Graphical abstract
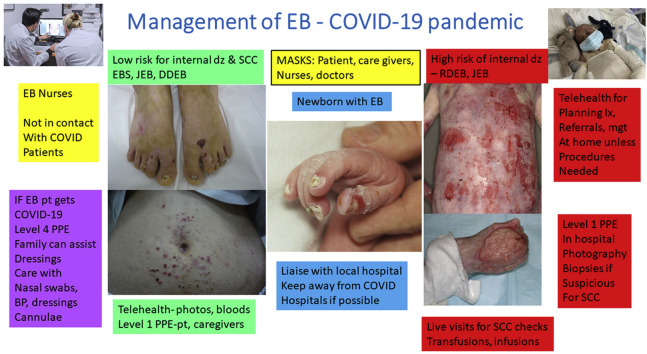
To the Editor: The 2019 novel coronavirus (COVID-19) pandemic became apparent in China during the International Congress on Epidermolysis Bullosa (EB) in London, in January 2020. Many patients with EB have medical problems that make them a vulnerable population of patients.1 We developed an international consensus to suggest the best management of patients with EB during the pandemic.
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus enters host cells using its spike protein binding to the cell receptor angiotensin converting enzyme 2 (ACE2), which is expressed in several tissues. Mucosae have high ACE2 expression, particularly the nasal epithelium. ACE2 is also expressed in the basal layer of keratinocytes and sebaceous glands of normal skin as well as in vascular endothelial cells, but its expression in wounded EB skin has not been studied.2
A questionnaire was drafted by an author (D.M.) into a table of suggested modifications to the management of EB during the COVID-19 pandemic. Fifty-seven well-known experts on EB were selected based on membership of the international Clin-et group or clinical expertise in EB, or both, demonstrated at International EB Congress participation. Responses and reasons for each response were requested individually to the lead author based on an ideal scenario, rather than what actually may happen in some centers with financial constraints. A priori, consensus was considered to be the agreement of more than 70% of respondents with the suggestion. Questionnaires were returned by 44 of the 57 EB experts, representing several areas of clinical expertise in EB (dermatology, pediatrics, internal medicine, and surgery) from 5 continents. After addition and revision of some items and 3 cycles of revoting, consensus was achieved for all items, which are summarized in Supplementary Table I (available via Mendeley at https://data.mendeley.com/datasets/zmpncb6zpr/2).
The main change in usual practice was the introduction of photographs from the patient/family and teledermatology as the primary visit for patients with less severe EB, with dressing supplies sent to the patients directly. For those patients with EB with significant internal disease, monitoring tests (blood and urine) must continue but can be obtained by local laboratories or family doctors close to home.3 If telehealth images are insufficient to assess lesions, assessments should be conducted at the EB center.4
One of the greatest fears of families caring for patients with severe forms of EB is how they will be perceived on admission to hospitals, especially institutions with limited resources, including ventilators. Because patients with EB often appear frail and emaciated, health care workers unfamiliar with the condition may underestimate their resilience and incorrectly assume that they have a low likelihood of survival.5 If a patient with EB required anticoagulation to manage COVID-19, there might be additional bleeding from the skin or mucosae, but blood transfusions will compensate for this. Supplemental Table I details protection for the skin and mucosae that is required for wearing masks and ventilation.
Footnotes
Funding sources: None.
Conflicts of interest: Dr Lucky is an investigator/advisor board member for Abeona, Amryt, and Lenus. Dr Paller is an investigator/advisory board member for Abeona. Dr Anna Bruckner is an investigator for Fibrocell, ProQR, and Phoenix Tissue Repair. Authors Murrell, Salas-Alanis, Woodley, Palisson, Natsuga, Nikolic, Ramirez-Quizon, Lara-Corrales, Barzegar, Sprecher, Has, Laimer, Bruckner, Nanda, Purvis, Hovnanian, Murat-Sušić, Bauer, Kern, Bodemer, Mellerio, Kowaleski, Robertson, Bruckner-Tuderman, Pope, Marinkovich, Tang, Su, Uitto, Eichenfield Teng, Koh, Lee, Khuu, Rishel, Sommerlund, Wiss, Hsu, Chiu, and Martinez have no conflicts of interest to declare.
IRB approval status: Not applicable.
References
- 1.Has C., Bauer J.W., Bodemer C., et al. Consensus reclassification of epidermolysis bullosa and other disorders with skin fragility. Br J Dermatol. 2020 doi: 10.1111/bjd.18921. [DOI] [PubMed] [Google Scholar]
- 2.Hamming I., Timens W., Bulthuis M.L.C., Lely A.T., Navis G.J., van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203:631–637. doi: 10.1002/path.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ramirez M., Murrell D.F., Fine J.D. Management of epidermolysis bullosa. Exp Opin Orph Drugs. 2013;1(4):279–293. [Google Scholar]
- 4.Mellerio J.E., Robertson S.J., Bernardis C., et al. Management of cutaneous squamous cell carcinoma in patients with epidermolysis bullosa—best clinical practice guidelines. Br J Dermatol. 2016;174(1):56–67. doi: 10.1111/bjd.14104. [DOI] [PubMed] [Google Scholar]
- 5.Bruckner A.L., Losow M., Wisk J., et al. The challenges of living with and managing epidermolysis bullosa: insights from patients and caregivers. Orphanet J Rare Dis. 2020;15(1):1. doi: 10.1186/s13023-019-1279-y. [DOI] [PMC free article] [PubMed] [Google Scholar]