Abstract
Rationale:
Perceived neighborhood characteristics have been linked to cognitive health in older adulthood. The pathways through which neighborhood characteristics could influence cognition in older adulthood, however, have not been fully explored. Poorer quality neighborhoods may negatively influence cognition through feelings of psychological distress.
Objective:
To examine whether perceived neighborhood physical disorder and social cohesion were associated with change in episodic memory and semantic verbal fluency through anxiety and depressive symptoms.
Methods:
Using the Health and Retirement Study (HRS; n = 13,919), mediation models were conducted. Change in cognition (episodic memory and semantic verbal fluency) were modeled using latent growth curve models.
Results:
Higher physical disorder was associated with worse initial episodic memory and verbal fluency through greater anxiety symptoms. Higher social cohesion was associated with better initial episodic memory and verbal fluency through both lower anxiety and fewer depressive symptoms. Further, individuals with higher social cohesion reported lower anxiety and in turn, showed a slower rate of verbal fluency decline. A direct effect of physical disorder on initial episodic memory remained, after accounting for indirect effects and covariates.
Conclusions:
Overall, individuals who live in neighborhoods with high physical disorder and low social cohesion may experience greater psychological distress. Symptoms of anxiety and depression, in turn, interfere with cognitive functioning. Neighborhood characteristics may be an important, targetable area for intervention to improve not only mental health outcomes, but cognitive health outcomes in older adulthood.
Introduction
Prior research has shown that age is associated with less time spent outdoors such that older adults tend to spend a majority of their time within their homes (Horgas et al., 1998; Spalt et al., 2016). Therefore, an individual’s surrounding neighborhood environment may be especially important for health-related outcomes in older adulthood. Consistent with this notion, prior research has demonstrated that older adults are at greater risk of the negative consequences of poor neighborhood environments compared to other sociodemographic groups (Whitley & Prince, 2005). Thus, neighborhood quality may be an important target for intervention to help preserve health and quality of life in older adulthood.
Neighborhood Characteristics and Cognitive Aging
Neighborhood characteristics may have important specific implications for cognitive health in older adulthood. For instance, individuals’ experiences in their neighborhoods may impede or facilitate the formation of social connections. Social interactions provide beneficial cognitive stimulation that may promote better cognitive aging (Bennett et al., 20016) in line with the theory of cognitive reserve (Stern, 2002). Objective indicators of neighborhood quality (i.e., crime rates, socioeconomic composition) have been consistently linked to cognitive health outcomes (Clarke et al., 2012; Clarke et al., 2015; Friedman et al., 2017). Some recent evidence, however, suggests that subjective perceptions of neighborhood quality play a more prominent role in explaining cognitive health than objective indicators (Lee & Waite, 2018).
Neighborhoods have several distinct characteristics that independently influence cognition in later life. In particular, perceptions of neighborhood physical disorder (i.e., presence of graffiti, liter, vandalism, and feelings of safety) and neighborhood social cohesion (i.e., mutual trust, solidarity among residents) independently contribute to cognitive health outcomes. For example, in a cross-sectional investigation, greater neighborhood physical disorder was associated with worse episodic memory, and lower neighborhood social cohesion was associated with worse semantic verbal fluency (Zaheed et al., 2019). In another cross-sectional study, controlling for sociodemographics and objective neighborhood characteristics, both perceived danger and social cohesion were independently associated with cognition (Lee & Waite, 2018). Additional cross-sectional evidence has further linked higher perceived social cohesion to better global cognition, better episodic memory, and better executive functioning in older adults (Zhang et al., 2019).
Although preliminary cross-sectional evidence has linked perceived neighborhood characteristics to cognitive functioning in later life (i.e., Lee & Waite, 2018; Zaheed et al., 2019; Zhang et al., 2019), much less is known regarding the specific pathways through which subjective perceptions of neighborhood characteristics might influence later-life cognitive trajectories. One potential pathway by which perceived neighborhood characteristics could influence later life cognition is through psychological distress. Older adults who reside within highly disordered and socially fragmented neighborhoods may experience poorer psychological outcomes due to fear of crime and perceptions of mistrust (Pearson et al., 2015; Whitley & Prince, 2005). Therefore, the current study aimed to explore the mediating role of psychological distress in explaining the relationship between perceived neighborhood characteristics and cognitive trajectories in older adulthood.
Neighborhood Characteristics and Psychological Distress
Perceived neighborhood characteristics may, in part, influence cognition through psychological distress. Anxiety and depressive symptomology may be especially influenced by perceptions of the physical context of one’s neighborhood. Individuals who live in highly disordered and socially fragmented neighborhoods are more likely to be victimized (i.e., being robbed; Sampson & Raudenbush, 1999) and, therefore, be hypervigilant toward potential environmental threats. Indeed, prior quasi-experiment research has shown that when adults are relocated to better neighborhoods, individuals are less likely to witness disorder and/or violence in their neighborhoods and, in turn, report fewer stressful life events and less anxiety (Casciano & Massey, 2012). Further, in a daily diary study, individuals who reported greater neighborhood violence also rated their daily stressors as more severe and experienced greater emotional reactivity (higher negative affect) when exposed to daily stressors (Scott et al., 2018). Overall, individuals who live in highly disordered neighborhoods are more likely to view their neighborhoods as threatening and hazardous, which has negative implications for mental health outcomes such as anxiety and depression (Aneshensel & Sucoff, 1996 Gary et al., 2007; Ivey et al., 2015;).
Similar to neighborhood physical disorder, perceptions of the neighborhood’s social environment also have implications for psychological functioning. Higher neighborhood social cohesion has been linked to fewer depressive symptoms cross-sectionally (Choi et al., 2015; Gary et al., 2007; Ivey et al., 2015) as well as longitudinally (Ruiz et al., 2018; 2019). For example, individuals who perceived that their neighbors were unwilling to help each other also reported higher levels of depressive symptoms (Ivey et al., 2015). Higher neighborhood social cohesion has also been linked to lower levels of stress and anxiety (Gary et al., 2007; Henderson et al., 2016). For example, in a daily diary study, individuals who lived in more cohesive neighborhoods exhibited less negative affect reactivity to daily stressors (Robinette et al., 2013).
Psychological Distress and Cognitive Aging
Symptoms of anxiety are a known risk factor for late-life cognitive decline and impairment (Becker et al., 2018). For instance, greater anxiety has been linked to worse memory and executive functioning among older adults (Yochim et al., 2013) as well as higher risk of cognitive impairment and dementia (Gallacher et al., 2009). Anxiety has negative implications for cognitive functioning through the depletion of available cognitive resources (Eysenck et al., 2007). Further, anxiety also triggers a physiological stress response and impairs cognitive functioning through dysregulation of the hypothalamic pituitary adrenal axis (i.e., HPA; Beaudreau & O’Hara, 2008; Furtado & Katzman, 2015).
Similarly, depressive symptoms are also a known risk factor for late-life cognitive decline and impairment (see review; Byers & Yaffe, 2012). More depressive symptoms have been prospectively linked to greater memory decline (Lohman et al., 2013; Zahodne, Stern & Manly, 2014) as well as greater decline in executive functioning (Brewster et al., 2017; Lockwood et al., 2002; Rapp et al., 2005). Depressive symptoms negatively influence cognitive functioning through multiple pathways, such as disengagement from beneficial activities that may promote cognitive reserve (Sharifian et al., 2020) as well as the extended release of glucocorticoids and subsequent hippocampal atrophy, which increases risk of cognitive impairment (Byers & Yaffe, 2012).
Overall, both anxiety and depressive symptoms have previously been identified as risk factors for later life cognitive impairment (Becker et al., 2008; Bierman et al., 2005; Byers & Yaffe, 2012). It may be that neighborhood characteristics influence later-life cognition through these markers of psychological distress.
The Present Study
The current study aimed to more fully examine longitudinal associations between perceived neighborhood characteristics and cognitive functioning in older adulthood. Prior research assessing links between perceived neighborhood characteristics and cognition have been predominantly cross-sectional in nature (i.e., Lee & Waite, 2018; Zaheed et al., 2019; Zhang et al., 2019) and thus, an examination of longitudinal associations may help to clarify the impact of neighborhood environmental context on cognitive aging processes. Thus, the first aim was to examine associations between perceived neighborhood characteristics and both initial levels and rates of change in episodic memory and verbal fluency. Second, this study aimed to extend past research by examining potential psychological mediators of these relationships. Specifically, we were interested in whether anxiety and depressive symptoms mediate the relationship between perceived neighborhood characteristics and cognitive trajectories. We hypothesized that higher neighborhood disorder and lower neighborhood social cohesion would be associated with greater anxiety and depressive symptoms, and in turn, would be associated with worse initial cognitive functioning and faster cognitive decline.
Method
Participants
Four waves of data from the Health and Retirement Study (HRS; Sonnega & Weir, 2014) were utilized in the current study (2010 – 2016). HRS is a nationally representative sample of Americans over age 50 followed biennially since 1992. More information regarding HRS’ design, sampling, and all assessment instruments are available on the HRS website (https://hrsoline.isr.umich.edu).
During the biennial interviews, participants underwent cognitive testing. Starting in 2006, a rotating 50% of the sample engaged in an in-person home interview and a psychosocial leave-behind questionnaire that included perceived neighborhood characteristics and anxiety symptoms. While the inclusion of the psychosocial questionnaire was initiated in 2006, it was not until 2010 that HRS introduced new measures of fluid cognition, specifically semantic verbal fluency, allowing for an examination of distinct domains of cognitive functioning (Fisher et al., 2013). As the psychosocial leave-behind questionnaire is given to a rotating 50% of the sample at any given wave, data on perceived neighborhood characteristics and the expanded cognitive battery were first available for half the sample in 2010, and the other half in 2012. To maximize sample size in the current study, these two subsamples were combined, and the baseline assessment was defined as this combined 2010/2012 wave. These individuals were then followed longitudinally two and four years later (2012/2014; 2014/2016). In other words, individuals with a 2010 baseline (T1) assessment were followed up in 2012 (T2) and 2014 (T3). Individuals with a 2012 baseline (T1) assessment were followed up in 2014 (T2) and 2016 (T3). Thus, all participants were followed biennially over a 4 year period (T1: 2010/2012; T2: 2012/2014; T3: 2014/2016).
Inclusion criteria for the current analyses were (1) age 51 or older, (2) available data on perceived neighborhood characteristics, and (3) not currently residing in a nursing home or institution. Descriptive statistics on the 13,919 participants included in the current study appear in Table 1. All participants provided written informed consent and all study procedures were approved by the University of Michigan’s institutional review board.
Table 1.
Unweighted Means and Standard Deviations of Variables of Interest at Time 1
| M | SD | Initial Wave Comparison | |
|---|---|---|---|
| Age | 67.55 | 10.40 | 2010 < 2012 |
| Female (%) | 58.50 | - | 2010 = 2012 |
| African American (%) | 15.80 | - | 2010 = 2012 |
| Hispanic (%) | 10.20 | - | 2010 < 2012 |
| Non-Hispanic Other (%) | 2.70 | 2010 = 2012 | |
| 2010 initial assessment (%) | 52.40 | - | - |
| Education | 12.92 | 2.97 | 2010 = 2012 |
| Chronic Illness Burden | 1.91 | 1.29 | 2010 < 2012 |
| Income (dollars) | 65510.11 | 92034.93 | 2010 < 2012 |
| Wealth (dollars) | 438202.72 | 886833.10 | 2010 = 2012 |
| Neighborhood Physical Disorder (T1) | 2.60 | 1.45 | 2010 = 2012 |
| Neighborhood Social Cohesion (T1) | 5.39 | 1.41 | 2010 > 2012 |
| Anxiety (T1) | 1.56 | 0.60 | 2010 = 2012 |
| Depressive Symptoms (T1) | 1.37 | 1.94 | 2010 = 2012 |
| Memory (T1) | .00 | 0.93 | 2010 > 2012 |
| Memory (T2) | .01 | 1.02 | 2010 < 2012 |
| Memory (T3) | −.05 | 0.95 | 2010 > 2012 |
| Fluency (T1) | 16.84 | 7.04 | 2010 < 2012 |
| Fluency (t2) | 15.93 | 6.93 | 2010 > 2012 |
| Fluency (t3) | 15.68 | 6.54 | 2010 = 2012 |
Note. One-way analysis of variance (ANOVA) were conducted to compare differences across participants who had the 2010 versus 2012 initial assessment wave. Less than and greater than symbols indicates significant differences whereas equal signs indicates nonsignificant differences.
Measures
Perceived Neighborhood Characteristics.
Two domains of perceived neighborhood characteristics were measured at T1 (2010 or 2012): neighborhood physical disorder and neighborhood social cohesion. Neighborhoods were defined as the respondent’s local area, or everywhere within a 20-minute walk or about a mile from their home.
Neighborhood physical disorder (NPD) was assessed with 4 items regarding perceptions of vandalism/graffiti, litter, vacant/deserted homes, and crime. Participants rated their perceptions of physical disorder in their neighborhood on a 7-point Likert-type scale based on their agreement with each set of opposing statements: “There is no problem with vandalism and graffiti in this area (1) / Vandalism and graffiti are a big problem in this area (7),” “People feel safe walking alone in this area after dark (1) / People would be afraid to walk alone in this area after dark (7),” “This area is kept very clean (1) / This area is always fully of rubbish and litter (7),” and “There are no vacant or deserted houses or storefronts in this area (1) / There are many vacant or deserted houses or storefronts in this area (7).” An NPD index was created by averaging responses across all items (α = .82) with higher scores representing greater perceived neighborhood physical disorder.
Neighborhood social cohesion (NSC) was assessed with 4 items regarding perceptions of trust and belonging within one’s neighborhood. Participants rated their perceptions of social cohesion on a 7-point Likert-type scale based on their agreement with each set of opposing statements: “I really feel part of this area (1) / I feel that I don’t belong in this area (7),” “Most people in this area can be trusted (1) / Most people in this area can’t be trusted (7),” “If you were in trouble, there are lots of people in this area who would help you (1) / If you were in trouble, there is nobody in this area who would help you (7),” and “most people in this area are friendly (1) / Most people in this area are unfriendly (7).” Items were reverse-coded, and a NSC index was created by averaging scores across all items (α = .86) such that higher scores indicated grater perceived social cohesion.
Depressive Symptoms.
At baseline, depressive symptoms over the past week were assessed using the 8-item version of the Center for Epidemiologic Studies Depression scale (CES-D; Radloff, 1977). Participants rated items such as “was depressed” and “sleep was restless” on a binary Yes (1) and No (0) scale. Scores across items were summed such that higher scores represented more depressive symptoms.
Anxiety Symptoms.
At baseline, anxiety was assessed with 5 items from the Beck Anxiety Inventory (BAI; Beck et al., 1988; Wetherell & Areán, 1997). Participants were asked to rate how often items such as “I had a fear of the worst happening” and “I felt my hands trembling” happened during the past week on a 4-point scale ranging from Never (1) to Most of the time (4). Responses were averaged across the items to create an index of anxiety, with higher scores representing greater anxiety (α = .82).
Cognition.
Two domains of cognitive functioning were assessed across all waves: episodic memory and semantic verbal fluency. Episodic memory was assessed using the HRS variant of the Consortium to Establish a Registry for Alzheimer’s Disease (CERAD; Ofstedal et al., 2006; Weir et al., 2014) word list learning task. Participants heard a list of 10 words once and were asked to recall those words immediately and again after a 5-minute delay during which they completed other tasks related to the interview. Consistent with prior research (i.e., Lim et al., 2016), episodic memory was calculated by converting the raw scores on the immediate and delayed recall trials into z-scores using means and standard deviations from baseline and then averaging the immediate and delayed z-scores to create an episodic memory composite score in order to improve reliability.
Verbal fluency was assessed using an animal fluency task (i.e., semantic verbal fluency; Fisher et al., 2013; Henry et al., 2004; Rosen, 1980). Participants were asked to name as many animals as they could in one minute. A semantic verbal fluency score was computed as a total number of correct responses, excluding repetitions.
Covariates.
As individuals within certain neighborhood types may be more similar than individuals between neighborhoods due to social stratification processes, it was important to account for sociodemographic, socioeconomic, and health factors that may influence selection into these neighborhoods. Additionally, as older adults with more health conditions may experience their neighborhoods differently than healthy individuals (i.e., due to mobility limitations) and chronic illness burden has been linked to worse mental and cognitive health, chronic illness burden was additionally included as a covariate. Therefore, all analyses controlled for baseline age, education, gender, race, ethnicity, chronic illness burden, income, wealth, and initial assessment wave (2010 or 2012).
Age was self-reported and represented as a continuous variable. Gender was a binary variable with male as the reference group. Race and ethnicity were self-reported and was dummy coded into four, mutually exclusive categories: non-Hispanic White, non-Hispanic Black, non-Hispanic Other, and Hispanic of any race (non-Hispanic White as the reference group). Number of years of education was self-reported (0–17). Total income was calculated by summing the respondent’s and their spouse’s income from all sources (i.e., earnings, pensions, etc.) during the initial assessment wave. Net wealth at the initial assessment wave was calculated by as the difference between the sum all wealth from all sources (i.e., property value, vehicles, etc.) minus the sum of all debts (i.e., mortgages, loans, etc.). Pre-calculated income and wealth variables were obtained from the RAND longitudinal file available on the HRS website. Chronic illness burden was calculated by summing the number of self-reported chronic diseases: diabetes, cancer, lung disease, heart problems, hypertension and arthritis. Finally, because the psychosocial leave-behind questionnaire is administered to alternating subsets of the HRS participants, initial assessment (2010 or 2012) was included in the model as a covariate to adjust for any failures of randomization.
Analytic Strategy
To address our research questions, initial latent growth curve models were conducted separately for episodic memory and verbal fluency, controlling only for centered age, to assess whether there was sufficient variability in interindividual change in each domain over the 4-year period. Subsequently, latent growth curve models were conducted separately for each of our dependent variables (memory, fluency), and the structure of these models are depicted in Figure 1. As shown, anxiety and depressive symptoms were regressed onto neighborhood physical disorder and neighborhood social cohesion and were allowed to covary. Neighborhood physical disorder and social cohesion were also allowed to covary. Time was parameterized as years from T1 (2010 or 2012). The intercept and slope of each cognitive domain were both regressed onto anxiety and depressive symptoms, as well as physical disorder and social cohesion, controlling for covariates. Exposure variables and mediators were also regressed onto covariates.
Fig. 1.
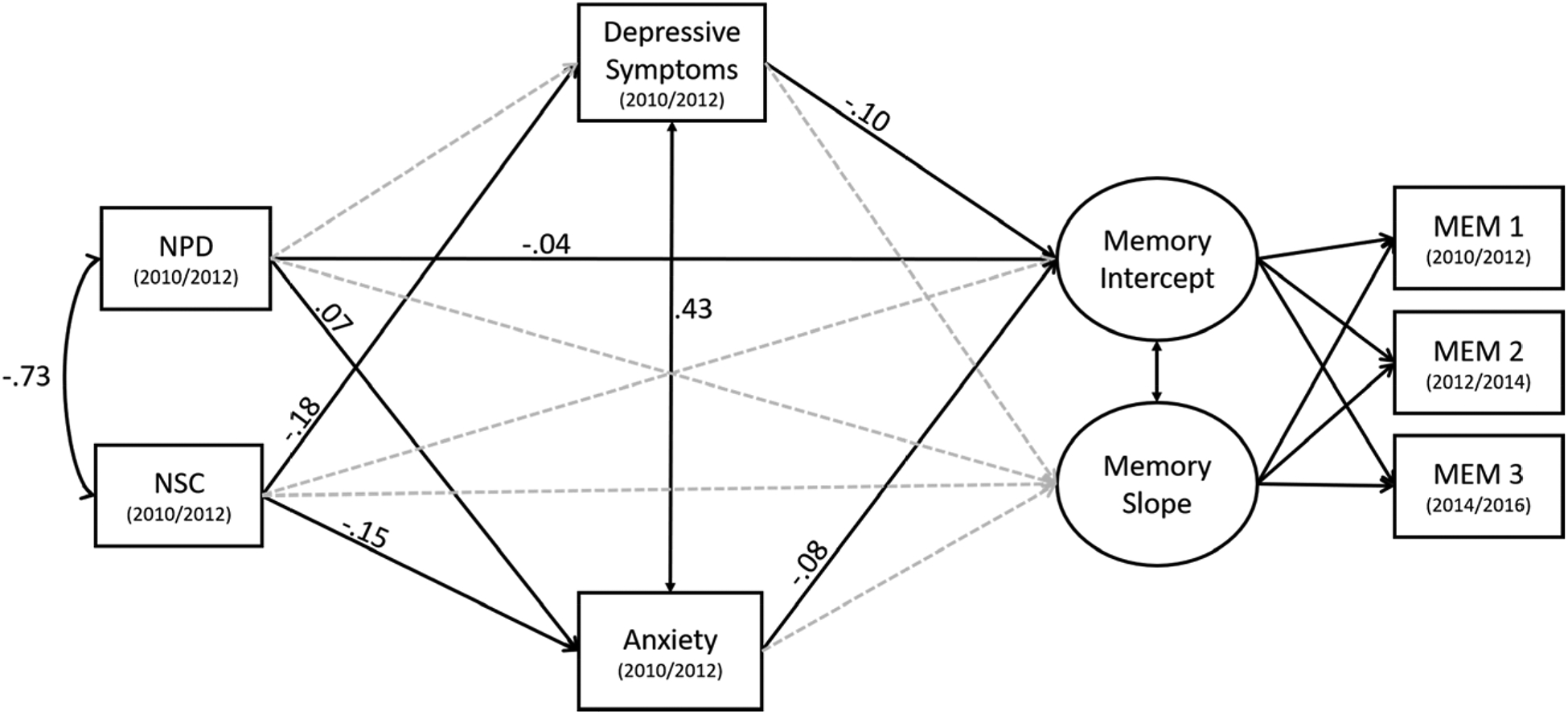
Mediational Pathways from Neighborhood Characteristics to Episodic Memory. Standardized estimate are reported. Significant pathways are represented by solid, black lines and nonsignificant pathways are represented by gray, dotted lines. For simplicity, covariate pathways are not depicted.
Missing data were managed with maximum likelihood with robust standard errors. Indirect effects were defined as the product of the association between a neighborhood characteristic (physical disorder or social cohesion) and a mediator (anxiety or depressive symptoms) and the association between that mediator and an outcome (initial cognition or cognitive change), independent of all covariates. Direct effects were defined as associations between a neighborhood characteristic and an outcome (i.e., initial cognition or cognitive change), independent of all mediators and covariates.
Model fit was determined based on fit indexes: Tucker-Lewis Index (TLI) and Comparative Fix Index (CFI) approximately .95 and a root mean squared error of approximation (RMSEA) of .06 or lower (Hu & Bentler, 1999). Descriptive statistics and correlations were calculated in SPSS (Version 25). The longitudinal mediation model was conducted in Mplus (Version 8; Muthén & Muthén, 2007). Finally, the current analyses were weighted using HRS psychosocial leave-behind sample weights from baseline. The use of sample weights allows for findings to be generalizable to the larger U.S population of adults over age 50.
Results
Unweighted descriptive statistics and correlations for main variables of interest are listed in Table 1 and Table 2, respectively. In the age-adjusted verbal fluency model, verbal fluency significantly declined over time (b= −.11, SE= .03, p< .001) and demonstrated significant interindividual change over time (b= .45, SE= .21, p= .035). The intercept of fluency was also significantly different from zero (b= 17.81, SE= .07, p< .001) and demonstrated significant variability (b= 29.30, SE= 1.68, p< .001). In the age-adjusted episodic memory model, episodic memory significantly decline over time (b= −.02, SE= .002, p< .001), however, did not demonstrate sufficient variability in interindividual change in memory over the 4-year period and therefore, the residual variance of memory slope was fixed to zero. The intercept of memory was significantly different from zero (b= .11, SE= .01, p< .001) and showed significant variability (b= .45, SE= .01, p< .001).
Table 2.
Unweighted Correlations between Neighborhood Characteristics, Mental Health and Cognitive Functioning
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. NPD | ||||||||||
| 2. NSC | −.77 | |||||||||
| 3. Depress | .17 | −.21 | ||||||||
| 4. Anxiety | .21 | −.22 | .48 | |||||||
| 5. T1 Memory | −.11 | .09 | −.16 | −.14 | ||||||
| 6. T2 Memory | −.09 | .08 | −.15 | −.14 | .53 | |||||
| 7. T3 Memory | −.10 | .07 | −.15 | −.12 | .60 | .57 | ||||
| 8. T1 Fluency | −.09 | .07 | −.13 | −.11 | .41 | .35 | .39 | |||
| 9. T2 Fluency | −.10 | .06 | −.13 | −.13 | .39 | .38 | .41 | .61 | ||
| 10. T3 Fluency | −.13 | .09 | −.13 | −.13 | .39 | .37 | .45 | .59 | .61 |
Note. All correlations are statistically significant, p < .001. NPD = neighborhood physical disorder, NSC = neighborhood social cohesion, Depress= depressive symptoms.
Episodic Memory
Model fit was good for the episodic memory latent growth curve model, χ2 (17)= 97.01, CFI= .99, TLI= .98, RMSEA= .02 [.01, .02], p= 1.00, SRMR= .01, and standardized estimates are depicted in Figure 1. All covariate associations are described in Supplementary Table 1.
Intercept.
Significant indirect effects through anxiety emerged for both neighborhood social cohesion (standardized indirect effect= .01, SE= .002, p< .001) and neighborhood physical disorder (standardized indirect effect= −.01, SE= .002, p= .001). Higher social cohesion was associated with lower anxiety (β= −.15, SE= .02, p< .001) and in turn, lower anxiety is associated with higher initial memory (β= −.08, SE= .01, p< .001). Higher physical disorder was associated with higher anxiety (β= .07, SE= .02, p< .001) and in turn, lower initial memory (see estimate above).
A significant indirect effect through depressive symptoms also emerged, but only for social cohesion (standardized indirect effect= .02, SE= .003, p< .001). Higher social cohesion was associated with fewer depressive symptoms (β= −.18, SE= .02, p< .001) and fewer depressive symptoms was associated with higher initial memory scores (β= −.10, SE= .01, p< .001). Neighborhood physical disorder was not associated with depressive symptoms (β= −.004, SE= .02, p= .803). After accounting for mediators and covariates, there was no significant direct effect of social cohesion (β= .03, SE= .02, p= .075) on initial memory, but a significant direct effect of neighborhood physical disorder on initial memory remained (β = −.04, SE = .02, p = .024). Specifically, higher neighborhood physical disorder was associated with lower initial episodic memory above and beyond anxiety and depressive symptoms.
Slope.
No significant effects of neighborhood physical disorder, neighborhood social cohesion, anxiety or depressive symptoms were found for the slope of memory (ps > .22).
Verbal Fluency
Model fit was good for the verbal fluency latent growth curve model, χ2 (15)= 68.68, CFI= .99, TLI= .98, RMSEA= .02 [.01, .02], p= 1.00, SRMR= .01 and standardized estimates are depicted in Figure 2. All covariate associations are described in Supplementary Table 1.
Fig. 2.
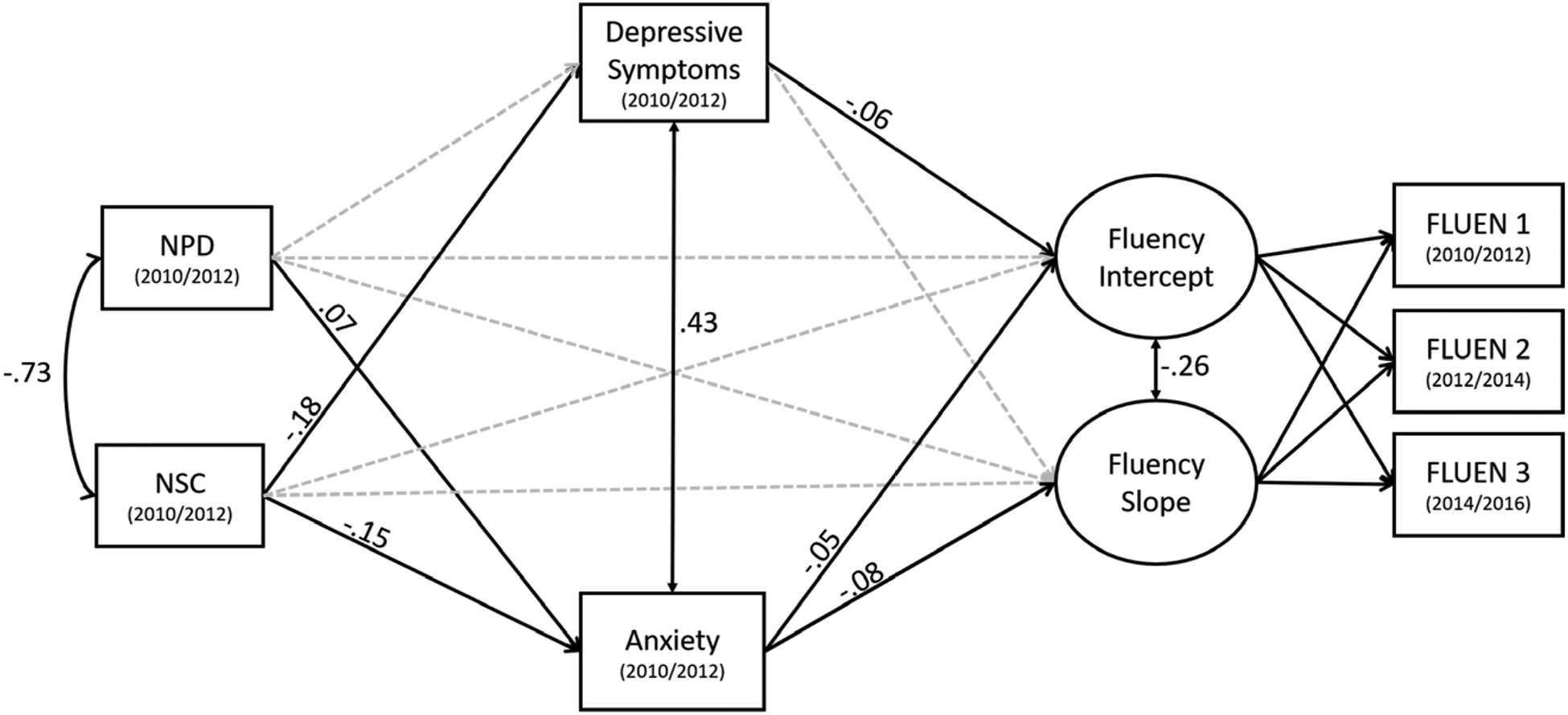
Mediational Pathways from Neighborhood Characteristics to Verbal Fluency. Standardized estimate are reported. Significant pathways are represented by solid, black lines and nonsignificant pathways are represented by gray, dotted lines. For simplicity, covariate pathways are not depicted.
Intercept.
For both neighborhood social cohesion (standardized indirect effect= .01, SE= .002, p< .001) and neighborhood physical disorder (standardized indirect effect= −.003, SE= .01, p= .005), anxiety significantly mediated their associations with initial fluency. That is, higher social cohesion (β= −.15, SE= .02, p< .001) and higher physical disorder (β= .07, SE= .02, p< .001) were associated with lower and higher anxiety, respectively. In turn, higher anxiety was associated with lower initial fluency (β= −.05, SE= .01, p< .001).
Further, depressive symptoms mediated the relationship between neighborhood social cohesion and initial fluency (standardized indirect effect= .01, SE= .003, p< .001). Higher social cohesion was associated with fewer depressive symptoms (β= −.18, SE= .02, p< .001) and in turn, fewer depressive symptoms were associated with higher initial fluency scores (β= −.06, SE= .01, p< .001). Neighborhood physical disorder was not significantly associated with depressive symptoms (β= −.004, SE= .02, p= .803). After accounting for mediators and covariates, no direct effects for social cohesion (β= .02, SE= .02, p= .167) or physical disorder (β= −.01, SE= .02, p= .726) remained.
Slope.
Anxiety significantly mediated the relationship between neighborhood social cohesion and the rate of verbal fluency change (standardized indirect effect= .01, SE= .01, p= .043). Higher social cohesion was associated with lower anxiety (see estimate above) and in turn, lower anxiety was associated with less decline in fluency over time (β= −.08, SE= .04, p= .039). Although higher neighborhood disorder was significantly associated with greater anxiety (see estimate above) and greater anxiety was associated with the slope of verbal fluency (see prior estimate), no significant indirect effect of physical disorder emerged (standardized indirect effect= −.01, SE= .003, p= .068). After accounting for mediators and covariates, no direct effects of social cohesion (β= −.08, SE= .05, p= .163) or physical disorder (β= −.09, SE= .05, p= .092) on fluency change emerged.
Sensitivity Analyses.
Sensitivity analyses were conducted to assess the impact of (a) excluding individuals who changed residences and (b) simultaneously modeling both cognitive domains and allowing their intercepts and slopes to vary (See Supplementary Materials). Importantly, our pattern of findings did not change.
Discussion
The current study aimed to clarify the underlying pathways linking perceived neighborhood characteristics and longitudinal trajectories of cognition. Overall, neighborhood social cohesion was linked to better cognition through both anxiety and depressive symptoms (See Figure 1), whereas negative associations between neighborhood physical disorder and cognition operated only through anxiety (see Figure 2). Specifically, we found that physical disorder was associated with lower initial levels of both episodic memory and verbal fluency through anxiety. Social cohesion was associated with higher initial levels of both episodic memory and verbal fluency through both anxiety and depressive symptoms. Further, higher social cohesion was associated with better longitudinal trajectory of verbal fluency through lower anxiety symptoms. These findings suggest that these psychological pathways play an important role in explaining the relationship between neighborhood characteristics and cognition and may be an important targetable area for intervention. After accounting for these indirect effects, higher neighborhood physical disorder was still associated with lower initial episodic memory. This finding suggests additional mechanisms, such as exposure to pollution, could further explain the link between physical disorder and memory functioning. Future research should investigate these additional pathways.
Neighborhood Context, Anxiety, and Cognitive Aging
Consistent with our hypothesis, individuals who lived in more physically disordered and less socially cohesive neighborhoods reported a greater level of anxiety. This finding coincides with prior research linking neighborhood characteristics to psychological distress in older adulthood (Brown et al., 2009; Choi & Matz-Costa, 2018; Weisburd et al., 2018). For example, in a study examining Hispanic older adults, those who lived in more positive neighborhood climates (i.e., self-reported positive and negative neighboring behaviors) had less anxiety, in part, due to greater availability of interpersonal social support (Brown et al., 2009).
Negative neighborhood characteristics alter perceptions of safety and fear of victimization, which could lead to greater experiences of anxiety. Indeed, neighborhood physical disorder, as rated by outside observers, has been linked to fear of crime (Taylor et al., 1984). When examining objective indicators of crime, individuals who lived in crime ‘hot spots’ (areas with a high concentration of crime) reported greater anxiety. Specifically, individuals who lived in crime hot spots had significantly greater reports of post-traumatic stress symptoms (i.e., hyperarousal, avoidance, etc.) compared to those who lived in ‘cold spots’ (Weisburd et al., 2018).
A disordered neighborhood environment may act as a chronic stressor and represent an underlying, persistent threat that elicits feelings of powerlessness and mistrust and in turn, greater stress and anxiety (Ross & Mirowsky, 2009). Consistently, socially fragmented neighborhoods may operate through the same mechanisms. Individuals who live in socially fragmented neighborhoods have previously been found to have a greater fear of violent and alcohol/drug-related crimes than those with low fragmentation (Pearson et al., 2015). If a neighborhood is perceived as being socially cohesive, individuals may feel more confident that others can be trusted or provide support in times of need. Feelings of trust and safety may further influence an older adults’ perceptions of when and where they can explore their neighborhoods. Prior research has shown that older adults who live in poorer neighborhood may experience ‘time and space inequalities’ such that they are concerned with staying out late or going to certain areas in their neighborhoods (Whitley & Prince, 2005). This may, in turn, restrict the level of activity engagement - whether social, physical, or cognitive - that help to maintain cognitive health in later life (i.e., Hultsch et al., 1999; Scarmeas et al., 2009; Zahodne et al., 2019).
Besides the potential restriction of engagement in beneficial activities, greater anxiety has also been directly linked to poorer cognitive functioning. Based on the processing efficiency theory (Eysenck & Calvo, 1992), state anxiety may negatively influence cognitive/task performance through the process of worrying, which utilizes some cognitive processing and storage resources. Anxiety also heightens arousal and depletes resources for self-regulation and attentional control.
Overall, poorer quality neighborhoods may increase anxiety and hypervigilance for potential threats of victimization. Older adults may be especially vulnerable to these negative neighborhood characteristics (Whitley & Prince, 2005) and thus, neighborhood characteristics may be an important targetable area for intervention to preserve mental, including cognitive, health outcomes. With the increase in population aging and the push towards ‘aging in place’ (i.e., older adults remaining in their own residences rather than institutions/communities), subjective neighborhood characteristics are one avenue in which the aging in place process can be optimized. At the individual level, increasing the functionality of an older adult’s residence (e.g., installing grab-bars, etc.) and access to care services (e.g., food delivery, etc.) may help older adults maintain quality of life within their own homes. At the community level, targeting subjective neighborhood characteristics can have broader effects for improving quality of life for older adults. For example, prior research has shown that the surrounding area to an older adult’s residence, such as cafes, local businesses and public transit, helps to facilitate healthy and beneficial social ties to the community (Gardner, 2011). Therefore, reducing the amount of perceived physical disorder and facilitating social cohesiveness within one’s community through neighborhood modification could increase comfort to explore and engage with one’s surrounding community. As anxiety was significantly associated with not only initial levels of episodic memory and verbal fluency, but the longitudinal trajectory of verbal fluency, this suggests that anxiety plays an important role in explaining individual differences in the rate of age-normative cognitive decline in later life. Future interventions targeting modifiable neighborhood characteristics may be especially relevant for older adults with fewer economic resources or have health concerns that restrict their ability to move to a different neighborhood to help reduce current health inequalities. Of note, future policy and intervention work could also use this information more broadly to affect change and reduce the negative impact of neighborhood characteristics on cognitive functioning throughout the lifespan in the general population (see proportionate universalism; Marmot & Bell, 2012).
Neighborhood Social Cohesion, Depressive Symptoms, and Cognitive Aging
Individuals who lived in more socially cohesive neighborhoods also reported fewer depressive symptoms, consistent with our hypothesis. Social engagement is a known protective factor for depressive symptoms (Glass et al., 2006), and prior research has consistently shown that older adults who are socially integrated report fewer depressive symptoms (Barger et al., 2014; Ramos & Wilmoth, 2003). When specifically examining social integration at the community level, prior research examining Chinese older adults who had a strong sense of community had lower risk of depression (Tang et al., 2018). Further, distinct aspects of one’s sense of community, such as feelings of belongingness (membership), a sense of mattering (influence), fulfilment of needs, and a sense of commitment (emotional connection), were all associated with lower risk for depression (Tang et al., 2018). Depressive symptoms, in turn, are a salient risk factor for decline in cognitive functioning (Lohman et al., 2013; Sharifian et al., 2020; Zahodne et al, 2014). Of note, only cross-sectional associations between depressive symptoms and both episodic memory and verbal fluency emerged. This may be because of the relatively short follow-up period. Prior research has shown an association between depressive symptoms and cognition when examined with substantially longer follow-up periods (i.e., Lohman et al., 2013). We cannot, however, rule out the possibility of reverse causation. That is, those who have poorer cognitive functioning may have greater depressive symptoms, consistent with the idea that depressive symptoms are a psychological reaction to cognitive impairment rather than a risk factor per se (see review, Jorm, 2000). Further investigation is necessary to clarify the association between neighborhood characteristics, depressive symptoms and cognitive functioning in later life.
The current study did not find a significant association between neighborhood physical disorder and depressive symptoms, inconsistent with our hypothesis and prior empirical research (Latkin & Curry, 2003; Weisburd et al., 2018; Wilson-Genderson & Pruchno, 2013). It may be important to note that prior research examining the link between neighborhood physical disorder and depressive symptoms did not also include anxiety symptoms within their model. Our current investigation modeled both pathways simultaneously and allowed them to covary revealing that anxiety and depressive symptoms were moderately correlated with one another. Therefore, it may be the case that some of the association between physical disorder and depressive symptoms is attributable to experiences of anxiety. Future research is necessary to disentangle the relationship between neighborhood physical disorder, anxiety and depressive symptoms.
Strengths, Limitations, and Future Directions
Although the current study has several notable strengths, such the use of longitudinal data, the simultaneous modeling of both anxiety and depressive symptoms to disentangle their independent effects on cognition and the use of sampling weights to increase generalizability of our findings to a representative U.S. sample, there are also some notable limitations. First, although three time points of data from HRS were used, the current study utilized concurrent waves of our exposure (neighborhood characteristics) and our mediators (psychological distress). This was done because anxiety and depressive symptoms were measured on a short-term scale (within the past week) and was deemed theoretically inappropriate to lag. Additionally, information on anxiety was only available every 4 years (i.e., in the psychosocial leave-behind questionnaire). If mediators were lagged, we would have been unable to look at longitudinal trajectories (i.e., slopes) of cognition. Therefore, the current study cannot disentangle the directionality of associations between neighborhood characteristics and psychological distress. Of note, prior quasi-experimental research did find a reduction in psychological distress in individuals who were moved out of highly disordered neighborhoods and relocated to better neighborhoods (Casciano & Massey, 2012), supportive of the proposed directionality.
Second, although our study is longitudinal in nature and the sample declined significantly, we did not find sufficient interindividual variability in memory change. This lack of variability may reflect the relatively short follow-up period (i.e., four years) and/or the relatively young age of our sample. Future studies should investigate the associations between neighborhood characteristics and cognition in older samples over longer follow-up periods. Relatively low interindividual variability in change may have also limited our ability to detect predictors of change. Specifically, we found multiple mediating pathways involving initial levels of both memory and verbal fluency whereas we found only one indirect effect involving verbal fluency change. It is important to note, however, that initial level of cognitive functioning is a critical determinant of incident dementia, as individuals who start out closer to an impairment threshold will reach that threshold faster than individuals who start our further from the threshold, even if they show an identical rate of decline. Thus, interventions that preserve or boost older adults’ initial levels of cognitive functioning without altering subsequent decline may still have the potential to delay the clinical onset of dementia.
Third, prior research has suggested that residential stability is an important factor when assessing the impact of neighborhood characteristics on health-related outcomes (Subramanian et al., 2006). Future research should further examine whether residential stability moderates these associations. Third, the current study utilized measures of subjective neighborhood characteristics which may, in part, be driven by objective neighborhood characteristics (e.g., neighborhood poverty). Although we do control for individual-level socioeconomic status (i.e., wealth, income, education), future research should further investigate the neighborhood-level SES, as well as other structural determinants of subjective neighborhood perceptions, in relation to psychological and cognitive functioning.
Additionally, prior research has made valid criticisms regarding neighborhood research regarding social stratification (or selective social mobility) (see review; Oakes, 2004). Specifically, individuals clustered within neighborhoods tend to be inherently more similar to one another than between-neighborhoods. Individuals are selected into poorer or higher quality neighborhoods based on sociodemographic, socioeconomic or health-related factors. Thus, a common fallacy of neighborhood research is that individuals within these poorer and higher quality neighborhoods are interchangeable (Oakes, 2004). The current study, however, addresses some of these concerns such that objective neighborhood characteristics were not utilized but rather, subjective perceptions of neighborhood disorder and social cohesion. The use of subjective indicators focuses our analyses on the individual rather than group level and reduces concerns about the selection within neighborhoods or clustering of neighborhood data. For instance, two neighbors may have very different perceptions of social cohesion. Therefore, there may be substantial variability in perceptions both within and between neighborhoods. Still, individuals who live in objectively disordered neighborhoods are more likely to report physical disorder, which is why the current study included a battery of covariates to address these selection effects such as age, education, wealth, income, and chronic illness burden that may influence access to resources and social mobility. As the current study utilizes observational data and cannot fully disentangle the effects of neighborhoods due to these concerns, future research that systematically addresses these issues is necessary before intervention or policy work can build of the results of these findings. Further, although significant associations between perceived neighborhood characteristics, psychological distress and cognition emerged, future research should examine the discriminatory accuracy of perceived neighborhood characteristics in predicting the prevalence of psychological distress and cognitive impairment.
Conclusion
In conclusion, neighborhood characteristics influence cognitive functioning through psychological distress in older adulthood. Individuals who live in highly disordered and less socially cohesive neighborhoods experience greater feelings of anxiety and/or depressive symptoms potentially due to heightened fear of crime and victimization or mistrust of other residents. This, in turn, negatively affects cognitive aging processes for older adults residing in these poorer quality neighborhoods, which could have important implications for health including dementia risk and psychological health. With the increase in population aging and the importance of aging in place, intervening on this environmental level (i.e., neighborhoods) as well on the individual level (i.e., psychological distress) may have broad implications for health equity and quality of life for older adult populations.
Supplementary Material
Highlights.
Neighborhood characteristics may influence cognition via psychological distress.
Perceived physical disorder is linked to worse cognition via higher anxiety.
Perceived social cohesion is linked to better cognition via lower anxiety and depression.
Acknowledgements
Sponsor’s Role: This work was supported by the National Institutes on Aging [grant numbers R00AG047963 and R01AG054520]. The HRS (Health and Retirement Study) is sponsored by the National Institute on Aging (grant number NIA U01AG009740) and is conducted by the University of Michigan. The sponsor had no role in the current analyses or the preparation of this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: The authors have no conflicts of interest.
References
- Aneshensel CS & Sucoff CA (1996). The neighborhood context of adolescent mental health. Journal of Health and Social Behavior, 37, 293–310. 10.2307/2137258 [DOI] [PubMed] [Google Scholar]
- Barger SD, Messerli-Bürgy N & Barth J (2014). Social relationship correlates of major depressive disorder and depressive symptoms in switzerland: Nationally representative cross sectional study. BMC Public Health, 14, 273 10.1186/1471-2458-14-273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaudreau SA, & O’Hara R (2008). Late-life anxiety and cognitive impairment: a review. The American Journal of Geriatric Psychiatry, 16(10), 790–803. 10.1097/JGP.0b013e31817945c3 [DOI] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, & Steer RA (1988). An inventory for measuring clinical anxiety: Psychometrics properties. Journal of Consulting & Clinical Psychology, 56, 893–897. 10.1037//0022-006x.56.6.893 [DOI] [PubMed] [Google Scholar]
- Becker E, Rios CLO, Lahmann C, Rücker G, Bauer J & Boeker M (2018). Anxiety as a risk factor of alzheimer’s disease and vascular dementia. The British Journal of Psychiatry, 213, 645–660. 10.1192/bjp.2018.173 [DOI] [PubMed] [Google Scholar]
- Bennett BA, Schneider JA, Tang Y, Arnold SE & Wilson RS (2006). The effect of social networks on the relation between alzheimer’s disease pathology and level of cognitive function in old people: A longitudinal cohort. Lancet Neurology, 5, 406–412. 10.1016/S1474-4422(06)70417-3 [DOI] [PubMed] [Google Scholar]
- Bierman EJM, Comijs HC, Jonker C, & Beekman ATF (2005). Effects of anxiety versus depression on cognition in later life. American Journal of Geriatric Psychiatry, 13, 686–693. 10.1176/appi.ajgp.13.8.686 [DOI] [PubMed] [Google Scholar]
- Brewster GS, Peterson L, Roker R, Ellis ML, & Edwards JD (2017). Depressive symptoms, cognition and everyday function among community-residing older adults. Journal of Aging & Health, 29, 367–388. 10.1177/0898264316635587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SC, Mason CA, Spokane A, Cruza-Guet MC, Lopez B, Szapocznik J (2009). The relationship of neighborhood climate to perceived social support and mental health in older Hispanic immigrants in miami, florida. Journal of Aging and Health, 21, 431–459. 10.1177/0898264308328976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byers AL & Yaffe K (2012). Depression and risk of developing dementia. Nature Reviews: Neurology, 7, 323–331. 10.1038/nrneuol.2011.60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casciano R & Massey DS (2012). Neighborhood disorder and anxiety symptoms: New evidence from a quasi-experimental study. Health Place, 18, 180–190. 10.1016/j.healthplace.2011.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi NG, Kim K, DiNitto DM & Marti CN (2015). Perceived social cohesion, frequency of going out, and depressive symptoms in older adults: Examination of longitudinal relationships. Gerontology & Geriatric Medicine, 26, 1–11. 10.1177/2333721415615478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi YJ & Matz-Costa C (2018). Perceived neighborhoods safety, social cohesion, psychological health of older adults. The Gerontologist, 58, 196–206. https://doi.or/10.1093/geront/gnw187 [DOI] [PubMed] [Google Scholar]
- Clarke PJ, Ailshire JA, House JS, Morenoff JD, King K, Melendez R, et al. (2012). Cognitive function in the community setting: The neighbourhood as a source of “cognitive reserve”? Journal of Epidemiology and Community Health, 66, 730–736. 10.1136/jech.2010.128116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke PJ, Weuve J, Barnes L, Evans DA, & Mendes de Leon CF (2015). Cognitive decline and the neighborhood environment. Annals of Epidemiology, 25, 849–854. 10.1016/j.annepidem.2015.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenck MW, Derakshan N, Santos R & Calvo MG (2007). Anxiety and cognitive performance: Attentional control theory. Emotion, 7, 336–353. 10.1037/1528-3542.7.2.336 [DOI] [PubMed] [Google Scholar]
- Fisher GG, McArdle JJ, McCammon R, Sonnega A, & Weir DR (2013). New Measures of Fluid Intelligence in the HRS. Ann Arbor: Retrieved from https://hrs.isr.umich.edu/publications/biblio/5959 [Google Scholar]
- Friedman EM, Shih RA, Slaughter ME, Weden MM, & Cagney KA (2017). Neighborhood age structure and cognitive function in a nationally representative sample of older adults in the U.S. Social Science & Medicine, 174, 149–158. 10.1016/J.SOCSCIMED.2016.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furtado M & Katzman MA (2015). Neuroinflammatory pathways in anxiety, posttraumatic stress, and obsessive compulsive disorders. Psychiatry Research, 229, 37–48. 10.1016/j.psychres.2015.05.036 [DOI] [PubMed] [Google Scholar]
- Gallacher J, Bayer A, Fish M, Pickering J, Pedro S, Dunstan F, Ebrahim S, & Ben-Shlomo Y (2009). Does anxiety affect risk of dementia? Findigns from the caerphilly prospective study. Psychosomatic Medicine, 71, 659–666. 10.1097/PSY.0b013e3181a6177c [DOI] [PubMed] [Google Scholar]
- Gardner PJ (2011). Natural neighborhood networks - important social networks in the lives of older adults aging in place. Journal of Aging Studies, 25, 263–271. 10.1016/j.jaging.2011.03.007 [DOI] [Google Scholar]
- Gary TL, Stark SA & LaVeist TA (2007). Neighborhood characteristics and mental health among african americans and whites living in a racially integrated urban community. Health & Place, 13, 569–575. 10.1016/j.healthplace.2006.06.001 [DOI] [PubMed] [Google Scholar]
- Glass TA, Mendes de Leon C, Bassuk SS & Berkman LF (2006). Social engagement and depressive symptoms in late life: Longitudinal findings. Journal of Aging and Health, 18, 604–628. 10.1177/0898264306291017 [DOI] [PubMed] [Google Scholar]
- Henderson H, Child S, Moore S, Moore JB & Kaczynski AT (2016). The influence of neighborhood aesthetics, safety, and social cohesion on perceived stress in disadvantaged communities. American Journal of Community Psychology, 58, 80–88. 10.1002/ajcp.12081. [DOI] [PubMed] [Google Scholar]
- Henry JD, Crawford JR, & Phillips LH (2004). Verbal fluency performance in dementia of the Alzheimer’s type: A meta-analysis. Neuropsychologia, 42, 1212–1222. 10.1016/J.NEUROPSYCHOLOGIA.2004.02.001. [DOI] [PubMed] [Google Scholar]
- Horgas AL, Wilms H, & Baltes MM (1998). Daily life in very old age: Everyday activities as expression of successful living. The Gerontologist, 38, 556–568. 10.1093/geront/38.5.556 [DOI] [PubMed] [Google Scholar]
- Hu L, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6, 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Hultsch DF, Hertzog C, Small BJ, & Dixon RA (1999). Use it or lose it: Engaged lifestyle as a buffer of cognitive decline in aging? Psychology and Aging, 14, 245–263. 10.1037/0882-7974.14.2.245 [DOI] [PubMed] [Google Scholar]
- Ivey SL, Kealey M, Kurtovich E, Hunter RH, Prohaska TR, Bayles CM & Satariano WA (2015). Neighborhood characteristics and depressive symptoms in an older population. Aging & Mental Health, 19, 713–722. 10.1080/13607863.2014.962006 [DOI] [PubMed] [Google Scholar]
- Jorm AF, (2000). Is depression a risk factor for dementia or cognitive decline: A review. Gerontology, 46, 219–227. 10.1159/000022163 [DOI] [PubMed] [Google Scholar]
- Latkin CA & Curry AD (2003). Stressful neighborhoods and depression: A prospective study of the impact of neighborhood disorder. Journal of Health and Social Behavior, 44, 34–44. 10.2307/1519814 [DOI] [PubMed] [Google Scholar]
- Lee H & Waite LJ (2018). Cognition in context: The role of objective and subjective measures of neighborhood and household in cognitive functioning in later life. The Gerontologist, 58, 159–169. 10.1093/geront/gnx050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim YY, Snyder PJ, Pietrzak RH, Ukiqi A, Villemagne VL, Ames D, Salvado O, Bourgeat P, Martins RN, Masters CL, Rowe CC, Maruff P and for the AIBL Research Group. Sensitivity of composite scores to amyloid burden in preclinical alzheimer’s disease: Introducing the z-score of attention, verbal fluency, and episodic memory for nondemented older adults composite score. Alzheimer’s and Dementia: Diagnosis, Assessment and Disease Monitoring, 2, 19–26. 10.1016/j.dadm.2015.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lockwood KA, Alexopoulos GS & van Gorp W (2002). Executive dysfunction in geriatric depression. American Journal of Psychiatry, 159, 1119–1126. 10.1176/appi.ajp.159.7.1119 [DOI] [PubMed] [Google Scholar]
- Lohman MW, Rebok GW, Spira AP, Parisi JM, Gross AL, & Kueider AM, (2013). Depressive symptoms and memory among older adults: Results from the ACTIVE memory training intervention. Journal of Aging and Health, 25, 209S–229S, 10.1177/0898264312460573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot M & Bell R (2012). Fair society, healthy lives. Public Health, 26, 4–10. 10.1016/j.puhe.2012.05.014 [DOI] [PubMed] [Google Scholar]
- Muthén LK., & Muthén BO (2007). Mplus User’s Guide (Sixth Edition). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Oakes JM (2004). The (mis)estimation of neighborhood effects: Causal inference for a practicable social epidemiology. Social Science & Medicine, 58, 1929–1952. 10.1016/j.socscimed.2003.08.004 [DOI] [PubMed] [Google Scholar]
- Ofstedal MB, Fisher GG, Herzog AR, Wallace RB, Weir DR, Langa KM, et al. (2005). HRS/AHEAD Documentation Report Documentation of Cognitive Functioning Measures in the Health and Retirement Study. Retrieved from https://hrs.isr.umich.edu/sites/default/files/biblio/dr006.pdf
- Pearson AL, Breetzke G, & Ivory V (2015). The effect of neighborhood recorded crime on fear: Does neighborhood social context matter? American Journal of Community Psychology, 56, 170–179. 10.1007/s10464-015-9741-z [DOI] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D Scale. Applied Psychological Measurement, 1, 385–401. 10.1177/014662167700100306. [DOI] [Google Scholar]
- Ramos M & Wilmoth J (2003). Social relationships and depressive symptoms among older adults in southern brazil. The Journals of Gerontology: Social Sciences, 58, 253–261. 10.1093/geronb/58.4.s253 [DOI] [PubMed] [Google Scholar]
- Rapp MA, Dahlman K, Sano M, Grossman HT, Haroutunian V & Gorman JM (2005). Neuropsychological differences between late-onset and recurrent geriatric major depression. American Journal of Psychiatry, 162, 691–698. 10.1176/appi.ajp.162.4.691 [DOI] [PubMed] [Google Scholar]
- Robinette JW, Charles ST, Mogle JA & Almeida DM (2013). Neighborhood cohesion and daily well-being: Results from a diary study. Social Science & Medicine, 96, 174–182. 10.1016/j.socscimed.2013.07.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen WG (1980). Verbal fluency in aging and dementia. Journal of Clinical Neuropsychology, 2, 135–146. 10.1080/01688638008403788. [DOI] [Google Scholar]
- Ross CE & Mirowsky J (2009). Neighborhood disorder, subjective alienation, and distress. Journal of Health and Social Behavior, 50, 49–64. 10.1177/002214650905000104 [DOI] [PubMed] [Google Scholar]
- Ruiz M, Malyutina S, Pajak A, Kozela M, Kubinova R & Bobak M (2019). Congruent relations between perceived neighbourhood social cohesion and depressive symptoms among older European adults: An east-west analysis. Social Science & Medicine, 237 10.1016/j.socscimed.2019.112454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz M, Scholes S & Bobak M (2018). Perceived neighborhood social cohesion and depressive symptom trajectories in older adults: A 12-year prospective cohort study. Social Psychiatry and Psychiatric Epidemiology, 53, 1081–1090. 10.1007/s00127-018-1548-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampson RJ & Raudenbush SW (1999). Systematic social observation of public spaces: A new look at disorder in urban neighborhoods. American Journal of Sociology, 105, 603–651. 10.1086/210356 [DOI] [Google Scholar]
- Scarmeas N, Luchsinger JA, Schupf N, Brickman AM, Cosentino S Tang MX, & Stern Y (2009). Physical activity, diet and risk of alzheimer disease. The Journal of the American Medical Association, 302, 627–637. 10.1001/jama.2009.1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott SB, Munoz E, Mogle JA, Gamaldo AA, Smyth JM, Almedia DM & Sliwinski MJ (2018). Perceived neighborhood characteristics predict severity and emotional response to daily stressors. Social Science & Medicine, 200, 262–270. 10.1016/j.socscimed.2017.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharifian N, Gu Y, Manly JJ, Schupf N, Mayeux R, Brickman AM, & Zahodne LB (2020). Linking depressive symptoms and cognitive functioning in older adulthood: The mediating role of leisure activity. Neuropsychology, 34, 107–115. 10.1037/neu000595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spalt EW, Curl CL, Allen RW, Cohen M, Adar SD, Stukovsky KH, Avol E, Castro-Diehl C, Nunn C, Mancera-Cuevas K & Kaufman JD (2016). Time-location patterns of a diverse population of older adults: The multi-ethnic study of atherosclerosis and air pollution (MESA Air). Journal of Exposure Science and Environmental Epidemiology, 26, 349–355. 10.1038/jes.2015.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonnega A, & Weir DR (2014). The Health and Retirement Study: A public data resource for research on aging. Open Health Data, 2, e7 10.5334/ohd.am. [DOI] [Google Scholar]
- Stern Y (2002). What is cognitive reserve? Theory and research application of the reserve concept. Journal of the International Neuropsychological Society, 8, 448–460. https://doi.org/10.1017.S1355617701020240 [PubMed] [Google Scholar]
- Subramanian SV, Kubzansky L, Berkman L, Fay M, & Kawachi I (2006). Neighborhood effects on the self-rated health of elders: Uncovering the relative importance of structural and service-related neighborhood environments. The Journals of Gerontology: Social Sciences, 61, 153–160. 10.1093/geronb/61.3.S153 [DOI] [PubMed] [Google Scholar]
- Tang F, Chi I, Xu L, & Dong X (2018). Exploring relationships of psychological sense of community with self-rated health and depressive symptoms among older chinese americans. Gerontology & Geriatric Medicine, 4, 1–7. 10.1177/2333721418778183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor RB, Gottfredson SD & Bower S (1984). Block crime and fear: Defensible space, local social ties and territorial functioning. Journal of Research in Crime and Delinquency, 21, 303–331. 10.1177/0022427884021004003 [DOI] [Google Scholar]
- Weir D, Mccammon R, Ryan L, & Langa K (2014). Cognitive Test Selection for the Harmonized Cognitive Assessment Protocol (HCAP). Retrieved from https://hrs.isr.umich.edu/sites/default/files/biblio/HCAP_testselection.pdf
- Weisburd D, Cave B, Nelson M, White C, Haviland A, Ready J, Lawton B, & Sikkema K (2018). Mean streets and mental health: Depression and PTSD at crime hot spots. American Journal of Community Psychology, 61, 285–295. 10.1002/ajcp.12232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitley R & Prince M (2005). Fear of crime, mobility and mental health in inner-city London, uk. Social Science & Medicine, 61, 1678–1688. 10.1016/j.socsimed.2005.03.044 [DOI] [PubMed] [Google Scholar]
- Wilson-Genderson M & Pruchno R (2013). Effects of neighborhood violence and perceptions of neighborhood safety on depressive symptoms in older adults. Social Science & Medicine, 85, 43–49. 10.1016/j.socscimed.2013.02.028 [DOI] [PubMed] [Google Scholar]
- Yochim BP, Mueller AE, & Segal DL (2013). Late life anxiety is associated with decreased memory and executive functioning in community dwelling older adults. Journal of Anxiety Disorders, 27, 567–575. 10.1016/j.janxdis.2012.10.010 [DOI] [PubMed] [Google Scholar]
- Zaheed AB, Sharifian N, Kraal AZ, Sol K, Hence A, & Zahodne LB (2019). Unique effects of perceived neighborhood physical disorder and social cohesion on episodic memory and semantic fluency. Archives of Clinical Neuropsychology, 34, 1346–1355. 10.1093/arclin/acy098 [DOI] [PubMed] [Google Scholar]
- Zahodne LB, Ajrouch K, Sharifian N, & Antonucci T (2019). Social relations and age-related change in memory. Psychology and Aging. 10.1037/pag0000369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahodne LB, Stern Y, & Manly JJ (2014). Depressive symptoms precede memory decline, but not vice versa, in non-demented older adults. Journal of the American Geriatrics Society, 62, 130–134. 10.1111/jgs.12600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang W, Liu S, Sun F, & Dong X (2019). Neighborhood social cohesion and cognitive function in U.S. chinese older adults - findings from the PINE study. Aging & Mental Health, 23, 1113–1121. 10.1080/13607863.2018.1480705 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


