Abstract
Objective
To evaluate the post-operative outcomes of the hips in CP patients with unilateral hip subluxation treated with bilateral and unilateral hip reconstruction.
Methods
A retrospective review was performed of all diplegic and quadriplegic patients with unilateral hip displacement treated with either bilateral or unilateral hip reconstructive surgery. Radiographic parameters [migration percentage (MP), pelvic obliquity angle (POA) and migration percentage difference (MPD)] and changes in functional ability (sitting, standing and walking) were evaluated and compared between the 2 groups. Failure was defined as post-operative MP>40%, POA>5° and MPD>30%.
Results
Eighteen patients had unilateral hip reconstruction and 42 patients had bilateral hip reconstruction. Mean age of 87 months and 90 months and means follow-up of 38 months and 40 months respectively. Post-operative MP was significant in both groups. However, of 18 patients in unilateral hip reconstruction group, 33.3% of patients had contralateral hip subluxation and 22.2% of patients had hip failure on the operated hip; compared to only one of 42 patients had hip failure and no contralateral hip problem in the other group. For assessment of pelvic symmetry, MPD was significantly improved in both group but POA was only significant in bilateral group. Overall functional improvement was significant in patients with bilateral hip reconstruction compared to unilateral group.
Conclusion
Bilateral hip reconstruction in unilateral displacement had shown to have better outcome in correcting unstable hip and pelvic asymmetry, thus provide good sitting balance and improvement in overall functional outcome.
Keywords: Bilateral hip reconstruction, Unilateral/contralateral hip subluxation, Prophylactic hip reconstruction, Pelvic obliquity, Functional outcome, Cerebral palsy
1. Introduction
Hip subluxation and progressive dislocation in patients with cerebral palsy (CP) varies according to the clinical pattern and functional level. Patients with spastic quadriplegia GMFCS level IV-V have shown to be at the highest risk.1, 2, 3 Imbalance in muscle forces around the hip and spasticity contribute to increase in femoral neck-shaft angle and femoral anteversion which eventually lead to hip subluxation and dislocation especially in non-ambulatory children.4, 5, 6, 7
Early detection of hip subluxation through hip surveillance helps in prevention of hip dislocation, preserved painless hip motion and improve functional status.8,9 Soft tissues release can prevent progression of hip subluxation; however, some hips continue to migrate despite early surgery. Varus derotational shortening osteotomy (VDRSO) and innominate osteotomy can effectively stabilise the hip, addresses both coxa valga and femoral malalignment as well as improve hip function and relieve pain in long term outcome.10, 11, 12
One of the controversial issue which remains unclear is whether there is a necessity for bilateral hip reconstruction in spastic diplegia or quadriplegia with unilateral hip displacement. Patients with GMFCS level III to V carry a high risk of recurrent hip subluxation of both originally operated hip and the contralateral hip. Contralateral hip subluxation and ipsilateral hip failure have been reported in several studies as a complication after unilateral hip reconstruction.13, 14, 15, 16 Changes in the balance of muscle forces that control pelvic alignment after unilateral hip surgery have been thought to cause contralateral hip subluxation and reversal of pelvic obliquity.17,18 Prophylactic surgery in radiologically normal contralateral hip is still not in favour for some authors and patients treated with unilateral hip surgery should be followed until skeletal maturity.19,20 However, some investigators stated that bilateral hip reconstruction in non-ambulatory quadriplegic patients should be considered to maintain symmetrical pelvic alignment to allow balance sitting position even if the contralateral hip is normal.11,12,21,22
The purpose of this study was to describe the radiological and clinical outcomes of bilateral hip reconstruction in comparison to unilateral hip surgery in patients with unilateral hip displacement.
2. Material and methods
A retrospective review was conducted on patients with diplegic and quadriplegic (CP) presented with unilateral hip displacement. These patients underwent either unilateral or bilateral hip reconstructive surgery from 2011 until 2016 at Queen Sirikit National Institute of Child Health, Bangkok, Thailand.
We have been performing hip reconstruction surgery for subluxated or dislocated hip only in early year of practice. However, we noted that the result was dissatisfying both in radiological and clinical outcome. Therefore, as our current protocol, patients with unilateral hip subluxation which indicated for surgery will undergo bilateral hip reconstruction. Furthermore, with the implementation of hip surveillance for all CP patients, early detection of problematic hips were possible.
The inclusion criteria for the study was diplegic or quadriplegic patients with unilateral hip displacement with migration percentage of Reimers’ (MP) > 40%22,23 and hip abduction contracture <30°. We excluded patients with hemiplegic cerebral palsy, involvement of bilateral hip subluxation, patients who had severe femoral head deformity and patients with structural scoliosis which may influenced measurement of pelvic obliquity angle (POA).26,27
Patient demographic and treatment information which includes age at time of surgery, gender, distribution of CP involvement (diplegia, triplegia or quadriplegia), Gross Motor Function Classification System level (GMFCS) level and operative procedures were reviewed. Surgical complications such as infections, fractures or hardware failure were recorded.
2.1. Surgical procedures
Patients were provided with physiotherapy program and general health assessment before the operation. All patients were treated with varus derotational and shortening osteotomy (VDRSO) of proximal femur at pre-determined neck-shaft angle of 110–120°. If inadequate acetabular coverage detected on fluoroscopy, and the acetabular index was more than 25°, Dega pelvic osteotomy would be performed.28,29 Percutaneous release of hip adductor longus muscle was performed if necessary. In patients with high hip dislocation, open reduction was considered if the hip failed to reduce by the former steps of surgery. Other soft tissue procedure including medial hamstring release or tendo-Achilles lengthening were performed selectively depending on pre-operative assessment.
Post-operative pain control with epidural anesthesia or continuous intravenous morphine was given for 2 days after operation. Post-operative immobilisation was prescribed only for selected patients. Abduction cast was applied as a part of pain management in patients whom had severe muscle spasticity. Hip spica cast was applied in patients whom had open hip reduction. Cast was removed after 6 weeks and post-operative physiotherapy program were commenced.
2.2. Patients evaluation
The operative results were evaluated on clinical and radiographic criteria. We reviewed pre-operative, post-operative 12 months and last follow-up anteroposterior and frog-leg pelvic radiographs. Radiological data was collected for each hip (ipsilateral and contralateral) and included MP, acetabular index (AI), POA and migration percentage difference (MPD). POA was measured as an angle between a line tangential to ischial tuberosities and line parallel to the ground in supine position. However, as POA measurement influences by many factors derived from either supra- or infrapelvic causes,25,26 therefore we measured MPD which is the MP difference between two hips as an additional new independent parameter to established hip symmetry which we believed had some correlation with pelvis balance and alignment.
As for evaluation of treatment outcome, post-operative hip MP>40%,24 POA >5°,25 and MPD >30% at last follow-up were regarded as poor outcomes in both unilateral and bilateral hip reconstruction groups. Any reversal in pelvic obliquity at contralateral hip was also recorded.
Patients’ mobility functions were reviewed at pre- and postoperative 12 months and at last follow-up. Three basic functional mobility were assessed: sitting, standing and walking ability. Sitting status was graded depending on their ability to sit independently or sitting with support or failed to sit at all. For the standing and walking assessment, patients were classified as follows: whether they were able to stand or walk independently or walking aid was needed. Those who incapable of holding the walking device, they were observed to stand or walk with the help of caretakers, or they failed to perform those function completely. Any changes in the mobility status were recorded at every clinic visit.
2.3. Statistical analysis
Statistical analysis was performed using Student's t-test for pre- and post-operative MP, POA and MPD within and between unilateral and bilateral hip reconstruction groups. The Pearson correlation test were performed to established relationship between the POA and MPD in regards to hip and pelvic symmetry. Overall functional improvement in each group were evaluated with Chi-square test. A p-value <0.05 was considered statistically significant.
3. Results
As we mentioned earlier, implementation of hip surveillance enabled early detection of subluxated hip. Furthermore, bilateral hip surgery was performed for all patients as a current protocol. Therefore, we had discrepancy in the demographic data between unilateral and bilateral hip reconstruction group.
There were 18 patients comprised of 9 males and 9 females with 18 operated hips in unilateral reconstruction group, with mean age at operation was 87.67 months (range 55–161) and mean follow-up of 38.22 months (range 18–72). The distribution of the CP was diplegia 4 patients, quadriplegia 14 patients and no triplegia. GMFCS level was one patient level III and IV respectively, whereas 16 patients classified GMFCS level V. Dega osteotomy were performed in 12 hips as addition to VDRSO in this group.
In bilateral hip reconstruction group, there were 42 patients comprised of 14 males and 28 females with 84 operated hips. Their mean age at operation were 90.43 months (range 44–240) and mean follow-up of 40.45 months (range 18–70). The distribution of the CP was diplegia 20 patients, triplegia 4 patients and quadriplegia 18 patients. GMFCS level was 4 patients level III, 5 patients level IV and 32 patients classified GMFCS level V. Twenty-seven hips had additional Dega osteotomy. The demographic data was depicted in Table 1.
Table 1.
Patient demographic data for unilateral and bilateral hip reconstruction.
| Unilateral group | Bilateral group | *p value | |
|---|---|---|---|
| Number of patients | 18 | 42 | |
| Number of operated hips | 18 | 84 | |
| Mean age (months) | 87.67 (range 55–161) | 90.43 (range 44–240) | 0.78 |
| Sex M/F | 9/9 | 14/28 | |
| βGMFCS (III/IV/V) | 1/1/16 | 4/5/32 | |
| Diagnoses (Diplegia/Triplegia/Quadriplegia) | 4/0/14 | 20/4/18 | |
| Mean follow-up (months) | 38.22 (range 18–72) | 40.45 (range 18–70) | 0.63 |
| Dega Pelvic Osteotomy | 12 | 27 | |
| £VDRO | 18 | 84 |
*statistically significant p < 0.05
βGMFCS means Gross Motor Functional Classification System
£VDRO means varus derotation osteotomy
Pre-operatively, both groups had high mean MP for subluxated hip but higher in unilateral group (76.7%) as compared to bilateral hip reconstruction group (61.7%) owing to the hip surveillance program (p = 0.007). Mean MP for contralateral hips in unilateral hip reconstruction group was 23.8% and 30.5% in bilateral group (p = 0.031). Meanwhile, pre-operative POA in both group were not significant which was 6.5° and 4.1° in unilateral and bilateral group respectively. As for MPD, high value was observed in unilateral group (52.9%) as compared to bilateral group (31.2%) which was highly significant (p < 0.005). Details of the overall results were shown in Table 2.
Table 2.
Comparison of the outcome of the radiographic parameters and functional status pre-operation, post-operative 12-months and at last follow-up between unilateral and bilateral hip reconstruction.
| Unilateral hip reconstruction n = 18 patients |
Bilateral hip reconstruction n = 42 patients |
αp value (unilateral:bilateral group) |
||||
|---|---|---|---|---|---|---|
| Mean Migration Percentage (%) | Ipsilateral hip | Contralateral hip | Ipsilateral hip | Contralateral hip | Ipsilateral hip | Contralateral hip |
| Pre-operative | 76.7 | 23.8 | 61.7 | 30.5 | 0.007 | 0.031 |
| Post-operative 12 months | 30.0 | 27.9 | 8.4 | 8.6 | 0.004 | <0.005 |
| Last follow-up | 33.4 | 30.8 | 11.0 | 12.2 | 0.004 | 0.002 |
| £p-value | <0.005 | *0.104 | <0.005 | <0.005 | ||
| Mean Pelvic Obliquity Angle (degrees) | ||||||
| Pre-operative | 6.5 | 4.1 | *0.21 | |||
| Post-operative 12 months | 4.4 | 1.9 | 0.004 | |||
| Last follow-up | 5.6 | 2.1 | 0.001 | |||
| £p-value | *0.423 | 0.007 | ||||
| Mean Migration Percentage Difference (%) | ||||||
| Pre-operative | 52.9 | 31.2 | <0.005 | |||
| Post-operative 12 months | 24.9 | 5.1 | <0.005 | |||
| Last follow-up | 29.2 | 7.6 | <0.005 | |||
| £p-value | <0.005 | <0.005 | ||||
| Functional status at last follow-up | ||||||
| Improvement in sitting | 5 | 21 | NA | |||
| Improvement in standing | 2 | 23 | NA | |||
| Improvement in walking | 1 | 6 | NA | |||
| Overall functional improvement | 6 (33.3%) | 31 (73.8%) | 0.031 | |||
| No changes | 12 (66.7%) | 11 (26.2%) | NA | |||
αp-value between unilateral and bilateral hip reconstruction group.
£p-value within ipsilateral and contralateral hip pre-operation and last follow-up.
*p-value>0.05 not statistically significant.
Post-operatively, there was significant improvement in MP in both groups. In unilateral group, the ipsilateral hip mean MP was 30% and 33.4% at 1-years post-operation and at last follow-up (p < 0.005), wherein bilateral group the mean MP was reduced to 8.4% and 11% respectively (p < 0.005). In contrast, different phenomenon was observed in contralateral hip. We noted the mean MP was gradually increased in unilateral group from 23.8% pre-operatively to 30.8% at last follow-up. However, these was not the case in bilateral group where the contralateral hip mean MP was not significantly changed at 12 months and at last follow-up. Comparison between unilateral and contralateral hip reconstruction in the radiological outcome were simplified in Fig. 2. For assessment of pelvic alignment, the POA improvement was not statistically significant (p = 0.423) in unilateral group but the difference was markedly significant (p = 0.007) in bilateral group at last follow-up. Both groups had improvement in mean MPD but major different were seen in bilateral group (p < 0.005).
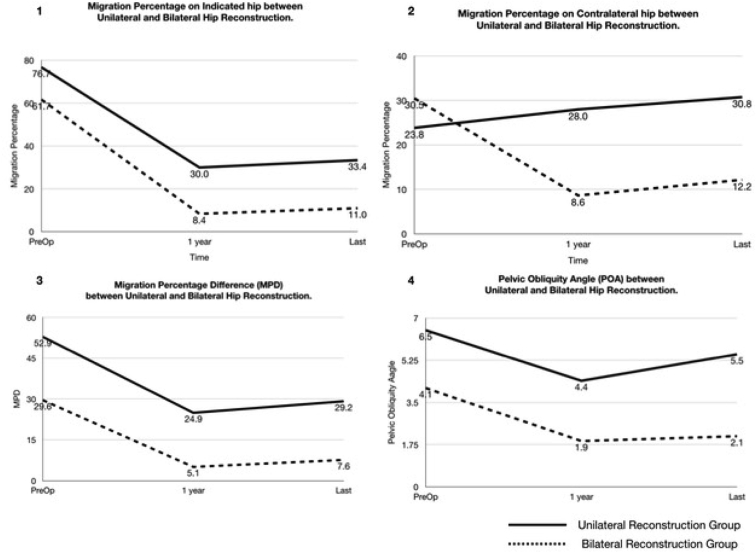
Fig. 2.
Pre- and post-operative MP, MPD and POA between unilateral and bilateral hip reconstruction over time (at 1-year and at last follow-up) were depicted in the above graph. Bilateral hip reconstruction (dotted line) had shown satisfactory outcome in all radiological parameters (in graph 1 to 4) pre- and post-surgery. In unilateral group, the mean MP had improved postoperatively in the operated hip as shown in graph 1; however, there was worsening of mean MP in contralateral hip over time (solid line) as depicted in graph 2. In graph 3 and 4, mean MPD and POA pre-operative and at last follow-up for unilateral hip reconstruction were increased as compared to bilateral hip reconstruction group.
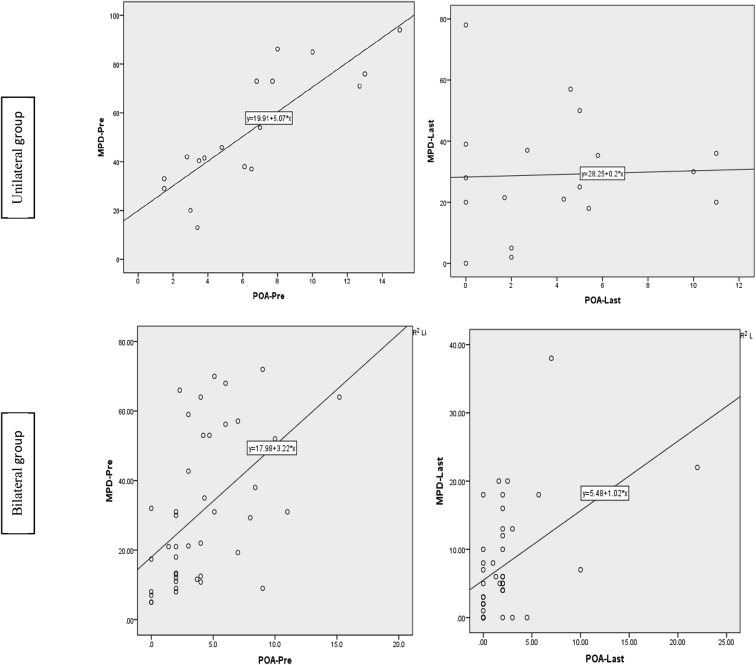
We evaluated the correlation of MPD and POA as an assessment of pelvic symmetry in both groups using Pearson correlation test. We observed a strong positive correlation at pre-operation as illustrated in Fig. 1 (p < 0.005). Improvement in MPD after bilateral hip stabilization had association with improvement of POA as shown in post-operative graph in bilateral group (<0.005). However, this correlation seems not significant in unilateral group after hip surgery (p = 0.488). MPD was improved by reconstruction procedure even though only ipsilateral hip surgery was performed, however single hip operation was seemingly inadequate to correct the POA.
Fig. 1.
The graphs illustrated the correlation between pre- and post-operative MPD and POA in determining hip and pelvic symmetry for unilateral and bilateral hip reconstruction groups. In bilateral hip surgery, there was a significant correlation between MPD and POA (p < 0.005). However, in unilateral hip reconstruction group, post-operation MPD and POA correlation was not significant (p = 0.488). It showed that even though unilateral hip reconstruction able to improve the MPD, this procedure was inadequate to correct the POA.
At final follow-up, we observed 6(33.3%) contralateral hip failure and 4(22.2%) recurrent hip failure in unilateral group as compared to only 1(2.4%) recurrent hip failure in bilateral group. None of the latter group had contralateral hip failure. Meanwhile for hip symmetry assessment, 1 patients in bilateral group and 8 patients in unilateral group had worsening MPD >30%. As for pelvic obliquity, POA >5° was observed in 5 patients and 3 patients from unilateral and bilateral groups respectively. We noted that 5 contralateral hips had reversal POA in unilateral group but none was observed in the other group. Post-operative outcome of hip failure was illustrated in Table 3.
Table 3.
Percentage of hip failure between unilateral and bilateral reconstruction group at last follow-up.
| Unilateral hip surgery (n = 18) | Bilateral hip surgery (n = 42) | |
|---|---|---|
| MP >40% | ||
| Ipsilateral hip | 4 (22.2%) | 1 (2.4%) |
| Contralateral hip | 6 (33.3%) | 0 |
| POA >5° | 5 (27.8%) | 3 (7%) |
| MPD >30% | 8 (44.4%) | 1 (2.4%) |
| Reversal Pelvic Obliquity | 5 (27.8%) | 0 |
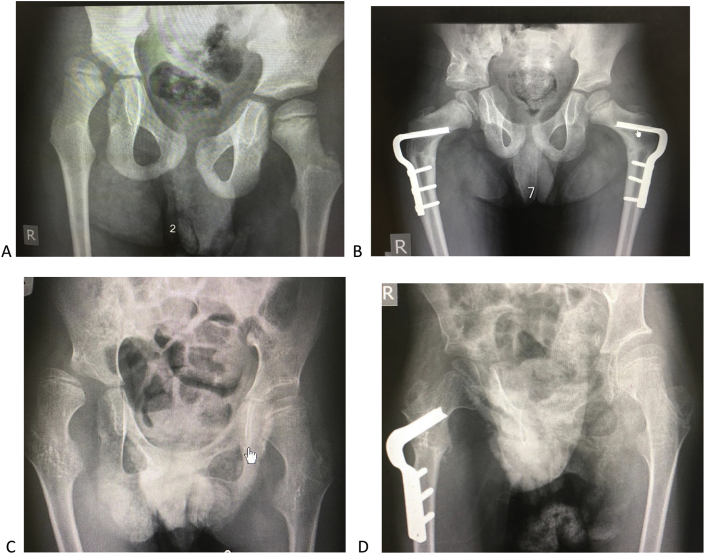
Overall functional status was improved tremendously in bilateral hip reconstruction group. Thirty-one patients (73.8%) had improvement after surgery in the former group, whereas only 6/18 patients (33.3%) were improved in unilateral hip surgery group (p = 0.031). Of the 3 functional status, 50% of patients had improvement in both sitting and standing function as compared to pre-operation. This result showed that bilateral hip reconstruction was good in obtaining pelvic symmetry and sitting balance in those patients (Fig. 3).
Fig. 3.
A, anteroposterior radiograph showed right hip subluxation (MP>60%) and pelvic obliquity (POA 8.4°) with elevation of right hip in a 10-years old spastic diplegic boy. The contralateral MP of 10% and noted coxa valga in both hips. B, bilateral VDRO and Dega osteotomy of right pelvic was performed. Both hips were symmetry after the operation; coxa valga and pelvic obliquity were corrected. The radiograph was 2 years after the surgery. C, right hip subluxation (MP>70%) with elevation of right hip in 9 years old spastic diplegic girl. Left hip was well seated. D, she was treated with right hip VDRO and Dega osteotomy; and femoral head was reduced after surgery. However, the pelvic obliquity still persisted; and contralateral hip coxa valga was not corrected After 1-year post surgery, left hip was subluxated (MP>30%) and pelvic was elevated to the left.
In this study, few surgical complications were observed. One patient had intraoperative sub-trochanteric fracture during hip reduction due to bone fragility. The fracture was fixed temporarily with dynamic plate and hip reconstruction was performed 1 year later after achieved fracture union. Peri-implant fracture was observed in another patient due to trauma one-year post surgery. There was no implant-related infection or wound dehiscence in both group. Indeed, in bilateral hip reconstruction surgery, the operative time were longer and anticipated more blood loss, however there was no added risk for intra- and post-operative complication in both groups. Length of hospital stay and amount of post-operative analgesic were found to be at similar rate.
4. Discussion
Hip instability in patients with cerebral palsy varies according to motor and functional severity and often ended with dislocation if left untreated especially those with spastic quadriplegia.1, 2, 3 The deformity of hip namely coxa valga and excessive femoral anteversion usually occurs in both hips as a result of muscle imbalance and spasticity in non-ambulatory patients,6 however hip displacement may have presented either unilateral or bilateral. Asymmetrical hip displacement may compromise the functional mobility and sitting posture as it frequently associated with pelvic obliquity and scoliosis.7,25, 26, 27, 30 Therefore, early detection through hip surveillance and operative procedure either soft tissue or bone procedure is mandatory.4,9 In cases of severe subluxation or dislocation, hip reconstruction surgery is the most appropriate effective procedure and yielded good outcome to reduce the hip displacement which include varus derotation and shortening osteotomy (VDRSO) of a proximal femur and Dega pelvic osteotomy.10, 11, 12,29
There are many factors influencing the success of reconstructive hip surgery. Many authors had outlined the predictive factors that leads to poor outcomes which correlates well with high degree of GMFCS level, severity of pre-operative hip displacement and young age at surgery.14,17 On top of that, many studies found that recurrent subluxation of operated hip and progressive displacement of contralateral hip happened in those patients that received unilateral hip reconstruction.13, 14, 15, 16 The changes in muscles-pulled around the hip that control pelvic alignment and loss of protective hip abduction especially in windswept deformity had postulated to be the reason for reversal of pelvic obliquity and progression of subluxation in contralateral hip.13, 14, 15 Therefore, there are some argument regarding the justification of bilateral hip reconstruction in severe non-ambulatory patients who had unilateral hip displacement to balance pelvic asymmetry. Some authors recommended close observation of both hips until further migration of contralateral hip and early soft tissue release in patient with abduction contracture.19,20 However, others suggested bilateral hip surgery at one stage.21,22 Therefore, from our previous experience that soft tissue release was inadequate to balance the pelvis and prevent progression of contralateral hip subluxation, we believed that bilateral hip reconstruction will restore the overall hip biomechanics by correcting asymmetrical hip displacement, addressed coxa valga and femoral malalignment in both hips, improved pelvic obliquity and prevent the risk of subsequent hip displacement. This in return will modify the functional mobility especially in patients with ambulation potential.
We had performed one stage bilateral hip reconstruction in spastic diplegia and quadriplegia who have unilateral hip subluxation. The main reason was due to unsatisfactory result in maintaining hip stability and fair functional improvement observed in patients whom had ipsilateral hip surgery. In our opinion, the hip pathology in diplegic and quadriplegic patients happened in both hips even though they presented only with unilateral hip displacement. Addressing only the subluxated hip will improve the femoral coverage, however imbalance in muscle tension still persisted in the contralateral hip. Thereby, the overall hip and pelvic asymmetry were inadequately corrected by only ipsilateral hip surgery.
In this study, both radiological and functional outcomes were shown to be more significant in patients whom received bilateral hip surgery. The mean MP was stable in both ipsilateral and contralateral hip and no significance increment of MP at last follow-up. Owing to the natural history cerebral palsy, the recurrence of coxa valga may happened in young age, thus may increase the MP annually. However, due to symmetrical hip and balance muscle force cross the hip to maintain pelvic alignment after bilateral hip reconstruction, the MP increment were minimal and did not warranted surgical management in both hip as demonstrated in our study. In contrast, progressive subluxation of contralateral hip as high as 33.3% was observed in unilateral surgery and this is consistent with previous studies. Noonan et al.13 and Shukla et al.17 reported 74.3% and 28% of cases had contralateral hip subluxation in patients underwent unilateral hip stabilization respectively, thus recommended bilateral hip surgery. They found that increased risk of contralateral hip displacement in non-ambulators, in young age (<6 years), high contralateral initial MP (>25%) and those with GMFCS IV and V. While there are number of studies recommended bilateral hip stabilization, there were lack of reports on the outcomes of prophylactic hip surgery. Hence, our study is one of the fewer that evaluate the outcome of the prophylactic VDRO.
Another important parameter associated with the outcome of hip surgery is pelvic obliquity. Balancing both hip by correcting bone deformity and soft tissue contracture may help to improve pelvic obliquity. In this study, we measured improvement of pelvic obliquity with pelvic obliquity angle (POA) and also the difference of MP in both hips (MPD). We used MPD for evaluating pelvic alignment as MP is known to be the most accepted measurement and yield minimal inter-observer differences, yet independent and is little influenced by rotation of the femur, contrary to POA which vastly correlated with supra- or infra-pelvic deformity.25, 26, 27 Interestingly, POA and MPD were correlated significantly in both pre-and post-operation in bilateral hip reconstruction group as observed in our study and reliable as an indicator for hip symmetry. However, we noted that the improvement of POA was not significant in the group of unilateral surgery but MPD was highly significant. Therefore, we concluded that even though MP was improved and MPD were small after hip stabilization surgery, hence hip symmetry achieved; the pelvic obliquity may not change as the opposite hip were in valgus and malrotated with imbalance muscles force. This condition may place the contralateral hip to progress into subluxation and reversal in pelvic alignment.
Our results have shown a significant improvement in the mobility function in bilateral surgery. Of 42 patients, 31 patients had overall functional improvement as compared to unilateral group. As good lever arm and normal hip biomechanics are importance to provide balance posture to sit and ambulate, therefore tremendous progress we observed in these group. Many authors have reported the better in nursing care, improvement of hip motion and eliminate pain in long term outcome after reconstruction. Correction of only one hip may not significantly improved the pelvic obliquity, thereby siting and standing upright balance were compromised, hence failed to demonstrate satisfactory outcome.
Another issue that of concerned were surgical complications in bilateral surgery which thought to be higher that unilateral surgery. Inan et al.31 evaluated surgical complications in uni- and bilateral hip surgery with pelvic osteotomy and demonstrated to be safe with no increased complications as one-stage surgery. Evaluation of early post-operative complication e.g. respiratory problems and anemia, as well as length of hospital stay were found to be similar. These results were consistent with our study; however, surgeon experience may have influenced the rate of surgical complications. Occurrence of intra-operative fracture that happened in our case could be avoided with gentle manipulation and reduction. Peri-implant fractures in this study were due to trauma and occurred after VDRO osteotomy had healed.
There were some limitations in this study. Firstly, as this was a retrospective study, some patients had short follow-up, however we excluded patients less than 18 months follow-up. Long term follow-up until skeletal maturity need to be carried out to further evaluate the outcome. Secondly, standardization of pelvic radiographs was difficult in patients with severe spasticity and poor GMFCS, therefore there might be some errors in establishing the POA which we compensated with MPD. Thirdly, the peri-operative surgical complications assessment was not studied comprehensively, therefore statistical comparison was unable to be carried out. However, the clinical data we obtained in patient records had shown the above discussed findings.
5. Conclusion
Bilateral hip reconstruction in unilateral hip displacement had shown to have satisfactory radiological outcome in correcting unstable hip and pelvic asymmetry, thus improvement in overall functional mobility. Given the benefits of bilateral hip surgery, we advocated this procedure for all spastic diplegia and quadriplegia patients with unilateral hip subluxation. In addition, we suggested MPD as a useful parameter in establishing hip symmetry along with POA as it is reliable and reproducible.
Acknowledgements
The authors thank Suttinan Mechoptham for the contribution in statistical analysis.
Contributor Information
N. Kamisan, Email: azian.kamisan@gmail.com.
V. Thamkunanon, Email: vetham2514@me.com.
References
- 1.Hägglund G., Lauge-Pedersen H., Wagner P. Characteristics of children with hip displacement in cerebral palsy. BMC Muscoskel Disord. 2007;8:101. doi: 10.1186/1471-2474-8-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Terjesen T. The natural history of hip development in cerebral palsy. Dev Med Child Neurol. 2012;54(10):951–957. doi: 10.1111/j.1469-8749.2012.04385.x. [DOI] [PubMed] [Google Scholar]
- 3.Pruszczynski B., Sees J., Miller F. Risk factors for hip displacement in children with cerebral palsy: systematic review. J Pediatr Orthop. 2016;36(8):829–833. doi: 10.1097/BPO.0000000000000577. [DOI] [PubMed] [Google Scholar]
- 4.Flynn J.M., Miller F. Management of hip disorders in patients with cerebral palsy. J Am Acad Orthop Surg. 2002;10:198–209. doi: 10.5435/00124635-200205000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Moreau M., Drummond D.S., Rogala E. Natural history of the dislocated hip in spastic cerebral palsy. Dev Med Child Neurol. 1979;21:749–753. doi: 10.1111/j.1469-8749.1979.tb01696.x. [DOI] [PubMed] [Google Scholar]
- 6.Robin J., Graham H.K., Selber P., Dobson F., Smith K., Baker R. Proximal femur geometry in cerebral palsy: a population-based cross-sectional study. J Bone Joint Surg Br. 2008;90:1372–1379. doi: 10.1302/0301-620X.90B10.20733. [DOI] [PubMed] [Google Scholar]
- 7.Samilson R.L., Tsou P., Aamoth G., Green W.M. Dislocation and subluxation of the hip in cerebral palsy. Pathogenesis, natural history and management. J Bone Joint Surg Am. 1972;54:863–873. [PubMed] [Google Scholar]
- 8.Ramstad K., Terjesen T. Hip pain is more frequent in severe hip displacement: a population-based study of 77 children with cerebral palsy. J Pediatr Orthop B. 2016;25:217–221. doi: 10.1097/BPB.0000000000000282. [DOI] [PubMed] [Google Scholar]
- 9.Hägglund G., Alriksson-Schmidt A., Lauge-Pedersen H. Prevention of dislocation of the hip in children with cerebral palsy: 20-year results of a population-based prevention programme. Bone Joint Lett J. 2014 Nov;96-B(11):1546–1552. doi: 10.1302/0301-620X.96B11.34385. [DOI] [PubMed] [Google Scholar]
- 10.Rutz E., Vavken P., Camathias C., Junermann S., Brunner R. Long-term results and outcome predictors in one-stage hip reconstruction in children with cerebral palsy. J Bone Joint Surg Am. 2015;97:500–506. doi: 10.2106/JBJS.N.00676. [DOI] [PubMed] [Google Scholar]
- 11.Mallet C., Ilharreborde B., Presedo A., Mazda K. One-stage hip reconstruction in children with cerebral palsy: long-term results at skeletal maturity. J Child Orthop. 2014 May;8:221–228. doi: 10.1007/s11832-014-0589-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barakat M.J., While T., Pyman J., Gargan M., Monsell F. Bilateral hip reconstruction in severe whole-body cerebral palsy: ten-year follow-up results. J Bone Joint Surg Br. 2007;89:1363–1368. doi: 10.1302/0301-620X.89B10.18446. [DOI] [PubMed] [Google Scholar]
- 13.Noonan K.J., Walker T.L., Kayes K.J., Feinberg J. Effect of surgery on the nontreated hip in severe cerebral palsy. J Pediatr Orthop. 2000;20:771–775. doi: 10.1097/00004694-200011000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Canavese F., Emara K., Sembrano J.N., Bialik V., Aiona M.D., Sussman M.D. Varus derotation osteotomy for the treatment of hip subluxation and dislocation in GMFCS level III to V patients with unilateral hip involvement. Follow-up at skeletal maturity. J Pediatr Orthop. 2010;30:357–364. doi: 10.1097/BPO.0b013e3181d8fbc1. [DOI] [PubMed] [Google Scholar]
- 15.Abdo J.C.M., Forlin E. Hip dislocation in cerebral palsy: evolution of the contralateral side after reconstructive surgery. Rev Bras Ortop. 2016;5:329–332. doi: 10.1016/j.rboe.2015.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Owers K.L., Pyman J., Gargan M.F., Witherow P.J., Portinaro N.M. Bilateral hip surgery in severe cerebral palsy a preliminary review. J Bone Joint Surg Br. 2001;83:1161–1167. doi: 10.1302/0301-620x.83b8.11266. [DOI] [PubMed] [Google Scholar]
- 17.Shukla P.Y., Mann S., Braun S.V., Gholve P.A. Unilateral hip reconstruction in children with cerebral palsy: predictors for failure. J Pediatr Orthop. 2013;33:175–181. doi: 10.1097/BPO.0b013e31827d0b73. [DOI] [PubMed] [Google Scholar]
- 18.Silver R.L., Rang M., Chan J., de la Garza J. Adductor release in non-ambulant children with cerebral palsy. J Pediatr Orthop. 1985;5:672–677. doi: 10.1097/01241398-198511000-00008. [DOI] [PubMed] [Google Scholar]
- 19.Carr C., Gage J.R. The fate of the nonoperated hip in cerebral palsy. J Pediatr Orthop. 1987;7:262–267. doi: 10.1097/01241398-198705000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Gordon J.E., Parry S.A., Capelli A.M., Schoenecker P.L. The effect of unilateral varus rotational osteotomy with or without pelvic osteotomy on the contralateral hip in patients with perinatal static encephalopathy. J Pediatr Orthop. 1998;18:734–737. [PubMed] [Google Scholar]
- 21.Sung K.H., Kwon S.S., Chung C.Y. Fate of stable hips after prophylactic femoral varization osteotomy in patients with cerebral palsy. BMC Muscoskel Disord. 2018;19:130. doi: 10.1186/s12891-018-2049-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Park M.S., Chung C.Y., Kwon D.G., Sung K.H., Choi I.H., Lee K.M. Prophylactic femoral varization osteotomy for contralateral stable hips in non-ambulant individuals with cerebral palsy undergoing surgery: decision analysis. Dev Med Child Neurol. 2012;54:231–239. doi: 10.1111/j.1469-8749.2011.04172.x. [DOI] [PubMed] [Google Scholar]
- 23.Reimers J. The stability of the hip in children: a radiological study of results of muscle surgery in cerebral palsy. Acta Orthop Scand. 1980;184:1–100. doi: 10.3109/ort.1980.51.suppl-184.01. [DOI] [PubMed] [Google Scholar]
- 24.Hägglund G., Lauge-Pedersen H., Persson M. Radiographic threshold values for hip screening in cerebral palsy. J Child Orthop. 2007;1:43–47. doi: 10.1007/s11832-007-0012-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Patel J., Shapiro F. Simultaneous progression patterns of scoliosis, pelvic obliquity, and hip subluxation/dislocation in non-ambulatory neuromuscular patients: an approach to deformity documentation. J Child Orthop. 2015;9:345–356. doi: 10.1007/s11832-015-0683-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hodgkinson I., Bérard C., Chotel F., Bérard J. Pelvic obliquity and scoliosis in non-ambulatory patients with cerebral palsy: a descriptive study of 234 patients over 15 years of age. Rev Chir Orthop Reparatrice Appar Mot. 2002;88:337–341. [PubMed] [Google Scholar]
- 27.Morrell D.S., Pearson J.M., Sauser D.D. Progressive bone and joint abnormalities of the spine and lower extremities in cerebral palsy. Radiographics. 2002;22:257–268. doi: 10.1148/radiographics.22.2.g02mr19257. [DOI] [PubMed] [Google Scholar]
- 28.Sales de Gauzy J. Pelvic reorientation osteotomies and acetabuloplasties in children. Surgical technique. Orthop Traumatol Surg Res. 2010;96:793–799. doi: 10.1016/j.otsr.2010.07.004. [DOI] [PubMed] [Google Scholar]
- 29.Robb J.E., Brunner R. A Dega-type osteotomy after closure of the triradiate cartilage in non-walking patients with severe cerebral palsy. J Bone Joint Surg Br. 2006;88:933–937. doi: 10.1302/0301-620X.88B7.17506. [DOI] [PubMed] [Google Scholar]
- 30.Abel M.F., Blanco J.S., Pavlovich L., Damiano D.L. Asymmetric hip deformity and subluxation in cerebral palsy: an analysis of surgical treatment. J Pediatr Orthop. 1999;19:479–485. doi: 10.1097/00004694-199907000-00011. [DOI] [PubMed] [Google Scholar]
- 31.Inan M., Senaran H., Domzalski M., Littleton A., Dobney K., Miller F. Unilateral versus bilateral peri-ilial pelvic osteotomies combined with proximal femoral osteotomies in children with cerebral palsy: perioperative complications. J Pediatr Orthop. 2006;26:547–550. doi: 10.1097/01.bpo.0000226277.08825.c2. [DOI] [PubMed] [Google Scholar]