeYoung, 2016). This current study reveals new findings on how higher-order dimensions of psychopathology relate to affective dynamics, and these novel results represent a significant extension of the prior disorder-specific dynamics literature. For instance, this is the first study to suggest that internalizing and externalizing disorders are characterized by distinct affective dynamics and may therefore benefit from distinct interventions. This project is further consistent with the goals of the Research Domain Criteria (RDoC) framework in its use of assessment techniques at multiple levels of assessment (e.g., self-report, behavior). A better understanding of how emotional signatures differ or remain consistent across diagnostic boundaries is essential for developing more effective interventions that target transdiagnostic affective processes. However, it should be noted that the effects observed here were small in magnitude, and hence, their clinical utility is not yet clear. An important direction for future research is to evaluate how changes in affective dynamics relate to longitudinal changes in clinical outcomes. We comment on this further below.
Although this study had several notable strengths, several limitations should be discussed. First, most prior studies examining the structure of psychopathology have done so in large, mixed-gender epidemiological samples, which differ markedly from the current at-risk community sample of 156 women in a restricted age range (18–24). All participants were selected for the current study based on clinically significant symptoms (i.e., aggressive or self-harm-related urges or behaviors), and hence, the sample included few people in the healthy range of functioning. A large proportion of the sample was also socioeconomically disadvantaged, identified as minority race, and reported substantial exposure to violence in their homes and communities, all factors that are social determinants of poorer health, both psychological and medical. Thus, although the sample is drawn from an understudied population at high risk for difficulties with emotion regulation and both internalizing and externalizing disorders, results should be interpreted in the context of these characteristics of the study sample, and may not necessarily generalize to men, older adults, healthier community participants, or individuals in clinical settings who experience less social adversity. It is likely that our findings regarding the structure of psychopathology in this sample (based on CFA models) are impacted by the selection criteria used in the study, and that findings regarding affective dynamics (based on DSEM models) are impacted by known gender and age-related differences in emotional reactivity and affective experiences. However, there was meaningful variability in other relevant demographic characteristics (e.g., educational attainment, SES, employment status) that allow us to draw inferences across racial and SES groups. The CFA results are also limited by the use of dichotomous (rather than dimensional) scores for each diagnosis; although dimensional scores would yield greater variability in diagnostic scores, the study did not include dimensional measures for all diagnoses. This limitation notwithstanding, our application of appropriate CFA methods for categorical data and use of the dimensional scores produced by CFA for the primary DSEM analyses enabled us to investigate affective dynamics in relation to transdiagnostic dimensions of psychopathology in way that has not been done in previous studies.
Some aspects of our study design and analytic methods also limited our ability to examine all effects of interest. For instance, given the sampling structure of the study itself, we used an interval of one hour to examine affective dynamics; however, other durations could be chosen, and our results may not generalize to different time intervals (e.g., several hours or days). This is an important consideration when evaluating our results against existing affective dynamics literature, as we would expect affective processes to vary as a function of the time scale of assessment (Hollenstein, 2015). Additionally, affect adjectives used in the study were selected to capture both negative and positive valence, but were not chosen to assess differing levels of arousal. Thus, our results cannot address dynamics of affective arousal, which should be considered in future work. We also chose not to examine dynamics of specific emotions such as anger, shame, and fear, as these emotional states may be more disorder-specific than general NA and PA dynamics. For instance, a recent study comparing participants with BPD, MDD, and bipolar disorder found that inertia of shame and reactivity of shame and guilt in response to interpersonal challenges were especially characteristic of BPD (Mneimne, Fleeson, Arnold, & Furr, 2018). In addition, although we controlled for linear temporal trends (i.e., changes in NA and PA over time), the complexity of our model precluded examination of other types of cycles, non-stationarity, or contextual moderators of effects. For example, NA inertia may vary as a function of specific situational factors or affective arousal level (De Haan-Rietdijk, Gottman, Bergeman, & Hamaker, 2016), and variability may be influenced by numerous internal or external factors (e.g., drug use, interpersonal stress, sleep quality, exposure to challenging environments) which could not feasibly be modeled due to the complexity of our analyses without these additional parameters. Importantly, recent work on dynamic systems models of personality suggests that traits such as neuroticism also exhibit within-person changes over time (Sosnowska, Kuppens, De Fruyt, & Hofmans, 2019), which were not explicitly examined in the current study.
Finally, it remains unknown whether common underlying processes explain transdiagnostic similarities in affective dynamics, or whether similar “emotional dynamic outcomes” may emerge from distinct multifinal pathways that vary by diagnostic presentation. Longitudinal research is needed to explicate causal relationships between psychopathology and affective dynamics and the potential mechanisms underlying these relationships. Some preliminary work (Hamaker et al., 2018) suggests that NA inertia and affective polarization prospectively predict the maintenance of depression over time, at least in young adults. Thus, more studies are needed to determine if and how affective dynamics shape the trajectory of different forms of psychopathology over time and in response to treatment. Further research is also needed to link specific affective dynamics to near-term outcomes of high clinical importance such as suicidality, substance use, or violence. Such data would inform questions about the clinical utility of assessing affective dynamics, and might aid in the development of novel real-time interventions to modify the dynamics of affect and prevent such consequences.
Findings from the present study suggest that internalizing and externalizing dimensions of psychopathology are characterized by unique affective dynamics, and therefore may benefit from different interventions. For example, interventions to modulate and stabilize negative emotions and to promote accessibility of positive emotions may be indicated among individuals with more prominent internalizing symptoms, whereas externalizing symptoms may be more effectively targeted by stabilizing positive affect and increasing adaptive strategies for achieving and sustaining positive emotional experiences. Nevertheless, comorbidity among internalizing and externalizing symptoms is common. Future studies with larger samples could explore potential interactions across these higher-order dimensions. Another important future direction is to identify person-specific affective dynamics that serve as proximal risk or protective factors for harmful behavior. Tracking an individual’s unique affective patterns using real-time monitoring would enhance just-in-time interventions among those who are at greatest risk.
Supplementary Material
Acknowledgments
This research and the efforts of the authors were supported by grants from the National Institute of Mental Health (K01 MH101289, PI: Scott; R01 MH115922, PI: Scott; R01 MH056630, PI: Loeber; R01 MH101088, PI: Stepp; K01 MH109859, PI: Beeney; R01 MH056888, PI: Pilkonis; T32 MH018269, PI: Goldstein; T32 MH018951, PI: Brent), the American Foundation for Suicide Prevention (YIG-0-131-14), National Institute on Drug Abuse (R01 DA012237, PI: Chung), the Office of Juvenile Justice and Delinquency Prevention (2013-JF-FX-0058, PIs: Hipwell/Stepp), the FISA Foundation, and the Falk Fund.
Footnotes
Because the SCID-5 had not yet been released when the study began in 2013, we used an amended version of the SCID for DSM-IV to capture significant changes in diagnostic criteria from DSM-IV to DSM-5. The resulting diagnoses can therefore be interpreted to be largely consistent with the current DSM-5 diagnostic criteria for these diagnostic categories. Further information on the amended interview can be obtained upon request from the first author.
As is often the case with momentary assessments of affect, the distribution of NA was positively skewed (skewness = 3.15). PA was also moderately skewed (skewness = 1.50). A natural log transformation reduced skewness to more acceptable levels (i.e., ≤ 3.0; log-transformed NA skewness = 1.90; log-transformed PA skewness = 0.74). However, when the final DSEM model was run for the log-transformed variables, the pattern of results and effect sizes remained consistent with the results with the raw untransformed data. Therefore, we report the results for the untransformed data to ease the interpretation of model estimates.
References
- American Psychiatric Association [APA]. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Asparouhov T, Hamaker EL, & Muthén B (2018). Dynamic Structural Equation Models. Structural Equation Modeling: A Multidisciplinary Journal, 25(3), 359–388. doi: 10.1080/10705511.2017.1406803 [DOI] [Google Scholar]
- Bylsma LM, Morris BH, & Rottenberg J (2008). A meta-analysis of emotional reactivity in major depressive disorder. Clinical Psychology Review, 28(4), 676–691. doi: 10.1016/j.cpr.2007.10.001 [DOI] [PubMed] [Google Scholar]
- Carstensen LL, Pasupathi M, Mayr U, & Nesselroade JR (2000). Emotional experience in everyday life across the adult life span. Journal of Personality and Social Psychology, 79(4), 644–655. doi: 10.1037/0022-3514.79.4.644 [DOI] [PubMed] [Google Scholar]
- Cheetham A, Allen NB, Yücel M, & Lubman DI (2010). The role of affective dysregulation in drug addiction. Clinical Psychology Review, 30(6), 621–634. https://doi.org/10/bmj8hc [DOI] [PubMed] [Google Scholar]
- Cloninger CR (1987). A systematic method for clinical description and classification of personality variants. A proposal. Archives of General Psychiatry, 44(6), 573–588. [DOI] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc. [Google Scholar]
- Coifman KG, Berenson KR, Rafaeli E, & Downey G (2012). From negative to positive and back again: Polarized affective and relational experience in borderline personality disorder. Journal of Abnormal Psychology, 121(3), 668–679. doi: 10.1037/a0028502 [DOI] [PubMed] [Google Scholar]
- Coifman KG, Bonanno GA, & Rafaeli E (2007). Affect dynamics, bereavement and resilience to loss. Journal of Happiness Studies, 8(3), 371–392. [Google Scholar]
- Conway CC, Latzman RD, & Krueger RF (2019). A meta-structural model of common clinical disorder and personality disorder symptoms. Journal of Personality Disorders, 1–19. doi: 10.1521/pedi_2019_33_383 [DOI] [PubMed] [Google Scholar]
- Cranford JA, Shrout PE, Iida M, Rafaeli E, Yip T, & Bolger N (2006). A procedure for evaluating sensitivity to within-person change: Can mood measures in diary studies detect change reliably? Personality and Social Psychology Bulletin, 32(7), 917–929. doi: 10.1177/0146167206287721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham WA, Dunfield KA, & Stillman PE (2013). Emotional states from affective dynamics. Emotion Review, 5(4), 344–355. doi: 10.1177/1754073913489749 [DOI] [Google Scholar]
- De Haan-Rietdijk S, Gottman JM, Bergeman CS, & Hamaker EL (2016). Get over it! A multilevel threshold autoregressive model for state-dependent affect regulation. Psychometrika, 81(1), 217–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton NR, Krueger RF, Keyes KM, Skodol AE, Markon KE, Grant BF, & Hasin DS (2011). Borderline personality disorder co-morbidity: Relationship to the internalizing-externalizing structure of common mental disorders. Psychological Medicine, 41(5), 1041–1050. doi: 10.1017/S0033291710001662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebner-Priemer UW, Houben M, Santangelo P, Kleindienst N, Tuerlinckx F, & Oravecz Z (2015). Unraveling affective dysregulation in borderline personality disorder: a theoretical model and empirical evidence. Journal of Abnormal Psychology, 124. doi: 10.1037/abn0000021 [DOI] [PubMed] [Google Scholar]
- Elkins IJ, King SM, McGue M, & Iacono WG (2006). Personality traits and the development of nicotine, alcohol, and illicit drug disorders: Prospective links from adolescence to young adulthood. Journal of Abnormal Psychology, 115(1), 26–39. [DOI] [PubMed] [Google Scholar]
- Erbas Y, Ceulemans E, Lee Pe M, Koval P, & Kuppens P (2014). Negative emotion differentiation: Its personality and well-being correlates and a comparison of different assessment methods. Cognition and Emotion, 28(7), 1196–1213. doi: 10.1080/02699931.2013.875890 [DOI] [PubMed] [Google Scholar]
- Fanning JR, Berman ME, & Guillot CR (2012). Social anhedonia and aggressive behavior. Personality and Individual Differences, 53(7), 868–873. https://doi.org/10/gf3nn8 [Google Scholar]
- First MB, Gibbon M, Spitzer RL, & Williams JBW (1997). Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I). Washington, DC: American Psychiatric Press. [Google Scholar]
- Garcia D, Adrianson L, Archer T, & Rosenberg P (2015). The dark side of the affective profiles: differences and similarities in psychopathy, machiavellianism, and narcissism. SAGE Open, 5(4), 215824401561516. 10.1177/2158244015615167 [DOI] [Google Scholar]
- Gray JA (1982). The neuropsychology of anxiety: an inquiry into the functions of the septo-hippocampal system. Oxford: Clarendon Press. [Google Scholar]
- Gray JA (1987). The psychology of fear and stress (Vol. 5): Cambridge University Press Archive. [Google Scholar]
- Hamaker EL, Asparouhov T, Brose A, Schmiedek F, & Muthén B (2018). At the frontiers of modeling intensive longitudinal data: Dynamic structural equation models for the affective measurements from the COGITO Study. Multivariate Behavioral Research, 1–22. doi: 10.1080/00273171.2018.1446819 [DOI] [PubMed] [Google Scholar]
- Hollenstein T (2015). This time, it’s real: Affective Flexibility, time scales, feedback loops, and the regulation of emotion. Emotion Review, 7(4), 308–315. https://doi.org/10/gfx6×9 [Google Scholar]
- Houben M, Noortgate W, & Kuppens P (2015). The relation between short-term emotion dynamics and psychological well-being: A meta-analysis. Psychological Bulletin, 141. doi: 10.1037/a0038822 [DOI] [PubMed] [Google Scholar]
- Hu L. t., & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. doi: 10.1080/10705519909540118 [DOI] [Google Scholar]
- James LM, & Taylor J (2008). Revisiting the structure of mental disorders: Borderline personality disorder and the internalizing/externalizing spectra. British Journal of Clinical Psychology, 47(Pt 4), 361–380. doi: [DOI] [PubMed] [Google Scholar]
- Johnson DM, Shea MT, Yen S, Battle CL, Zlotnick C, Sanislow CA, … Zanarini MC (2003). Gender differences in borderline personality disorder: Findings from the Collaborative Longitudinal Personality Disorders Study. Comprehensive Psychiatry, 44(4), 284–292. doi: 10.1016/S0010-440X(03)00090-7 [DOI] [PubMed] [Google Scholar]
- Jongerling J, Laurenceau J-P, & Hamaker EL (2015). A multilevel AR (1) model: Allowing for inter-individual differences in trait-scores, inertia, and innovation variance. Multivariate Behavioral Research, 50(3), 334–349. [DOI] [PubMed] [Google Scholar]
- Kashdan TB, & Farmer AS (2014). Differentiating emotions across contexts: Comparing adults with and without social anxiety disorder using random, social interaction, and daily experience sampling. Emotion, 14(3), 629–638. doi: 10.1037/a0035796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keenan K, Hipwell A, Chung T, Stepp S, Stouthamer-Loeber M, Loeber R, & McTigue K (2010). The Pittsburgh Girls Study: Overview and initial findings. Journal of Clinical Child and Adolescent Psychology, 39(4), 506–521. doi: 10.1080/15374416.2010.486320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, & Nelson CB (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52(12), 1048–1060. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, & Walters EE (2005). Prevalence, severity, and comorbidity of 12-month DSM–IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62, 617–627. 10.1001/archpsyc.62.6.617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Komulainen E, Meskanen K, Lipsanen J, Lahti JM, Jylhä P, Melartin T, … Ekelund J (2014). The effect of personality on daily life emotional processes. PloS one, 9(10), e110907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korotitsch WJ, & Nelson-Gray RO (1999). An overview of self-monitoring research in assessment and treatment. Psychological Assessment, 11(4), 415. [Google Scholar]
- Kotov R, Gamez W, Schmidt F, & Watson D (2010). Linking “big” personality traits to anxiety, depressive, and substance use disorders: A meta-analysis. Psychological Bulletin, 136(5), 768–821. [DOI] [PubMed] [Google Scholar]
- Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby RM, … Clark LA (2017). The Hierarchical Taxonomy of Psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of Abnormal Psychology, 126(4), 454–477. [DOI] [PubMed] [Google Scholar]
- Koval P, Sütterlin S, & Kuppens P (2016). Emotional inertia is associated with lower well-being when controlling for differences in emotional context. Frontiers in Psychology, 6 https://doi.org/10/gccx65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krone T, Albers CJ, Kuppens P, & Timmerman ME (2018). A multivariate statistical model for emotion dynamics. Emotion, 18(5), 739–754. doi: 10.1037/emo0000384 [DOI] [PubMed] [Google Scholar]
- Krueger RF, & DeYoung CG (2016). The RDoC initiative and the structure of psychopathology: RDoC and psychopathology structure. Psychophysiology, 53(3), 351–354. https://doi.org/10/gfx6zd [DOI] [PubMed] [Google Scholar]
- Krueger RF, McGue M, & Iacono WG (2001). The higher-order structure of common DSM mental disorders: Internalization, externalization, and their connections to personality. Personality and Individual Differences, 30(7), 1245–1259. doi: 10.1016/S0191-8869(00)00106-9 [DOI] [Google Scholar]
- Kuppens P, Allen NB, & Sheeber LB (2010). Emotional inertia and psychological maladjustment. Psychological Science, 21(7), 984–991. 10.1177/0956797610372634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuppens P, Oravecz Z, & Tuerlinckx F (2010). Feelings change: accounting for individual differences in the temporal dynamics of affect. Journal of Personality and Social Psychology, 99(6), 1042–1060. doi: 10.1037/a0020962 [DOI] [PubMed] [Google Scholar]
- Kuppens P, & Verduyn P (2015). Looking at emotion regulation through the window of emotion dynamics. Psychological Inquiry, 26(1), 72–79. doi: 10.1080/1047840x.2015.960505 [DOI] [Google Scholar]
- MacLaren VV, Fugelsang JA, Harrigan KA, & Dixon MJ (2011). The personality of pathological gamblers: A meta-analysis. Clinical Psychology Review, 31(6), 1057–1067. 10.1016/j.cpr.2011.02.002 [DOI] [PubMed] [Google Scholar]
- Miller DJ, Vachon DD, & Lynam DR (2009). Neuroticism, negative affect, and negative affect instability: Establishing convergent and discriminant validity using ecological momentary assessment. Personality and Individual Differences, 47(8), 873–877. doi: 10.1016/j.paid.2009.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller MW, & Resick PA (2007). Internalizing and externalizing subtypes in female sexual assault survivors: implications for the understanding of complex PTSD. Behavior therapy, 38(1), 58–71. doi: 10.1016/j.beth.2006.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mneimne M, Fleeson W, Arnold EM, & Furr RM (2018). Differentiating the everyday emotion dynamics of borderline personality disorder from major depressive disorder and bipolar disorder. Personality Disorders: Theory, Research, and Treatment, 9(2), 192–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray L, Waller R, & Hyde LW (2018). A systematic review examining the link between psychopathic personality traits, antisocial behavior, and neural reactivity during reward and loss processing. Personality Disorders: Theory, Research, and Treatment, 9(6), 497–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2017). Mplus user’s guide (8th ed.). Muthén & Muthén. [Google Scholar]
- Oravecz Z, Tuerlinckx F, & Vandekerckhove J (2011). A hierarchical latent stochastic differential equation model for affective dynamics. Psychological Methods, 16(4), 468–490. doi: 10.1037/a0024375 [DOI] [PubMed] [Google Scholar]
- Pe ML, Kircanski K, Thompson RJ, Bringmann LF, Tuerlinckx F, Mestdagh M, … Gotlib IH (2014). Emotion-network density in major depressive disorder. Clinical Psychological Science, 3(2), 292–300. doi: 10.1177/2167702614540645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pe ML, & Kuppens P (2012). The dynamic interplay between emotions in daily life: Augmentation, blunting, and the role of appraisal overlap. Emotion, 12(6), 1320–1328. doi: 10.1037/a0028262 [DOI] [PubMed] [Google Scholar]
- Prinstein MJ, Boergers J, & Vernberg EM (2001). Overt and relational aggression in adolescents: Social-psychological adjustment of aggressors and victims. Journal of Clinical Child and Adolescent Psychology, 30(4), 479–491. doi: 10.1207/S15374424JCCP3004_05 [DOI] [PubMed] [Google Scholar]
- Rafaeli E, Rogers GM, & Revelle W (2007). Affective synchrony: Individual differences in mixed emotions. Personality and Social Psychology Bulletin, 33(7), 915–932. doi: 10.1177/0146167207301009 [DOI] [PubMed] [Google Scholar]
- Ruiz MA, Pincus AL, & Schinka JA (2008). Externalizing pathology and the Five-Factor Model: A meta-analysis of personality traits associated with antisocial personality disorder, substance use disorder, and their co-occurrence. Journal of Personality Disorders, 22(4), 365–388. doi: 10.1521/pedi.2008.22.4.365 [DOI] [PubMed] [Google Scholar]
- Santangelo PS, Limberger MF, Stiglmayr C, Houben M, Coosemans J, Verleysen G, … Ebner-Priemer UW (2016). Analyzing subcomponents of affective dysregulation in borderline personality disorder in comparison to other clinical groups using multiple e-diary datasets. Borderline Personality Disorder and Emotion Dysregulation, 3(1), 5. doi: 10.1186/s40479-016-0039-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott LN, Wright AGC, Beeney JE, Lazarus SA, Pilkonis PA, & Stepp SD (2017). Borderline personality disorder symptoms and aggression: A within-person process model. Journal of Abnormal Psychology, 126(4), 429–440. doi: 10.1037/abn0000272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schultzberg M & Muthén B (2018). Number of subjects and time points needed for multilevel time series analysis: A simulation study of dynamic structural equation modeling. Structural Equation Modeling: A Multidisciplinary Journal, 25(4), 495–515, doi: 10.1080/10705511.2017.1392862. [DOI] [Google Scholar]
- Shiffman S, Stone AA, & Hufford MR (2008). Ecological Momentary Assessment. Annual Review of Clinical Psychology, 4(1), 1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415 [DOI] [PubMed] [Google Scholar]
- Sosnowska J, Kuppens P, De Fruyt F, & Hofmans J (2019). A dynamic systems approach to personality: The Personality Dynamics (PersDyn) model. Personality and Individual Differences, 144, 11–18. 10.1016/j.paid.2019.02.013 [DOI] [Google Scholar]
- Spindler G, Stopsack M, Aldinger M, Grabe HJ, & Barnow S (2016). What about the “ups and downs” in our daily life? The influence of affective instability on mental health. Motivation and Emotion, 40(1), 148–161. doi: 10.1007/s11031-015-9509-7 [DOI] [Google Scholar]
- Trull TJ, Lane SP, Koval P, & Ebner-Priemer UW (2015). Affective Dynamics in Psychopathology. Emotion Review, 7(4), 355–361. doi: 10.1177/1754073915590617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trull TJ, Solhan MB, Tragesser SL, Jahng S, Wood PK, Piasecki TM, & Watson D (2008). Affective instability: Measuring a core feature of borderline personality disorder with ecological momentary assessment. Journal of Abnormal Psychology, 117, 647–661. [DOI] [PubMed] [Google Scholar]
- Watson D, & Clark LA (1999). The PANAS-X: Manual for the positive and negative affect schedule-expanded form.
- Watson D, Stasik SM, Ellickson-Larew S, & Stanton K (2015). Extraversion and psychopathology: A facet-level analysis. Journal of Abnormal Psychology, 124(2), 432–46. [DOI] [PubMed] [Google Scholar]
- Wolf EJ, Miller MW, Harrington KM, & Reardon A (2012). Personality-based latent classes of posttraumatic psychopathology: personality disorders and the internalizing/externalizing model. Journal of Abnormal Psychology, 121(1), 256–262. doi: 10.1037/a0023237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zautra AJ, Potter PT, & Reich JW (1997). The independence of affects is context-dependent: An integrative model of the relationship between positive and negative affect In Warner Schaie K & Powell Lawton M (Series Ed.), Focus on Emotion and Adult Development: Vol. 17. Annual Review of Gerontology and Geriatrics. Springer. [Google Scholar]
- Zuckerman M (1996). The psychobiological model for impulsive unsocialized sensation seeking: A comparative approach. Neuropsychobiology, 34(3), 125–129. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.